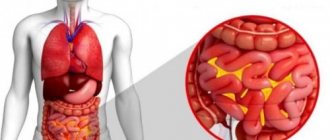
Peritonitis is a process of inflammation of the peritoneum. With peritonitis, organ functioning is disrupted due to severe intoxication of the body. The connective tissue of the peritoneum envelops all the internal organs of the abdominal cavity and serves as a limiter between the internal environment of the abdominal cavity and the abdominal muscles.
When exposed to pathogenic microorganisms or chemical agents on the surface of the peritoneum, it is capable of releasing special substances that stop this process. If the number of pathogenic factors is large, then the peritoneum becomes involved in inflammation and peritonitis occurs. Peritonitis is a very life-threatening condition. If it occurs, emergency medical attention and urgent treatment are required, otherwise death is possible.
Causes of peritonitis
Peritonitis is a very serious condition!
Peritonitis is classified as primary or secondary. In primary peritonitis, the causative agent is microorganisms that entered the peritoneum along with the blood flow from the infectious focus in the body. At the same time, the integrity of the peritoneum is preserved.
Primary peritonitis is classified as:
- spontaneous childhood primary peritonitis (usually girls under 7 years of age);
- spontaneous adult primary peritonitis (due to ascites, side effect of hemodialysis);
- primary peritonitis in persons suffering from active tuberculosis.
Secondary peritonitis is accompanied by damage or rupture of all layers of the peritoneum as a result of penetrating trauma to the abdomen or a violation of the integrity of one of the internal organs.
Secondary peritonitis is classified into:
- peritonitis caused by a violation of the integrity of internal organs;
- peritonitis caused by penetrating or blunt abdominal trauma;
- peritonitis, which developed in the postoperative period.
There is tertiary peritonitis, which develops in the abdominal cavity after peritonitis has already occurred. That is, in essence, this is a relapse of peritonitis. Fortunately, it is rare. Its peculiarity is an erased course, severe intoxication and failure of almost all internal organs. It occurs when the body's defenses are severely depleted. Such peritonitis often does not respond to therapy and ends in the death of the patient.
Causes of pathology
The root cause of the inflammatory reaction in the tissues of the abdominal cavity, which leads to peritonitis, in most cases is a bacterial infection (caused by microflora located in the digestive tract). The following gram-negative and gram-positive microorganisms can provoke this complication:
- streptococci;
- staphylococci;
- bacteroides;
- clostridia;
- Pseudomonas aeruginosa;
- peptococci;
- Proteus;
- enterobacter;
- eubacteria;
- fusobacteria.
In the vast majority of cases - according to various statistical data, 60-80% - inflammation of the peritoneum is caused not by one, but by an association of microbes. More often, this pathological process is provoked by E. coli or staphylococci. In more rare cases, the development of peritonitis is caused by pathogens such as pneumococcus, Koch's bacillus (Mycobacterium tuberculosis), gonococcus and hemolytic streptococcus. Considering the above-described facts about the variability of possible pathogens of peritonitis, when prescribing treatment, the doctor must wait for the results of an analysis of the sensitivity of pathogenic microflora to antibiotics.
Lethal outcomes from inflammation of the peritoneum can reach significant values - according to statistics, in gastroenterological diseases, death from such a complication occurs in 20-30% of patients, and in severe illnesses this figure reaches 40-50%. We may recall that it was traumatic peritonitis after an injury to the abdominal cavity that caused the death of A. S. Pushkin.
The process of development of peritonitis
The speed and severity of the development of peritonitis symptoms largely depends on the state of the body, on the pathogenicity of microbes, and on the presence of provoking factors.
The main points in the development of peritonitis are as follows:
- Intestinal paresis, as a result of which the absorption function is impaired, and the body loses a large amount of water and electrolytes.
- Dehydration and decreased pressure in blood vessels leads to strong heartbeat and shortness of breath.
- The rate of development of peritonitis and the severity of damage to the peritoneum depends on the number of pathogenic bacteria and the magnitude of intoxication.
- Autointoxication is added to intoxication caused by microbes. In response to the aggression of microorganisms, antibodies are released in the blood that attack the lipopolysaccharide wall of the bacterium. The compliment system is activated and many active substances are released, the effect of which is manifested by intoxication.
