Malignization: stages, causes of appearance
Malignization is understood as the process during which healthy cells degenerate into cancer cells. Any healthy tissue or tissue of benign neoplasms can be subject to this process.
With malignancy, there is a decrease in the level of cell maturation, changes in cell morphology, disruption of the role and excessively active proliferation of cells, the rapid development of malignant neoplasms, and the development of distant tumor foci.
To identify the process, clinical, diagnostic, instrumental and laboratory studies are used.
Treatment of the resulting malignant tumor involves surgery, therapy, chemotherapy and radiation. Additionally, hormones, immunostimulants and other drugs are used.
The fundamental differences between a malignant neoplasm and a benign neoplasm:
- The level of cell maturation decreases;
- Changes in their morphology;
- Functional activity is impaired;
- Uncontrolled cell division;
- Increase in neoplasm;
- Formation of metastases.
The initial stages of the process do not reveal themselves by symptomatic manifestations, which creates a serious problem in terms of diagnosis and, accordingly, timely initiation of treatment. Carrying out systematic preventive examinations and modern research methods help only partially identify the beginning of the development of the process.
Malignancy can develop in people of different ages, but the likelihood of its occurrence is higher in older people. The lungs, stomach, mammary gland, liver, and large intestine are most susceptible to the process in question.
World statistics show that the prevalence of the process is growing year by year, which is influenced by many factors, for example, an unfavorable environmental situation, increasing life expectancy, bad habits, etc.
Causes and symptoms
The reasons for “starting” the process are very different:
- Chemical carcinogens;
- Ultraviolet radiation;
- Excessive weight gain;
- Poor nutrition;
- Ionizing radiation;
- Viruses;
- Hormonal imbalance;
- Genetic predisposition.
TNM classification
As we have already noted, the initial stages of the process are asymptomatic. Therefore, preventive studies and screening programs play an important role in diagnosing the disease.
Malignancy
The cause of cell malignancy is a combination of several factors, among which experts indicate chemical carcinogens, environmental features, some viruses, hormonal imbalance conditions, age, bad habits and unfavorable heredity. When conducting research, it was found that malignancy can be provoked by more than 2000 different chemical substances, however, the degree of their influence on the processes of malignant degeneration of cells can vary greatly.
The list of chemical compounds that certainly cause cell malignancy includes polycyclic aromatic hydrocarbons (sources include transport, industrial enterprises and heating systems), nitrosamines (found in cigarettes, some types of beer and amidopyrine), hydrazine derivatives (included in herbicides and some medicinal products). products), asbestos and other mineral fibers (sources from industrial production), as well as some metal compounds.
The most significant physical factor of malignancy is solar radiation, the level of which directly affects the likelihood of developing skin cancer. The lighter the skin and hair and the longer a person is exposed to sunlight, the higher the risk of developing melanoma, basal cell carcinoma and squamous cell skin cancer. In addition, malignancy can be stimulated by ionizing radiation, which provokes the occurrence of leukemia, bone tumors (radioactive strontium) and thyroid cancer (radioactive cesium and iodine).
It has been proven that the likelihood of malignancy increases when cells are exposed to certain viruses, in particular the ATLV virus (causes leukemia), the Epstein-Barr virus (provokes the development of Burkitt's lymphoma), the human papilloma virus (plays a role in the occurrence of cervical cancer) and the herpes virus Type II. Malignancy is also promoted by hormonal imbalances. Hormones can directly provoke malignancy, act indirectly on cells by stimulating their proliferation, have a negative effect on the immune system and change the metabolism of certain carcinogens.
Genetic predisposition plays a significant role in the process of malignancy. Many hereditary diseases with a high probability of malignancy have been described, for example, systemic intestinal polyposis, in which most patients develop colon cancer by the age of 40-50, or Down's disease, in which the risk of developing leukemia is 11 times higher than the population average. There is a connection between malignancy and congenital malformations.
A relationship is revealed between the likelihood of malignancy in the tissues of certain organs and the gender of the patient. Men are 2.4 times more likely to suffer from eye tumors, 2.1 times more likely to suffer from stomach tumors, 2 times more likely to suffer from malignant lesions of the nasopharynx, and 1.7 times more often to suffer from bone tumors. In women, malignancy of thyroid tissue is detected twice as often. The first place in prevalence in men is occupied by tumors of the respiratory tract, in women - tumors of the genital organs and breast. In most cases, the likelihood of malignancy in patients of both sexes increases with age, but some types of neoplasms are more often detected in children or young adults.
