Quick transition Treatment of ulcerative colitis
Ulcerative colitis is a rare chronic disease characterized by inflammation of the inner layer of the colon, the mucous membrane. In this case, blood appears in the stool, and bowel movements themselves can become very frequent. In severe forms of the disease, anemia (decreased hemoglobin), weight loss may develop, and joints and skin may become inflamed. Fortunately, most cases of ulcerative colitis present with only intestinal symptoms.
Rectal erosion: causes
Defects in the intestinal mucosa can be of a polyetiological nature, that is, they arise for several reasons:
- unhealthy diet (excess hot, spicy and fatty foods irritate the mucous membranes, provoking the formation of first inflammatory and then erosive lesions);
- mechanical injuries to the mucous membrane of the rectum (for chronic constipation - with solid particles of feces or the tip of an enema, during anal sexual intercourse);
- infectious diseases (Escherichia coli, cocci, chlamydia, cytomegalovirus produce toxic waste products that damage the intestinal wall) and helminthic infestation (helminths damage the mucous membrane mechanically);
- pathology of other organs of the gastrointestinal tract (hepatitis, pancreatitis, cholelithiasis) and the digestive disorders caused by them;
- autoimmune and other pathologies accompanied by the formation of ulcers and erosions on the mucous membranes (Crohn's disease);
- malignant neoplasms of the final sections of the intestine, as well as radiation therapy of tumors.
Why is inflammation of the intestinal walls dangerous?
Recently, the number of Russians diagnosed with IBD has increased annually by an average of 10–12%. Most often, residents of modern megacities suffer from ulcerative colitis and Crohn's disease. In the first case, the mucous membrane of the colon is affected, and in the second, the end of the small intestine and the beginning of the large intestine. Inflammation leads to the formation of bleeding ulcers and progresses rapidly, leading to irreversible tissue damage if undiagnosed and treated.
- Patients with Crohn's disease have a significantly increased risk of intestinal obstruction and, as a result, fistula formation.
- Massive bleeding in ulcerative colitis can cause intestinal perforation and life-threatening peritonitis.
- Finally, IBD is recognized as one of the factors that significantly increases the likelihood of tumor formation in the intestine.
Even at the initial stage, intestinal diseases manifest themselves with unpleasant symptoms that significantly reduce the quality of life.
Erosion of the rectal mucosa: types
Erosion of the rectal mucosa can be single or multiple. The disease manifests itself in flat, polyp-like or hemorrhagic forms. If an infection gets into the eroded surface, purulent inflammation may develop, which entails serious complications.
Erosive lesions of the rectal mucosa are acute (with a process duration of up to two weeks), subacute (with symptoms persisting for up to 5–7 weeks) and chronic (up to several years).
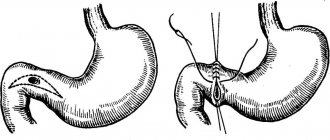
The process of transition of an acute ulcer into a chronic fissure
The transformation of an acute anal fissure into a chronic pathological process occurs against the background of a spasm of the internal anal sphincter. Its resolution is a key problem in ulcer healing. In the treatment of chronic anal fissure, proctologists at the Yusupov Hospital are increasingly using non-surgical methods of influencing the tone of the internal anal sphincter (“chemical sphincterotomy”) in order to reduce it.
Theories explaining the mechanism of the appearance of ChAT should also comment on such features of the course of the disease as the favorite position along the posterior wall of the anal canal and the lack of growth of granulations in the area of the mucosal defect.
Doctors believe that after minor traumatic impacts on the posterior wall of the anal canal in the area of the anorectal angle, in some patients anal ulcers do not heal due to a secondary low level of local blood flow. This is how a chronic anal fissure is formed.
Rectal erosion: symptoms
Single lesions in 90% of cases do not manifest themselves clinically and are asymptomatic. With rectal erosion, symptoms and treatment depend on the form of the process: the more acute it is, the more pronounced the clinical picture of proctitis and the need for its treatment are.
