Erosive gastroduodenitis is an inflammatory disease that is characterized by damage to the epithelial layer of the stomach and duodenum and the formation of erosions (defects of the mucous layer, which, unlike ulcers, do not affect the submucosa and muscular membranes). Symptoms of the disease may include pain in the epigastric zone, heartburn, vomiting with the presence of dark blood clots and black stools. To diagnose erosive gastroduodenitis, esophagogastroduodenoscopy with biopsy and determination of the presence of Helicobacter pylori infection is used. Treatment is aimed at reducing the acidity of gastric juice, eradicating Helicobacter pylori and protecting the mucous membrane.
General information
Inflammatory and degenerative diseases of the stomach and, in particular, the gastroduodenal zone are widespread among people of all ages.
Particularly high rates of increase in diseases of the gastroduodenal zone are observed in children and adolescents. At the same time, children and adolescents living in urban areas suffer from these diseases much more often than children from rural areas. But first, let's define what gastroduodenitis is? Gastroduodenitis is a common combined inflammatory disease of the mucous membrane of the stomach and duodenum, characterized by structural (diffuse/focal) dys- and atrophic restructuring of the mucous membrane and accompanied by motor-evacuation disorders and secretory disorders.
What kind of disease is this and can it be considered as a separate nosological unit or as a combination of chronic gastritis and chronic duodenitis? On the one hand, both diseases are different diseases, at first glance, with different pathogenetic mechanisms. However, on the other hand, these differences are not so significant and both diseases have much in common, which contributes to their combined development and the relative rarity of isolated nosological forms, especially in childhood.
In fact, these diseases belong to acid-dependent conditions that develop when there is an imbalance between aggressive and protective factors in the mucous membrane of the stomach and duodenum. According to many authors, there is a single pathogenetic process that leads to the development of gastritis in the stomach and duodenitis in the duodenum. In addition, the inflammatory process in the stomach causes/maintains inflammation in the duodenum and vice versa. Accordingly, the domestic school believes that gastroduodenitis should be considered as a single whole, combining two nosological units into a single diagnosis. ICD-10 gastroduodenitis code: K29.9.
Recently, in patients living in environmentally unfavorable conditions and with low-quality nutrition, the clinical picture of CGD often does not correspond to the classical course, which is manifested by the erasure of gastroenterological symptoms (dyspeptic/pain syndrome), mild symptoms of damage to the upper gastrointestinal tract.
Diagnostics
A gastroenterologist determines the range of diagnostic procedures and prescribes treatment. To identify pathology, a complex of instrumental and laboratory methods is used:
- Esophagogastroduodenoscopy. Helps determine the presence of inflammatory changes in the mucous membrane in the stomach or duodenum, the size of erosions and their location. The endoscopist detects swelling and redness of the mucous membrane, its friability and increased vulnerability. In addition, bleeding is often observed at the site of formation of defects in the mucous layer. The criterion for diagnosing erosive gastroduodenitis is the identification of small hemorrhages and multiple erosions, which are usually covered with a gray film. As a rule, the size of epithelial defects is in the range of 0.3-0.5 mm. To clarify the nature of morphological changes, endoscopic biopsy is used.
- Detection of Helicobacter pylori infection. Due to the fact that erosive gastroduodenitis in most cases develops against the background of Helicobacter pylori infection, it is necessary to use special diagnostic methods for identifying this microorganism. Helicobacter pylori can be detected by morphological examination of biopsy samples of the gastric and duodenal mucosa using microscopy. A more accurate method is PCR diagnostics of Helicobacter and a breath test. In addition, they often search for antibodies in the blood and determine Helicobacter in stool using ELISA.
- UAC. All patients with suspected erosive gastroduodenitis must undergo a general blood test. In the presence of frequent and prolonged bleeding from erosive defects, a decrease in the level of red blood cells, hemoglobin and color index can be detected. This indicates anemia due to chronic blood loss.
