Relevance of the problem
Due to the increase in life expectancy of the population, the adverse effects of environmental factors, poor nutrition, and an increase in the level of diagnostics, in recent years there has been a tendency towards an increase in the proportion of patients with concomitant surgical diseases, the frequency of their occurrence ranges from 2.8 to 63%.
As a rule, there is a causal connection between changes in one organ and the development of disease processes in another, sometimes without pronounced subjective and clinical manifestations until these changes move into the sphere of pathological and functional.
In 1985, the World Health Organization published statistics according to which 25-30% of patients subject to surgical treatment for any disease are additionally identified with one or more diseases requiring surgical treatment. However, despite the existence of real opportunities to provide the required volume of medical care to this category of patients and achieve maximum medical, social and economic effect, to date only 1.5-6% of such patients undergo simultaneous surgical interventions.
Simultaneous laparoscopic surgical interventions in surgery and gynecology
Periodically, cases of repeated surgical interventions are identified due to severe complications of concomitant surgical diseases that were not eliminated during the first operation.
Definition of the concept of simultaneous operations
Simultaneous operations
are considered to be operations aimed at simultaneous correction of changes in two or more organs due to their independent diseases.
The extremely low number of simultaneous interventions performed, which does not correspond to the real needs for them, is explained by a number of reasons: incomplete examination of patients in the preoperative period, insufficient intraoperative examination of the abdominal organs, exaggeration of the degree of operational risk when determining the possibility of performing simultaneous operations, the tendency of surgeons to perform multi-stage surgical treatment of concomitant diseases, increased responsibility of the surgeon in the event of a possible unsuccessful outcome of the operation, psychological unpreparedness of surgeons and anesthesiologists to expand the scope of surgical intervention. In our opinion, this is due to the lack of clear, generally accepted, scientifically based principles of treatment tactics for patients with concomitant diseases.
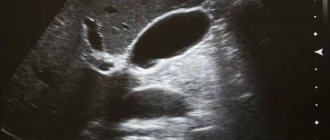
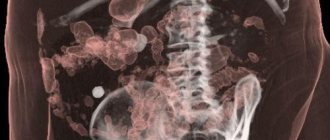
Improving the diagnostic capabilities of practical medicine, improving anesthesiological and resuscitation support for operations and the early postoperative period, the widespread introduction of ultrasound, electrocoagulation, stitching devices and other technical means that allow surgical interventions to be performed less traumatically and for less duration, create real conditions for expanding the scope of surgical interventions and performing simultaneously several operations for combined surgical diseases.
With the advent of minimally invasive endovideosurgical technology, the issue of more active introduction of simultaneous operations into surgical practice and the possibility of expanding the indications for them has become especially relevant. A number of undoubted advantages of laparoscopic techniques, confirmed by numerous studies (reducing the trauma of surgical intervention, reducing intra- and postoperative complications, reducing the length of the patient’s stay in the hospital and the duration of temporary disability, reducing postoperative mortality), creates broad prospects for improving the results of treatment of patients with concomitant diseases .
At the same time, despite the fact that in large hospitals in Russia the percentage of laparoscopic operations performed from the volume of all abdominal operations is 20-30%, and in specialized centers it reaches 70%, the percentage of simultaneous laparoscopic surgical interventions remains just as low, and the above problems in the treatment of patients with combined diseases of the abdominal cavity, pelvis and retroperitoneal space remain unresolved.
When considering combined diseases of the abdominal organs, it is necessary, first of all, to focus on the gastrointestinal tract.
Numerous clinical and experimental studies have confirmed the close connection between all parts of the digestive tract, which make up the physiological system and respond to various changes in other organs. Reflex, neurohumoral, motor, secretory interdependence of the functions of the digestive organs is well known and often determines the pathogenesis of diseases. Functional or anatomical changes in one of them lead to dysfunction of other organs or the entire system.
In particular, patterns of combination of reflux esophagitis caused by a sliding hiatal hernia with cholelithiasis, pancreatitis, gastric and duodenal ulcers, duodenostasis, etc. have been identified. The relationship between hiatal hernia and calculous cholecystitis has been established. A hiatal hernia due to trauma, tension of the trunks and hepatic branches of the vagus nerves and the occurrence of pathological viscero-visceral reflexes can cause dyskinesia of the gallbladder and biliary tract, dysfunction of the pyloroduodenal zone, cholestasis and the formation of gallstones. Over time, the stomach and organs of the hepatopancreatoduodenal zone are involved in the pathological process with the occurrence of functional and then organic disorders. In turn, long-term pathological impulses from the receptors of the vagus nerves in chronic cholecystitis and peptic ulcer disease through viscero-visceral reflexes can lead to the occurrence of a traction hernia of the esophageal opening of the diaphragm.
The opinions of many authors about the interdependence of the above diseases are justified by a significant percentage of their combination - 80.1% of patients with hiatal hernia have concomitant diseases of the abdominal organs. In 15.2% of cases, the pathology in question is combined with two or more diseases.
Diseases of the abdominal organs accompany pathological conditions of the female genital area and urinary tract are described in 2.8-63% of cases, the appendix with the organs of the female genital area - in 3.1-3.3%, with the gall bladder.
