The inflammatory process that covers the mucous membrane of the esophagus with the formation of erosions and ulcers on it is called erosive esophagitis.
This disease occurs equally often in men and women. According to the international classification of diseases ICD-10, the pathology is coded K 22.1, and when GERD is added - K 22.0. The erosive form requires immediate treatment, as it can cause serious complications, including malignant neoplasms. Therefore, if heartburn and burning behind the sternum appear, you need to contact a gastroenterologist to receive special treatment.
Erosive esophagitis: what is it?
We found out what the ICD 10 code for , we follow further. Esophagitis causes inflammation of the mucous membrane of the esophagus and develops in acute and chronic types. An acute course occurs when:
- fungal infections;
- alkalis;
- acids;
- salts of heavy metals;
- hot food or steam;
- alcohol.
Also, unpleasant sensations in the form of heartburn are caused by overeating and physical work immediately after eating. In addition, esophagitis can be caused by reflux, that is, the reflux of stomach contents back into the esophagus. The hydrochloric acid contained in gastric secretions irritates the epithelium of the esophageal tube. When affected by these factors, the mucous membrane of the esophagus becomes inflamed, red and swollen. So what are the typical symptoms? Erosive esophagitis causes the patient to:
- heartburn;
- burning in the chest;
- sore throat.
This condition is treated by using a gentle diet, and if the disease is caused by an infectious factor, then antibiotic therapy is added.
If treatment is not started in time, erosions will appear on the mucous membrane in addition to hyperemia, hence the name erosive esophagitis. It develops during the chronic course of the disease.
Necrotizing esophagitis
This is a form of acute disease, which does not occur very often and occurs in people with reduced immunity due to infectious diseases (scarlet fever, sepsis, measles, mycosis). The disease is characterized by severe inflammation of the esophageal mucosa, forming necrotic (dead) areas, which, when rejected, form deep ulcerative lesions . During the healing of ulcers, the epithelium of the esophagus becomes covered with purulent or bloody exudate.
Against the background of symptoms corresponding to the underlying disease, the following are observed:
- chest pain;
- vomiting mixed with necrotic tissue;
- dysphagia (impaired swallowing).
This form of the disease often causes complications in the form of bleeding, acute purulent inflammation of the mediastinum, and substernal abscess.
Treatment of necrotizing esophagitis takes a long time and requires the patient to be patient and strictly follow all the doctor’s instructions. After the ulcers heal, scarring forms in the esophagus, which brings discomfort to the patient.
Peptic esophagitis
Treatment of reflux esophagitis includes conservative and surgical measures.
- Conservative treatment
Drug treatment of peptic esophagitis should begin with the elimination of the underlying disease that caused it, if it is, in principle, amenable to therapeutic correction (peptic ulcer, chronic cholecystitis and pancreatitis, etc.). Severe gastroesophageal reflux within hiatal hernias appears to require surgical intervention.
Formulating this idea somewhat differently, it can be argued that the elimination of peptic lesions of the esophageal mucosa is hardly possible without eliminating or at least significantly leveling the intensity of gastroesophageal reflux. It is this goal that is met by recommending patients a certain lifestyle and an appropriate diet.
Based on the conditions for the occurrence of esophagogastric reflux, situations that are accompanied by a significant increase in intra-abdominal pressure or facilitate the flow of intragastric contents into the esophagus should be avoided. Overeating, drinking large amounts of carbonated drinks, lifting weights of more than 8-10 kg with both hands, as well as all types of work that involve bending the body forward are prohibited. It is necessary to eliminate all physical exercises that are accompanied by overstrain of the abdominal muscles. Wearing corsets, bandages and tight belts is not recommended. You should sleep on a bed with the head end raised.
Particular importance is attached to the regimen and nature of nutrition, which should be fractional (at least 4-6 times a day). Afternoon naps are strictly prohibited. At least 3-4 hours must pass from the last meal before going to bed. After eating, a light walk or staying in an upright position is recommended, which facilitates faster evacuation of food from the stomach.
The diet should be mechanically, chemically and thermally gentle. For the period of exacerbation of the process, the “esophageal table” is prescribed, table No. 1 and 1a according to Pevzner, in the presence of concomitant chronic cholecystitis or chronic pancreatitis - table No. 5. It is advisable to exclude from the diet those foods that help reduce the tone of the lower esophageal sphincter: coffee, animals fats, chocolate, citrus fruits, tomatoes, alcohol, as well as dishes containing them. Vegetable fats taken 1 hour to 11 days before meals help reduce acidic gastric secretion, and therefore are not contraindicated in patients with peptic esophagitis.
