Peritonitis is a deadly inflammation of the membrane lining the abdominal cavity and surrounding the internal organs located in the abdominal area - the peritoneum. In the absence of qualified medical care, the patient’s condition is rapidly deteriorating, and every hour it will become increasingly difficult to guarantee that he will be able to save his life.
Various factors can lead to the development of an inflammatory process in the abdominal cavity in a person, for example:
- perforation of the gallbladder, which can be a consequence of acute cholecystitis and is accompanied by the pouring of the contents of this hollow organ into the abdominal cavity;
- lack of treatment for pancreatic inflammation;
- rupture of an inflamed appendix;
- perforation of the wall of the stomach or duodenum due to the lack of effective treatment for an ulcer of this organ;
- blockage of the intestine and the spread of its pathogenic microflora into the abdominal cavity, etc.
The likelihood of developing all kinds of health problems after peritonitis, including disability and, in extreme cases, death, is very high. Therefore, when the first signs appear that may indicate that the patient has inflammation of the peritoneum, you should immediately seek qualified medical help - after all, it may not even be hours, but minutes. The recovery process after peritonitis also involves monitoring the patient by the attending physician.
Peritonitis - what kind of disease is it?
Peritonitis is an inflammatory process that develops in the peritoneum and can occur locally or diffusely. Let's take a closer look at what abdominal peritonitis is. In fact, peritonitis is not an independent disease - it is rather a serious complication of inflammation of the organs that line the peritoneum. The peritoneum is a serous covering of organs inside the abdominal cavity, formed by two layers of connective tissue: parietal (parietal) and visceral. Between the peritoneum and the walls of the abdomen there is a layer of connective tissue, in which there is adipose tissue of varying degrees of severity - preperitoneal tissue.
There is no fiber in the area of the diaphragm, but on the posterior wall of the abdomen it is most developed, and covers the ureters, kidneys and adrenal glands, the abdominal aorta and the inferior vena cava with its branches. Anatomically, the cavity formed by the peritoneum is divided into three sections: upper, middle and lower. The upper one is bounded below by the mesentery of the transverse colon, and above by the diaphragm. The middle one extends between the colon and the entrance to the pelvis. Lower - within the pelvis. The inflammatory process can develop in any of them. In this article we will look in detail at the symptoms of peritonitis in adults, causes and treatment.
Therapy before hospitalization
Patients should be treated before hospitalization. Because of this, emergency doctors and local family doctors are obliged to determine the clinical manifestations of peritonitis, homeostasis disorders that arise in the case of widespread peritonitis, and not to make a mistake in assessing the general condition of the patient. Patients should be sent to a specially equipped department. If the infection is severe and hemodynamics are impaired, resuscitation measures should immediately begin, which do not stop while the patient is being transported to the hospital. Administered intravenously:
- rheopolyglucin,
- rheosorbilact,
- reforman,
- Ringer-Locke, Darrow,
- five percent solution of glucose and insulin (1 unit of insulin per 5 g of dry glucose),
- cardiac glycosides (1-2 ml of 0.025% digoxin solution or 1-2 ml of 0.02% celanide solution, which is previously dissolved in 10 ml of 5% glucose solution),
- vitamins,
- 100-150 mg hydrocortisone,
- antiallergic drugs.
The patient must be transported in a semi-sitting position. If there is vomiting, you need to insert a permanent tube into the stomach cavity to remove the contents. Under no circumstances should painkillers, narcotics or antispasmodics be administered.
Causes of pathology
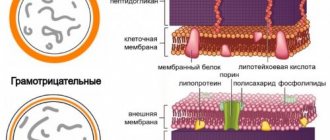
The root cause of the inflammatory reaction in the tissues of the abdominal cavity, which leads to peritonitis, in most cases is a bacterial infection (caused by microflora located in the digestive tract). The following gram-negative and gram-positive microorganisms can provoke this complication:
- streptococci;
- staphylococci;
- bacteroides;
- clostridia;
- Pseudomonas aeruginosa;
- peptococci;
- Proteus;
- enterobacter;
- eubacteria;
- fusobacteria.
In the vast majority of cases - according to various statistical data, 60-80% - inflammation of the peritoneum is caused not by one, but by an association of microbes. More often, this pathological process is provoked by E. coli or staphylococci. In more rare cases, the development of peritonitis is caused by pathogens such as pneumococcus, Koch's bacillus (Mycobacterium tuberculosis), gonococcus and hemolytic streptococcus. Considering the above-described facts about the variability of possible pathogens of peritonitis, when prescribing treatment, the doctor must wait for the results of an analysis of the sensitivity of pathogenic microflora to antibiotics.
Lethal outcomes from inflammation of the peritoneum can reach significant values - according to statistics, in gastroenterological diseases, death from such a complication occurs in 20-30% of patients, and in severe illnesses this figure reaches 40-50%. We may recall that it was traumatic peritonitis after an injury to the abdominal cavity that caused the death of A. S. Pushkin.
Causes of peritonitis
Among the main causes of peritonitis are:
Inflammatory diseases of various organs located in the abdominal cavity - cholecystitis, pancreatitis, appendicitis, salpingitis.
Perforations in the gastrointestinal tract (stomach, intestines, gall bladder, etc.), which can act as complications of gastric or duodenal ulcers, appendicitis, destructive cholecystitis, ulcerative colitis, and malignant diseases. This leads to the fact that the contents of the stomach, gall bladder, and bladder (hydrochloric acid, bile, urine, blood) enter the free abdominal cavity, which causes irritation and then inflammation.
