Symptoms
The symptoms of a rectocele depend on the organ that descends along with the back wall of the vagina. In principle, all symptoms can be divided into two groups:
- Symptoms associated with rectal prolapse: difficulty defecating, the need to squeeze feces out of the protrusion of the posterior vaginal wall, the need to empty the formed “pocket” in the rectum independently (with a finger through the anus), defecation in portions, incontinence of gases and stool (when combined with damage to the sphincter rectum).
- Specific symptoms arising from prolapse of the loops of the small intestine and omentum are either completely absent or are expressed in pulling sensations in the lower abdomen, bloating and flatulence.
Common to both groups is the feeling of a foreign body in the vagina, possible injury to prolapsed mucosa when walking, dryness of the vaginal mucosa, and discomfort during sexual intercourse. Considering the fact that the contents of the hernial protrusion can be heterogeneous, the symptoms are also often mixed.
| anonymously to the doctor, through the feedback form, we will try to help you. | Ask a Question |
Causes
The main causes of diverticular disease are:
- Dystrophic changes in the muscle wall of the large intestine
- Changes in her motor skills, weakness of the muscle component
- Impaired blood supply to the intestinal wall and the development of atherosclerosis with ischemic changes
Increased intraintestinal pressure due to prolonged spasm, leading to divergence of muscle fibers.
Diverticula are the final manifestation of intestinal wall disease, atrophy and expansion in sloping areas.
There are some prerequisites for the development of diverticula in the colon:
- the presence of an outer muscle layer in the form of three stripes, helping to weaken the intestine before external and internal influences
- the presence of haustra, in which increased intraintestinal pressure is generated
Causes
The causes of rectocele are the same as for other forms of prolapse: childbirth and pregnancy, heavy physical activity, chronic constipation and, of course, a hereditary factor. Despite this, it is with this type of vaginal prolapse that labor and constipation play a special role.
The first factor is especially important in the case of episiotomy (perineal incision during childbirth) and perineal ruptures (large fetus, rapid (very fast) labor, incorrect obstetric care).
At this moment, the main “defender” of the posterior wall of the vagina, the perineum and pelvic floor muscles, suffers; without them, the entire load falls on the thin fascia separating the vagina and rectum. That is why any surgical treatment always includes reconstruction of the perineum. The second most important factor is chronic constipation.
In the presence of this pathology, the supporting structures of the posterior wall experience constant high loads, as a result of which a rupture of the fascia occurs, through which part of the rectum emerges.
| Most patients receive care for free (without hidden additional payments for “network”, etc.) as part of compulsory health insurance ( under the compulsory medical insurance policy ). | Application for treatment under compulsory medical insurance |
Megacolon - symptoms and treatment
Diagnosis of megacolon begins with examination of the patient. On examination , an enlarged abdomen is usually noticeable. Muscle tension in the anterior abdominal wall may be present. Percussion (tapping) usually produces a tympanic sound (loud, medium-high or high-frequency sound, similar to the sound of beating a drum).
A digital examination of the rectum reveals dense stool above the anorectal ring. Digital examination of the rectum in patients with Hirschsprung's disease may be accompanied by the release of large amounts of fecal content.
In patients with megarectum, the rectum may be filled and distended with fecal matter, which often leads to a gaping anus due to secondary dysfunction of the internal anal sphincter. In such patients, incontinence (failure to retain feces) and leakage of liquid stool may be present.
Differential diagnosis of megarectum must be carried out with various types of intestinal obstruction:
- malignant neoplasms of the large intestine;
- fecal blockage is a complication of chronic constipation, in which the intestines do not empty for a long time, and the feces become compacted and subsequently turn into stones;
- intussusception is a pathological condition in which one part of the intestine invades another, resulting in intestinal obstruction;
- rectal prolapse - partial or complete prolapse of the rectum beyond the anus;
- anal atresia - absence of the anus.
Laboratory research:
- Determination of blood electrolytes (potassium, sodium, chlorine, calcium, magnesium, phosphorus). It is necessary to exclude intestinal obstruction of another etiology, for example, acute pseudo-obstruction of the colon (Ogilvie's syndrome), which is accompanied by electrolyte disturbances, primarily potassium loss.
- Determination of thyroid function. Hypothyroidism, caused by decreased thyroid function, can cause slower bowel movements. Laboratory indicators for hypothyroidism:
- thyroid-stimulating hormone (TSH) - increased;
- total and free triiodothyronine (T3) - reduced;
- total and free thyroxine (T4) - reduced.
For primary diagnosis, a plain radiography of the abdominal cavity . This helps to clarify the situation and assess its severity.
After a plain X-ray of the abdominal cavity indicating the presence of megacolon, in most cases it is recommended to perform irrigography (irrigoscopy) (X-ray examination of the abdominal cavity using a contrast agent) [12]. This study allows you to safely assess the size of the large intestine and the location of its anatomical sections, as well as find out which area is pathologically dilated. Irrigography is also used to assess the potential ability to empty the large intestine using conservative methods [24].
It is possible to make a differential diagnosis between a total slowdown in the functioning of the large intestine and a functional obstruction at the exit (rectosigmoid obstruction) by monitoring the passage of a radiocontrast substance through the intestine. At least two days before the test, the patient is recommended to take 30 g of dietary fiber daily, and also avoid taking laxatives and performing enemas. The patient drinks a contrast agent and then has a plain abdominal x-ray on days one, three, and five to accurately determine bowel patency and the location, shape, and function of the colon.
