Aliens somehow flew to Earth. We looked: glaciers are melting, ozone holes are growing, pandas are not reproducing. We began to think about why this was all happening. We went down to the Biryulyovo district of Moscow. They took a hundred people, stripped them, groped them, interrogated them. They concluded: the ozone holes are due to brunettes (there were a lot of them), pandas do not reproduce because of men - more than half of them were on the flying saucer. Well, global warming is because of the ruble: all the residents of Biryulyovo ended up with this currency in their pockets. The aliens flew to their home and, based on the results of the research, printed ten Ph.D. theses with their green tentacles.
This is how “dysbacteriosis analysis” is carried out. Let's talk about this diagnosis with GMS Clinic gastroenterologist Alexey Golovenko.
What's wrong with this study? Doctors often prescribe it!
- Let's make a reservation: it is prescribed by doctors only in the countries of the former USSR. Outside these states, simple stool culture to detect microflora imbalance is not performed. You will not find any indication of the need for this testing in the WGO guidelines for irritable bowel syndrome, or the ACG (American College of Gastroenterology) guidelines for acute diarrhea, or the AAFP (American Association of Family Physicians) standard for monitoring newborns with colic. Well, of course, there is no diagnosis of “dysbacteriosis” either in the International Classification of Diseases or in at least one (!) non-Russian-language textbook.
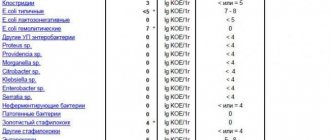
- Our gastrointestinal tract is home to at least 1000 (thousands!) species of bacteria, and the number of all identified species is 2172. When performing a “stool test for dysbacteriosis,” we place stool in a nutrient medium and wait for the growth (the appearance of colonies) of approximately 20 species of bacteria, which we have chosen only because they are able to grow in this nutrient medium. Most of the intestinal inhabitants are not cultivated, that is, we cannot see their colonies in a Petri dish with our own eyes. In other words, when drawing conclusions about the state of microflora based on the reproduction of 20 species, we ignore the vast majority of bacteria.
- The normal amount of bacteria in the stool, which we see in the dysbacteriosis test form, was determined in an unknown way. There is an entire industry standard for treating patients with dysbiosis. There is not a single phrase in it about why we should consider the content of any enterococci from 10^5 to 10^8 per gram of stool to be normal. The standard is full of references to literature, but, suspiciously, there is not a single foreign publication among them. Well, the articles and textbooks themselves do not describe how exactly the microflora of healthy and sick people was compared, that is, how exactly the conclusion was made about the normal content of a particular bacterium.
- The bacteria found in stool (which forms in the colon) is not the same bacteria found in the mouth or small intestine. In addition, the bacteria in the stool (that is, in the lumen of the intestine) are not the bacteria that live in the mucus that protects the intestinal wall. In general, an insane amount of foreign bacteria, fungi and viruses “fly” through our digestive tract. Fortunately, most of them cannot get close to the intestinal wall: the parietal microflora that lives there competes with the “aliens.” We call this phenomenon colonization resistance, and it is to it that we owe the fact that the very first opportunistic bacteria swallowed with a glass of Moscow water does not cause diarrhea in us.
- The composition and ratio of intestinal bacteria is different for each person. By studying (not by stool culture, of course, but by the most complex genetic methods) the composition of bacteria in the stool, you can, for example, guess whether a sample belongs to a resident of New York or the Amazon coast. Well, or in which region of a particular country (for example, Denmark). lives the person who sent his feces for analysis. In general, the true composition of the intestinal microflora is our “fingerprints,” and it is ridiculous to assume some kind of general norm, much less judge the “normality” of the flora based on only 20 species out of 1000.
- Whether bacteria will multiply on a nutrient medium depends not only on what bacteria live in the stool, but also on how the stool was collected (from the toilet, from sterile paper), how it was stored (in the refrigerator, near a radiator, near a window ), how quickly they were delivered to the laboratory. How many people who were recommended to test for dysbacteriosis read these instructions, according to which the stool needs to be collected in a sterile container, placed in the refrigerator and carried to the laboratory not by hand, but in a thermos with an ice cube? However, even when performing these actions, a normal doctor cannot interpret the result of the test for dysbacteriosis. Which means he shouldn’t even try to do it.
Colonies of bacteria appeared in the nutrient medium. Fortunately for us, the truly dangerous Salmonella grows in a nutrient medium. Most intestinal bacteria, alas, do not.
References
- Quigley, E. Gut bacteria in health and disease. Gastroenterol Hepatol., 2013. - Vol. 9(9). — P. 560-569.
- Fröhlich, E., Farzi, A., Mayerhofer, R. et al. Cognitive impairment by antibiotic-induced gut dysbiosis: Analysis of gut microbiota-brain communication. Brain Behav Immun., 2016. - Vol. 56. - P. 140-155.
