The gastrointestinal tract system is one of the key systems in the human body. Accordingly, pathological processes affecting the organs of the gastrointestinal tract cause serious harm to human health. Moreover, such diseases differ in their causes, course characteristics, and severity. One of the most severe pathologies of the digestive system is intestinal abscesses. Treatment of intestinal abscesses in Germany is a common reason for coming to us.
At the Vivantes clinic in Germany, diagnosis and treatment of intestinal abscesses are carried out by highly qualified doctors of the first category. The specialists of our gastroenterology department conduct all necessary studies using modern high-precision equipment. Treatment of intestinal abscesses is performed according to the most effective methods of conservative therapy and involves operations of varying degrees of complexity.
What are intestinal abscesses?
Intestinal abscess is a severe pathological process characterized by purulent damage to the intestinal wall. This purulent formation has clear boundaries and an inflammatory nature. In other words, we are talking about a capsule located in the intestinal wall, which is filled with purulent contents.
Purulent abscesses are a dangerous pathology primarily because their contents include many infectious agents and pathogenic bacteria. In case of spontaneous opening of an abscess, the purulent contents pour out into the intestine or into the abdominal cavity, which is a serious threat of large-scale infection, even sepsis.
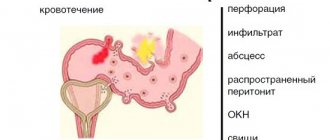
Intestinal abscesses can be single or multiple, and they are also classified depending on the stage of progression. The earliest stage is infiltrative, in which case the risk of rupture is minimal and conservative treatment is possible. If there are signs of intoxication and softening of the infiltrate, urgent surgical intervention is required.
As for the causes of intestinal abscesses, the most common of them are:
- consequences of the operation on the structures of the abdominal cavity;
- progression of transient peritonitis;
- infectious lesion (Escherichia coli, anaerobic flora, staphylococci, streptococci);
- consequences of the injury;
- perforation of the hollow organs of the peritoneum.
The most common types of abscesses are post-operative. Moreover, if pathology occurs in the first days after surgery, there is a high risk of the formation of multiple abscesses. If the neoplasm appears after 1-2 weeks, most likely it will be single.
results
A method has been developed to improve the technique of percutaneous drainage with a stylet catheter under ultrasound guidance by infiltrating the interloop tissue (intestinal mesentery, omentum) with an anesthetic solution. Injecting fluid into the adjacent tissue allows you to increase the space for acoustic access, displacing the intestinal wall, and outline the drainage path, bypassing large vessels and the intestinal wall and thereby avoiding their damage.
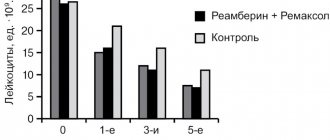
Drainage was performed in 103 patients. The duration of the manipulation was 20±8.2 minutes. In 97 of 103 patients, one intervention was required to adequately drain the cavity. In 6 cases, additional drainage was performed on days 3–11 due to the insufficient effectiveness of primary drainage. In 3 patients, repeated drainage was performed on the 60th day after surgery due to failure of the intestinal anastomosis and failure to close the internal fistula. Cure occurred in 101 (98%) patients within 10–73 days. Mortality rate was 1.9% ( n
=2). A 53-year-old patient died from pulmonary embolism 2 months after undergoing surgery (laparoscopic gastrectomy for stomach cancer, gastric bleeding). The second patient, 74 years old, died due to adhesive intestinal obstruction, which required surgical intervention - laparotomy, adhesiolysis. The course of the postoperative period was complicated by multiple intestinal fistulas, abdominal abscesses, and suppuration of the postoperative wound. In none of the cases was repeated open drainage of the abscess required. In 2 cases of the formation of external intestinal fistulas in the postoperative period, obstructive intestinal resection was required.
The results of dynamic ultrasound and fistulography were analyzed. It was revealed that in 67% the data coincided, which makes it possible to abandon fistulography at the final stage of treatment if the clinical course is positive. Therefore, only ultrasound is sufficient to assess the residual cavity. In addition, ultrasound-guided drainage is an effective independent method of treating abscesses associated with hollow organs without additional interventions to close the fistula.
Symptoms and diagnosis of intestinal abscesses
The clinical picture for this pathological process can vary greatly. In the early stages of progression, the clinical picture of the abscess is similar to the underlying pathology (peptic ulcer, injury, appendicitis). However, with further development, complications arise that are characterized by the following clinical signs:
- symptoms of general intoxication of the body (constantly increasing);
- constant nausea, which is soon replaced by intense vomiting;
- a sharp increase in body temperature to 39°C and above;
- severe pain in the abdominal cavity (corresponding to the location of the abscess).