The problem of surgical correction of concomitant gynecological diseases in women of reproductive and perimenopausal age with metabolic syndrome and cholelithiasis is especially interesting, which is explained by the high prevalence (33 - 57% of cases) of this nosology in obese individuals, the more frequent development of this pathology in women (2 - 6% of cases). times more often than in men) and about 2/3 of the incidence occurs between 40 and 45 years of age.
4.Bases for emergency medical care
Calling an ambulance should literally be a reflex, without hesitation, thought or delay, if there is pain in the abdominal cavity:
- does not subside or increases within 1-2 hours;
- accompanied by vomiting (especially streaked with blood) or bloody diarrhea;
- develops against the background of an unusual (dark tar) color of stool in recent days;
- occurs in a pregnant woman;
- so strong that the patient loses consciousness or cannot move;
- associated with severe abdominal contusion.
In all other cases, trying to endure pain in the abdominal cavity (in the hope that it will go away “as usual” in a couple of hours or days) is no less dangerous. Visiting a gastroenterologist has long been no longer a problem even in remote regions (not to mention large cities), and in this case it is much better to play it safe than to risk your life.
Arrangement of the surgical team and choice of surgical approach
The placement of the surgical team when correcting concomitant diseases using laparoscopic access depends on a number of conditions (the principle of asepsis, ablastics, anesthesiological preference for the order of changing body position, determination of the underlying disease and concomitant pathology, etc.) and can change several times during the operation. As a rule, operations are first performed on the upper floor of the abdominal cavity, then in the pelvic area.
When performing the first stage of surgery on the organs of the upper floor of the abdominal cavity, the patient’s position on the operating table is on the back, with the hips apart and the head end raised by 30°. In our opinion, it is the most convenient, since the surgeon’s eyes, hands, surgical area and monitor are on the same line. All endoscopic equipment and the monitor are located to the right of the patient, on a stand, at the head end of the operating table so that the monitor and control panels of all devices are in the surgeon’s field of view. In order to facilitate the work of assistants and perform the second stage of the operation on the lower floor of the abdominal cavity, it is advisable to install an additional monitor to the left of the patient, at the foot end of the operating table.
Performing surgical intervention on the pelvic organs requires changing the position of the patient on the operating table - transferring from the Fowler position to the Trendelenburg position, moving the operating team.
Clinical picture of nonspecific peritonitis
Chronic nonspecific peritonitis has a blurred clinical picture. The smooth development of the pathology is explained by the absence of typical symptoms: acute abdominal pain, nausea and vomiting. In the initial stages, the patient’s body compensatoryly copes with the effects of toxins released by the pathogen. Severe intoxication can lead to the development of asthenic syndrome. This specific disease has the following symptoms:
- Significant reduction in body weight;
- Increase in body temperature to thirty-eight degrees;
- General weakness of the body;
- Increased fatigue;
- Drowsiness;
- Episodic pain syndrome;
- Increased sweating;
- Shortness of breath when performing physical exercises;
- Abnormal stool.
The main causes of chronic nonspecific peritonitis are tubercle bacilli and pneumococci.
Sequence of stages and method of completing laparoscopic surgery
The order of performing the stages of the operation, based on the principles of asepsis, was determined by the degree of infection of the organ. Our experience shows that it is better to begin intervention for combined pathology from cleaner stages, so we performed correction of other pathology in case of hiatal hernia after performing fundoplication, and cholecystectomy always preceded surgery on the pelvic organs.
Extraction of macropreparations can be carried out through an extended umbilical access, after preliminary immersion in a plastic container. After supravaginal amputation of the uterus, splenectomy, the uterus and spleen are removed by morcellation, which does not require expansion of the umbilical puncture for any size of the organ. The 20 mm diameter of the instrument allows you to remove the gallbladder, cyst or fragments of the resected ovary through it. When hysterectomy is combined with any other surgical intervention, the drugs are removed through the vagina by sequentially capturing them with a 10-mm rigid clamp inserted through a vaginal obturator, ensuring the tightness of the abdominal cavity.
Useful links to various sections of the site on surgical treatment of combined diseases:
preparation for surgery for combined diseases ... pain relief during surgery for combined diseases ... simultaneous (simultaneous) operations for combined diseases ... clinical sites ... reviews of operated patients with combined diseases ... reviews of other medical specialists ... scientific publications on combined diseases
1. Abdominal pain: general information and principles of response
There are so many vital organs in the abdominal cavity that any problems and functional problems, any painful, uncomfortable or even simply unusual sensations in this area should cause alarm.
Literally hundreds of diseases, anomalies, pathological conditions and phenomena can be hidden behind the words “stomach ache,” which each of us utters more than once throughout our lives. This topic is so vast that only a multi-volume textbook on gastroenterology could cover it sufficiently fully. And yet, there are a number of points and principles of response that every adult should know, even without being a doctor; Neglect of abdominal symptoms, self-medication, procrastination or incorrect behavior are in some cases deadly.
A must read! Help with treatment and hospitalization!