In patients with a total slowdown in the functioning of the large intestine, the passage of the contrast agent through the intestine slows down and spreads from the cecum to the rectum. While in patients with a functional obstruction at the outlet (rectosigmoid obstruction), the contrast agent moves through the intestines at a normal pace and then accumulates in the rectum.
Anorectal manometry can help in the differential diagnosis of congenital and acquired megacolon This is a research method that allows you to evaluate the tone of the anorectal muscle complex, as well as the coordination of contractions of the walls of the anal sphincters and rectum. The test is carried out by inserting a rectal tube connected to a device that measures the pressure exerted by the anal sphincters. If, in response to stretching of the rectal wall, the internal sphincter of the anus relaxes and the external sphincter contracts, the patient does not have Hirschsprung's disease. If this reflex is absent, a rectal biopsy is necessary to confirm the diagnosis of Hirschsprung's disease.
Testing for conduction delay along the pudendus (pudendal nerve) may reveal problems related to intestinal motility, as well as mechanical and/or anatomical problems with defecation. The study is carried out using electrodes that are attached to the skin at the site where the nerves being studied pass through. An electrical current stimulates nerve activity, and electrodes measure the speed and strength of electrical signals passing through the nerve. If the nerve is damaged, the current will flow slowly and weakly.
Colonoscopy is necessary to exclude an obstructive cause of intestinal dilatation (narrowing or closing of the intestinal lumen). During colonoscopy, the large intestine is examined using a special optical device - a colonoscope, which allows you to examine the walls and lumen of the intestine.
Histological examination allows us to determine the etiology (cause) of the disease. Fine needle biopsy is the established standard for diagnosing Hirschsprung's disease. However, in most cases, aspiration biopsy of the mucous membrane is sufficient to establish the diagnosis. The disease is characterized by the absence of nerve cells, so Hirschsprung's disease cannot be excluded or confirmed by routine manometric studies. In other cases, a biopsy is not indicated, since the presence of nerve cells is normal.
Diagnostics
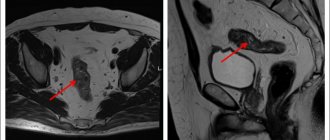
Diagnosis of rectocele consists of collecting the patient’s complaints, ascertaining the history of the disease and life. This allows us to determine the causes of the disease and suggest existing anatomical defects of the pelvic floor. Next, a standard gynecological examination is performed, which gives an idea of the degree of prolapse and the condition of the perineum. There are four degrees of rectocele:
- 1st degree – when there is a slight prolapse, which is determined only during a gynecological examination and does not reach the entrance to the vagina by more than 1 cm;
- 2nd degree - when the prolapse of the posterior wall does not reach the entrance to the vagina a little or falls below it, but not more than 1 cm;
- 3rd degree - in this case, the rectocele descends more than 1 cm from the entrance to the vagina, but no more than 5-7 cm;
- 4th degree – complete inversion of the posterior vaginal wall.
To clarify what exactly comes out along with the back wall of the vagina, a gynecological examination is always supplemented by a digital rectal examination - examination of the rectum with a finger through the anus.
Treatment
Treatment of rectocele includes both conservative and surgical methods. The first group includes training the pelvic floor muscles, aimed at increasing their tone. Exercises can be effective only in the initial stages of prolapse and in patients with preserved muscle apparatus. This type of treatment can show real results in young women, especially in the first year after childbirth. A separate issue is the correctness of the exercises (it is not entirely clear what needs to be reduced and whether it is reduced), on which their effectiveness depends.
For control, biological feedback devices (BFB therapy) have been created, which can increase the effectiveness of training several times. Another non-surgical treatment option is pessaries. This is a whole group of devices of various shapes and sizes, made of rubber or silicone. The pessary is inserted into the vagina and blocks the way out for prolapsed organs.
Unfortunately, this device causes chronic inflammation, discomfort and requires regular replacement, which means visiting a gynecologist.
general description
Diverticular disease of the colon is a chronic disease in which pouch-like protrusions through the muscle layer form in the wall of the large intestine.
The protrusions themselves form in weak spots of the intestinal wall, where blood vessels pass through it. Typically, the size of diverticula varies from 5 to 10 mm. Diverticular disease includes:
- Diverticulosis - the presence of several diverticula in the intestine
- Diverticulitis - inflammation of the diverticulum
The prevalence of the disease among young people is very low - about 2-5%, with obese men most affected. With age, the risk of developing the disease increases and by the age of 70-80 reaches 65%. Up to 70 years of age, the incidence among men prevails over women.
Operation
Video lecture for patients and colleagues. Prolapse of the uterus, bladder, rectum: symptoms, diagnosis, treatment, surgery. urologist, MD Shkarupa Dmitry Dmitrievich
The main treatment method for rectocele is surgery. Moreover, both gynecologists and proctologists (transanal reconstruction) deal with this pathology. However, according to international standards, the vaginal route is preferable, as it is more effective and safe. Surgery for rectocele consists of repairing the fascial defect (colporrhaphy) between the rectum and vagina, as well as reconstructing damaged structures of the perineum.
It has been proven that the use of synthetic prostheses in this case does not improve results, but significantly increases the risk of complications.
During the operation, it is very important to correctly reassemble the damaged fascia and perineum and excise old scars; otherwise, pain may occur, including during sexual intercourse, as well as problems with defecation. Moreover, the cosmetic effect will also largely depend on the experience of the surgeon.