It is important to understand that if the abscess spontaneously opens, the patient’s condition improves. However, this is only a temporary improvement, followed by extremely serious consequences. For this reason, our clinic’s specialists focus on early diagnosis and pay attention to every nuance.
When starting a diagnosis, the gastroenterologist records all clinical signs, studies the patient’s medical history, and conducts a general examination. After this, laboratory and hardware tests are carried out as soon as possible, among which the most relevant are the following:
- examination and palpation of the abdominal cavity;
- X-ray examination of the abdominal cavity (with contrast);
- sonography;
- computed tomography or magnetic resonance imaging;
- At the same time, blood tests (general, biochemical, coagulogram), general clinical urine examination, coprogram, and fecal occult blood test are performed.
Cryptitis: diagnosis
Diagnosis of cryptitis in the coloproctology department of the Yusupov Hospital proceeds as follows: first, the doctor clarifies all the complaints that the patient has, then his general condition is assessed.
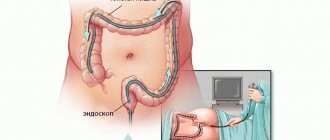
After this, an external examination of the perineal area, perianal area and a thorough digital rectal examination begins, during which the condition of the anal canal is assessed. Then anoscopy and sigmoidoscopy are performed. If necessary, rectal ultrasound, proctography and biopsy are performed (if a tumor process is suspected).
When only the crypt is involved in the process, no changes are usually noted during external examination of the anus. A digital rectal examination in the upper third of the anal canal and palpation in the area of the crypt itself reveals pain and swelling.
When examined through an anoscope, you can sometimes notice swelling and hyperemia (redness) in the area of the crypt, fibrin deposition, and when pressing on the crypt, pus may be released from it. However, unfortunately, with these types of research it is not always possible to see the bottom of the crypt itself.
Using sigmoidoscopy, the doctor can assess the condition of the mucous membrane of the rectum and the closest one - the distal sigmoid colon, and therefore exclude possible other causes of pain and discharge from the anus.
Treatment of intestinal abscesses in Germany
For the most effective treatment of intestinal abscesses, an individual approach is extremely important. Depending on the clinical case, doctors have enough time for conservative therapy or, on the contrary, urgent surgical intervention is required and they must act quickly. Therefore, our specialists compare all available data and pay special attention to physical examination and symptoms.
Conservative
As mentioned earlier, conservative therapy is effective in the early stages. In this case, medications of the latest generations are used, demonstrating high efficiency with a low risk of adverse reactions.
For each patient, all drugs are selected individually, their dosage and period of use are calculated separately. The main groups of drugs are:
- antipyretic drugs;
- antispasmodic;
- Massive antibiotic therapy is mandatory;
- probiotics.
Surgical
Surgical interventions are more relevant in late and intermediate stages, when there is a risk of abscess rupture and complications. To carry them out, highly qualified surgeons are involved and modern equipment is used. The choice of surgical method depends on the location of the abscess and a number of other factors.
The main direction in the surgical treatment of abscesses is drainage and aspiration of purulent contents. The following methods can be used for this:
- through transrectal access;
- through transthoracic access;
- through transabdominal access;
- through midline laparotomy.
4.Treatment
Antibiotic therapy, which is usually very powerful and effective against a wide range of pathogens, in the case of a confirmed abdominal abscess is mandatory, but is still of an additional nature: the abscess itself cannot be cured with medications alone. It is necessary to surgically open the purulent capsule and drain its contents. Antibiotics serve only as a preventive “cover” before surgery (if there is time for any preoperative preparation) and during the rehabilitation period. The main task is to prevent spontaneous opening of the abscess with the spread of pus, teeming with infectious agents and toxins, in the visceral (internal) space. In prognostic terms, the time factor is critically important: timeliness of seeking help, promptness and accuracy of diagnosis, adequacy of measures taken (if necessary, urgently). A lot also depends on the general condition of the patient, the presence of background and concomitant diseases (for example, cardiovascular, nephrological, etc.), localization of the abscess, etc. It is impossible not to take into account that the mortality rate of abdominal abscesses is very high and, according to various sources, reaches from 10 to 40 percent of all registered cases. Therefore, it would not be amiss to once again recall what seems to be known to everyone, but is still often ignored. There are no “trifling” symptoms in the abdominal cavity, and the purulent infectious-inflammatory process here will not “go away by itself”; This is one of those cases about which they say: delay is like death. If the symptoms described above appear, you should consult a doctor as soon as possible.