The infection enters the circulatory or lymphatic system (hematogenous and lymphogenous pathways), which leads to the spread of pathogenic microflora throughout the body, and accordingly, affects the abdominal cavity. This can occur with direct infection of the body, or secondarily, when the infection enters the blood from boils, carbuncles and other infectious foci on the skin.
Injury to the abdominal organs, or the abdomen itself - development occurs during injuries, after surgical treatment.
Other reasons include:
- Rupture of appendicitis;
- Ultra-high distension of the intestine with intestinal obstruction;
- Necrosis of the gastrointestinal tract;
- The presence of ulcers in lymphoid plaques during typhoid fever;
- Excessive production of serous fluid in the abdomen or disruption of its circulation (ascites);
- Internal bleeding and others.
The most common pathogens of peritonitis are bacteria - staphylococci, streptococci, pneumococci, Escherichia coli, Enterobacter, Enterococcus, Eubacteria, Peptococcus, Clostridia, Proteus, Fusobacteria, Bacteroides, Mycobacterium tuberculosis.
Quite often, inflammation of the peritoneum is caused by the association of several types of infection simultaneously.
Laboratory and instrumental diagnostics
Typically, peritonitis is a complication of any diseases or injuries of the abdomen, therefore, at the beginning of the development of the disease, the symptoms of the underlying disease (against which peritonitis developed) come to the fore. Laboratory research methods:
- A general blood test (to identify possible anemia (“anemia”, a decrease in the content of erythrocytes (red blood cells) and hemoglobin (oxygen carrier protein)), usually there are signs of an inflammatory process (increased ESR, leukocytes (white blood cells)).
- General urine test if infection is suspected.
- Blood and urine cultures are performed to detect infection.
- Biochemical blood test - determination of liver enzymes (special proteins involved in chemical reactions in the body)
Instrumental research methods:
- Ultrasound (US), magnetic resonance imaging (MRI), or computed tomography (CT) to look for pathological (abnormal) changes in the abdominal organs.
- An electrocardiogram (ECG) is a method of recording electric fields that are formed during the work of the heart.
- Survey radiography of the abdominal organs to identify a possible source of peritonitis (“primary focus”).
- Ultrasound of the pelvic organs for suspected inflammation of the pelvic peritoneum (pelvioperitonitis).
- Laparoscopy is an endoscopic examination and surgical intervention on the abdominal and pelvic organs.
- Laparocentesis (puncture of the anterior abdominal wall to obtain exudate (abdominal fluid)).
The prognosis of the disease with timely and adequate therapy is favorable, although postoperative peritonitis has high mortality rates (about 40%).
Types of peritonitis
Peritonitis is classified as follows...
According to the clinical course:
- Acute peritonitis;
- Chronic peritonitis.
By the nature of the exudate:
- Serous - only the usual fluid produced by the serous membrane is present;
- Fibrinous - in the serous fluid there are fibrin fibers that form adhesion processes;
- Purulent - pathological exudate consists of pus;
- Hemorrhagic - pathological exudate contains blood impurities.
By etiology
- Infectious (bacterial) peritonitis - the cause of the disease is infection; — Aseptic; — Special forms:
- Peresitary;
- Rheumatoid;
- Granulomatous;
- Carcinomatous.
According to the nature of infection:
Primary – the infection penetrates the peritoneum by hematogenous (through the blood) or lymphogenous (through lymph) route.
Secondary – infection of the peritoneum occurs due to trauma or surgical diseases of the abdominal organs. Can be divided into:
- Perforated;
- Infectious-inflammatory;
- Traumatic;
- Postoperative.
Tertiary - the development of the inflammatory process occurs when the peritoneum is infected against a background of weakened immunity or exhaustion of the body - after injuries, operations, general pathological conditions due to exposure to adverse factors (frequent stress, hypothermia, hypovitaminosis, vitamin deficiencies, poor-quality nutrition, drug abuse without consultation with a doctor).
By prevalence:
Local - characterized by inflammation in one anatomical part of the abdominal cavity. May be:
- Limited peritonitis - characterized by the formation of abscesses or infiltrate;
- Unbounded – characterized by the absence of clear boundaries of inflammation.
Common - characterized by the formation of 2-5 inflammatory-pathological areas in various parts of the abdominal cavity.
General (total) – characterized by total damage to the peritoneum.
Symptoms of peritonitis in an adult
The severity and symptoms of peritonitis largely depend on the severity of the underlying cause of the disease, infection, localization of the inflammatory process and the patient’s health status. However, let's look at the symptoms of peritonitis in adults and what it means. The first signs of peritonitis:
- Periodic sharp pain in the abdomen;
- Increased body temperature;
- General malaise, weakness;
- Nausea.
The main symptoms of peritonitis:
- Acute pain in the abdomen, especially aggravated by pressing on the anterior abdominal wall;
- Muscle tension in the anterior abdominal wall;
- Increased and high body temperature;
- Nausea, vomiting;
- High blood pressure, which drops sharply after some time;
- Rapid pulse, tachycardia;
- Flatulence;
- Diarrhea with constipation;
- Pallor of the skin, acrocyanosis;
- Increased sweating;
- Dehydration (dehydration);
- Shchetkin-Blumberg symptom;
- Mendel's symptom;
- Franciscus symptom;
- Voskresensky's symptom.
On the part of the circulatory system, hypovolemia develops, which is accompanied by an increase in heart rate, an increase in blood pressure, which soon drops to low values, a decrease in the speed of portal blood flow, a decrease in venous return to the heart, and tachycardia. From the gastrointestinal tract - intestinal atony appears as a reaction to the inflammatory process.