Pathogenesis
The pathogenesis of gastroduodenitis is based on the complex effect of nutritional, acid-peptic, autoimmune, allergic and hereditary factors, which have, to varying degrees, a damaging effect on the gastric mucosa and 12 p.c. and create favorable conditions for infection of HP, which has a unique mechanism for overcoming protective barriers of the gastric mucosa by producing urease.
In turn, HP triggers autoimmune mechanisms of gastroduodenitis pathogenesis (inflammation → atrophy → dysplasia). Along with this, activation of T-lymphocytes , an increase in the synthesis of antibodies, the production of γ-interferon, heat shock proteins, cytokines , etc. As a consequence, a violation of secretory acid formation, damage to the epithelium and disorders of its regeneration and mucus production, microcirculatory disorders. The figure below shows a diagram of the pathogenesis of gastroduodenitis.
Causes of pathology
Gastroduodenitis develops for the same reasons as gastritis, since these two anatomical structures are very close.
There is currently no special systematization of gastroduodenitis, therefore, to establish the causes, a classification of chronic gastritis is used, based on its types:
- Type A - occurs as a result of autoimmune disorders in the body, occurring with a tendency to atrophy, primarily of the mucous membranes of the stomach, and subsequently the duodenum. This type is also characterized by a decrease in hemoglobin.
- Type B - inflammation of the stomach develops as a result of infection. In most cases, the causative agent is H. pylori (about 70% of cases), and much less frequently, which is typical for children, enterovirus and Epstein-Barr virus. As a result of gastric metaplasia (“relocation”) of the epithelium, inflammation of the duodenum occurs.
- Type C – which is also called chemical or reactive. The causes of the development of gastritis and duodenitis in this form are caused by alcohol, medications (antibiotics, NSAIDs, corticosteroids), smoking, poor diet, and stress. These factors cause ulceration of the intestinal and gastric walls.
Classification
There are several classifications of gastroduodenitis depending on the underlying factors. According to the etiological factor, HD is divided into primary and secondary (concomitant). Downstream: acute gastroduodenitis and chronic gastroduodenitis.
According to the endoscopic picture:
- Superficial gastroduodenitis is characterized by moderate inflammation of the gastric/duodenal mucosa with no erosion.
- Erosive gastroduodenitis (characterized by the presence of superficial defects of the mucous membrane).
- Atrophic gastroduodenitis (characterized by thinning and atrophy of the mucous membrane with dysfunction of the glands with a decrease in the production of enzymes necessary for normal digestion of food).
- Hyperplastic - characterized by increased proliferation and metaplasia of the epithelium with the formation of polyps and thick rigid folds.
- Mixed gastroduodenitis is a combination of different types of gastroduodenitis.
According to clinical manifestations, phases of exacerbation, incomplete and complete remission are distinguished.
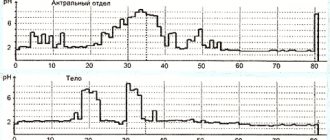
According to the nature of the secretory and acid-forming function of the stomach: gastroduodenitis with preserved, increased and decreased function.
By infection ( HP-associated and HP-non-associated ).
Causes
Gastroduodenitis is characterized by polyetiological genesis. It is the combined effect of exo/endogenous damaging factors, as well as disorders of regenerative processes, that cause damage to the mucous membrane. Of particular importance among them are:
- Nutritional factor (improper diet, overeating, unbalanced diet, fasting, consumption of foods that chemically/mechanically irritate the mucous membrane of the gastroduodenal zone, improper cooking of foods, abuse of herbs and spices, dry food, consumption of too hot or rough food).
- Alcohol abuse, smoking.
- Long-term use of certain antibiotics, glucocorticosteroids and NSAIDs ( Diclofenac , Aspirin , Ibuprofen ).
- Genetic predisposition.
- Helicobacter pylori infection.
- Endocrine disorders ( adrenal insufficiency , diabetes mellitus , etc.)
- Psychotraumatic situations, prolonged stress.