Drug treatment of this disease includes the use of astringents, enveloping agents, antacids, and motor regulators. functions of the gastrointestinal tract, cholinergic drugs, as well as drugs that reduce the acid-producing function of the stomach. Treatment should be comprehensive, i.e., affect various aspects of the pathogenesis of reflux esophagitis. Monotherapy usually has a very minor effect.
Astringents and enveloping agents (aluminum hydroxide, bismuth subnitrate, dermatol, silver nitrate, collargol, tannin, white clay, Shostakovsky balm, etc.) have an anti-inflammatory and cytoprotective effect. Entering into a chemical reaction with the protein components of the esophageal mucosa, they form poorly soluble compounds, consisting mainly of albumin and lining the inner surface of the esophagus in the form of a thin film. This protein film protects the mucosa from the action of various types of irritants, including proteolytic enzymes of gastric juice. In addition, astringents eliminate the looseness of the esophageal wall caused by the inflammatory process, reduce swelling, hyperemia and pathological impulses from the affected area. Possessing antibacterial properties, drugs in this group suppress the vital activity of microorganisms.
It is advisable to take solutions of astringents and enveloping agents in a lying position with the head of the head low and in small sips for 10 minutes to ensure the longest possible contact with the esophageal mucosa.
The domestic combination drugs Vikalin and Vikair have proven themselves well. The latter is similar in composition to the Roter tablets produced abroad. Vikalin and vikair are prescribed in crushed form, 1-2 tablets 4 times a day (last time at night) along with 1/3 glass of warm water. The resulting suspension is taken according to general rules.
Bismuth and bismuth-containing drugs are usually well tolerated by patients. Their side effects include dark green or black stool, which can sometimes mimic melena. Bismuth is radiopaque and can therefore significantly complicate X-ray examinations of the abdominal organs. This can be avoided by prior withdrawal of the drug.
A solution of silver nitrate, especially if it is introduced into the esophagus through a probe (and this is used to lengthen the time of contact of the drug with the mucosa), can itself cause a retrosternal burning sensation and nausea. When used for several months, silver nitrate turns the patient's skin a characteristic gray color (argyrosis).
The purpose of prescribing antacid therapy is to reduce the proteolytic aggression of gastric juice. By increasing intragastric pH, these drugs also eliminate the pathogenic effect of pepsin on the esophageal mucosa. Neutralization of acidic gastric contents leads to this enzyme losing its activity.
The arsenal of modern antacid drugs has reached an impressive size and is constantly being replenished with new highly effective agents. And although the so-called traditional alkalizing medications (burnt magnesia, aluminum hydroxide, magnesium trisilicate, Bourget's mixture, etc.) have largely lost their leading positions, their use in a number of cases is still justified. The advantage of these drugs is that they are well tolerated by most patients and the rapid onset of clinical effect.
The above alkalizing drugs are usually used 5-6 times a day, 40-60 minutes after meals, when heartburn and retrosternal pain most often occur, and also always before going to bed. The dose of antacids should be sufficient to quickly eliminate and prevent the symptoms of reflux. When treating peptic esophagitis with antacids, doctors recommend adhering to the following rule: each attack of pain or heartburn must be stopped immediately, since these symptoms indicate progressive damage to the esophageal mucosa.
In addition to oral administration, another method of using antacids is possible. It makes sense to use liquid antacids for long-term irrigation of the esophageal mucosa through a thin probe, which has a very beneficial effect in severe forms of peptic esophagitis.
Currently, alkalizing agents are produced, as a rule, in the form of complex preparations. These include almagel and the anesthesin-containing almagel A, gastal, phosphalugel, De-Nol, ritacid, geluzil, as well as the anesthetic geluzillac, etc. Their main active ingredients are aluminum hydroxide, magnesium trisilicate, bismuth nitrate. Some of the above complex antacids are available in tablets, others in gel form. With regard to diseases of the esophagus, the latter form of release is the most convenient. However, it is quite acceptable to prescribe tablets (ritacid), which can either be dissolved in a small amount of water immediately before use, or dissolved in the mouth.
The drug Topalcan (Topaal) has proven itself well in the treatment of reflux esophagitis. It contains aluminum hydroxide, magnesium hydroxide, magnesium bicarbonate and alginic acid, which causes the formation of a foamy suspension in the stomach. During any episode of reflux, the drug in the form of foam again enters the esophagus and causes a long-term therapeutic effect. Topalkan is prescribed 1 tablet (1 powder) 30-40 minutes after meals and at night.