Prof. Dr. Hans Cherubl
Gastroenterology and gastrointestinal oncology
Head of the Department of Internal Medicine, Gastroenterology, Gastrointestinal Oncology and Infectious Diseases
Specialization
- Gastroenterology
- Infectious diseases
- Diabetes
- Endoscopy
- Cirrhosis of the liver
- Neuroendocrine and carcinoid tumors
- Liver cancer
- Interventional treatment of the liver and biliary tract
- Gastrointestinal oncology
Show doctor's personal profile
Reasons for the development of the disease
The root cause of the disease is infection (Escherichia coli, staphylococci, streptococci) that enter the cellular space from the rectum. Any wounds, household injuries and microtraumas, surgery on the mucous membrane are the entrance gates for such infections.
Staphylococci and streptococci penetrate into the cellular space not only through cracks in the rectal mucosa. There is an internal path: caries, sinusitis or any other source of sluggish (chronic) infection. With the flow of blood and lymph, pathogens from the epicenter of inflammation are transferred to other organs and tissues.
Another way pathogens penetrate the cellular space is by blocking the anal gland duct.
The appearance of the disease is favored by poor nutrition, a sedentary lifestyle and the presence of low-grade inflammatory processes. Additional aspects that increase the risk of the disease:
- weakened immune system;
- diabetes;
- vascular atherosclerosis;
- anal intercourse;
- fissures in the anus.
In particularly severe manifestations of the disease, inflammation can affect several areas located near the intestines.
Prof. Dr. Martin K. Kuhlmann
Nephrology, arterial hypertension and diabetology
Head of the Nephrology Department
Specialization
- Certified doctor of the highest category in the field of general therapy, nephrology and diabetology
- Hypertension specialist (DHL)
- Specialization in areas: All types of renal replacement therapy (hemodialysis, peritoneal dialysis, apheresis, transplantation)
- Acute renal failure
- Prevention and treatment of chronic renal failure (CRF)
- Diet for kidney failure
- Diagnosis and treatment of secondary arterial hypertension
Show doctor's personal profile
What it is?
Paraproctitis is an acute or chronic inflammation of the perirectal tissue. This is one of the most common proctological diseases (20-40% of all rectal diseases). Paraproctitis is in 4th place in frequency after hemorrhoids, anal fissures and colitis.
Men get sick more often than women. This ratio ranges from 1.5:1 to 4.7:1. Paraproctitis is a disease of adults: descriptions of rectal fistulas in children are rare.
Dr. Frank Job
Preventive medicine
Director of the Center for Preventive Medicine – ViPC
Specialization
- The examination clinic covers the full range of advanced diagnostic and therapeutic services in the field of internal medicine and cardiology in close collaboration with all Vivantes International Care specialists.
- The personalized care team provides expert medical advice, diagnosis and therapy for patients with chronic or unclear diseases throughout the field of internal medicine.
Show doctor's personal profile
Classification
Forms of pathology:
- according to the depth of the pathology - superficial, deep;
- along the course - acute (first formed) and chronic (formed fistulas);
- in relation to the fistula to the anal sphincter - intra-, extra- and transsphincteral;
- according to the complexity of the structure of the fistula tracts - simple and complex (presence of several tracts, leaks and purulent pockets);
- according to the presence of a fistula exit - incomplete (there is only an entrance through the anal crypt) and complete (the abscess has found its way out through the skin, into the abdominal space or into the lumen of the rectum);
- according to the localization of purulent foci - subcutaneous, submucosal, intrasphincteral (located between the fibers of the external and internal sphincter), ischiorectal (the abscess is located in the perineum, outside the anal sphincter), pelviorectal (high location, high threat of total purulent process).
Prof. Dr. Ulrich Böcker MA
Gastroenterology – Oncology Center
Head of Therapeutic Department – Gastroenterology and Diabetology
Specialization
- Internal medicine
- Gastroenterology
- Hepatology
- Infectious diseases
- Interventional endoscopy
- Inflammatory bowel diseases
- Viral hepatitis, chronic liver diseases, liver cirrhosis
- Acute and chronic pancreatitis
- Diabetology
- Gastrointestinal oncology
Show doctor's personal profile
Cryptitis: symptoms
If you have cryptitis, you will likely experience signs or symptoms caused by a bowel disease such as ulcerative colitis or infectious colitis.
Symptoms associated with cryptitis may include:
- abdominal pain;
- diarrhea;
- fever;
- chills;
- bloody stool;
- flatulence;
- bloating;
- constipation;
- loss of appetite;
- frequent need for urgent bowel movements.