On the part of the respiratory system - disorders appear mainly in the late stages of the development of peritonitis and are characterized by hypoxia, impaired microcirculation in the lungs and their edema, pulmonary perfusion appears, which, in combination with hypovolemia, leads to disruption of the myocardium and lungs. On the part of the liver - disorders are observed in the initial stages of the development of the disease, and are characterized by hypovolemia and hypoxia of liver tissue, which ultimately can lead to degeneration of the parenchyma.
Surgical intervention
Depending on the prevalence of peritonitis, its original source and severity, the surgical technique may differ slightly, however, the general tactics of any surgical intervention are carried out in accordance with a specific scheme - immediately after the patient is admitted to the hospital, they begin to prepare him for surgery. Next, as quickly as possible, you need to start doing the actual operation. After its completion, the recovery period initially takes place in the intensive care unit.
Preparing for surgery
Preparation lasts no more than 3 hours, since a longer delay reduces the patient’s chances of surviving during and after the operation. At this time, intensive infusion therapy is carried out. The purpose of infusion administration of drugs before surgery is to improve the basic vital functions of the body by:
- correction of water-electrolyte balance indicators;
- increased central venous and blood pressure;
- restoration of the amount of circulating blood in the bloodstream;
- decreased heart rate;
- stabilization of diuresis.
If it is not possible to restore kidney function within three hours, the operation is still performed, but this reduces the chances of a favorable outcome for the patient.
In addition, preparation for surgery includes installing a catheter in the subclavian vein to control central venous pressure and conduct infusions. To measure hourly urine output, bladder catheterization is performed.
The gastrointestinal tract also requires preparation measures - it is emptied using a special hollow probe, which is not removed until gastrointestinal motility is restored after surgery.
Progress of the operation
Modern medicine knows several schemes for performing surgery for peritonitis:
- closed: performed laparotomically, with removal of the source, sanitation of the cavity without drainage, and tightly suturing the laparotomy wound;
- semi-closed: classic technique, similar to closed, but with drainage of the cavity;
- laparoscopy using video endoscopic technologies;
- combined: in this case, a classic semi-closed operation is performed with programmed video-endoscopic sanitation of the cavity;
- semi-open: classical scheme in combination with surgical sanitation and temporary closure of the postoperative wound;
- open: performed without temporary closure of the abdominal wall, with surgical sanitation.
Before surgery, general anesthesia is performed if the diagnosis is made before surgery. If peritonitis is detected directly during laparotomy with local anesthesia, the patient is transferred to endotracheal anesthesia.
After the onset of anesthesia, it is necessary to provide access to the source of the pathology. In the presence of widespread peritonitis, a midline incision is made, the location and size of which depend on the source of inflammation. During the operation, if necessary, the incision is enlarged, expanding the boundaries up or down.
If the patient has a preoperative diagnosis of “peritonitis,” access is opened with an incision that is localized within the presumed source of inflammation, for example, an oblique incision is made in the hypochondrium or in the iliac zone. It is important that the length of the penetrating incision is sufficient to ensure complete and reliable sanitation of the source of inflammation.
In the case where local peritonitis was initially suspected, and after a lateral incision a widespread type was discovered, the lateral incision is supplemented by the corresponding median one, through which sanitation is carried out. The lateral one remains for drainage.
After the autopsy, to minimize the morbidity of the operation, the patient is administered novocaine blockade of reflexogenic zones through the root of the mesentery of the small intestine. Typically, a solution of 0.25% novocaine is used in an amount of 200 ml, heated to a temperature of 37 degrees.
The course of the operation begins with an inspection of the cavity to detect the source of peritonitis. Exudate that is found in the cavity is necessarily selected for bacteriological examination. After the effusion is removed from the peritoneum with gauze pads and electric suction, the actual inspection of the cavity begins. If the operation is performed through a lateral incision, the effusion is removed from it immediately after identifying the source of peritonitis.
Based on the results of examining the cavity through a lateral approach, doctors determine the presence or absence of indications for making a median incision and performing a median laparotomy. If the initially suspected source is not detected through the lateral incision, but the diagnosis is definitely confirmed and we are talking about peritonitis, then in the presence of a diffuse form, they immediately proceed to a median laparotomy.
The inspection in search of the source of inflammation takes place strictly in order, through an incision of at least 20 centimeters in length. Initially, the examination begins from the upper floor of the cavity, including checking the diaphragm and pancreas. Next, the doctor examines the lower floor, the pelvis and the retroperitoneal space.
The next stage of the operation is the most important, although not always achievable. We are talking about removing the source of peritonitis. To achieve this goal, the surgeon may:
- remove completely or partially the affected organ (perform an appendectomy, cholecystectomy, resection of part of the intestine), followed by suturing the wall;
- apply fistulas;
- drain the area of inflammation.
The last two options are used if the source of inflammation cannot be removed due to danger to the patient, or due to technical difficulties. In conditions of diffuse, widespread peritonitis, anastomoses between organs are prohibited, since the sutures in this case will be incompetent. If possible, external drainage of organs is performed.
For perforated ulcers and peritonitis, only suturing of the perforated hole is performed. After intestinal resection with diffuse fecal or purulent peritonitis, anastomoses are not applied; it is necessary to apply an end colostomy or ileostomy, if possible removing both knees of the intestine close to or at a minimum distance from each other, so that in the future the restoration of intestinal continuity is easier.
