Bowel pain is the most common complaint in bowel diseases. Medical experts describe aching, colicky and cramping pain in the intestines. The intestines begin to hurt after spasms. Severe pain in this organ is a clear sign of diseases that affect the large or small intestine. The process of spasms leads to the accumulation of lactic acid in the body, which negatively affects the nerve endings and causes pain.
Severe pain in the intestines is the result of poor nutrition, a side effect after taking medications, or an inflammatory process. Inflammatory processes in the intestines are accompanied by pain syndromes, nausea, bloating, and colic.
The patient feels discomfort in the intestinal area after long-term diets and fasting. The human body secretes an excessive amount of gastric juice, which leads to pain syndromes.
Types of intestinal pain
Medical specialists distinguish several types of pain:
- Acute pain in the intestines. Acute pain in the intestines is accompanied by disorders of the gastrointestinal tract. The patient suffers from diarrhea and constipation. The feeling of discomfort disappears after bowel movement.
- Aching dull pain in the intestines. Aching pain intensifies with coughing and physical activity. Such pain syndromes are characteristic of inflammatory bowel diseases.
- Cramping pain is typical in advanced cases.
- Colicky pain in the intestines recurs at intervals of several minutes and lasts for several days.
Causes of pain in the intestines
Among the most common causes of abdominal pain are the following:
- Inflammation of the intestinal mucosa.
Under the influence of the inflammatory process, the small or large intestine is irritated. Patients also experience inflammation of the sigmoid colon or appendix.
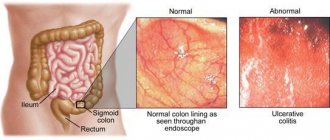
- Autoimmune diseases.
During disturbances in the functioning of the immune system, the body begins to produce antibodies against colon tissue. This process leads to the development of ulcerative colitis.
- Inflammatory process.
The inflammatory process indicates intestinal pathology. The disease has different origins and etiologies. The patient develops pathological processes in the intestinal mucosa, which result in a decrease in the functionality of the organ.
- Pain in the intestines during pregnancy.
During pregnancy, the size of the uterus increases monthly. The growth of the uterus provokes the appearance of pain in the intestines and stimulates the development of pathological processes in the organ.
- Acute intestinal obstruction.
This diagnosis indicates the appearance of neoplasms, tumors, and foreign bodies in the human body.
- Mesenteric thrombosis.
Mesenteric thrombosis is a blockage of the arteries supplying the intestines by a thrombus. Necrosis occurs, popularly known as necrosis of a section of the intestine with severe pain that cannot be relieved by taking painkillers.
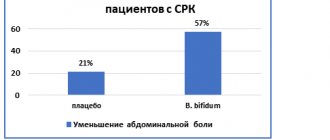
- Irritable bowel syndrome.
Appears in the body as a result of gastrointestinal disorders. The patient is diagnosed with acute pain in the intestines, accompanied by bloating and cramping pain. Irritable bowel syndrome refers to a disorder of the gastrointestinal tract, as well as frequent constipation.
- Chronic pancreatitis.
Chronic pancreatitis is an inflammatory process of the pancreas, in which the amount of digestive enzymes in the body decreases. This disease is the result of insufficient food processing and fermentation processes with the release of gases.
SMT clinic, multidisciplinary medical center
Most often, intestinal pain is localized in the iliac regions on the left. Recall that the iliac region is located in the lower part of the abdominal cavity. The pain intensifies during meals, and after taking antispasmodics, during bowel movements, or when gas is released, it decreases.
Why do antispasmodics help with intestinal pain?
The principle of action of antispasmodics is based on a lowering effect on the tone of smooth muscle organs, or on a disruptive effect on nerve impulses associated with smooth muscles. In other words, the drugs prevent spasm. The latter creates a painful contraction of the intestinal muscles.
Another feature of pain in the intestines is their rare occurrence at night. As a rule, the nature of the pathology comes in waves, with an increase in the daytime and intensification after eating food.
Pain in the intestines may be accompanied by constipation or diarrhea. The latter arises from urges. After going to the toilet, the feeling of incomplete bowel movement persists. In the case of constipation, with pain, sheep feces or other dense masses are often released.
Additional accompanying symptoms:
- bloating;
- stretching;
- flatulence;
- rumbling stomach.
Symptoms of anxiety
Pain in the intestines is not always harmless. Immediately make an appointment with a doctor if, in addition to pain in the intestines, you observe:
- weight loss;
- presence of blood in the stool;
- fever, rise in temperature;
- weakness.