The following symptoms are characteristic of acute forms of erosive lesions:
- intense pain in the rectum, increasing during bowel movements;
- false urge to defecate;
- loose, unformed stools;
- the presence of mucus and blood impurities in the stool;
- sphincter spasms;
- heat.
Chronic forms are characterized by a blurred clinical picture: complaints from patients with a long, sluggish process are usually inexpressive and include:
- dull or aching pain in the lower abdomen and perineum;
- a feeling of discomfort in the anal area, rarely - mild itching;
- the presence of mucus in the stool;
- low-grade fever;
- anemia and associated pallor of the skin.
Due to the mild severity of symptoms, chronic forms of erosion in the anorectal area are more often detected during preventive examinations or during an endoscopic examination by a coloproctologist.
DIAGNOSIS AND TREATMENT of Crohn's disease and ulcerative colitis
How to differentiate between Crohn's disease, ulcerative colitis and irritable bowel syndrome? What tests should a general practitioner carry out? What drugs should be used to treat these diseases?
| Figure 1. Inflamed intestinal wall in Crohn's disease. After World War II, its incidence increased sharply in many regions. |
Treatment for inflammatory bowel disease (IBD) generally produces good results, although its chronic nature inevitably causes confusion and frustration for both patients and physicians from time to time.
With the increasing use of immunosuppressive drugs, which is accompanied by an increase in the incidence of complications, and new types of treatment, it seems appropriate that a significant proportion of these patients receive therapy under the supervision of a gastroenterologist.
The general practitioner should be able to recognize in which cases of severe colitis requires emergency hospitalization, as this can save the patient's life.
Many patients with IBD, especially those with mild disease, are treated exclusively by a general practitioner, but co-management of such patients with gastroenterology specialists is often the best approach.
The introduction of more active drug and surgical treatment has reduced mortality in these diseases. However, it remains to be seen whether new drugs based on a better understanding of the immunological mediators of intestinal inflammation will live up to initial hopes.
IBD usually includes ulcerative colitis (UC) and Crohn's disease (CD), although lesser-known diseases such as collagenous colitis and eosinophilic colitis are also sometimes included.
UC and CD are diseases of northern countries and are more common in urban populations [1]. However, in recent decades, their incidence has increased in Japan and southern Europe, in parallel with rising living standards.
The effect of gender is weak: men are slightly more predisposed to UC, and women - to CD.
There are two peaks of incidence: at the age of 15–25 years and 50–80 years. CD is rare in children under 10 years of age, while UC can occur in early infancy. In Northern Europe, the estimated incidence rates for UC and CD are respectively 10 (prevalence 140) and 6 (prevalence 65) per 100,000 population.
The epidemiology of IBD indicates that UC and CD are separate pathological conditions with a common etiological factor in the form of genetically determined, increased susceptibility to some environmental factor. Relatives of someone with IBD are more likely to develop a similar disease (but not necessarily the same type), and studies of monozygotic twins support the existence of a genetic factor.
Currently, research is being carried out in Oxford and other centers to identify various loci in the genome that determine such susceptibility. The role of many etiological factors in the development of IBD (including tobacco smoke, carbonated drinks, toothpastes, oral contraceptives, measles, and M. paratuberculosis) has been hypothesized, but none has received widespread acceptance.
It seems that in such diseases, for some reason, the tolerance of the intestinal mucosa to a variety of bacterial and food antigens is lost and an uncontrolled inflammatory process develops.
Symptoms and clinical examination findings
| Figure 2. Ulcerative colitis. |
Manifestations of UC and CD reflect the degree of activity of the pathological process. With UC, the mucous membrane of the rectum and colon is inflamed, covered with superficial ulcerations, which causes abdominal pain (often left-sided), blood and mucus in the stool, diarrhea, often accompanied by pain during bowel movements and sometimes tenesmus.
In addition, general malaise, loss of appetite and weight loss are often observed. Upon palpation, the entire abdomen can be moderately painful; rectal examination also often causes pain, and blood remains on the glove.
CD can cause colitis and present with symptoms (in approximately 30% of cases), but most often affects the distal small intestine, either with or without colitis.