Sanitation during an operation to remove a focus of local peritonitis does not require lavage, as this can provoke the spread of infection further throughout the abdominal cavity. In this case, it is advisable to drain with suction and sterile gauze swabs. Fibrous formations tightly fixed in the peritoneum should not be removed, as this contributes to the destruction of the walls of the organs to which they are adjacent.
If we are talking about diffuse peritonitis, all parts of the abdominal cavity are already infected, so the cavity is washed with 10-12 liters of saline, and then the washing liquids are removed with suction. Rinsing can be repeated several times as necessary, and the last time an antiseptic solution, for example, dioxidine, chlorhexidine, is used.
The duration of the operation to remove peritonitis cannot be predicted in advance, since the real picture of the condition of the peritoneum is revealed to the surgeon only after direct opening of the abdominal cavity.
During the operation to remove widespread peritonitis, complicated by intestinal obstruction or severe adhesions, intestinal drainage may be performed. The most gentle method for the patient is drainage with a Miller-Abbott probe using the nasogastrointestinal method. Particularly important is the drainage of the initial section of the jejunum to a length of up to 70 centimeters. Complete drainage of the stomach is achieved by leaving a separate end of the tube.
Drainage of the abdominal cavity is one of the final stages of the operation. Drainages are necessary to ensure adequate drainage of exudate. Counter-openings are made in the iliac and subcostal regions.
Possible consequences of the operation
Penetration into the abdominal cavity when removing the focus of peritonitis practically does not pass without consequences. Often, patients in the postoperative period develop one or more complications, which are observed and treated in the hospital. For example, postoperative consequences caused by surgeon errors include:
- necrosis of the remaining part of the intestine if it has undergone a destructive change: in this case, relaparotomy with resection of this area, subsequent sanitation and drainage is indicated;
- unjustifiably economical resection of a section of intestine that has undergone necrosis;
- failure of the anastomotic sutures: this requires relaparotomy, intestinal decompression and the application of a fistula to the intestine, then removal of the intestinal loop and drainage of the cavity.
In addition, if asepsis requirements are not observed during or after surgery, there is a high probability of infection in the suture. This consequence of the operation is easy to detect - the suture swells and turns red, begins to hurt, and after a day or two pus begins to ooze from it. Against this background, signs of a disturbance in general health develop: fever, weakness, chills.
Approximately 1 patient out of 100 people may develop repeated, so-called tertiary, peritonitis. People with an exhausted body, an insufficiently balanced diet, weak immunity, and also after long-term antibiotic therapy are especially susceptible to it. In this case, the operation must be repeated.
Intestinal paresis is the complete loss of motor ability. If normally the intestine moves food masses along its length due to its own peristalsis, then with paresis such movement becomes completely impossible. This complication often occurs after diffuse peritonitis, as well as after prolonged operations. The patient has total constipation and severe bloating.
The formation of adhesions is a typical complication after operations for peritonitis. It is provoked by any violation of the integrity of the peritoneum, since, in fact, the formation of adhesions is a protective reaction of the body. In this case, adhesions are strands of connective tissue that connect the intestinal loops, causing complete or partial obstruction. Possible formation in the late postoperative period. To solve the problem, most often, a repeat operation and surgical dissection of the adhesions are needed.
How is peritonitis diagnosed?
Signs of peritonitis depend on the stage of development of the process, of which there are three:
- Reactive (up to 24 hours): the reaction to irritation of the peritoneum increases. Characteristic severe pain, the localization of which depends on the location of the inflammatory process. They can radiate to various parts of the body. Intoxication at this stage is usually mild.
- Toxic (24-72 hours): pain becomes diffuse, intoxication increases, sometimes to the point of shock.
- Terminal (after 72 hours): depletion of compensatory mechanisms and the development of severe disturbances in the functioning of many organs and systems. The pain at this stage subsides, which is associated with paralysis of the nerve endings.
Already from the first stage, in addition to pain, nausea and vomiting appear, first reflex, then due to intestinal paresis. The first portions of vomit contain the contents of the stomach, the subsequent portions contain bile and feces. Gradually, as a result of paresis, intestinal obstruction develops. Usually, examination, palpation and percussion of the abdomen are sufficient for a doctor to diagnose peritonitis. The diagnosis is confirmed by positive peritoneal symptoms (symptoms of peritoneal irritation):
- Shchetkin-Blumberg: the anterior abdominal wall is pressed with the hand, and when it is removed, severe pain appears;
- Mendel: pain in the area of inflammation when tapping over the entire surface of the abdominal wall;
- Voskresensky (“shirts”): pain when quickly running the palm along the anterior abdominal wall (over the shirt).
With percussion, a dullness of sound is determined, with auscultation - a decrease in peristalsis activity. The diagnosis can be confirmed, the localization of the process and the amount of effusion can be determined using x-ray examination methods and ultrasound. A complete blood count reveals signs of inflammation, usually bacterial (neutrophilic leukocytosis and increased ESR). If the diagnosis is in doubt, laparoscopy or laparocentesis may be performed.
Signs of peritonitis
The symptoms of peritonitis are very characteristic, so every surgeon can diagnose it!
Manifestations of peritonitis are due to the reasons that provoked its development. But the main signs of one stage or another are the same in any case.
Reactive stage
This is the first stage, it occupies the first day of the disease. The lesions are local in nature. Patients first feel sharp pains that appear unexpectedly. In this case, you can accurately determine the place where the pain comes from. Some compare the pain at this stage to the blow of a dagger.
The localization of pain is associated with the organ that became the source of the disease. For example, with appendicitis, pain will be felt in the inferolateral zone on the right. If this is a perforation of a stomach ulcer, then pain will appear in the left hypochondrium or in the epigastric region. The pain is felt strongly, and it gradually spreads.