- Tomasello, G., Mazzola, M., Leone, A. et al. Nutrition, oxidative stress and intestinal dysbiosis: Influence of diet on gut microbiota in inflammatory bowel diseases. Biomed Pap Med FacUniv Palacky Olomouc Czech Repub., 2016. - Vol. 160(4). — P. 461-466.
So, there is no such thing as “dysbacteriosis”?
Of course have. For example, pseudomembranous colitis - severe inflammation of the colon after an antibiotic - is a real dysbiosis: competitors have died, and therefore Clostridium difficile multiplies. Just to treat this, there is absolutely no need to state the obvious - the composition of bacteria in the intestine has changed. It is enough to confirm the infection (identify C. difficile toxins) and prescribe treatment.
Intestinal microflora, without a doubt, affects all processes in our body. By transplanting stool from an obese mouse to a mouse of normal weight, we induce obesity in the latter. The composition of gut bacteria is fundamentally different between people with anxiety and depression. Well, adding the probiotic Bacteroides fragilis to mice that have been artificially induced to have autism improves their social skills. Read the popular book “Look What's Inside You” by the famous microbiologist Rob Knight: our knowledge about microflora is colossal, but we are just beginning to apply it in practice (that is, to treat diseases).
The composition of bacteria can and should be studied. This is the subject of an ambitious international study, the Human Microbiome Project, with a budget of $115 million. Naturally, no “stool cultures” are used. Metagenomics methods are used to analyze the microbial jungle of the gut. They make it possible to describe how many unique DNA sequences are present in a particular person, which groups of bacteria predominate and which are absent. By the way, when such technologies (for example, 16S rRNA sequencing) appeared, it turned out that 75% of the species detected during genetic analysis of the same feces are not known to science at all.
How does the baby's microflora change after birth?
The fetus in the womb is in sterile conditions. The intestines produce meconium (primary stool), which is passed in the first days of life. Already moving along the birth canal, the baby encounters the microflora of the mother’s body for the first time.
Normally, bifidobacteria, lactobacilli, and E. coli are present here. During breastfeeding, the baby acquires other microorganisms, and the intestines are colonized with their own microflora.
Ideal calculations show that a breast-fed baby should have almost 99% lactobacilli and bifidobacteria in its intestinal microflora. The rest is provided by opportunistic microorganisms.
Stop. So there is no point in doing stool culture at all?
I did not say that. We always perform a stool culture if we want to detect the growth of truly harmful bacteria. For example, in a person with bloody diarrhea, we look for Salmonella or Shigella, Campylobacter, or a special type of E. coli. Here, stool culture is vital, because this way we can prescribe antibiotic treatment to kill a specific pathogen.
A competent physician performs a diagnostic test only when the result may change treatment. If the same medicine or diet is prescribed for both a “deficiency” of lactobacilli and an “excess” of E. coli, the analysis is a waste of money.
A full study of one’s own microflora can already be done on a commercial basis in the USA and Europe. The “pleasure” costs about 100 euros, and as a result of a genetic analysis of the microflora you will receive a conclusion (for example, this one) about the bacteria predominant in your digestive tract. The problem is that these results cannot be applied in practice. Because:
We do not yet have a way to selectively change the composition of intestinal bacteria.
Suppose we have clearly established that a person has a deficiency of a specific microorganism (for example, lactobacilli). We can:
- Give a probiotic (that is, a specific live bacterium) and hope that it will remain living in the intestines.
- Give a prebiotic (that is, “food” for the bacteria) and hope that this will enhance the growth of the bacteria we need.
- Give an antibiotic (poison for the bacterium) and hope that it is the overly multiplied bacterium that dies.
- To transplant someone else's microflora into a person - to perform a fecal microbiota transplant (introduce diluted stool from a healthy person into a sick person).
Obviously, only the administration of a probiotic can be considered a selective action. The maximum dose of the best commercial probiotic is 10 billion viable bacteria per dose of the drug. The intestines are home to about 100 trillion bacteria. That is, for every bacteria “from the pharmacy” there are 10 thousand bacteria already “living” in the intestine. It is unlikely that this insignificant number of bacteria will be able to overcome colonization resistance and “populate” the intestine. In addition, the mechanism of action of probiotics (when they work) may generally be associated not with the bacteria themselves: in transgenic mice predisposed to intestinal inflammation, this very inflammation was stopped by using not a “live” probiotic, but in general DNA and some proteins isolated from a drug “killed” by temperature.
