All vital organs for humans are located in the abdominal cavity. Neglect of sterility, incorrect injection or surgical intervention as part of the treatment process is fraught with serious complications. These include local tissue inflammation, suppuration, and sepsis. One of the most dangerous consequences is the accumulation of infiltrate in the retroperitoneal space. Toxic substances and dead cells form a compaction, which leads to a deterioration in well-being. The neoplasm requires immediate treatment in a hospital setting.
Definition of abdominal infiltrate and ICD-10 code
Infiltration of the abdominal cavity is a pathological compaction of dead cells, lymph, and blood. Cellular elements accumulated in the peritoneal area are not normally characteristic of this area of living tissue.
The infiltrate is characterized by increased density and tends to increase in size.
Since infiltration is not an independent disease, it cannot be found in the International Classification of Diseases (ICD) 10th revision. The exact ICD-10 code depends on the type of inflammation. For example, post-injection seal should be searched for code T80.8. If the neoplasm is associated with a ruptured appendix, then the pathology is indicated by code K35.3. Lymphoid infiltrate appears with infectious lesions of the body, and tumor infiltrate with oncology. A complete description of the disease is located in the relevant sections of the system.
3. Symptoms and diagnosis
Pathognomonic symptoms - i.e. clinical manifestations specific only and exclusively for an abdominal abscess do not exist. Diagnosis requires a thorough analysis of complaints, anamnesis and dynamics, palpation results, measurement of blood pressure (in the presence of an abscess, blood pressure usually increases) and other indicators.
The clinical picture depends on the specific location of the abscess(s) and can be very different, resembling a number of other pathological conditions with similar symptoms. Thus, there is fever, hypertonicity of the abdominal muscles, frequent urination, dyspeptic symptoms (nausea, vomiting, diarrhea, constipation), all kinds of pain and discomfort with varying irradiation, “forced posture,” increased temperature, etc.
To confirm abscess formation, almost all modern instrumental diagnostic methods are used (depending on the clinical situation) - radiographic, ultrasound, tomography, etc. - as well as laboratory tests, including bacteriological identification of the infectious agent and assessment of its sensitivity to antibiotics.
About our clinic Chistye Prudy metro station Medintercom page!
Causes of abdominal infiltration
Infiltration of the peritoneum occurs as a result of the entry of atypical cells into the cavity naturally or artificially. Most often, pathological compaction is a consequence of an incorrectly performed injection. Antibiotics, alcohol or elements of the anesthetic solution are mixed with blood, lymph and a tumor forms at this site. Factors that influence the development of the disease:
- incorrectly chosen site for drug administration;
- performing an injection with a blunt needle;
- administering the drug to the same place;
- using the wrong needle;
- failure to comply with asepsis rules.
It is worth noting that the technique for performing subcutaneous and intramuscular injections is different. Needles for injections are chosen short and sharp. All instruments must be disposable and sterile.
Other causes of the infiltrative process:
- accumulation of cholesterol in blood vessels;
- accumulation of glycogen in diabetes;
- accumulation of triglycerides in liver cells;
- accumulation of fibrin in the lungs;
- inflammation in the pelvis;
- impregnation of the skin with chemicals.
Postoperative infiltrate appears 1-2 weeks after the intervention. The seal contains alcohols, anesthetics, and antibiotics. The inflammatory variety occurs in acute forms of peritoneal diseases (appendicitis, cholecystitis, peritonitis), immunological problems, allergic reactions or congenital pathologies. Excessive amounts of lymphocytes, white blood cells, lymph and blood accumulate in the affected area.
In the presence of chronic infections, pathogenic bacteria can travel throughout the body through the lymphoid route. In the abdominal cavity they multiply very quickly and form an infiltrate.
A neoplasm in the peritoneum of a tumor nature consists of benign or malignant cells, for example, sarcoma or fibroids.
Infiltrate
The article was prepared by a specialist for informational purposes only. We urge you not to self-medicate. When the first symptoms appear, consult a doctor.
What is infiltration?
Infiltrate is a compaction formed in a tissue area or organ (liver, muscle, subcutaneous tissue, lung), the occurrence of which is caused by the accumulation of elements of cells, blood, and lymph. There are several forms of infiltration. The inflammatory form is formed as a result of the rapid proliferation of tissue cells and is accompanied by the appearance of a significant number of leukocytes and lymphocytes, blood and lymph, which sweat from blood vessels.
The tumor infiltrate consists of cells characteristic of different types of tumors (cancer, fibroids, sarcoma). Its manifestation consists of infiltrated tumor growth. With this formation, a change in the volume of tissue occurs, a change in color, its density and pain increase. The surgical form of infiltration is a compaction that occurs in tissues when they are artificially saturated with an anesthetic, antibiotic, alcohol, and so on.