Self-diagnosis methods
Peritonitis has a clear clinical picture. The manifestations of peritonitis are difficult to separate from the underlying disease, but it is worth noting that one of the main symptoms of peritonitis is severe pain. The pain spreads throughout the abdomen and increases. 1-2 hours after the onset of the attack, the pain subsides for a while before becoming more intense.
The infection in the peritoneum spreads quite quickly, and since the peritoneum is a well-absorbing tissue, symptoms of general intoxication increase - tachycardia, severe weakness, fever.
With peritonitis, the functioning of all organs of the abdominal cavity is disrupted, primarily the intestines, which is manifested by nausea, vomiting, and bloating.
Multiple organ failure develops. Without treatment, the prognosis is always poor. Suspicion of peritonitis is an indication for emergency hospitalization in a surgical hospital. The earlier the patient sought medical help from the onset of the disease and the earlier the diagnosis was made and treatment started, the more favorable the prognosis of the disease.
Symptoms and manifestations
In the case of acute pancreatitis, significant symptoms appear. But at the same time, a situation is possible when no signs of damage to the peritoneum are detected, the temperature does not rise during the first stage of the illness, although the patient suffers from incessant vomiting, girdle pain, and sluggish bowel sounds are auscultated throughout the entire abdominal area. The amount of diastase in the urine and blood increases greatly.
At an early stage, clinical signs of peritonitis and acute mechanical intestinal obstruction can be distinguished. When peritonitis develops, the differential diagnosis of these diseases is difficult. But it is important to remember that in the first case the pain is constant, and in the second it is felt as intense attacks. Noises in the intestines during obstruction first intensify, and a visible wave-like contraction of the walls is detected.
With hepatic colic, the patient feels attacks of pain under the right rib, usually radiating to the right shoulder blade, and suffers from vomiting a small dose of stomach contents with a certain amount of bile. After using antispasmodic drugs, the attack of the disease is interrupted.
If a peptic ulcer worsens and penetrates the pancreas, then continuous severe pain is felt in the abdominal area. In this case, protective tension of the abdominal muscles, Shchetkin-Blumberg symptom, and normal bowel sounds are not observed. The temperature does not rise or fall, the heartbeat is normal, the tongue is not dry.
In the case of renal colic, the patient may feel severe pain in the abdomen, suffer from bloating, constipation, while gases do not pass away in time, the symptoms are similar to acute abdomen, the pain is localized in the lumbar region. It is distinguished from peritonitis by the following characteristics: it occurs in attacks, spreading to the thigh and genitals; when changing body position, the nature of the pain remains unchanged; the patient behaves restlessly; there is no redness of the skin or signs of peritoneal irritation; the number of leukocytes is normal; in the urine - manifestations characteristic of this disease.
Discriminating diagnostics are also carried out with diseases that are not directly related to damage to organs in the abdominal cavity (pneumonia, acute myocardial infarction, basal pleurisy, rib fractures, herpes zoster) and are accompanied by manifestations that are similar to the symptoms of peritonitis. At the same time, it is important to conduct a thorough study of the organs of the chest cavity, using instrumental methods, starting with radiology.
Pathology treatment methods
Treatment of this complication requires immediate hospitalization and, as a rule, emergency surgery. Under no circumstances should the disease be treated on an outpatient basis, since the course of this disease is unpredictable and, in addition to surgical intervention, requires observation of the patient both before and after surgery. Treatment of peritonitis must be timely and comprehensive and consists of several stages:
- preoperative preparation;
- surgical intervention;
- intensive care and monitoring after surgery.
Preoperative preparation. Preparation for surgery should be complete and last no more than 2, maximum 3 hours. Preoperative preparation includes:
- catheterization of the central vein (installation of a subclavian catheter);
- urinary catheterization;
- gastric emptying (removal of gastric contents using a gastric tube);
- massive infusion therapy of colloids and crystalloids of at least 1.5 liters (replacement of circulating blood volume, normalization of microcirculation disorders, fight against metabolic acidosis);
- preparation for anesthesia (premedication);
- administration of antibiotics (drugs are selected empirically before surgery);
- antienzyme therapy;
- normalization of the cardiovascular system;
- maintaining liver and kidney function.
Surgery. Surgical intervention has the following goals:
- eliminate the primary focus that caused inflammation of the peritoneum;
- cleansing the abdominal cavity;
- intestinal decompression;
- effective drainage of the abdominal cavity.
Management of the postoperative period should be carried out under monitoring, be complete and adequate, with a quick change of prescriptions and tactics in the absence of positive dynamics.
Treatment of peritonitis
How to treat peritonitis? Treatment of peritonitis largely depends on concomitant diseases, course, cause, presence of complications and extent of the disease.
Treatment of peritonitis includes:
1. Hospitalization. 2. Surgical treatment. 3. Drug treatment. 4. Diet.
Hospitalization
If peritonitis is suspected, the patient is immediately taken to a medical facility, due to the possibility of rapid development of the disease, the appearance of septic shock and the sudden death of the patient.
Surgical treatment of peritonitis
Surgical intervention (operation) for peritonitis is one of the main points in the treatment of this disease. This is due to the fact that the inflammatory process of the abdominal cavity is almost always accompanied by the presence of adhesions and abscesses that isolate the infectious focus. In addition, neighboring organs can be involved in the processes of adhesion (adhesion). And more about the reason - perforation of the walls of internal organs due to various diseases, after which hydrochloric acid, bile, blood, often infected ones, reach the walls of the peritoneum, in most cases they are the main cause of the development of peritonitis.