Treatment of chronic paraproctitis
If the patient is diagnosed with chronic paraproctitis, then the formed fistula will need to be excised. But during active purulent inflammation of the paraproctitis fistula, surgical intervention is contraindicated, so doctors first open the abscesses, clean them of contents and drain them - after which they can proceed with the operation.
If there are infiltrated areas in the fistula canal, then doctors first carry out antibacterial therapy using physiotherapeutic methods. But the operation to remove the fistula must be carried out as quickly as possible after preliminary treatment - relapse with purulent inflammation is inevitable.
Important: old age, severe somatic diseases and closure of fistula tracts are contraindications for surgical treatment of chronic paraproctitis. Doctors must first stabilize the patient’s condition and only then refer him for surgical treatment.
Serous-fibrinous and serous peritonitis
Serous-fibrinous peritonitis is a pathology based on the inflammatory process of the peritoneal layers, accompanied by the accumulation of serous-fibrous exudate in the peritoneal cavity. The disease is characterized by severe pain in the abdominal cavity, tension in the abdominal muscles, nausea, vomiting, upset stool, increased body temperature and deterioration in the general condition of the patient.
Serous peritonitis is an inflammatory process in which serous exudate is observed in the abdominal cavity.
The main cause of the development of all peritonitis is infection of the peritoneal layers as a result of bacterial microorganisms entering the abdominal cavity.
The main reasons for the development of peritonitis are:
- Acute or chronic appendicitis;
- Blunt and penetrating traumatic injury to the abdomen;
- Acute inflammatory processes of the internal female genital organs;
- Perforation in the gastrointestinal tract of ulcerative formations;
- Damage to the intestinal walls or bile ducts.
Among the bacterial microorganisms that can cause the development of peritonitis, both gram-negative and gram-positive bacteria are noted. In this regard, the selection of antibacterial therapy becomes significantly more complicated.
Based on the mechanism of pathogenic flora entering the abdominal cavity, peritonitis is divided into two types: primary and secondary.
Primary peritonitis develops when infection spreads from other foci of infection in the body.
Secondary peritonitis is a complication of local diseases of the gastrointestinal tract.
Local serous-fibrinous/serous peritonitis
Local peritonitis is an inflammatory process of the peritoneum, limited to a specific area and localized around the organ that is the cause of the pathological process.
Local serous-fibrinous peritonitis occurs due to the development of adhesions and the ability of the peritoneum to limit the inflammatory process. Most often, local serous peritonitis is closely associated with an acute disease of one or another abdominal organ (stomach, duodenum, gallbladder, segment of the small or large intestine, pelvic organs, kidneys).
The main reason for the development of such peritonitis is perforation due to peptic ulcer of a hollow organ (stomach, duodenum, ulcerative colitis, gangrenous appendicitis, etc.). Local inflammatory processes in the abdominal cavity occur much more easily than generalized peritonitis; in some cases, patients even remain able to work. However, even with this course of the disease, untimely diagnosis and treatment can lead to a destructive process and the formation of abscesses in the abdominal cavity.
Clinical picture
To make a diagnosis, the doctor needs to collect a detailed history of the disease. Most often, patients with serous-fibrinous peritonitis report the following complaints:
- Abdominal pain, the localization of which depends on the source of inflammation;
- Nausea;
- Vomiting (possibly mixed with bile and contents of the large intestine);
- Suffering face;
- Pale skin;
- Cold sweat;
- Immobility;
- Forced position of the body (on the back or on the side with the legs brought to the stomach);
- Increased body temperature;
- Drop in blood pressure;
- Impaired consciousness (as the patient’s condition progresses);
- Pointed facial features;
- Yellowish tint of the skin and mucous membranes;
- Bloating.
Diagnostics
Making a diagnosis of serous fibrinous peritonitis is associated with certain difficulties, so this process should only be carried out by a qualified doctor. At the Yusupov Hospital, specialists every day encounter various emergency conditions that require immediate diagnosis and treatment. The hospital has innovative equipment that is successfully used for diagnostic purposes to obtain results as quickly as possible.
After collecting anamnestic data, to complete the examination, doctors use:
- Palpation and auscultation to determine the characteristic symptoms of the disease. When listening to bowel sounds, it is due to the accumulation of free fluid in the abdominal cavity. Noises are usually weakened or completely absent.
- X-ray examination of the abdominal organs. A characteristic sign of a subphrenic ulcer is the presence of a layer of air. A specific symptom of “cups” is with intestinal obstruction.