Causes of infiltration
The reasons why inflammatory infiltrates occur constitute a group with diverse etiological factors. Research revealed that 37% of patients had a traumatic source as the cause of the disease, 23% had an odontogenic infection, and in the remaining patients, the inflammatory infiltrate developed as a result of various infectious processes. This form of the inflammatory process occurs with equal probability in any age category.
Infiltrates of the inflammatory form are often observed in the tissues of the perimaxillary location, in particular in children with the occurrence of pulpitis and periodontitis, which can be confused with reactive processes. The diseases of periadenitis and serous periostitis are also a type of inflammatory infiltrate. To accurately assess the patient’s condition, it is necessary to recognize the non-purulent stage of the process. The group of odontogenic inflammations is of an inflammatory nature, affecting the jaw bones, tissues adjacent to the jaw, and regional lymph nodes.
The causative agents of odontogenic inflammation are considered to be agents representing the microflora of the oral cavity (staphylococci, candida, streptococci and others). Along with them, the cause of the development of a negative process is the resistance of microorganisms, which is determined by specific and nonspecific protective factors, the reactivity of the organism of an immunological nature. Inflammatory infiltrate manifests itself during a contact type infection and through the lymphogenous route of its spread, followed by tissue infiltration.
The cause of the infiltrate may lie in a complicated condition of acute appendicitis. This is an inflammatory type tumor, in its center there is a worm-shaped process and an inflamed condition that occurs in the absence of timely surgical treatment. A type of infiltrate can be post-injection type. It represents a local type of inflammation that develops in the place where the intramuscular injection was given, that is, its cause is improper medical manipulation and violated sanitary rules.
Symptoms of infiltration
The development of the inflammatory infiltrate takes several days. The patient's temperature during this period may be normal or subfebrile (slightly elevated temperature that does not return to normal for a long time). In the affected area, swelling and tissue compaction appear with a clearly visible outline, the area of distribution of which is distributed over one anatomical area or several. Palpation of the affected area may cause severe or mild pain.
It is not possible to determine the presence of fluid (fluctuation for pus, blood) in the resulting cavity. The skin of the lesion is slightly tense, red or slightly hyperemic. In this area, all soft tissues are affected - skin, mucous membrane, subcutaneous fat and muscle tissue, several fasciae with lymph nodes being drawn into the process of infiltration. Infiltrates with traumatic origin are localized in the buccal, maxillofacial region and oral cavity.
The infiltrate, which is based on a complication of acute appendicitis, develops up to 3 days from the onset of the disease. The inflammatory process forms in the lower abdomen on the right side. Its symptoms are a persistent aching pain, a low temperature of up to 37.5°C, there is a possibility of a reverse development of the process, with abscess formation the temperature rises to 39°C, which is accompanied by chills, an abscess is formed and recovery is possible only after the intervention of a surgeon.
Diagnosis of infiltration
Inflammatory infiltrate is diagnosed using a differential approach, which takes into account the factors of the cause and conditions under which the disease occurred, as well as the factor of its duration. The accuracy of the diagnosis is confirmed by the following signs: normal or subfebrile body temperature, clear contours of the infiltrate, sharp pain during palpation, absence of pus in the closed cavity of the inflamed tissue.
Mild distinctive symptoms are: absence of solid intoxication, slight hyperemia of the skin without detecting tension and a shiny effect of the skin. Diagnosis is made difficult by purulent foci, the localization of which is in a space delimited by a group of muscles from the outside. In such cases, the increase in signs of inflammation determines the prognosis of the disease. In doubtful cases, the diagnosis is made based on the results of a puncture from the source of inflammation.
By studying the histological structure of the material obtained from the infiltrate, that is, by conducting a morphological version of the study of the biopsy, it is possible to detect cells typical of the proliferative inflammatory phase in the complete absence or small number of leukocytes of the segmented neutrophil type. This indicator is typical for non-purulent inflammations. In infiltrates, as a rule, yeast and filamentous fungi are found in large clusters. This indicates the presence of dysbacteriosis.
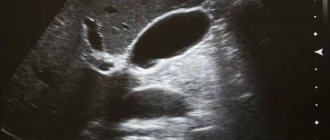
Appendiceal infiltrate is determined during examination by a doctor. As a rule, special diagnostic methods are not used. In cases of suspected abscess formation, an echographic examination is performed. This method clearly shows the structure of the infiltrate and reveals cystic formations with the clear presence of capsules containing heterogeneous fluid, which will be an indicator of the accumulation of purulent exudate.