Statistically, 1% of people experiencing intestinal pain have colitis. Food intolerance/irritable bowel syndrome occurs in 25% of cases. In 6% of cases, we are talking about thyroid dysfunction (especially important for residents of endemic regions, for example, for residents of the Urals). Tumors occur in 0.3% of cases. In statistics, much depends on the gender and age structure of patients.
What to do?
Regardless of age and personal prejudices regarding the disease, make an appointment with a doctor.
If symptoms of anxiety are identified, or additional risk factors are identified (for example, age), the patient will be prescribed additional examination, including an endoscope. If there are no deviations, we will establish a diagnosis and examine visceral sensitivity.
About visceral sensitivity in the context of pain in the intestines
Irritable bowel syndrome can be caused by stress, infections, smoking, medications, and certain types of foods. Gut sensitivity is how it responds to physiological stimuli. As you know, even strong fear or any other emotional impact causes gastrointestinal reactions.
Other accompanying symptoms indicating the possibility of other pathologies:
- persistent disruption of food digestion may indicate bacterial overgrowth in the intestines;
- fever, palpable inflammation in the left lower quadrant of the abdomen - signs of diverticulitis;
- endometriosis in women is accompanied by enlarged lymph nodes.
Don't diagnose yourself - make an appointment with a doctor.
Treatment of intestinal pain
To make a diagnosis, symptoms alone are not enough, so the doctor prescribes an additional examination, including:
- A coprogram is a detailed examination of stool, with the help of which medical experts determine the nature of the completeness of food digestion. This diagnostic test determines whether the patient is suffering from gastrointestinal disorders.
- Bacteriological examination of stool. Bacteriological examination of stool provides informative data about the presence of the causative agent of intestinal infection in the body and the ratio of bacteria of healthy and opportunistic flora.
- Endoscopy. An endoscopic examination of the body is carried out by inserting a fiber optic tube into the upper or lower parts of the gastrointestinal tract. The fiber optic tube is equipped with a special camera and lighting. This diagnostic examination makes it possible to directly see the condition of the mucous membrane.
- Colonoscopy. An intestinal examination is performed using a device that allows you to visually evaluate the surface of the intestinal walls.
- Computed tomography can detect tumor diseases and internal changes in organs.
After a diagnostic examination, the patient is prescribed anti-inflammatory drugs. This group of medications will relieve pain syndromes and stop the progression of the disease.
For consultation, tests and various studies, we advise you to contact the private clinic “KDS Clinic”. You will receive qualified assistance, attention from the best proctologists in the Russian Federation and treatment at affordable prices. For more accessible information about services, please visit the official website of our medical institution.
The most accurate methods for diagnosing intestinal diseases are colonoscopy and computed tomography. These diagnostic examinations have a number of contraindications. Computed tomography and magnetic resonance imaging are strictly prohibited:
- Children under sixteen years of age. The human body at this age is quite weak, so diagnostic tests using radiation can damage healthy organs.
- Pregnancy or lactation period. During pregnancy, computed tomography and magnetic resonance imaging are contraindicated. They can harm the condition of the fetus, especially in the early stages. During the lactation period, computed tomography and magnetic resonance imaging are not performed. If these diagnostics are necessary, then it is advisable for the woman to express milk after the procedure and refrain from feeding the baby for 48 hours.
The medical specialist diagnoses and treats intestinal diseases and conducts a comprehensive examination. We invite you to make an appointment with a proctologist and endoscopist.
IRRITABLE BOWEL SYNDROME
Irritable bowel syndrome (IBS) is a disorder of motor-evacuation function, manifested by abdominal pain and/or defecation disorders. IBS develops as a result of psychological, visceral and other influences on an overreacting intestine.
Prevalence
IBS is the most common disease of internal organs. According to our data, it affects 26.2% of the working population [1]. It can appear at any age, including children. In women, IBS is 2-3 times more common.
Despite the extreme prevalence of IBS, approximately 75% of the adult population do not consider themselves sick and do not seek medical help. The exception is people with deviations in the psycho-emotional personality profile. Psychopathological disorders are characterized by a shallow level of damage (neuroses and neurotic reactions). In some patients, endogenous psychoses are possible (schizophrenia, circular psychosis, involutional melancholia, etc.). Concomitant psycho-emotional disorders aggravate the course of IBS and lead to a decrease or even loss of ability to work. As a rule, IBS in these cases is difficult to treat. The quality of life of such patients is so low that it can be compared with the quality of life of patients with type 1 diabetes. Often such patients have some kind of endogenous disease and are subject to examination and treatment by a psychiatrist. The vast majority of patients with IBS have psychopathological disorders of a shallow level; such patients are under the supervision of a therapist and gastroenterologist.