Surgery for peritonitis allows you to remove the source of this disease, eliminate perforations, remove abscesses and other pathological processes in the abdominal organs.
To gain access to the abdominal organs, a midline laparotomy is performed.
Among the most commonly used methods of surgical treatment of peritonitis are:
- Suturing the perforated hole;
- Resection of the necrotic area of the intestine;
- Appendectomy;
- Colostomy;
- Decompression of the small intestine (nasointestinal intubation);
- Drainage of the colon.
During the operation, usually using electric suction, pathological contents are removed from the abdominal cavity - purulent formations, bile, blood, feces, etc.
At the end of surgical treatment, for further sanitation of the abdominal cavity - aspiration of exudate and administration of antibacterial drugs, vinyl chloride drains are installed in it.
Next, we will consider the main points of treatment of peritonitis after surgery.
Why is peritonitis dangerous?
Complications of peritonitis in the acute period of the disease are:
- Pulmonary complications
. They develop in the toxic stage of peritonitis, when toxins and bacteria from the peritoneal cavity are carried through the bloodstream throughout the body. Once in the lungs, they cause blood stagnation, disrupting the process of oxygen transfer into them. - Acute renal failure
. It is a severe consequence of peritonitis, which is characterized by a sharp decrease in kidney function. It is known that the main function of the kidneys is to remove toxic metabolic products from the body. - Toxic shock
. It is one of the causes of death due to peritonitis. It develops in the toxic stage, when toxins spread from the source of inflammation throughout the body. It is known that one of the pathogenetic links in peritonitis is increased vascular permeability. Bacteria and their toxins easily enter the bloodstream through the damaged wall. - Dehydration of the body
. Characterized by a loss of fluid from the body of 5 percent of normal or more. With exicosis, there is a lack of water not only in the bloodstream, but also in all cells of the body. Since water is the source of life, it participates in all metabolic processes in the human body.
The consequence of peritonitis is also prolonged exhaustion of the patient. His recovery continues for months. Patients may lose a significant portion of their body weight. This happens because with peritonitis there is an increased breakdown of all the building substances of our body (proteins, fats, carbohydrates). This phenomenon is also called a “catabolic storm.” Therefore, patients who have suffered peritonitis are as exhausted and weakened as possible.
Fatalities
The death of a patient due to inflammation of the peritoneum depends on many reasons: the speed of hospitalization, whether the operation was performed on time and its adequacy, how extensive the affected area is, how long the patient has been sick, how strong the immune system is, what is the causative agent, how capable the pathogen is of infecting the body, what is the age of the patient, is whether there are concomitant diseases, how experienced the doctors are.
The older the patients, the higher the risk of death. This is explained by the fact that the development of the disease causes changes in many organs and systems of the body. And with the progression of the process, all organs and systems are involved in a vicious circle of changes in homeostasis and are quickly affected by aggressive mediators, which can cause rapid decompensation.
The main causes of mortality in peritonitis, according to experts, are progressive endotoxicosis and purulent-septic complications that cause multiple organ failure. Mortality in the first (reactive) phase of peritonitis is 9.1%, in the second and third phases – 33.9%.
The mortality of patients at the first stage of the disease was explained, first of all, by complications associated with the work of the heart, blood vessels, lungs, ulcers of the digestive system, which resulted in gastrointestinal bleeding, and exacerbation of concomitant diseases. Carrying out complex therapy measures, when active methods are used (laparotomy and further irrigation of the abdominal cavity) leads to a reduction in mortality by 1.3 times, and in the later stages of peritonitis - by 1.4 times.
So, the high level of mortality due to inflammation of the peritoneum is explained by a whole range of reasons: untimely consultation with a doctor, the age of the patient, diagnostic errors at each stage of treatment, low returns from antibiotic therapy, the occurrence and progression of multiple organ failure.
When is surgery needed?
Peritonitis is an inflammation of the peritoneum that can lead to disruption of various body functions and also cause death. The cause of inflammation is a bacterial infection of various types: E. coli, staphylococcus, etc. Sometimes inflammation occurs due to a specific type of microflora, for example, due to Mycobacterium tuberculosis.
When treating peritonitis, a surgical method is used - surgery is usually performed urgently to minimize risks. In its process, exudate is removed from the abdominal cavity, and then all internal organs are checked to understand what was the cause of peritonitis in a particular situation.
After identifying the cause and correcting it, the abdominal cavity is washed with special solutions, and the wound is sutured (with or without drainage).
Next comes the recovery, rehabilitation period. At this time, the patient is in the hospital, he is treated with antibiotics, given painkillers, and medications that increase immunity. If the patient has additional problems (for example, with the heart), special supportive medications are prescribed.
Treatment of peritonitis with folk/home remedies is unacceptable in any form! A patient with symptoms of peritonitis requires immediate hospitalization and surgery - otherwise it will end in death.
Medicines used
Medical products (drugs, medicines, vitamins, medicines) are mentioned for informational purposes. We do not recommend using them without a doctor's prescription. We recommend reading: “Why can’t you take medications without a doctor’s prescription?” Considering that peritonitis is a secondary pathology, its initial treatment is aimed at removing the original source, for example, cutting off an inflamed or perforated appendix, suturing perforated ulcers of the stomach or intestines, or removing an inflamed gallbladder.