Well, and most importantly: theory and laboratory research are one thing, clinical trials (that is, studying the effect of drugs in people) are another matter. Let’s look at three typical situations for Russia when a person is asked to take a “stool test for dysbacteriosis”:
Colic in a newborn
The mother complains that the child cries a lot. By the way, any child in the first three months of life screams from 117 to 133 minutes per day (meta-analysis). The presence or absence of colic (unreasonable crying for more than 3 hours a day at least 3 days a week), in general, does not affect the risk of child developmental delay. In one study, simply talking to parents about colic "safety" reduced crying time from 2.6 to 0.8 hours per day. Children are empaths.
More often than not this is not the case. A stool test is performed for dysbacteriosis, and naturally (the norm is taken from the “ceiling”), “deviations” are found. A probiotic is prescribed. And it often helps: of course, because the frequency of colic inexorably decreases with the age of the child. However, we are not sure that probiotics are generally effective for colic. Numerous meta-analyses examining the treatment and prevention of this condition have failed to unequivocally confirm the effectiveness of probiotics. The probiotic Lactobacillus reuteri may have some beneficial effects. But in order to prescribe this drug, we do not need a stool test for “dysbacteriosis”.
Atopic dermatitis in a child
Everyone is sure that skin problems are caused by the “stomach”. If this were so, atopic dermatitis would probably be perfectly treated with probiotics. But this approach is not very effective. The latest meta-analysis shows that the use of probiotics (mainly Lactobacillus rhamnosus GG) slightly reduces the severity of eczema, but this effect is very symbolic, and additional probiotic therapy does not reduce the frequency of use of topical steroids, which (together with skin hydration) remain the mainstay of treatment for atopic dermatitis. And again: we can prescribe this probiotic regardless of the “results” of the “dysbacteriosis test”.
Bloating and abdominal cramps in an adult
Bloating is most often a symptom of small intestinal bacterial overgrowth (SIBO), which is helped not by a probiotic but by an antibiotic such as rifaximin. This condition is diagnosed using a special breathing test. Often, constant bloating is a consequence of exocrine pancreatic insufficiency: a deficiency of enzymes in the stool can be detected using a test for fecal elastase, and if it decreases, constant enzyme therapy can be prescribed. But most often, the feeling of “bloating” is associated with increased sensitivity of the gut (visceral hypersensitivity), which develops in people with irritable bowel syndrome. As you may have guessed, in order to assess the number of bacteria in the small intestine, the function of the pancreas, or the sensitivity of the intestine to distension, it is pointless to study 20 bacteria in the stool. And the effectiveness of probiotics for irritable bowel syndrome is questionable.
What should parents of an infant remember?
Experienced pediatricians do not advise focusing on daily stool frequency. It is believed that this indicator is very individual and depends on:
- on the functional maturity of the digestive system;
- type of feeding;
- course of pregnancy and childbirth.
The main thing is to monitor the baby’s well-being, activity, regular bowel movements, and the absence of painful signs and pathological impurities in the stool. In the first month of life, defecation occurs after feeding. The frequency is allowed from once a day to 10–12. The main thing is that the child does not strain too much or scream. The consistency of the liquid mass is gradually replaced by the formed one. We should not forget that the liquid is absorbed into the diaper, so lumps remain on the surface.
The color of stool varies from golden yellow to yellow-green or yellow-brown. If breastfeeding is stopped, it becomes darker. The green tint is associated with the release of bilirubin from feces for up to six to nine months. The yellow discharge may turn green when the diaper is left exposed to air.
If the child has never had this symptom, but appeared against the background of other disorders, then a stool analysis should be checked. Both functional disorders (reaction to the introduction of complementary foods, lack of milk in the mother) and diseases of the baby that cause dysbacteriosis are possible.
When kissing, parents “share” their germs with their baby
The baby's stool may contain mucus and undigested white lumps. If the baby is feeling well, this indicates intolerance to complementary foods and a violation of the diet by the nursing mother. What inclusions are always alarming are: the presence of blood or pus. The symptom is considered dangerous. Parents should react appropriately and consult a doctor immediately.
PCR studies
Examination of feces using the PCR (polymerase chain reaction) method guarantees reliable results. It is used to detect cells of certain pathogenic microbes and identify their varieties. Recommended if you suspect the presence of parasites in the body. It could be Helicobacter pylori, Giardia, Ascaris.
Preparation for the analysis does not have any specific features (following a diet, avoiding medications). It is recommended to collect material from several points.
An important advantage of such a study is the rapid result. Within 24 hours, the patient receives an answer about the presence or absence of pathogenic microflora.
Bacteriology
Stool culture is recommended if there is a suspicion of the presence of certain groups of bacteria and helminths in the body. The procedure has no restrictions. It is performed regardless of age and health status.
There are 2 options for taking the test: self-emptying your bowels and collecting material from a health care worker. In the second case, the specialist uses tampons and loops.
The patient lies on his side on the couch and spreads his buttocks. At a depth of approximately 10 cm, the healthcare worker inserts a loop into the anus, through which material is collected from the intestinal walls.