- Diseases of other organs of the digestive system (neuro-reflex effect on the gastric mucosa and 12 p.k. from other digestive organs - gall bladder/liver, pancreas, intestines).
- Functional/organic disorders of the gastrointestinal tract ( duodenogastric reflux , constipation / diarrhea , dysbacteriosis , etc.).
- Metabolic disorders.
- Helminthic and parasitic infestations.
- Food allergies.
Causes of gastroduodenitis
The etiological factors for the development of the disease include:
- Heredity
- Unbalanced diet (lack of regular meals, insufficient fluid intake, excess alcohol, rough, hot, spicy foods)
- Intestinal infectious diseases
- H. pylori infection
- Chronic inflammatory process in the oral cavity, pharynx
- Diseases of the hepatobiliary system
- Long-term use of medications (a number of antibacterial drugs, acetylsalicylic acid)
- Chronic stress
- Smoking
Symptoms of gastroduodenitis
Acute gastroduodenitis in adults is most often caused by the direct influence of an etiological factor and usually develops a few hours after eating poor-quality food, overeating, drinking alcohol, coarse fried or spicy foods. The patient complains of nausea, dizziness, and severe weakness.
Complaints of trembling fingers, fever, and palpitations may also appear. The skin becomes cold and pale. Somewhat later, nausea turns into vomiting of food eaten, sometimes with an admixture of mucus and streaks of blood. At the height of the disease, diarrhea often occurs, later giving way to constipation.
Acute gastroduodenitis in adults is usually accompanied by pain that occurs suddenly, initially localized in the upper abdomen, and later in the epigastrium and left hypochondrium.
The pain syndrome is caused primarily by swelling of the mucous membrane of the duodenum, leading to paralysis of the smooth muscles of the small intestine, swelling of the papilla of Vater and difficulty in evacuation of bile and pancreatic juice from the biliary tract. Distension of the inflamed stomach and duodenum by food masses, as well as digestive juices, also plays a certain role in the genesis of pain syndrome.
In acute gastroduodenitis, pain is relieved in the left side/squatting position. In this case, taking antacids does not have an analgesic effect (unlike ulcers). Less commonly observed is heartburn , the occurrence of which is caused by hypersecretion of the gastric mucosa and is not associated with changes in gastric acidity. Diarrhea is also associated with increased production of digestive juices in the inflamed duodenum and concomitant damage to the pancreas.
Other symptoms (headache, weakness, dizziness, palpitations and pain in the heart area, tremor of the fingers) are caused by hormonal/reflex disorders associated with intoxication of the body and the inflammatory process in the stomach and duodenum.
Symptoms of gastroduodenitis in adults during its chronic course are determined mainly by its form. In most patients with chronic gastroduodenitis (ICD-10 code for chronic gastroduodenitis: K29.9) caused by exogenous factors, inflammation and mild changes are determined mainly in the mucous membrane of the antrum of the stomach and duodenum (chronic superficial gastroduodenitis).
A feature of the course of this variant of gastroduodenitis is the increased/preserved function of acid/enzyme formation, as well as discoordination of the motor and secretory functions of the stomach and duodenum. Patients experience headaches, irritability, dyspeptic disorders ( heartburn , sour belching), and sometimes thirst. The appetite is often preserved, and there is a white coating on the tongue. Pain in the abdomen of moderate intensity localized in the epigastrium/pyroduodenal zone. In this case, pain occurs both after eating and on an empty stomach. There is a tendency to constipation.
With the predominance of endogenous and toxic risk factors, and with a longer duration of the disease, the fundus of the stomach is also involved in the process. At the same time, against the background of inflammatory, focal atrophic/subatrophic changes, multiple erosions of the gastric mucosa (chronic erosive gastroduodenitis) appear.
The main signs in adults of this variant of the disease are gastric atony and decreased acid/enzyme production. Patients experience: lethargy, weakness, fatigue, various dyspeptic manifestations - distension and a feeling of heaviness in the epigastrium after eating, belching with air . Pain in the abdomen is low-intensity, occurs more often after eating, there may be flatulence , and there is a tendency to loose stools. Palpation - pain in the upper/middle third of the distance between the navel and the xiphoid process.