With rare exceptions, antacids are well tolerated by most patients. Their side effects are minor. For example, magnesium preparations have a laxative effect, calcium carbonate and aluminum hydroxide have a fixing effect. In addition, aluminum-containing drugs, when used for a long time, can cause hypophosphatemia. After a series of chemical transformations, these drugs form poorly soluble compounds, which include phosphorus, in the human intestine. This can be avoided by prescribing phosphorus-containing agents (for example, phosphalugel, but its alkalizing ability is approximately 2 times less than that of almagel).
The administration of sodium bicarbonate (baking soda) is inappropriate for several reasons. Firstly, when this substance interacts with hydrochloric acid, carbon dioxide is formed, which can itself stimulate gastric secretion. Secondly, long-term use of baking soda leads to the retention of sodium ions in the body, which is strictly contraindicated for people suffering from edema and arterial hypertension.
Massive therapy with calcium carbonate is contraindicated in hypercalcemia, osteochondrosis, and the presence of calcium-containing stones in the kidneys and gall bladder.
Perhaps the most serious complication that develops during treatment with antacids is alkalosis. This latter develops especially often when so-called absorption agents (calcium carbonate and sodium bicarbonate) are used in combination with a dairy diet. Azotemia, renal failure and nephrocalcinosis occur, referred to as Barnett's milk-alkali syndrome. Such patients complain of an aversion to milk and alkalis, general weakness, dizziness, headache, increased excitability, and hyperreflexia. Mild cases of Barnett's syndrome require discontinuation of the medications that caused it and transfer to non-absorbable antacids (Alma-gel, phosphalugel, Gastal, etc.). Severe alkalosis is an indication for the prescription of an isotonic sodium chloride solution to correct hypochloremic azotemia, as well as rehydration.
In extremely rare cases, treatment with non-absorbable antacids may be accompanied by the formation of insoluble conglomerates in the intestine, which can induce intestinal obstruction.
Relief of severe retrosternal pain in peptic esophagitis is facilitated by the administration of so-called local anesthetics, which are used as an addition to therapy with astringent, enveloping and alkalizing drugs. For this purpose, anesthesin is widely used, produced in powders, tablets and mucous mixtures. Anestezin is also included in Almagel. A single dose of anesthesin is 0.3 g 3-4 times a day 10-15 minutes before meals.
The use of drugs from the group of anticholinergic and antispasmodics for the treatment of peptic esophagitis is currently very limited. Atropine and its analogues, although they reduce gastric secretion, also reduce the tone of the lower esophageal sphincter, thereby increasing cardia failure. They are contraindicated in glaucoma and prostate adenoma.
Anticholinergic drugs have been replaced by so-called regulators of the motor function of the gastrointestinal tract, a typical representative of which is metoclopramide (Raglan, Cerucal). According to its mechanism of action, metoclopramide is classified as an antidopaminergic drug. It has virtually no effect on gastric secretion, however, it tones the lower esophageal sphincter and accelerates evacuation from the stomach, i.e., it affects the main links in the pathogenesis of gastroesophageal reflux. Metoclopramide also has a pronounced antiemetic effect, which makes it very valuable in the treatment of some forms of esophagitis caused by persistent vomiting.
The drug is available in ampoules, tablets and suppositories. It is prescribed 10 mg 3-4 times a day (if used four times, the last dose is immediately before bedtime). The most preferred route of administration is oral or rectal. Ensuring that an adequate dose of Cerucal is maintained by injection can be quite difficult, especially if this drug is used for quite a long time.
Metoclopramide is usually well tolerated by patients. In some cases, it can cause oppressive weakness, insomnia, and a feeling of discomfort throughout the body (“neither lie down, nor stand up, nor sit down”). In such situations, it is necessary to reduce its dose or abolish it completely. The drug is contraindicated in persons suffering from extrapyramidal disorders.
A very promising drug from the group of regulators of the motor function of the gastrointestinal tract is domperidone, marketed under the commercial name “Motilium”.
In most patients with peptic esophagitis, it is possible to achieve stable remission through a combination of locally acting drugs (astringents, enveloping agents, antacids) and metoclopramide.
In the absence of positive dynamics from the use of the above drugs, treatment of peptic esophagitis should be supplemented with drugs that reduce the secretory activity of the stomach. One of the most powerful medications with these properties are histamine Hr receptor blockers. These are cimetidine and its analogues (belamet, tagamet, histadil), ranitidine (peptoran, Zantac, Ranisan), famotidine, nizatidine.