Unlike UC, CD can affect any part of the gastrointestinal tract - from the mouth to the anus, causing transmural inflammation leading to such serious complications as strictures and fistulas.
If the ulcers heal and leave behind fibrous stenosis, then symptoms of obstruction appear. Patients often point to a specific area where swelling and pain occur at times. A painful mass may be palpable in the right iliac fossa.
Abscesses often lead to the formation of fistulous tracts between loops of intestine or between the intestine and other organs, such as the vagina or bladder. The condition of such patients is often deplorable, as they suffer from constant pain and systemic symptoms, and their disease progresses more aggressively. Anorexia, weight loss, and intermittent fever are common.
IBD typically waxes and wanes, with alternating periods of remission and relapse. The course of UC is determined mainly by the prevalence and severity of the pathological process during the first year after diagnosis. In patients who have had mild intermittent proctitis for five years, most likely, this disease will continue to proceed in the same way.
Conversely, the risk of colostomy is highest in the first year, when patients have not yet had time to get used to the idea that they have UC, and the greater the shock the ileostomy becomes for them.
The prognosis for UC is currently very good. In the recent past, the mortality rate was 55% over 15 years, but nowadays, due to active modern treatment, both medical and surgical, this figure is only slightly higher than the mortality rate in the general population. However, in the age group over 60 years of age, the prognosis is less favorable.
CD is more severe and unpredictable, however, the rule is that in most patients the type and severity of the disease remain the same as at diagnosis.
With the development of fibrous strictures, the course of the pathological process is often benign, and with the formation of abscesses and fistulas there is a tendency for it to be more aggressive. In 1/2-2/3 of patients with CD, there is eventually a need for surgical treatment, with reoperation rates reaching 50%. About 6% of patients with CD die directly from complications of this disease [2].
Differential diagnosis and research methods
In patients admitted with typical manifestations of IBD, enterocolitis of an infectious nature should first be excluded. It is necessary to examine stool for the presence of pathogens of the genera Salmonella, Shigella, Campylobacter and Yersinia, as well as for worm eggs, cysts and parasites. Pseudomembranous colitis caused by Clostridium difficile is excluded by testing the stool for the toxin of this pathogen.
However, IBD can coexist with and even be caused by intestinal infections, so if symptoms do not resolve within two weeks, further investigation is necessary.
Sometimes ischemic colitis or acute or chronic radiation colitis can be mistaken for IBD, especially CD. Lymphoma, intestinal tuberculosis and cancer are also included in the differential diagnostic range.
Many patients with irritable bowel syndrome (IBS) end up having a colonoscopy to rule out IBD—the two conditions share some common features. Of course, blood in the stool is not typical for IBS. Another useful feature for differentiation is the presence of nocturnal symptoms, which are very rare in IBS.
Sigmoidoscopy and biopsy of the posterior wall of the rectum should be performed as early as possible (ideally, when the patient first contacts a general practitioner), since in this case effective treatment can be started in a timely manner. Most patients, frightened by their disease and alarmed by bleeding from the rectum, have to be reassured and convinced of the need for a thorough examination, despite the fact that some of the diagnostic techniques used are extremely unappealing. Blood tests are important to rule out anemia and to monitor the progression of the disease, but they cannot significantly help in making the diagnosis itself. However, with abdominal pain and diarrhea, abnormal findings on this test may be more likely to indicate IBD rather than IBS. It is quite enough to conduct a general blood test, determine ESR or C-reactive protein, electrolytes and liver function indicators.
In UC, the extent and severity of the disease is most accurately assessed by colonoscopy with biopsies taken for histological examination from each part of the colon. Iliocolonoscopy is also a good method for diagnosing CD and allows this diagnosis to be confirmed histologically; this is the only way to detect early stage involvement of the ileum or colon in this disease. X-ray examination with barium sulfate ingestion over time helps to identify small intestinal strictures and fistula tracts in CD. Irigoscopy is still used to detect colonic lesions, but this method is less sensitive than colonoscopy, especially for mild disease. Scanning using technetium-labeled leukocytes is an informative method for assessing the activity of a pathological process during follow-up.