Surgery for peritonitis is a difficult procedure for the patient, despite the fact that the patient is already in a difficult condition, therefore, intensive and rapid preparation must be carried out before surgery. The administration of blood replacement fluids, saline solutions, weak diuretics, albumin, and antibacterial drugs is prescribed. The patient is given:
- protein;
- polyglucin;
- rheopolyglucin;
- glucose solution at a concentration of 5 or 10%;
- Ringer's solution.
In case of obvious tachycardia and heart failure, the patient is added to the treatment regimen with a solution of strophanthin at a concentration of 0.05%, 0.5 ml per 500 ml of solution, twice a day. The appointment is carried out both before surgery and in the postoperative period.
The most common microbiological factor that plays a role in the development of peritonitis is anaerobic bacteria, E. coli, staphylococcus or several different types of microbes, so primary antibiotic therapy is prescribed based on this flora. Typically a combination of sulfonamides, antibiotics and antimicrobial antiseptics such as tinidazole, ornidazole or metronidazole is used. Next, the attending physician pays attention to the emerging sensitivity of the microflora and adjusts the therapy in accordance with it.
The administered daily doses have a high concentration of active substances. The penicillin group is administered at the rate of 10-15 million units, ampiox, ampicillin and methicillin are administered at 3-5 grams. Aminoglycosides are used in 2-3 grams (monomycin and kanamycin), or 240 mg (gentamicin). The group of cephalosporins, represented by ceporin, kefzol and cefotaxime, is used at a dose of 5 grams per day. Aminoglycosides, except gentamicin, are administered intracavitary, and other drugs are administered through intramuscular or intravenous injections.
If a patient develops hyperthermic syndrome after surgery, it is necessary to urgently begin the procedure for restoring water and electrolyte balance:
- physical cooling;
- intramuscular injections of hydrocortisone, analgin, diclofenac;
- intravenous administration of perfalgan.
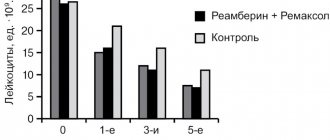
Detoxification treatment is carried out infusionally through:
- blood transfusions;
- prescription of reamberin;
- administration of rheopolyglucin and sodium chloride solution;
- prescribing antihistamines and antienzymes.
In acute peritonitis, the patient develops a state of so-called “catabolic storm”, that is, a sharp acceleration of metabolism. To slow it down, the patient must be given anabolic steroids, for example, retabolil, as well as saline solutions.
If the patient has repeated profuse vomiting, this indicates a disturbance in gastrointestinal motility and electrolyte balance. To eliminate disorders, provided that the kidneys are functioning normally, 40-60 ml of liquid is administered daily for each kilogram of the patient’s weight, as well as chloride salts of potassium, sodium, magnesium and calcium.
To prevent acute renal failure, the patient is prescribed heparin 5 thousand units. intramuscularly 3 times on the first day after surgery. The drug improves the rheological properties of blood and microcirculation.
Stimulation of the function of the gastrointestinal tract is achieved by installing hypertensive enemas, as well as intravenous administration of sodium chloride solution, intramuscular injections of nibufin, aceclidine, cerucal.
Prevention of peritonitis
Preventive measures are aimed at reducing the risk of developing a life-threatening disease. Thanks to prevention, it is possible to promptly identify and begin treatment of diseases that can potentially be complicated by peritonitis. These include peptic ulcer of the stomach and duodenum, cholelithiasis, cholecystitis, as well as other nosologies. During screening examinations, the doctor talks about the dangers of the disease and diagnostic methods. Educational activities increase the literacy of the population, thus reducing the number of complications.
In addition to treating chronic diseases and performing screening tests, it should be remembered that sanitary and hygienic procedures are an integral component of postoperative recovery.
Sutures that were placed on the anterior abdominal wall during surgery can become infected if the rules of asepsis and antisepsis are not followed.
When the first symptoms of acute peritonitis appear, you should immediately consult a doctor. Only a specialist identifies signs of peritonitis, can make an accurate diagnosis and prescribe treatment. Self-treatment increases the likelihood of death, especially when it comes to peritonitis in children.
Nutrition for peritonitis
Diet therapy is an important part of postoperative rehabilitation after peritonitis. Surgical intervention causes disruption of the body's functionality, so the reserves of proteins, fats and carbohydrates are depleted. Therefore, the patient’s diet after peritonitis must be balanced and include all elements to normalize energy metabolism. The determination of the final diet (composition, duration) depends on the cause that caused peritonitis. The postoperative period is divided into several stages, which determine the patient’s nutritional pattern. The rules of the basic diet are:
- Diet - should consist of 5 - 6 meals.
- Pauses between meals are no more than 4 hours. Dinner - 1 - 2 hours before going to bed.
- The temperature of the dishes is average. Excessively hot or cold food is excluded.
- The consistency of the food is liquid and mushy. When boiled, food may have a denser structure than porridge, but should be served pureed.
- The recommended heat treatment is boiling or steaming. The use of an oven is also allowed, but without forming a crust on the products.
- Rest after meals - if possible, especially during lunch hours, after eating food you should take a horizontal position for 15 - 30 minutes.
- Fluid intake - tea, milk and other drinks should be consumed 20 - 30 minutes after meals. The amount of liquid taken at one time should not exceed 1 glass.
To ensure that the food you eat does not have an aggressive effect on the organs of the digestive system, it is necessary to exclude foods that are strong stimulants of secretion.
Postoperative rehabilitation
The postoperative recovery period after surgery is divided into three stages:
- early (from 3 to 5 days);
- late (2-3 weeks after the intervention);
- remote (until it becomes possible to go to work, or until you become disabled).