For the treatment of reflux esophagitis, cimetidine is used in doses of 800 mg and 1600 mg (400 mg 2 times a day and 400 mg 4 times a day, respectively). The course of treatment averages 12 weeks. After this period, there is a reliable and significant decrease in the frequency and duration of esophagogastric reflux, as well as a leveling of the inflammatory process in the mucous membrane of the esophagus. It is curious that the use of the drug in daily doses of 800 mg and 1600 mg has approximately the same effect on the symptoms of peptic esophagitis. Apparently, it is preferable for such patients to prescribe cimetidine 400 mg 2 times a day, which significantly reduces the number of its side effects.
Reducing the dose of cimetidine after the onset of clinical and morphological remission of peptic esophagitis should be carried out gradually. Otherwise, the so-called withdrawal syndrome develops: a significant and rapid increase in gastric secretion leads to an increase in acid-peptic aggression and, as a consequence, to an exacerbation of the process.
The main side effects of this drug are diarrhea, muscle pain, skin rashes, headache, dizziness, depression, gynecomastia, and impaired kidney and liver function.
The disadvantages of cimetidine are largely absent from ranitidine (Peptoran, Ranisan). This relatively new drug, according to its mechanism of action, also belongs to the group of Hg-histamine blockers, but is much more effective than its predecessor, cimetidine. Ranitidine has low toxicity and is well tolerated by most patients. For the treatment of patients with peptic esophagitis, this drug is used in a daily dose of 300 mg (150 mg 2 times a day or once 300 mg at night, which has approximately the same clinical effect). The use of ranitidine for 6 weeks causes remission of peptic esophagitis in 74.5-81.6% of cases, and a 12-week course of treatment is effective in 93.6-95.9% of patients. No side effects were identified.
Some studies report relatively high effectiveness of ranitidine at a dose of 150 mg 2 times a day in patients with reflux esophagitis due to systemic scleroderma. The course of treatment in this case lasted 20 weeks.
Thus, the experience of using histamine Hr receptor blockers convincingly demonstrates their high effectiveness in eliminating the symptoms of gastroesophageal reflux. However, the specific mechanism of their beneficial effects on gastroesophageal reflux has not yet been established. The fact is that a significant decrease in gastric secretion under the influence of, for example, ranitidine does not correlate with the duration and frequency of gastroesophageal reflux. Moreover, a significant reduction in heartburn and retrosternal pain with the use of this drug is not accompanied by a similar leveling of regurgitation, dysphagia, or the severity of esophagitis according to the results of esophagoscopy with targeted biopsy.
While eliminating, to one degree or another, acid-peptic aggression towards the esophageal mucosa, Hr-histamine blockers have virtually no positive effect on the frequency and duration of gastroesophageal reflux.
For the last few years, bethanechol (duvoid, urecholine), a drug from the group of M-cholinergic drugs, has been used to treat peptic esophagitis. This drug stimulates the tone of the lower esophageal sphincter and thereby reduces the severity of gastroesophageal reflux.
Doctors report the high effectiveness of bethanechol at a dose of 25 mg 4 times a day against the symptoms of reflux esophagitis. The course of treatment lasted 4 weeks, which is much shorter than the duration of drug correction of peptic esophagitis with H2-histamine blockers.
Such optimism, however, was expressed by some clinicians who studied the effect of bethanechol in combination with antacids on the severity of peptic esophagitis in comparison with a group of patients receiving only placebo and antacids. As the results of the study showed, the combination of bethanechol with antacids in its therapeutic effect is only slightly superior to the combination of antacids with placebo (the difference is not statistically significant).
Thus, the question of the advisability of using this drug for the treatment of patients with reflux esophagitis is subject to further study.
In terms of its final effect, a new medicinal substance, cisapride, which is a stimulator of the release of acetylcholine in the intestinal wall, has much in common with bethanechol. Cisapride significantly increases the tone of the lower esophageal sphincter and is very promising for the treatment of peptic esophagitis.
The combined drug sucralfate, which contains sucrose sulfate and aluminum salts, has the ability to protect the mucous membrane of the esophagus from acid-peptic effects. Scientists have demonstrated in experiments on rabbits that the present drug in a dose of 1 g has a mainly local protective effect on the esophageal mucosa, preventing contact between it and active pepsin. Used in liquid or gel form. In this regard, sucralfate is very close to astringents and enveloping agents. Experts used sucralfate in a daily dose of 4 g to treat peptic esophagitis for 12 weeks. After the specified period, 90% of patients showed complete disappearance of histological signs of the disease, which was accompanied by a decrease in the frequency and duration of esophagogastric reflux and restoration of normal motor function of the distal esophagus.