Distinguishing UC from CD is not always easy. Their manifestations coincide in a number of ways, so CD limited to the rectum and sigmoid colon may resemble UC. Sometimes histological examination does not allow a definitive diagnosis, and in approximately 10-15% of cases the diagnosis remains unspecified, at least for some time. In many of these cases, upon follow-up, the patient turns out to have CD.
Treatment
Given the above, the situation is made easier by the fact that the treatment of UC and CD is very similar, but at the same time, this fact may simply reflect the limitations of our means of combating these diseases.
Perhaps the next generation of drugs will allow a more differentiated approach to the treatment of these two diseases.
The goal of therapy for IBD is to relieve symptoms, induce remission, and prevent relapses. Currently, drug treatment is prescribed according to a stepwise scheme.
Sulfasalazine and 5-aminosalicylates (5-ASA)
These are anti-inflammatory drugs that are used to treat mild to moderate IBD, but they are more widely used to maintain remission.
They have a multifaceted effect on the immune system, in particular they suppress inflammation - both on the surface of epithelial cells and at the level of metabolism inside them.
Sulfasalazine was first used 50 years ago, and it achieves remission in 35-80% of patients. With its use, side effects are common (in 20% of patients), mainly nausea, vomiting, headaches and loss of appetite, but this drug is very cheap.
There is no need to use new 5-ASA drugs in the remaining 80% of patients who do not experience significant side effects when using sulfasalazine. The only exception is, perhaps, young men, since sulfasalazine worsens sperm parameters.
Sulfasalazine is broken down by bacteria into sulfapyridine (which causes most of the side effects) and the active component 5-ASA (mesalazine), and is therefore released in the colon.
Asacol, a coated dosage form of mesalazine that is released at pH>7, and olsalazine, a dimeric form of 5-ASA broken down by bacteria, also act in the distal intestinal tract.
Pentasa, a microgranular dosage form of mesalazine, is released throughout the small intestine and colon; therefore, it is more effective in CD involving the ileum. In practice, Pentasa may also be the best remedy for UC with diarrhea, since such patients often note the excretion of unchanged asacol tablets in their feces.
Balsalazide is another 5-ASA derivative that has been effective in acute (moderately to severe) UC and is better tolerated than mesalazine [3]. Whatever drug is chosen, all accumulated experience shows that significant doses are required to suppress active disease (namely 3.2-4.8 g per day).
Rectal preparations of mesalazine are expensive but play a significant role in the treatment of recalcitrant proctocolitis. Finally, 5-ASA drugs are not without side effects: they sometimes increase abdominal pain and diarrhea; In addition, there are a number of reports in the literature of the occurrence of myocarditis, neuropathy, pancreatitis and nephrotoxicity.
Corticosteroids
In UC and CD, corticosteroids can achieve remission, but they are less effective in maintaining it.
For moderately severe disease, prednisolone is used in doses of 30-40 mg, which are then gradually reduced to approximately 10 mg with a positive effect. Then the drug is discontinued even more carefully.
Long-term therapy with corticosteroids is undesirable, especially in young patients. This is due to their known systemic effects, but these disadvantages can be overcome to some extent with the help of locally acting drugs when the distal parts of the intestine are affected.
Another way to limit systemic toxicity is the use of budesonide, which has the advantage of having a high affinity for glucocorticoid receptors and breaking down a significant amount of it on its first pass through the liver. It is available in tablet form for gradual release in the ileum and cecum.
Immunosuppressants
Azathioprine and, in the US, 6-mercaptopurine are very effective for chronic active IBD that has not achieved remission with corticosteroids or has frequent relapses.
However, a significant time passes before the effect occurs (on average 12 weeks), and in approximately 10% of patients, treatment must be stopped due to side effects such as nausea or vomiting, pancreatitis and hematopoietic suppression.
There is also an increased risk of infection (but no greater than with steroid treatment) and a small chance of developing a risk of neoplasia.