In the presence of hereditary morpho-functional changes in the coolant with a high risk of transformation into peptic ulcer disease, it should be considered as a pre-ulcerative condition.
Nosologically, this course of the disease can be defined as gastroduodenitis with continuous acid/enzyme formation and severe inflammatory, erosive and hyperplastic changes in the gastric/duodenal mucosa.
In such patients, hyperplasia of the fundic glands of the gastric mucosa occurs with an increase in the number of main parietal cells. Clinical manifestations are similar to duodenal ulcer. The leading symptom is pain on an empty stomach: before meals and after meals 2-3 hours later. The pain is paroxysmal, stabbing, intense, localized in the left hypochondrium (pyloroduodenal zone), frequent sour belching. For 1/3 – 1/2 of patients, the pain syndrome is seasonal (exacerbation in spring and autumn).
Stool with tendency to harden. On palpation of the abdomen - pain in the pyloroduodenal zone, a positive Mendelian symptom (pain on percussion). The symptoms of chronic gastroduodenitis, regardless of its form, are mild beyond the acute stage.
Gastroduodenitis. Peptic ulcer of the stomach and duodenum
Causes
For a long time, peptic ulcer disease was associated mainly with nutritional (food) factors. However, the twentieth century radically expanded and deepened the understanding of etiopathogenesis. Unhealthy diet (in the broadest sense), as well as drunkenness, smoking, overwork, lack of sleep, unfavorable environmental conditions - are still considered today among the most significant risk factors, but the causes of peptic ulcer disease are more complex and varied; This disease belongs to the group of polyetiological (multi-cause) diseases. To date, the role of such factors as:
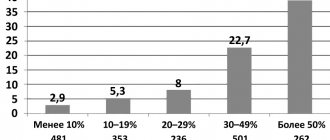
- hereditary predisposition;
- neuropsychic stress;
- activity of the bacterium Helicobacter Pylory;
- <systemic endocrine-metabolic disorders./li>
The influence of the hereditary factor is beyond doubt; its significance is estimated, depending on the methodological approach to the study, in the statistical range from 10 to 50 percent. Blood type, Rh factor and other congenital characteristics also appear to have a certain significance.
Further, it is no coincidence that peptic ulcer disease is in second place, after arterial hypertension, in the so-called. Big Seven psychosomatic diseases. The relationship between physiological and neuropsychic processes (as well as their disorders) is very close, has long been proven and remains the object of intensive research, revealing ever new trends and patterns. Various types of stress, momentary and chronic; mental and emotional overload; neurotic disorders (especially anxiety-phobic and neurasthenic) - all this inevitably affects the general condition of the body and, in particular, the functional status of the gastrointestinal tract.
With regard to the pathogenic microorganism Helicobacter Pylory, an uncertain and even paradoxical situation has developed in gastroenterological science for a long time. A priori, it was considered impossible for the existence of bacterial cultures capable of active life in hydrochloric acid (its sufficiently high concentration in gastric juice is necessary for the normal course of enzymatic digestive processes). At the same time, hypotheses, supported by many facts and observations, have been repeatedly expressed that such a microorganism not only exists, but may be the direct cause of peptic ulcer disease. Moreover, Helicobacter Pylory (literally “gatekeeper spiral bacterium”) was discovered several times by various researchers, but these discoveries either did not receive due attention or were not sufficiently conclusive to overcome the established skeptical prejudice towards the “bacterial” hypothesis. Only by the mid-1980s were all questions finally resolved; ideas about the etiopathogenesis of gastroduodenitis and peptic ulcer disease have once again changed dramatically. Today it is known that Helicobacter Pylory is present in the body in 75% of patients with gastric ulcer and in 95% of patients with duodenal ulcer.