Cases of long-term reflux esophagitis, especially in elderly and senile people, as well as the presence of erosive and ulcerative defects of the esophageal mucosa are an indication for the prescription of reparatives, or agents that stimulate regeneration. Of the medicinal substances in this group, the most active and harmless are pyrimidine derivatives (methyluracil, pentoxyl, potassium orotate), solcoseryl, and allanthone.
Pyrimidine derivatives normalize nucleic acid metabolism in the mucous membrane, enhance regenerative processes, reduce exudation and cellular infiltration, and also increase the phagocytic activity of leukocytes and the production of antibodies.
Methyluracil (methacyl) is used orally after meals, 095 g 4 times a day. It is usually well tolerated by patients. In some cases, allergic skin rashes such as urticaria, headache, and dizziness are possible. Contraindicated in acute and chronic leukemia, lymphogranulomatosis. Pentoxyl is taken orally 0.2-0.3 g 3-4 times a day after meals. The drug has low toxicity; sometimes moderate dyspeptic symptoms are observed. The contraindications are the same as for methyluracil. Potassium orotate is prescribed 0.25-0.3 g 2-3 times a day an hour before meals or 4 hours after it, the method of administration is oral. Side effects of pentoxyl include allergic dermatoses and dyspepsia.
The mechanism of action of solcoseryl is associated with the activation of the enzymes cytochrome oxidase and succinate dehydrogenase, as a result of which the utilization of oxygen by tissues improves, tissue metabolism is normalized, and epithelization is accelerated. The drug is used intramuscularly, 2 ml 2 times a day for 2 weeks. After the specified period, you should switch to oral administration of 100 mg 3 times a day. The course of treatment is 3-4 weeks. As a rule, there are no side effects.
Allanton is obtained from the roots of elecampane; it has anti-inflammatory, capillary-strengthening and antiseptic effects, stimulates the regeneration of the gastrointestinal mucosa. Allanton is used in a dose of OD g 3-4 times a day before meals. Side effects of the drug are heartburn, epigastric pain, which is observed in the first few days from the start of therapy and soon goes away on its own, as well as allergic reactions.
Particular attention should be paid to some medications used in the pharmacotherapy of bile, or “alkaline”, reflux esophagitis. As mentioned above, the latter is largely due to the effect on the esophageal mucosa, primarily of bile and pancreatic enzymes. In addition to its direct effect, bile enhances the diffusion of hydrogen ions in the tissue of the esophagus. This leads to one of the main tasks of drug correction of “alkaline” esophagitis - neutralization and binding of bile acids. This property is largely possessed by aluminum-containing antacids (almagel, phosphalugel, gastal), as well as cholestyramine (questran). Being an anion exchange resin, the latter forms non-absorbable complexes with bile acids in the intestine, which are subsequently excreted from the body. The drug reduces the utilization of cholesterol in the intestines, reduces the content of 6-lipoproteins and triglycerides in the blood. Prescribed 12-16 g per day orally.
The reverse diffusion of hydrogen ions into the esophageal mucosa is inhibited by sodium carbenoxolone (biogastron, duogastron, caved S). In addition, it has the property of stimulating mucus formation and regeneration of epithelial cells. Side effects of carbenoxolone are associated with its mineralocorticoid activity (retention of sodium and fluid ions in the body, hypokalemia, arterial hypertension, muscle weakness, increased levels of serum transaminases, myoglobinuria).
It is advisable for all patients with peptic esophagitis to undergo sedative therapy, as well as physical therapy: electrophoresis of novocaine or magnesium sulfate on the area of the cervical sympathetic ganglia, nuchal zone or Zakharyin-Ged zones corresponding to the esophagus, galvanic collar according to Shcherbak, etc.
Combination therapy for peptic esophagitis. Almost each of the above-described drugs used at the present stage for the treatment of patients with peptic esophagitis primarily affects one aspect of the pathogenesis of this disease. Meanwhile, as a rule, not one, but several factors are simultaneously involved in its development, which can only be eliminated by a combination of various medications. Moreover, some drugs have certain disadvantages, which, however, are the flip side of their advantages. For example, the M-cholinomimetic bethanechol, widely used in most gastroenterological clinics in the West, can not only tone the muscles of the lower esophageal sphincter, but also to some extent enhance gastric secretion, to suppress which it is necessary to use appropriate medications. These are the main arguments in favor of a combined approach in the treatment of peptic esophagitis. The counterarguments of supporters of monotherapy (difficulties in taking a large number of medications for patients, an increase in the number of side effects, increased costs of treatment, etc.) look unconvincing in this light.