Treatment of infiltration
The inflammatory infiltrate is treated with conservative methods that combine anti-inflammatory therapy and physiotherapeutic agents (laser irradiation, bandages using Vishnevsky ointment and alcohol). Suppuration of the infiltrate leads to the appearance of phlegmon, then surgical treatment cannot be avoided. Physiotherapy fulfills the main goal - the rehabilitation of infectious foci to eliminate inflammatory processes.
If there are no purulent manifestations in the infiltration or they have a small quantitative content without significant fluctuation and general reaction, physiotherapeutic methods resolve the infiltrate (anti-inflammatory method), reduce swelling (anti-inflammatory method), and relieve pain (analgesic method). Anti-inflammatory therapy is prescribed for dense infiltrate without purulent melting to increase blood flow in the local area and eliminate stagnation.
When using it, the intensity of the effect is important, but in the presence of purulent microflora, the high-intensity technique will provoke a purulent inflammatory form. Other methods with a thermal effect are prescribed in the absence of provocation on their part, preferably on the fourth day after UHF therapy or SUV irradiation. Electrophoresis of antibiotics plays an antibacterial role, and calcium electrophoresis is prescribed to delineate the source of inflammation.
Appendiceal infiltration can be treated only in a hospital setting. It includes therapy with antibacterial drugs, diet and limiting physical activity. Within 14 days, the inflammatory process resolves and recovery occurs. In order to prevent such attacks, after 90 days it is recommended to perform an operation, as a result of which the appendix is removed.
Abscess formation of the infiltrate (formation of a cavity around the appendix filled with pus) requires surgery to open the abscess; in this case, the appendix is preserved. Final recovery will occur after removal of the appendix six months after the abscess was opened.
Author of the article:
Mochalov Pavel Alexandrovich |
Doctor of Medical Sciences therapist Education: Moscow Medical Institute named after. I. M. Sechenov, specialty - “General Medicine” in 1991, in 1993 “Occupational diseases”, in 1996 “Therapy”. Our authors
Clinical picture
Manifestations of infiltration in the peritoneal space depend on the primary disease that caused this complication. However, there are general symptoms that are characteristic of all types of seals:
- dull, aching, prolonged pain in the abdomen;
- protruding navel;
- the appearance of a dent on the skin when pressed;
- hyperthermia;
- disruption of the gastrointestinal tract;
- difficulty in stool.
All soft tissues in the area of accumulation of infiltrate are affected: skin, mucous membrane, muscle, fat. There is swelling of the skin and severe redness. Palpation of the lesion causes pain. In extreme cases of intoxication, the pain becomes unbearable and fever appears.
Endometriotic infiltrate in the abdominal cavity accumulates not only on the surface, but also in the deep layers of the retroperitoneal space. It is a dense lump of rough scar tissue. Accompanied by cramps in the lower abdomen, painful and heavy periods.
Periappendicular infiltrate is localized in the right iliac region. On palpation, it is felt as a painful, dense and immobile formation. Symptoms of peritoneal irritation persist: Shchetkin-Blumberg, Obraztsov, Sitkovsky, Rovzing, etc.
Diagnostics
The first stage in diagnosing abdominal infiltration is taking an anamnesis and physical examination. The doctor palpates the hypochondrium, umbilical area, and lower abdomen. Most often, the Obraztsov-Strazhesko technique is used, which allows one to palpate all the internal organs of the peritoneum. The appearance of a painful syndrome during examination is a sign of a pathological process. To obtain more complete information about the patient's condition, additional tests are prescribed.
Basic methods for examining the abdominal cavity for infiltration:
- Ultrasound. The echographic diagnostic method allows you to determine the structure of the compaction. The presence of fluid inside the capsule indicates its cystic nature.
- Histological analysis. The material is collected by puncture biopsy. The contents and a piece of tissue of the pathological formation are subject to examination.
- CT scan. A more extensive research method. It is carried out only if there is not enough information to make a diagnosis.
2. Reasons
An abdominal abscess develops according to the scenario described above, and in most cases is a complication of diffuse (spread) peritonitis - inflammation of the peritoneum. These types of abscesses, single or multiple, can occur in a variety of areas of the intra-abdominal space and are usually formed as a result of the vigorous activity of several pathogenic and opportunistic cultures at once, which, under favorable conditions, literally “pounce” on healthy tissue.
Abscess formation is often complicated by abdominal injuries, including surgical ones (0.5-1.5% of planned and emergency abdominal surgeries), perforation of stomach and duodenal ulcers, infectious and inflammatory diseases of the gastrointestinal tract and other internal organs.
Visit our Gastroenterology page