Some of the habits that have the greatest impact on cell malignancy include smoking, poor diet and alcohol intake. Smokers are 11 times more likely to develop lung cancer; tumors of the oral cavity, larynx and pharynx – 7 times more often; bladder neoplasms – 2.2 times more often; pancreatic tumors – 1.7 times more often than in non-smokers. The main dietary habits that increase the likelihood of malignancy are the intake of large amounts of meat, fatty, hot and spicy foods, a tendency to over-salt and the consumption of insufficient amounts of plant fiber. Alcohol itself does not cause malignancy, but acts as an activator, enhancing the impact of other factors.
Staging
Stage one is initialization. The beginning of the process is a genetic mutation in the cell. The constant production of cells in the body is controlled by the immune system, which turns on the mechanism of apoptosis to destroy cells.
Mutational changes affect the genes responsible for the apoptosis mechanism, due to which the mutated cell does not die and continues to divide.
Next comes the promotion stage. Oncogenes are activated, mutated cells divide more and more actively. They develop, mature and begin to perform the functions of the tissue where they are localized.
For the complete occurrence of cancer pathology, a disruption of the process of cellular maturation is necessary, as a result of which the number of atypical cells grows, the tissue where they are localized changes, and a malignant neoplasm occurs.
The instability of mutated cells is characterized by the appearance in the tumor of a predominant clone of cells that forms its basis. Uncontrolled cell division leads to the appearance of other clones. This, by the way, explains why the drugs used to treat the tumor have no effect on it over time.
The last stage is tumor progression. Malignant cells grow into surrounding tissues and organs, spread throughout the body, forming metastases.
Peptic ulcer of the stomach and duodenum in elderly and senile people
Peptic ulcer of the stomach and duodenum is not a rare disease in elderly and senile people. According to our long-term observations, patients over 60 years of age make up about 10% of all patients with peptic ulcer disease. There appears to be no age limit at which this disease can occur (in the literature, for example, there is a description of a 103-year-old patient with a perforated peptic ulcer).
Speaking about peptic ulcer disease in elderly and senile people, it is necessary to distinguish between 2 options for the development of the disease.
It is necessary to distinguish long-term peptic ulcer disease, which first appeared in young and middle age and has retained the periodicity of alternating exacerbations and remissions in elderly patients.
According to various sources, this variant accounts for 30 to 50% of all cases of peptic ulcer disease in the elderly. Long-lasting peptic ulcer (the term “old peptic ulcer” used by some authors seems to us to be stylistically less successful) differs from that in young and middle-aged people only in the higher frequency of combined forms of damage (stomach and duodenum), longer exacerbations and slower scarring ulcerative defect. Clinical picture
Peptic ulcer of the stomach and duodenum, which first appeared in old age, is characterized by a certain unique clinical picture and course. To designate this variant of the development of the disease, we usually use the term “late peptic ulcer”
.
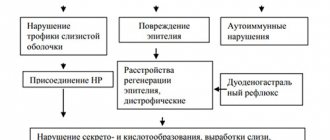
The expression “senile ulcers”, often used in such cases, which generally correctly interprets the essence of the existing changes, can hardly be considered successful from a deontological point of view. In the pathogenesis of late peptic ulcer disease in elderly and senile people, the role of factors that contribute to the weakening of the protective properties of the mucous membrane of the gastroduodenal zone increases.
The importance of these factors (primarily atherosclerotic changes in the vessels of the stomach, reducing the trophism of its mucous membrane) becomes especially noticeable in cases where the disease occurs without the participation of Helicobacter pyloricus (in 20–30% of patients with gastric ulcers). Peptic ulcer disease in such patients often develops against the background of hypertension, coronary heart disease, obliterating atherosclerosis of the vessels of the lower extremities, diabetes mellitus, chronic nonspecific lung diseases, diabetes mellitus and other diseases that contribute to impaired microcirculation in the gastric mucosa.
Late gastroduodenal ulcers (most often localized in the subcardial region and body of the stomach) often occur with a blurred and atypical clinical picture [1]. Pain syndrome and dyspeptic disorders are often very mild. The frequency of pain and its connection with food intake, as well as the seasonality of exacerbations, may be absent. The level of hydrochloric acid secretion in elderly patients with peptic ulcer disease (especially when the ulcer is localized in the stomach) is usually significantly lower than in young and middle-aged patients.