There is no universal, once-and-for-all pharmacotherapy regimen for peptic esophagitis. And the reason for this is the abundance of manifestations of this disease, determined by the individuality of each specific case. In addition, the arsenal of drugs used to treat peptic lesions of the esophageal mucosa is steadily expanding with new, more active drugs. Hence the known abundance of drug combinations and the lack of consensus among clinicians regarding the effectiveness of each of these combinations. However, despite all the apparent diversity, there is a certain commonality between them. Based on modern ideas about the pathogenesis of peptic esophagitis, the main objectives of pharmacotherapy for the latter are the following:
- correction of the “main” disease that caused it, if any;
- reducing the frequency, duration and volume of gastroesophageal reflux, which is usually achieved by prescribing drugs that tonify the cardioesophageal sphincter and facilitate the evacuation of food from the stomach;
- leveling the aggressive properties of gastric or duodenal contents;
- protecting the esophageal mucosa from the damaging effects of the above factors and, if necessary, accelerating its regeneration.
In our opinion, the solution of the mentioned problems is facilitated by the administration of the following exemplary combinations of drugs.
Treatment of gastroesophageal (“acid”) reflux:
- cerukal, bismuth preparations, long-acting aluminum-containing antacids (almagel, gastal, phosphalugel);
- cerucal, antacids, NG-histamine blockers;
- bethanechol, antacids, NG-histamine blockers;
- bethanechol (cerucal), antacids, NG-histamine blockers, reparants.
Treatment of “alkaline” reflux esophagitis:
- cerucal, aluminum-containing antacids;
- cerucal, cholestyramine, aluminum-containing antacids;
- cerucal, aluminum-containing antacids, cholestyramine, carbenoxolone.
If necessary, treatment can be supplemented by the prescription of psychotropic drugs (minor tranquilizers, antipsychotics, antidepressants). In some cases this brings some benefit.
Naturally, the above drug combinations are not able to provide for the entire variety of possible shades of reflux esophagitis. Therefore, schemes can be changed in accordance with the characteristics of a particular situation.
The failure of conservative treatment of peptic esophagitis is an indication for surgical correction of gastroesophageal reflux.
Results of conservative treatment, prevention and medical examination of patients with peptic esophagitis. According to a number of authors, complex drug correction of reflux esophagitis makes it possible to achieve its remission in 64.4-92% of cases. The presence of remission is determined on the basis of clinical data with mandatory morphological confirmation. A year after completion of the initial course of treatment, these indicators drop to 38.8% of cases.
The effectiveness of drug treatment for patients with peptic esophagitis is influenced by the following factors: the severity of damage to the esophageal mucosa, the adequacy of the therapy, the nature of the “main” disease.
The long-term results of conservative treatment of patients with peptic esophagitis associated with hiatal hernias have been studied in detail.
Primary prevention of reflux esophagitis should take place in such pathological processes as hiatal hernia, peptic ulcer of the stomach and duodenum, cholecystitis, pancreatitis, scleroderma of the esophagus, etc.
Prevention of relapses of peptic lesions of the mucous membrane of the distal esophagus, and they occur in 23.5% of cases, is carried out in the process of dispensary observation of such patients. In addition, the purpose of clinical examination is the timely identification and treatment of possible complications. All persons suffering from peptic esophagitis are subject to clinical observation, which can be carried out both on an outpatient basis and in a hospital setting. In addition to a general examination of these patients, esophagoscopy with targeted biopsy, intraesophageal pH-metry and radiography of the esophagus are mandatory. The mentioned diagnostic procedures make it possible to assess the nature, frequency and duration of gastroesophageal reflux and, if necessary, prescribe appropriate therapeutic measures. Anti-relapse treatment is usually carried out 2 times a year, its volume and duration are determined primarily by the condition of the mucous membrane of the distal esophagus. The presence of erosive and ulcerative defects is an indication to increase the number of anti-relapse courses of treatment up to 4 times a year.
The ability to work of patients with reflux esophagitis in some cases should be limited. They are not recommended for all types of activities associated with increased intra-abdominal pressure and forward bending of the body. Patients with severe peptic esophagitis need to be transferred to disability group II.
- Surgery
Indications for surgical treatment are failure of drug treatment, repeated bleeding, frequent aspiration pneumonia associated with gastroesophageal reflux. Especially often, indications for surgery arise when reflux esophagitis is combined with a hiatal hernia.
The goal of surgical treatment is to restore the normal closure function of the cardia. To do this, after surgery, the pressure in the lower esophagus should be approximately 3 times higher than the pressure inside the stomach.