However, azathioprine is now increasingly used for maintenance therapy in CD. The study showed encouraging results: the group receiving this drug had a remission rate of 42%, and only 7% in the placebo group. However, this effect requires sufficient doses (2 mg/kg per day). The advantage of using cyclosporine is the rapid onset of effect. Therefore, it is used for the following indications: as a means of rapid relief for acute, severe forms of CD and UC, in the absence of relief from high doses of corticosteroids. Yet the nephrotoxicity of this drug limits its use in other situations.
Several new treatments are currently undergoing various phases of clinical trials. These techniques involve the use of monoclonal antibodies against individual cytokines (such as IL-12, TNF-α and against recombinant cytokines (IL-10). Preliminary results indicate that the effect of antibodies against TNF-α in CD can lead to long-term remission several months. However, their use is limited by the need for intravenous administration of the drug and its high cost. Thalidomide, a strong TNF-α inhibitor, has been successfully used in the treatment of IBD. Clinical trials of its new analogues, which are reported to be less severe, are now beginning , characteristic of thalidomide, as toxicity to the fetus.
Other Treatment Approaches
Some gastroenterologists use metronidazole and ciprofloxacin as first-line drugs for the treatment of CD. Remissions are often achieved, but relapses occur earlier. Nutrition with elemental mixtures has been successful in treating IBD in children, achieving remission at the same rate as corticosteroid treatment. A Cambridge research group recently reported their preliminary results showing the effectiveness of elemental mixtures in treating CD. At the same time, certain types of food are gradually introduced into the diet until the product that causes an exacerbation of the disease is discovered. According to some reports, a number of patients were cured using this method. Unfortunately, elimination diets are rarely beneficial for IBD, except in the few cases where a dairy-free diet may help UC.
It is important to pay attention to the patient’s lifestyle. It is very difficult to reduce stress, but it should be remembered that stress can play a significant role in the development of relapses of both UC and CD. Smoking appears to be protective in UC, but it significantly worsens the prognosis in CD, and patients with this disease should be strongly advised to quit smoking. Nonsteroidal anti-inflammatory drugs often cause relapses and should be avoided if possible.
Surgery
Surgery is indicated for UC in cases where colitis is fulminant in nature or if remission is not achieved during a long course of the disease, despite the use of the best drugs. In CD, when stenosis and obstruction develop, strictureplasty or resection is sometimes necessary. For this disease, surgical treatment may also involve draining abscesses or performing anastomoses to bypass inflammatory masses or fistulas.
When is hospitalization necessary?
Acute, severe colitis is an indication for immediate hospitalization, bed rest and intravenous corticosteroids. This means that any patient diagnosed with ulcerative colitis, manifested by frequent bloody diarrhea (6 or more times a day) and fever (more than 37 ° C) or tachycardia (more than 90 per minute), should be hospitalized. Anemia (hemoglobin less than 100 g/l), ESR more than 30 mm/h, or albumin less than 35 g/l are considered valuable additional indicators of attack severity.
For moderately severe disease, treatment should consist of oral corticosteroids. Such patients must be urgently referred to the hospital clinic. Mild cases should be treated with 5-ASA and/or rectal steroids (or rectal 5-ASA).
Most gastroenterology clinics are also happy to consult on mild cases, but long-term follow-up usually falls on the shoulders of general practitioners. CD, except for its most mild forms, should ideally be treated in a clinic with gastroenterological and surgical services.
Literature
1. Shivananda S., Lennard-Jones J., Logan R., Fear N., Price A., Carpenter L., van Blankenstein M. Incidence of inflammatory bowel disease across Europe: there is a difference between north and south Results of the European Collaborative Study of Inflammatory Bowel Disease (EC-IBD). Gut, 1996; 39 (5): 690-697. 2. Inflammatory Bowel Disease, Allan, RN et al (eds). London: Churchill Livingstone, 1997. 3. Green JR, Lobo AJ, Holdsworth CD, Leicester RJ, Gibson JA, Kerr GD, Hodgson HJ, Parkins KJ and Taylor MD Balsalazide is more effective and better tolerated than mesalamine in the treatment of acute ulcerative colitis The Abacus Investigator Group. Gastroenterology 1998; 114(1):15–22.