Etiology and pathogenesis
Psychoemotional disorders play a role in the etiology and pathogenesis of IBS. The role of psychoemotional disorders is confirmed by the following observations:
- IBS patients who visit doctors have a history of chronic stress;
- when examined by a psychoneurologist, they are diagnosed with neuroses, neurotic personality development or psychopathy;
- All patients with IBS experience autonomic disorders with a predominance of parasympathetic influences.
The importance of intestinal infections in the etiology of IBS is confirmed by the fact that in approximately 30% of patients the onset of the disease was preceded by an acute intestinal infection. In the pathogenesis of chronic disease, intestinal dysbiosis and damage to the enteric nervous system by antigens of acute intestinal infections are important [2].
Clinical picture
The leading symptoms of IBS are pain, abdominal discomfort and bowel movements. Often in the feces you can see a large amount of mucus, the secretion of which is stimulated by the influence of parasympathetic innervation on the function of goblet cells. On examination, a spastically contracted, painful colon is palpated. Spasm of various parts of the colon, as well as pain on palpation, is observed inconsistently and can change localization on different days.
Patients with IBS have many extraintestinal symptoms, some of which are associated with dysfunction of other digestive organs, and others with disorders of the autonomic nervous system and psychological status. The latter cause rapid fatigue, weakness, headaches, decreased appetite, sleep disturbances, paresthesia, palpitations, sweating, attacks of “lack of air,” frequent urination, low-grade fever, etc. Patients often suffer from cancerophobia.
There are three main types of IBS: constipation-predominant, diarrhea-predominant, and pain-predominant.
Diagnosis
The diagnosis of IBS can be made based on typical clinical symptoms in the absence of other intestinal diseases, which are excluded during additional studies. During proctological examination, anal sphincter spasms and pain are often observed. Colonoscopy reveals intestinal hyperkinesia of a spastic type. Persistent spasm often prevents insertion of the endoscope and causes significant pain. The intestinal mucosa looks somewhat swollen, hyperemic, often with deposits of mucus on the intestinal walls. Due to increased tone, the folds are thickened and rough. We noticed that changes in the intestine in patients with IBS are transient and are often not detected during removal of the device from the intestine. When examined using a barium enema, dyskinesia and an increase in the number of haustrations are often detected [3].
Clinical criteria for IBS have been repeatedly improved. Currently, the Rome II Criteria (2000) are used to diagnose IBS in adults [4].
"Roman Criteria-II (2000)"
For at least 12 weeks (not necessarily consecutive) in the past 12 months, you have experienced abdominal discomfort or pain that has at least two of the following three characteristics:
- decrease after defecation;
- onset is associated with a change in stool frequency;
- the onset is associated with a change in the shape of the stool.
Thus, the clinical diagnosis of IBS is based on identifying functional disorders associated with intestinal function in the patient. IBS is diagnosed only if there is a connection between pain and discomfort in the abdomen and stool. Symptoms appear before stool and subside after a bowel movement, depending on changes in stool regularity or consistency.
To prevent diagnostic errors, you should pay attention to a number of symptoms that are not typical for IBS, which may indicate the presence of organic diseases (the so-called “alarm” symptoms or “red flags”).
Symptoms of anxiety
- Rectal bleeding
- Losing body weight
- Chronic diarrhea
- Anemia
- Fever
- Onset of the disease in persons over 50 years of age
- Family history (cancer and inflammatory bowel disease in parents)
- The appearance of pain and diarrhea at night
However, the presence of “anxiety” symptoms is not yet a reason to exclude IBS in such patients. Thus, the onset of the disease in people over 50 years of age is quite possible, but mandatory instrumental examination is required. Rectal bleeding may be due to hemorrhoids; loss of body weight and low-grade fever are manifestations of depression or hypochondriacal syndrome.
Differential diagnosis
Differential diagnosis should be carried out if the following diseases are present:
- malabsorption diseases;
- inflammatory bowel diseases;
- intestinal tumors;
- endocrine enteropathy;
- hypolactasia and other types of disaccharidase deficiency.
The differential diagnosis of IBS with diseases of the small intestine should be based on the exclusion of symptoms of impaired absorption characteristic of the pathology of this part of the intestine. Malabsorption syndrome is manifested by quantitative (body weight deficiency) and qualitative (trophic disorders) nutritional disorders.