The low-symptom and blurred clinical picture of peptic ulcer disease in elderly people is combined with a more severe course of the disease. This is manifested primarily in the larger size of the ulcer (especially when localized in the stomach) compared to young and middle-aged patients. Thus, according to our data, in more than 1/3 of cases, gastric ulcers in elderly patients are large (more than 2 cm in diameter) or gigantic (more than 3 cm in diameter) in size
. We observed a 70-year-old patient whose stomach ulcer (with very minor clinical manifestations) was 6 cm in diameter. The patient had widespread atherosclerosis (including severe obliterating atherosclerosis of the vessels of the lower extremities) and an atherosclerotic aneurysm of the abdominal aorta, which largely determined the “trophic” genesis of this ulcer.
In elderly patients with peptic ulcers, the incidence of gastrointestinal bleeding (melena) is almost twice as high as in young and middle-aged patients
(observed in more than 1/4 of elderly patients with peptic ulcer).
Iron deficiency anemia (often as a result of hidden blood loss) is detected in elderly patients even more often (according to our data, in 1/3 of cases). Differential diagnosis
When an ulcerative defect in the stomach is detected in elderly and senile people, it is important to confirm the benign nature of the ulcer.
It should be borne in mind that malignancy (malignancy) of a long-existing gastric ulcer is much less common than is commonly assumed (the risk of malignancy of a gastric ulcer in general is not higher than the risk of gastric cancer in a patient who does not have an ulcer). As our own experience and literature data show, the vast majority of malignant gastric ulcers are not represented by malignant benign ulcers, but by the primary ulcerative form of gastric cancer.
The primary ulcerative form of gastric cancer is supported by such signs as short (usually less than 1 year):
1) medical history, 2) localization of the ulcerative defect on the greater curvature of the stomach, 3) very large size of the ulcer, 4) pronounced weight loss and lack of appetite, 5) anemia and accelerated ESR, 6) histamine-resistant achlorhydria,
7) characteristic radiological data (detection of an irregularly shaped “niche” with uneven contours, breakage of the folds of the mucous membrane, rigidity of the stomach wall at the site of the lesion, etc.),
endoscopic signs (irregular shape of the ulcer, uneven edges, tuberous bottom, stepped breakage of the walls of the ulcer crater, infiltration of the mucous membrane adjacent to the ulcer, rigidity and bleeding of the edges of the ulcer, etc.).
At the same time, the infiltrative-ulcerative form of gastric cancer can give an X-ray and endoscopic picture of a benign ulcer, so a final conclusion about the nature of the ulceration can be made only after repeated histological examination of biopsy samples taken from the edges and bottom of the ulcer.
Treatment
Treatment of elderly and senile patients with peptic ulcer disease is based on the generally accepted scheme. If pyloric Helicobacter is detected (by morphological or urease method), anti-Helicobacter therapy is carried out according to one of the schemes for 7 days: proton pump blockers
• omeprazole 20 mg 2 times a day, lansoprazole 30 mg 2 times a day, pantoprazole 40 mg 2 times a day)
• clarithromycin (250 mg 2 times a day)
• metronidazole (0.5 g 2 times a day), proton pump blockers + amoxicillin (1 g 2 times a day)
• metronidazole (0.5 g 2 times a day), proton pump blockers + amoxicillin (0.5 g 2 times a day)
• clarithromycin (500 mg 2 times a day).
The combination of ranitidine-bismuth-citrate (400 mg 2 times a day) with clarithromycin (250 mg 2 times a day) and metronidazole (0.5 g 2 times a day) has also proven itself well. In parallel with eradication therapy, a basic course of antisecretory drugs
(ranitidine 150 mg 2 times a day, famotidine 20 mg 2 times a day or omeprazole 20 mg 1 time a day), lasting in normal cases 4–6 weeks (for duodenal ulcers) and 6–8 weeks (for ulcers stomach).
Due to the often slow scarring of gastroduodenal ulcers in elderly and senile patients, the course of basic antisecretory therapy necessary for complete healing of the ulcer can last up to 10–12 weeks in such patients. antacids
can be prescribed for symptomatic purposes to relieve pain and dyspeptic disorders If successful eradication of Helicobacter pyloricus is confirmed, which is carried out no earlier than 4 weeks after the end of antisecretory therapy, subsequent maintenance of antiulcer drugs is usually not required.