Recommendations for patient care, depending on the phase, are somewhat different. In general, the rehabilitation period is carried out by a doctor directly in the hospital, or, after discharge, under his periodic supervision. In the absence of positive dynamics and evidence of recovery of the body, the tactics of postoperative therapy are changed according to indications.
General principles of therapy after surgery:
- adequate pain relief;
- intensive infusion therapy;
- detoxification of the patient's body;
- antimicrobial effect;
- preventing the onset of intestinal paresis;
- normalization of the functioning of the gastrointestinal tract system and all other systems affected by pathology.
Primary care after surgery begins immediately upon completion and lasts until the patient is fully able to work.
In the early phase, the patient is transferred on a gurney to the intensive care unit, and the room is provided with warmth and comfort. A warm heating pad is placed on the legs, and an ice pack is placed on the postoperative wound for up to half an hour. The patient should lie in bed in the Fowler's position, that is, the head is raised 45 degrees, the legs are bent at the knees and tucked at the hip joints. Unconscious patients are placed horizontally, without a pillow under their head.
In the first 2-3 days, strict bed rest and fasting are observed. According to indications, the patient is connected to an artificial lung ventilation system. On the second day, the first dressing change occurs. If the postoperative bandage becomes loose or contains blood from the wound, it is changed earlier. Every hour, pulse, respiration, urine output and drainage discharge are monitored. Drains need to be washed periodically, and the dressings around the drains must be changed personally by the doctor.
From the second day, parenteral nutrition is prescribed through infusions - the patient is given a 10% solution of glucose, amino acids, and salt. On the first day after surgery, drinking is excluded, and then you are allowed to drink 1 teaspoon of water once an hour. If intestinal motility is established, enteral nutrition with liquid mixtures through a nasogastric tube is allowed.
After the second day, constant stay in bed becomes undesirable, as it contributes to the occurrence of complications. After the first day, the patient needs to start moving in bed - bending and unbending his limbs, turning. On the 2-3rd day you need to start sitting up in bed and move around the room with the help of a nurse.
The late phase of recovery begins when a person has stable intestinal motility, gases and stool appear. Such signs are an indication to transfer the patient to independent feeding without a tube. Food is allowed in liquid and pureed form, divided meals up to 6 times a day, in small portions. In the first week, only liquid food is allowed, namely:
- broths;
- jelly;
- jelly;
- vegetable puree soups.
By the end of the first week, the menu includes pureed low-fat cottage cheese, soft-boiled eggs, boiled meat and low-fat fish, chicken (all in the form of pureed meatballs, soufflés or cutlets), slimy soups and decoctions. Boiled oatmeal and rice porridge are allowed. Any difficult-to-digest foods that require special efforts from the digestive tract to process are excluded. Cold and carbonated drinks are prohibited. A week after the operation, it is allowed to add yesterday’s white bread and crackers from it, as well as a limited amount of honey and marmalade (about once a day). Short walks around the department are allowed. The sutures are removed after 8-9 days, and the drainage is removed within 4 days after surgery. The patient is usually discharged on the day the sutures are removed.
After discharge, the patient’s routine does not immediately return to normal. In the first months, he needs to comply with a list of restrictions, for example, he is prohibited from lifting weights of more than 3 kilograms or engaging in physical activity. Intimate life is excluded for up to one and a half months. It is mandatory to perform therapeutic exercises, which include training the respiratory organs, cardiovascular system, strengthening and moderate stimulation of the abdominal muscles, and gradual restoration of working capacity. During this period, limited walking, skiing, and swimming are useful for the patient. In some cases, sanatorium treatment is prescribed.
Meals are based on the principle of fractional meals, at least 5 times a day. You can't overeat, just like you can't starve. All food should be boiled or steamed, without crusts, fried or spices. Products that are irritating and difficult for the gastrointestinal tract are excluded. In the future, the consumption of lard, margarine, smoked meats, sugar, baked goods, jam and sweets is limited.
Disease prognosis
Peritonitis is considered a pathology with a high mortality rate. Acute peritonitis, which occurs in three phases, is least dangerous at the reactive stage; here the likelihood of dying is not so high. Regarding the toxic phase, statistically the mortality rate ranges from 18 to 25%. In the absence of normal treatment and when the condition reaches the terminal stage, out of 10 patients only one has a chance to survive. In the presence of complications of peritonitis, including toxic shock, multiple organ failure, sepsis, survival rate is up to 50%. Purulent and diffuse peritonitis leads to death in approximately 15% of patients.
First aid
If there are suspicions of diseases that can cause peritonitis, or if signs of an existing infection of the abdominal cavity appear, the patient must be urgently taken to the nearest hospital, providing transportation independently, or with the participation of an ambulance team. In this case, only an urgent operation can save a person’s life.
It should be noted that at the slightest suspicion of peritonitis, the use of any painkillers, including analgin, diclofenac, morphine or pantopon, is strictly prohibited, since blurring the clinical picture significantly complicates diagnosis and treatment.
Any attempts to stimulate intestinal motility with enemas or medications are also not allowed, since they interfere with the delimitation of inflammation and contribute to its spread.
Manifestations of heart failure require the introduction and use of appropriate drugs - cordiamine, caffeine, water-soluble camphor, digoxin. Taking into account respiratory failure, oxygen inhalations are performed.
The patient is transported with maximum comfort. Before hospitalization, the patient should be provided with bed rest in a semi-sitting position with bent knees. A cold compress is placed on the stomach. Eating any food is prohibited, and drinking is limited.
As for the use of any medications, antibiotics, infusion solutions, gastric lavage or insertion of a gastric tube, the decision on their use is made only by the emergency physician.