The interdependence of all structural elements of the gastrointestinal tract, endocrine system, hemodynamic and biochemical factors is also undeniable. Any imbalance in this area, the presence of chronic diseases and foci of infection in any system of the body, especially in combination with an unhealthy lifestyle (see above), create the preconditions for the activation of pathogenic microflora, the development of gastritis and peptic ulcers with all its life-threatening consequences and complications.
It should be emphasized that gastroduodenitis and peptic ulcer disease are considered by us in one article only for reasons of their certain symptomatic, etiological and pathomorphological similarity, as well as a single localization. In fact, a direct cause-and-effect relationship (or a sequential change of phases, stages and conditions) between gastritis and peptic ulcer disease is not always traceable. On the contrary, gastroduodenitis in many cases is secondary in nature and is a consequence of a long-standing peptic ulcer, or complicates the course of other chronic gastrointestinal diseases, or acts as an independent disease without any signs of an ulcer.
Treatment of gastroduodenitis
Treatment of chronic gastroduodenitis should be comprehensive and aimed at eradicating HP, normalizing acid/enzyme formation and motor function, increasing the protective properties of the mucous membrane of the duodenum and stomach, and treating concomitant diseases. Treatment of gastroduodenitis in adults begins with eradication of H. Pylori.
Eradication is carried out using drugs in the form of standard triple therapy, including a proton pump inhibitor (PPI), clarithromycin and amoxicillin . As an alternative, a four-component classical therapy based on a bismuth drug in combination with a PPI, tetracycline and metronidazole .
How to treat chronic gastroduodenitis in the acute stage?
Drug therapy includes several groups of drugs. To suppress gastric secretion of hydrochloric acid (reduce acidity), proton pump inhibitor drugs ( Rabeprazole , Omeprazole , Esomeprazole , etc.) are used.
If the patient, after eradication of H. Pylori and relief of acid-related symptoms, continues to have dyspeptic complaints (early satiety, nausea, bloating, feeling of fullness of the stomach), the drugs of choice are prokinetics - Domperidone ( Motilium , Metoclopramide ).
The drugs effectively block D2-dopamine receptors, which stimulates the motor-evacuatory function of the duodenum. To suppress the secretion of hydrochloric acid, selective M1 anticholinergics ( Pirenzepine ) can be prescribed in combination with prokinetics. Ranitidine , Roxatidine , Cimetidine , Famotidine , etc.) can be prescribed in combination with prokinetics
A good effect is observed when prescribing antacid drugs ( Phosphalugel , Gastrogel , Almagel , Gelusil , etc.), which react directly in the stomach with neutralization with hydrochloric acid. They have an enveloping, adsorbing, neutralizing and cytoprotective effect, but the effect develops quite slowly.
To increase protective coolants, antipeptic drugs with different mechanisms of action are prescribed - tablets for the treatment of gastroduodenitis ( De-nol , Solcoseryl , Biogastron , Akgovegin , Carbenoxolone ), as well as rosehip/sea buckthorn oil.
Also, to improve the regeneration of coolant and duodenum, the administration of Cyanocobalamin (Vit. B12) is indicated. For severe pain, antispasmodics are indicated; to relieve emotional tension, sedatives (infusion of valerian root) are prescribed. For gastroduodenitis against the background of diseases of the biliary system, enzyme and choleretic drugs are prescribed. Treatment of concomitant diseases of the gastrointestinal tract organs is carried out in accordance with the nature of the pathology.
Gastroduodenitis in children
The specificity of the course of CGD in children is due to the presence of critical periods during which the formation of the gastrointestinal tract occurs. These periods are characterized by uneven growth of the body, intensity of morphofunctional changes and metabolism , immaturity of enzyme systems and restructuring of the neuroendocrine system.
Chronic gastroduodenitis in children is characterized by a predominance of pain with a predominant localization in the epigastric/peri-umbilical areas of an aching nature and the presence of severe dyspeptic syndrome in the form of belching, lack of appetite, and nausea. In children 5–9 years old, peri-umbilical localization of abdominalgia and loose stools are more common, and in children 10–15 years old, epigastric localization of abdominalgia and heartburn . The most common form of chronic gastroduodenitis among children is superficial negative Helicobacter pylori gastroduodenitis against the background of increased acid-forming function.