If an elderly patient has a peptic ulcer that is not associated with Helicobacter pyloricus, only antisecretory therapy is performed to heal the ulcer. After achieving scarring of the ulcers, such patients are advised to take daily maintenance antisecretory drugs (H2 blockers or proton pump blockers), most often in half doses, to avoid relapses.
Damage to the stomach and duodenum when taking non-steroidal anti-inflammatory drugs
A separate group consists of ulcerative lesions of the stomach and duodenum resulting from taking non-steroidal anti-inflammatory drugs (NSAIDs)
. These lesions (NSAID gastropathy) represent a very important problem in modern gastroenterology and gerontology. Studies conducted in the USA, Canada, Australia and other countries have shown that 10–20% of elderly and senile people regularly take NSAIDs (acetylsalicylic acid, ketoprofen, indomethacin, etc.) for deforming osteoarthritis, neuralgia and myalgia, spinal osteochondrosis . At the same time, the risk of ulcerative lesions of the stomach and duodenum, caused primarily by inhibition of prostaglandin synthesis in the mucous membrane, is 20–25%. The frequency of hospitalizations in elderly people for gastrointestinal complications associated with taking NSAIDs is 4 times higher than in young and middle-aged patients. If an elderly patient has anamnestic indications of the presence of a previous peptic ulcer, then the risk of developing erosive and ulcerative lesions when taking NSAIDs increases 14–17 times (!) [2, 3].
Gastroduodenal ulcers caused by NSAIDs are often acute, multiple, and clinically manifest as sudden gastrointestinal bleeding (melena or vomiting of contents that look like coffee grounds).
The highest likelihood of ulcerogenic side effects is observed when taking NSAIDs such as piroxicam, ketoprofen, indomethacin, the lowest is when taking ibuprofen.
It must be remembered that ulcerative lesions of the stomach and duodenum can occur even when taking large doses of acetylsalicylic acid (less than 300 mg per day), often prescribed to older people, for example, to prevent complications from coronary heart disease.
In addition, changing the dosage forms of the drug also does not completely eliminate the possibility of NSAID gastropathy.
Treatment of gastroduodenal ulcers caused by taking NSAIDs in elderly people includes, first of all, reducing the dose or completely stopping the non-steroidal anti-inflammatory drug. If its cancellation for some reason is impossible, antiulcer therapy is carried out while continuing to take NSAIDs. At the same time, the healing time of ulcerative lesions naturally increases.
The drugs of choice for the treatment of gastroduodenal ulcers caused by NSAIDs are proton pump blockers, which are prescribed in standard doses
(omeprazole 20 mg per day, lansoprazole 30 mg per day, pentoprazole 40 mg per day). In case of complicated course, multiple nature of ulcers and their large size, slow healing dynamics, as well as if it is necessary to continue taking NSAIDs, the doses of proton pump blockers can be doubled.
Instead of proton pump blockers for the treatment of gastroduodenal ulcers associated with taking NSAIDs, synthetic analogs of prostaglandins (mesoprostol 200 mg 4 times a day) or histamine H2 receptor blockers (ranitidine 150 or 300 mg 2 times a day, famotidine 20 or 40 mg 2 times a day), although the effectiveness of these drugs, as recent studies show, is lower than that of proton pump blockers.
The feasibility of conducting anti-Helicobacter eradication therapy in patients with NSAID gastropathy has not yet been fully determined.
Nevertheless, most gastroenterologists believe that carrying out such treatment (according to one of the given schemes) significantly reduces the likelihood of relapses of gastroduodenal ulcers and increases the resistance of the mucous membrane of the stomach and duodenum to repeated exposure to NSAIDs.
To prevent the development of gastroduodenal ulcerative lesions when using NSAIDs, elderly patients (especially those with concomitant diseases of the cardiovascular system and liver, as well as a history of peptic ulcer disease or receiving anticoagulants) are advised to take proton pump blockers in standard doses
(for example, omeprazole 20 mg per day), mesoprostol (100-200 mg 4 times a day) or histamine H2 receptor blockers (preferably in double doses), as well as carrying out - in cases of detection of Helicobacter pyloric - eradication therapy, which reduces the risk the occurrence of erosive and ulcerative lesions of the mucous membrane of the stomach and duodenum while taking NSAIDs.
An important part of the prevention of gastroduodenal ulcers associated with taking NSAIDs in the elderly is careful consideration of the indications and contraindications for the use of these medications.