The main type of surgery for reflux esophagitis is Nissen fundoplication, which gives more favorable immediate and long-term results than other types of surgical interventions used to treat this disease.
When reflux esophagitis is combined with severe hyperacidity of gastric juice or duodenal ulcer, fundoplication is performed simultaneously with truncal vagotomy and pyloroplasty or selective proximal vagotomy. This allows you to significantly reduce the acidity of gastric juice and achieve rapid relief of the symptoms of peptic reflux esophagitis. In the case of a combination of reflux esophagitis with a gastric ulcer, gastric resection is most often performed according to Billroth-I or Billroth-P (preferably in the Roux-en-Y modification, which also excludes alkaline reflux) together with fundoplication.
The greatest difficulties arise when reflux esophagitis is complicated by secondary shortening of the esophagus. In such a situation, preference is given to fundoplication using the Nissen-Rosetti method, leaving part of the proximal stomach in the pleural cavity, or valve transabdominal gastroplication using the Kanshin method. Abroad, gastroplasty using the Collis method is used to treat such patients. The operation consists of dissecting the anterior and posterior walls of the stomach in a vertical direction, starting from the angle of His, for 12-15 cm, followed by suturing the gastric tube, lengthening the esophagus, and forming the gastric vault with an acute angle of His. However, due to the relative complexity and morbidity, this type of surgical intervention is used infrequently.
Chronic erosive esophagitis of the esophagus
The chronic course of the disease occurs due to the following reasons:
- GERD;
- cardiac valve dysfunction;
- stomach and duodenal ulcers;
- obesity;
- frequent consumption of salty, spicy and fatty foods;
- hiatal hernia.
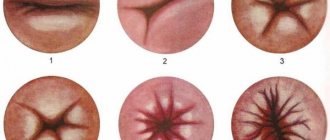
Gastroesophageal reflux disease leads to chronic inflammation of the esophageal epithelium. Due to insufficient closure of the sphincter muscle ring separating the esophagus and stomach, food can flow back into the esophageal tube, irritating the mucous membrane. Hyperemia and swelling of the epithelium of the walls of this internal organ is determined by the first stage of the disease. Symptoms during this period are not pronounced, mainly heartburn. If GERD is not treated, the membrane will not only turn red, but erosions will form on it. This is the second stage of the disease.
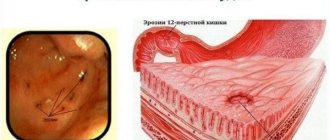
This is what doctors diagnose when patients come to them with complaints of heartburn and burning along the esophagus. During an endoscopic examination of the walls of the internal organ, the presence of single or multiple erosions is noted on the epithelium of the walls, which do not merge and form defects on the mucosa in the area of one fold. The walls of the esophagus are covered with fibrous plaque.
The third stage is characterized by the degeneration of erosions into ulcers. This is already erosive ulcerative esophagitis. At this stage, not only the surface layer of the epithelium is affected, but also the underlying tissue. The defects extend beyond one fold and can be observed around the circle of the esophageal mucosa. With further progression, the muscle tissue of the esophageal tube is damaged. The condition worsens as the above symptoms are supplemented by a persistent cough , vomiting mixed with blood, and pain along the esophagus , which occurs regardless of food intake.
This stage is dangerous due to the development of complications:
- bleeding;
- stenosis;
- Barrett's esophagus.
In addition, when an infectious factor is added to the background of erosive esophagitis, purulent inflammation of the esophagus can develop. Such conditions lead to a deterioration in the general condition of the patient, and in case of bleeding require emergency hospitalization. Erosive fibrinous esophagitis should not be allowed to develop.
Diagnosis of esophagitis
To diagnose esophageal esophagitis, a gastroenterologist, in addition to collecting anamnesis and complaints, needs to conduct a series of studies to determine the form and type of the disease. This will help effectively eliminate inflammation and restore the functions of the esophagus. If there is a pronounced symptom complex that combines heartburn, pain, cough and other symptoms, it will not be difficult for the doctor to identify the disease. If the pathology has become chronic, to make a correct diagnosis you will need to:
- X-ray of the esophagus and stomach with contrast;
- diagnostic endoscopy of the esophagus (endoscopic esophagoscopy, gastroscopy), and, if necessary, the stomach.
This diagnosis helps determine the degree of damage to the mucous membrane, the location of the inflamed areas and their size. X-ray diagnostics is prescribed if the presence of ulcers of the esophagus is suspected.
To determine the causes of the inflammatory process in the esophagus, additional studies are prescribed:
- zophagomanometry for diagnosing motor functions of the esophagus;
- Ultrasound, CT or MRI to identify problems with the stomach and intestines, if there are signs of such;
- laboratory tests (general and biochemical analysis of blood, urine, stool tests for dysbacteriosis and parasites).