Note!
- The epidemiology of IBD indicates that UC and CD are separate pathological conditions with a common etiological factor in the form of genetically determined, increased susceptibility to some environmental factor.
- Ulcerative colitis causes abdominal pain (often on the left side), blood and mucus in the stool, diarrhea, often accompanied by pain and sometimes tenesmus. In addition, symptoms such as general malaise, loss of appetite and weight loss are often observed.
- Crohn's disease can cause colitis and present with symptoms (in approximately 30% of cases), but most often affects the distal small intestine, either with or without colitis. Unlike ulcerative colitis, Crohn's disease can affect any part of the gastrointestinal tract, from the mouth to the anus, causing transmural inflammation with two important consequences: strictures and fistulas. If the ulcers heal and leave behind fibrous stenosis, then symptoms of obstruction appear. Patients often point to a specific area where swelling and pain occur at times. A painful mass may be palpable in the right iliac fossa.
- Inflammatory bowel diseases usually wax and wane, with alternating periods of remission and relapse.
- Many patients with irritable bowel syndrome (IBS) end up having a colonoscopy to rule out inflammatory bowel disease—the two conditions share some common features. Of course, blood in the stool is not typical for IBS. Another useful feature for differentiation is the presence of nocturnal symptoms, which are very rare in IBS.
- Sigmoidoscopy and biopsy of the posterior wall of the rectum should be performed as early as possible (ideally, when the patient first contacts the doctor), since in this case effective treatment can be started immediately.
- Treatment for UC and CD is largely the same. The goal of therapy for IBD is to relieve symptoms, induce remission, and prevent relapse. Currently, drug therapy is often prescribed in a stepwise manner.
What to tell the patient?
- You have a disease that will last your entire life and that cannot yet be completely cured.
- Sometimes the inflammation will recede, and you will not be bothered by the manifestations of the disease. Such periods are called “remissions”. Our task is to prolong remissions as much as possible.
- From time to time, sometimes for quite a long time, you will need to take anti-inflammatory drugs to achieve remission and prevent relapses of the disease.
- For women of childbearing age, there is no reason why you cannot get pregnant and have a healthy baby.
- In some patients, pregnancy can lead to an exacerbation of the disease, in others, on the contrary, it improves the condition. If possible, inform us in advance about your planned pregnancy so that we can select medications that are safe for the fetus.
- For the last few years, your illness has been mild, so it is very likely that it will be of the same nature in the future. Of course, we will continue to carefully monitor its progress to make sure of this.
- We have several leaflets for patients where you can find more detailed information. If you have any questions, we will be happy to answer them.
Patients with ulcerative colitis
- In most cases, the disease occurs in a mild form, for which treatment it is enough to take pills.
- We have to admit that in a small number of patients, ulcerative colitis becomes severe, which sometimes requires removal of the colon. This may mean that the patient's ileum will be exposed to the skin of the abdomen (with a colostomy bag), but in such patients it is usually possible to restore intestinal continuity and natural passage of intestinal contents later.
- With the right treatment, you will feel better and can continue to lead a full and active life.
- If the disease affects the entire colon, then after about 8-10 years you will need to have regular colonoscopies - once a year or every two years. This is done in order not to miss rare cases of the development of cancerous changes against the background of prolonged inflammation.
Patients with Crohn's disease
- Crohn's disease in some patients is quite mild, in rare cases it is quite severe; between these two extremes there can be all shades of the “spectrum” of severity.
- Nowadays, with the help of medications and operations, it is possible to achieve much greater treatment results than before. Research is being conducted on new therapy methods that will allow further success to be achieved.
- There are reports in newspapers and on television about the connection between Crohn's disease and measles, as well as stories about the role of bacteria passing from the cow's body into dairy products. These messages are of some interest and are being actively verified by scientists. However, there is still no conclusive evidence that these factors actually cause Crohn's disease.
It is very important that we do not lose sight of you. Even if the symptoms of the disease do not bother you much, you will need to continue to see your doctor regularly.