In many cases (especially when short-term use of analgesics and antipyretics is necessary), it is advisable to replace NSAIDs with drugs that do not adversely affect the mucous membrane of the stomach and duodenum (paracetamol).
The combination of paracetamol and NSAIDs allows you to reduce the dose of the latter and thereby reduce the risk of ulcerogenic effects. References
1. Brooks P. Use and benefits of nonsteroidal anti-infalammatory drugs. Am J Med. 1998; 104(3A):9S–13S.
2. Griffin MR Epidemiology of nonsteroidal anti-inflammatory drug-associated gastrointestinal injuri.Ibid: 23S–9s.
3. Soll H. Petic ulcer and its complications. Sleisenger & Fordtran's Gastrointestinal and liver disease (Ed. Feldman et al.) 1998; 6th Editon, 1: 620–78
| Applications to the article |
| The low-symptom and blurred clinical picture of peptic ulcer disease in elderly people is combined with its more severe course. |
| A final conclusion about the nature of the ulceration can be made only after repeated histological examination of biopsies taken from the edges and bottom of the ulcer |
| Fig.1. Stomach ulcer |
| Treatment of gastroduodenal ulcers caused by NSAIDs in the elderly includes, first of all, dose reduction or complete withdrawal of NSAIDs |
Stages
If we take the morphological aspect, then the process of malignancy arises and develops as follows:
- An excessive number of structural elements are formed in the tissue (hyperplasia);
- Due to cell division, the tissue grows;
- A benign tumor forms;
- Healthy tissue cells begin to transform into atypical ones (dysplasia);
- A “Cancer in situ” situation arises: the resulting malignant neoplasm does not affect the underlying tissue layers
- The malignant tumor becomes invasive.
Properties of a cancerous tumor
A malignant tumor has a number of characteristics that healthy cells and tissues do not have:
- Rapid growth, which is accompanied by compression or damage to surrounding tissues;
- Germination into surrounding tissues (infiltration);
- Spread throughout the body and formation of new tumor foci;
- Production of toxins;
- “Disobedience” to the immune system;
- High tendency to mutations;
- Significant reduction in cellular maturation;
- Severe cellular and tissue atypia;
- Stimulating the growth of blood vessels.
Therapeutic and preventive measures
Preventive measures include:
- Quitting smoking and drinking alcohol;
- Proper nutrition, which should be balanced in calories;
- Personal protective equipment when working in hazardous conditions;
- Limiting exposure to ultraviolet radiation;
- Adequate physical activity;
- Following the work and rest schedule;
- Systematic examination, including participation in screening programs.
The chances of recovery are significantly increased if the malignant tumor is diagnosed in the early stages.
Surgical manipulations, chemotherapy and radiation therapy are used as methods of treating oncological diseases.
The Onco.Rehab integrative oncology clinic uses a comprehensive approach to the treatment of cancer, in which, in addition to traditional treatment methods, they use hyperthermia, targeted therapy, photodynamic, immunotherapy and other modern methods that have shown to be highly effective.
Treatment and prevention of malignancy
Prevention of malignancy refers to measures similar to those recommended for cancer prevention:
- Quitting bad habits, in particular the use of tobacco and alcohol.
- A balanced diet with adequate calorie content, containing sufficient macro- and micronutrients. Experts recommend paying attention to sufficient fiber intake. It ensures regular bowel movements and, like a brush, collects toxic and carcinogenic substances.
- Use of personal protective equipment when working with harmful production factors.
- Protect from ultraviolet radiation with clothing, sunscreen and glasses.
- Compliance with the work and rest regime, sufficient physical activity.
Timely completion of screening programs. This is a very important point, which has already been discussed above. Screening examination makes it possible to detect patients with malignant neoplasms at an early stage and promptly carry out special treatment.
Oncologists treat cancer. Surgery, radiation therapy and drug therapy are used. For a number of nosologies, enormous results in treatment success have been achieved. For example, many leukemias and lymphomas can be cured permanently, and the same applies to many solid tumors in the early stages. Moreover, the earlier a malignant tumor is detected, the less traumatic intervention is required, and the higher the chances of a complete recovery.
However, even with advanced stages, when there are metastases, it is possible to achieve an acceptable level of quality of life and increase its duration.
Thus, in the federal network of expert oncology clinics “Evroonko” there is an entire pain therapy department. In addition, we work with the most modern treatment and diagnostic technologies, which allow us to solve many problems quickly, minimally traumatic and, most importantly, effectively. Book a consultation around the clock +7+7+78