These measures are designed to detect the causes of the inflammatory process, be it parasitic or helminthic infestation, bacterial, fungal or viral infection of the digestive tract.
Therapeutic measures
Therapy for the erosive form of the disease is similar in treatment principles to other types of esophagitis and GERD. It consists of:
- drug treatment;
- dietary nutrition;
- preventive measures.
Drug therapy
- Drugs that reduce gastric acidity - antacids . In combination with them, medications are prescribed that create a protective film on the surface of the gastric mucosa, as well as on the food bolus, which reduces the harmful effects of hydrochloric acid on the walls of the esophagus - alginates . The drugs of choice are Rennie , Gaviscon , Phosphalugel .
- Prokinetics are medications that help food move faster through the esophagus into the stomach and thereby reduce the irritating effect of food on the lining of the esophageal tube ( Cirukal , Metaclopramide , Motylium ).
- If erosions occur as a result of reflux caused by insufficient function of the cardia, then a PPI . These are medications that increase the contractility of the sphincter that separates the esophagus and stomach ( Omez ).
- For better regeneration of epithelial cells of the esophageal mucosa, Solcoseryl and Alanton .
- In the presence of infectious inflammation, vitamins and antibiotics .
If complications arise or drug therapy is ineffective, then surgery is performed. This may be a traditional technique (an incision in the chest or abdomen) or laparoscopy, which is less traumatic.
Treatment of esophagitis
To carry out full treatment of esophagitis, if unpleasant symptoms appear, you need to contact a gastroenterologist. After the examination, he prescribes complex therapy, which includes:
- medication treatment;
- physiotherapy;
- diet.
In case of chemical damage to the mucous membrane of the esophagus, an urgent gastric lavage is performed through a tube, which means neutralizing aggressive liquids and removing them through the tube to the outside.
This procedure is carried out due to the fact that classic lavage (using artificially induced vomiting) can cause extensive chemical burns of the esophagus.
In case of an infectious lesion of the mucous membrane of the esophagus, patients are prescribed antibiotics, antifungal or antiviral agents, depending on the type of pathogens detected at the diagnostic stage. The following groups of drugs help relieve pain and heartburn:
- prokinetics (Cerucal, Motilium, Domperidone);
- reparants (Venter, Solcoseryl);
- antacids (Almagel, Phosphalugel, Maalox, Gaviscon and others).
If reflux esophagitis is diagnosed, the disease is treated with the use of proton pump blockers (Omez, Lanzoprazole, Rabenprazole and others).
An important detail of therapy is strict adherence to the diet. Products that irritate the mucous membrane of the esophagus are excluded from the menu: chocolate, alcohol, carbonated drinks, spices. Only warm foods are eaten, since cold and hot foods irritate inflamed mucous membranes.
Diet
Diet plays a big role. The diet for erosive esophagitis is aimed at reducing the irritating effect of foods on the esophageal mucosa. The following dishes are excluded from the diet:
- spicy;
- salty;
- spicy;
- fat;
- fried.
And also products:
- fresh vegetables;
- sour fruits;
- legumes;
- black bread;
- mushrooms.
Alcohol and smoking are strictly prohibited.
Patients should eat small meals at least 5-6 times a day so as not to overload the stomach and cause reflux. After eating, you should not lie down to rest, but you should walk around a little, but not do physical work, especially one that requires bending your torso forward. There should be at least 3 hours between your last meal and bedtime.
Patients can eat
steamed , baked or boiled .
Also, you should not eat very hot or cold food. During meals, you need to chew food well and do not eat rough food, so as not to injure the esophageal mucosa. When GERD with erosive esophagitis is diagnosed, the diet must be followed.
Prevention
After treatment, patients need to monitor not only their diet, but also change their lifestyle. Such people should not engage in sports associated with abdominal tension. You also need to reduce physical and emotional stress. If the work is related to the position - bending the body forward, then this type of activity needs to be changed. You should not wear tight clothing, tight belts or corsets.
Walking before bed, as well as drinking tea ( mint , lemon balm , calendula , chamomile ), which has a sedative and anti-inflammatory effect, give good results.
It must be remembered that when the first signs of the disease appear, you should consult a doctor, since self-medication or the use of traditional methods will not completely cure the disease, and in some cases leads to exacerbations. Once a year, such patients need to visit a gastroenterologist with a mandatory endoscopic examination. If the patient's condition worsens, consultation is needed immediately.