Diagnostics
The diagnosis is established on the basis of patient complaints, visual and manual examination, assessment of the results of a clinical blood test and iron content, and an occult blood test. Instrumental research methods include colonoscopy, rectoscopy, capsule endoscopy or radiography with contrast. If an infection is suspected, the doctor will prescribe a stool culture to determine the type of pathogen and its sensitivity to antibiotics.
Differential diagnosis is carried out with irritable bowel syndrome, colitis syndrome, chronic colitis, diarrhea of infectious origin.
How to treat erosions on the rectum?
For rectal erosion, treatment is aimed at healing damage to the mucosa and preventing the defect from deepening into an ulcer. Often, it is enough to eliminate the underlying disease that caused damage to the inner lining of the intestine. With significant amounts of bleeding, before treating erosions in the rectum, patients are prescribed blood-replenishing therapy. Cases of extensive intestinal erosion are treated in a hospital setting. During the acute period of the disease, patients are advised to remain in bed.
An important part of therapy is normalization of nutrition. The diet involves avoiding foods that are irritating to the intestinal mucosa: fried, smoked, spicy, salty, fatty foods. In acute forms of the erosive process, it is also recommended to exclude fresh vegetables and fruits from the diet. The priority in nutrition is warm, low-fat, semi-liquid dishes prepared by boiling in water or steaming. You should eat in small portions up to 6 times a day, chewing food thoroughly and slowly.
Recommended products include viscous porridges, jelly, vegetable soups, low-fat cottage cheese, dietary meat and fish, steamed omelettes, cheesecakes and curd cakes, dry biscuits, unsweetened compotes.
The diet is complemented by physical therapy: patients are recommended to take sitz baths with potassium permanganate or chlorophyllipt.
Drug treatment methods include anti-inflammatory drugs (sulfonamides and antibiotics, and for cytomegalovirus infection - antiviral drugs). Helminthic infestation is an indication for the prescription of antihistamines. For pain and severe spasms in the intestines, antispasmodics are used. Suppositories and ointments for rectal erosion (for example, Relief) are used to relieve itching, burning and discomfort. Suppositories for rectal erosion with methyluracil accelerate the healing of mucosal defects.
The restoration of the integrity of the mucous membrane is also facilitated by therapeutic microenemas with sea buckthorn oil, collargol and colibacterin.
Multiple bleeding erosions are treated with laser cauterization or diathermocoagulation. With late diagnosis, erosions can become infected, which leads to the development of complications in the form of paraproctitis and scarring of the intestinal wall. In such cases, surgical treatment is usually resorted to.
Treatment methods for proctitis
Treatment of proctitis includes the use of medications, diet and physical therapy. In case of complications, surgical treatment is performed.
Drug therapy
Treatment for proctitis involves the use of antibacterial therapy. Antibiotics are prescribed depending on what infection caused the inflammation.
Typically, patients are also prescribed medicinal enemas and baths. For this purpose, decoctions of medicinal herbs are used to relieve irritation in the intestines, eliminate inflammation and have an antiseptic effect. Rectal suppositories are also used.
Antispasmodics and antihistamines are used to relieve pain and spasms.
Diet correction
If you have proctitis, you should follow a special diet. Food should not be fatty, salty, hot, spicy or sour. In case of exacerbation, it is necessary to avoid eating fresh fruits and vegetables. Alcohol should not be consumed during illness.
Physiotherapy
For patients with proctitis, prolonged sitting is contraindicated: this leads to weakening of the pelvic muscles and congestion in the pelvis and legs. To speed up recovery, it is recommended to perform a set of exercises prescribed by your doctor.
More information about the treatment method
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
Popular questions about rectal erosion
How to diagnose the disease yourself?
Diagnosis of rectal erosion includes laboratory and instrumental research methods, so independent diagnosis of the disease is impossible.
How long does it take to treat intestinal erosion?
The duration of therapy depends on the form of the disease, its root cause and the general condition of the patient’s body and differs for each specific case.
Is it possible to cure rectal erosion?
A properly selected therapeutic regimen, adherence to diet and other recommendations of the attending physician can cure rectal erosion in most patients.