With IBS, a lack of body weight is often observed, but it is not associated with impaired assimilation of nutrients, but with peculiarities of the neuropsychic status or with poor appetite. There are no qualitative trophic disorders in patients with IBS.
Qualitative nutritional disorders are manifested by dryness and flaking of the skin, changes in its color (a kind of dirty gray tint), the appearance of pigment spots on the face, hands and legs, and other trophic disorders. In contrast to diarrhea with impaired absorption in IBS, the stool is scanty in volume.
Differential diagnosis with inflammatory diseases is based on the correct interpretation of the results of instrumental studies, including biopsy. Unlike inflammatory diseases, blood is never found in the stool with IBS.
Treatment
Treatment of IBS should be comprehensive and affect the main pathogenetic mechanisms.
Medical nutrition. For patients with predominant constipation, diet No. 3 with the addition of wheat bran is indicated. If diarrhea predominates during an exacerbation, it is recommended to limit foods rich in fiber (diet No. 4c).
Correction of psycho-emotional disorders. A psychoneurologist or psychotherapist proficient in methods of psychotherapy and psychotropic pharmacotherapy should be involved in the treatment of patients with concomitant neuroses and other deviations from the norm in their psycho-emotional status. A set of measures aimed at improving the functions of the central nervous system and correcting autonomic disorders includes psychotropic drugs, rational psychotherapy, and hypnosuggestive effects. Optimally, the diagnosis of psycho-emotional disorders and their elimination should be carried out by a neuropsychiatrist or psychotherapist, or, even better, a specially trained gastroenterologist.
Antibacterial and bacterial drugs. Antibacterial drugs are prescribed to most patients with IBS in order to free the body from pathogens of acute intestinal infections during long-term persistence in the intestine (including in the intestinal wall), suppress excessive bacterial growth in the upper parts of the small intestine and eliminate dysbiosis of the large intestine [5].
Clinical indications for the use of antibacterial drugs for IBS are diarrhea, flatulence and abdominal pain. Antibacterial drugs are used in courses of 7-10-14 days.
Biseptol (Septrin, Bactrim), furazolidone, ersefuril, metronidazole (Trichopol), as well as oxyquinoline derivatives, quinolones intetrix, nitroxoline and nevigramon are recommended.
After antibacterial therapy, long-term (up to 1.5-2 months) use of bacterial preparations (probiotics) is recommended: bifidum- and lactobacterin, bifiform, hilaka-forte, etc.
Regulators of intestinal motor-evacuation function. For diarrhea, imodium (loperamide) and alosetron, a selective competitive antagonist of serotonin 5-HT3 receptors, have a symptomatic effect.
For patients with predominant constipation, prokinetics cerucal and motilium are indicated. For persistent pain, antispasmodics pinaverium bromide (dicetel) - the prototype of a new class of Ca2+ antagonists - and duspatalin (mebeverine) have a good effect.
Symptomatic remedies. All patients with IBS with exacerbation of diarrhea are prescribed astringent, antispastic, enveloping and neutralizing organic acids drugs: smecta, bismuth nitrate, dermatol, tanalbin, white clay, calcium carbonate, as well as herbal decoctions of similar action (chamomile, peppermint, St. John's wort, alder pine cones, blueberries and bird cherry). For a similar purpose, you can use some antacid drugs (Almagel, phosphalugel, Maalox) and drugs containing bismuth (Venter).
In case of IBS with a predominance of constipation, it is necessary to teach patients how to develop the lost morning reflex to defecation and increase the amount of dietary fiber in the diet by introducing wheat bran into it. To stimulate defecation at the first stage of developing the lost reflex, Duphalac (lactulose) should be prescribed the night before, 1-2 dessert spoons. Duphalac has a mild laxative effect based on an increase in osmotic pressure in the intestinal lumen, and does not irritate its overly sensitive receptors. In addition, Duphalac reduces the pH of the intestinal environment and promotes the growth of acidophilus bacteria.
The condition of patients with IBS, the effectiveness of treatment and prognosis largely depend on the severity of concomitant psychopathological manifestations. In achieving sustainable clinical remission, overcoming intrafamily, public and social conflicts that are the cause of the formation of neurosis in the patient is often crucial.
The ability to work of patients with IBS and the prognosis for this disease largely depend on the severity of concomitant psycho-emotional disorders.
For questions about literature, please contact the editor