Diagnostics
For diagnosis, as a rule, it is sufficient to collect complaints, anamnesis of the disease and an external examination. In rare cases, especially with a deep location of the abscess, there may be difficulties in differentiating the diagnosis. Then instrumental research methods may be required, for example, computed tomography or ultrasound with a rectal sensor.
In the presence of fistulas, fistulography is performed - staining of the fistula tract to determine its depth, length and direction of the tract.
Laboratory research methods determine the presence of inflammation.
Purulent peritonitis: symptoms of the disease
Purulent peritonitis is an inflammatory lesion of the peritoneum, which occurs with the participation of pyogenic flora. This is an infectious nonspecific or specific lesion that occurs as a result of acute surgical pathologies or trauma to the abdominal organs.
Most often, the development of acute purulent peritonitis is associated with the following reasons:
- Violation of the integrity of the wall of the abdominal organ and the entry of its contents into the peritoneum (most often with gangrenous-perforated appendicitis, perforation of a stomach and duodenal ulcer, perforated cholecystitis, damage to the intestine by a foreign body, rupture of a diverticulum of the stomach or intestine, with germination of the wall of the stomach or intestine with a tumor development of perforation);
- The transition of inflammation from the source of infection to one of the sheets of the peritoneum without violating the integrity of the organ (with phlegmonous appendicitis, inflammatory gynecological disease, purulent cholecystitis, pancreatitis);
- Injuries to the abdominal organs. If the integrity of the organ is violated during or after surgery (purulent peritonitis after surgery occurs if the rules of asepsis and antisepsis are not followed, postoperative care of the patient is disrupted);
- Contamination of organs with several types of bacteria (staphylococci, streptococci, E. coli, enterococci, Proteus, Pseudomonas aeruginosa, clostridia, pneumococci, Mycobacterium tuberculosis, Neisseria gonorrhea).
The onset of acute purulent peritonitis is characterized by symptoms of the underlying disease, and later specific symptoms of inflammation of the peritoneum are added. The main symptoms are:
- Abdominal pain (has a precise localization, very intense, intensifies with any physical activity, sneezing or coughing). If the intensity of pain decreases or completely disappears against the background of deterioration of the condition, then this is a poor prognostic sign, as it indicates necrosis of the peritoneum and its nerve endings;
- Nausea, vomiting (first with stomach contents, and then with intestines and fecal contents). This condition is associated with intestinal paresis;
- Dehydration;
- Severe flatulence (due to intestinal paresis);
- Forced position of the patient on his side with his knees pulled up to his chest (as a result, the tension of the peritoneum decreases);
- Dryness and pallor of the skin, possible marbled pattern, acrocyanosis (cyanosis);
- Cold and wet extremities;
- Coating of the tongue with a dirty gray coating;
- Bad breath;
- Tachycardia, increased blood pressure;
- Anxiety, feeling of fear;
- Increased breathing rate;
- Multiple organ failure (due to severe water-ion deficiency). Manifested by confusion up to the point of coma, development of convulsions;
- Increased peristalsis (contraction of the intestinal walls);
- Dark brown urine (with dehydration and intoxication);
- Gas and stool stop passing.
When palpating the abdomen, pronounced tension in the abdominal muscles occurs (the abdomen becomes board-shaped), a positive Shchetkin-Blumberg sign (when pressing on the abdominal wall, severe pain is noted, which intensifies when the hand is suddenly removed). Tympanitis (a ringing sound characteristic of a large amount of gas) is detected upon percussion. In some places there is a dullness of sound (with effusion in the abdominal cavity). In the later stages of purulent peritonitis, the sound of splashing and the sound of a falling drop can be heard.
Diagnosis of purulent peritonitis
If the development of purulent peritonitis is suspected, diagnostic measures should be carried out very quickly, since surgery performed on the first day guarantees recovery in 95% of cases. Patients are urgently advised to:
- Ultrasound diagnostics of the abdominal organs (distended intestinal loops, effusion into the abdominal cavity, peristalsis state are visualized);
- Survey radiography of the abdominal organs (intestinal arches, darkening in certain places, indicating the presence of fluid, levels of pathological contents are revealed);
- Multislice spiral computed tomography (it is possible to examine the abdominal organs in detail, the presence of effusion);
- Consultation with an endoscopist (for the purpose of diagnostic laparoscopy). Thanks to this method, the source of development of purulent peritonitis, the inflammatory process, and purulent-fibrinous effusion are visible. The data obtained is sent to the laboratory to determine the sensitivity of microflora to antibiotics;
- Complete blood count (leukocytosis, anemia, thrombocytopenia);
- Biochemical blood test (decrease in sodium, potassium, chlorine levels).