Popular questions about gastroduodenitis
What medications should I take for gastroduodenitis?
Treatment is prescribed strictly by a doctor. The treatment regimen is developed taking into account the etiology, clinical manifestations of the disease, results of laboratory and instrumental research methods. It may include antibacterial and antisecretory agents, antacids, antispasmodics, enzymes, sedatives and other drugs.
How does the stomach hurt with gastroduodenitis?
When the acute form manifests itself, there is severe cramping pain in the upper abdomen, mainly in the epigastric region.
Chronic gastroduodenitis is accompanied by pain of moderate intensity. The aching pain is localized in the epigastric region and is associated with food intake.
What should you not eat if you have gastroduodenitis?
When a diagnosis is made, the patient should avoid eating fried, salted, smoked foods, canned food, spicy spices, alcoholic and carbonated soft drinks, and spices. Fruit and vegetable juices, teas, coffee, cabbage, cucumbers, onions and green onions are not recommended.
Diet for gastroduodenitis
Diet for gastroduodenitis
- Efficacy: therapeutic effect for 14-21 days
- Time frame: 21 days
- Cost of products: 1280 - 1500 rubles per week
In the acute stage for 5-7 days - Diet No. 1A , the menu includes: fresh cottage cheese, milk (if tolerated), jelly, mucous and pureed soups from cereals and milk, fish soufflé, salt restriction.
Next, Diet No. 1B for 10-14 days: nutrition is expanded by including crackers, cereal soups with milk, pureed dietary meats, fish, and cereals in the diet. Salt in moderation. In the future, Diet No. 1 with strict adherence to the principle of chemical/mechanical sparing. For CGD with secretory insufficiency, Diet No. 2 . For CGD with high acidity, the diet should include foods with high buffering properties (boiled beef/veal, oatmeal, milk).
Small meals, 6 times a day, it is recommended to include dietary fiber (wheat bran) in the diet. The duration of a gentle diet is determined by the patient’s condition. With improvement, dietary nutrition is expanded. At the remission stage, alternating Diets No. 5 and No. 15 . In this case, poorly tolerated foods and roughage should be completely excluded from the diet.
Prevention
There are primary and secondary prevention. The primary one comes down to measures that contribute to the normalization of the function of the gastrointestinal tract and the body as a whole: giving up bad habits, working and resting hours, rational nutrition in accordance with age, gender, energy costs, sanitation of the oral cavity, and undergoing periodic preventive examinations.
Secondary prevention comes down to the correction of risk factors, anti-relapse therapy and includes dietary nutrition corresponding to the clinical-endoscopic stage of the inflammatory-dystrophic process in the coolant/duodenum with sufficient sleep, increased physical activity, physical therapy, and hardening.
List of sources
- Ivashkin V.T., Ivashkina N.Yu., Baranskaya E.K. and others. Rational pharmacotherapy of diseases of the digestive system: a guide. / Ed. Ivashkina V. T. - M.: "Literra" - 2011. - 848 p.
- Balabolkin I.I. Helicobacter pylori infection in chronic gastroduodenitis and atopic dermatitis in children / I.I. Balabolkin, A. S. Potapov, JI.B. Kudryavtseva // Current problems of abdominal pathology in children. M., 2001. - P. 83.
- Volkov A.I. Chronic gastroduodenitis and peptic ulcer in children / A.I. Volkov // Rus. honey. magazine 1999. - T.7, No. 4. - P. 179-186.
- Shcherbakov P. L. Epidemiology of helicobacteriosis. Gastroenterology of childhood. Ed. S. V. Belmer and A. I. Khavkin. M., 2003.
- Gastroenterology national guide / Ed. Ivashkina V. T., Lapina T. L. - M.: "GEOTAR-Media" - 2012. - 480 p.