If the human body is weakened or the microorganism is highly pathogenic, then peritonitis is not limited, but becomes diffuse or widespread. The spread is especially facilitated by increased peristalsis, as well as blood and exudate in the abdominal cavity.
Disease prognosis
Peritonitis is considered a pathology with a high mortality rate. Acute peritonitis, which occurs in three phases, is least dangerous at the reactive stage; here the likelihood of dying is not so high. Regarding the toxic phase, statistically the mortality rate ranges from 18 to 25%. In the absence of normal treatment and when the condition reaches the terminal stage, out of 10 patients only one has a chance to survive. In the presence of complications of peritonitis, including toxic shock, multiple organ failure, sepsis, survival rate is up to 50%. Purulent and diffuse peritonitis leads to death in approximately 15% of patients.
Clinical manifestations of peritonitis
The initial symptoms of peritonitis are very varied
Symptoms depend on the cause of the disease, so the initial signs can be very varied. But there are several successive stages, depending on the time of onset of symptoms.
Reactive stage
Develops in the first day. Severe pain occurs, the patient can clearly determine the location. If the cause of peritonitis is perforation of a hollow organ, then this pain is described as dagger-like. For example, perforation of a stomach ulcer is described as severe sharp pain in the epigastric region, rupture of the appendix is described as pain in the right iliac region.
The pain gradually spreads to other areas of the abdomen. Sometimes, after it occurs, the pain becomes less intense and does not bother the patient as much. This is how a symptom of imaginary well-being manifests itself. After some time, the pain returns.
The face of a patient with peritonitis is very typical. It is pale, sometimes even with an earthy tint. Covered with drops of sweat when pain occurs. Facial features become sharp due to dehydration. Severe pain forces the patient to take a comfortable position in order to somehow alleviate it. More often, a person lies on his side with his legs bent, sparing his stomach in every possible way, trying not to strain it.
When examining such a patient, tense abdominal muscles are found - a plank-shaped abdomen. The Shchetkin-Blumberg symptom is pronounced, in which a sharp removal of the hand from the surface of the abdomen at the time of palpation leads to increased pain.
Nutrition for peritonitis
Diet therapy is an important part of postoperative rehabilitation after peritonitis. Surgical intervention causes disruption of the body's functionality, so the reserves of proteins, fats and carbohydrates are depleted. Therefore, the patient’s diet after peritonitis must be balanced and include all elements to normalize energy metabolism. The determination of the final diet (composition, duration) depends on the cause that caused peritonitis. The postoperative period is divided into several stages, which determine the patient’s nutritional pattern. The rules of the basic diet are:
- Diet - should consist of 5 - 6 meals.
- Pauses between meals are no more than 4 hours. Dinner - 1 - 2 hours before going to bed.
- The temperature of the dishes is average. Excessively hot or cold food is excluded.
- The consistency of the food is liquid and mushy. When boiled, food may have a denser structure than porridge, but should be served pureed.
- The recommended heat treatment is boiling or steaming. The use of an oven is also allowed, but without forming a crust on the products.
- Rest after meals - if possible, especially during lunch hours, after eating food you should take a horizontal position for 15 - 30 minutes.
- Fluid intake - tea, milk and other drinks should be consumed 20 - 30 minutes after meals. The amount of liquid taken at one time should not exceed 1 glass.
To ensure that the food you eat does not have an aggressive effect on the organs of the digestive system, it is necessary to exclude foods that are strong stimulants of secretion.
Methods for diagnosing peritonitis
Treatment of peritonitis - surgical method
In order to make a diagnosis of peritonitis, the doctor must rely on clinical data from the disease, medical history, external symptoms, and examination data of the patient.
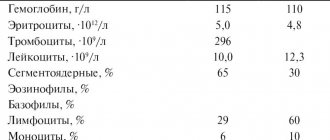
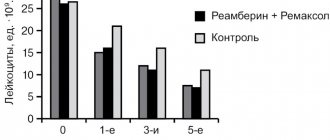
Blood test and instrumental data are important.
Changes in the hemogram are aimed at increasing the number of white blood cells, shifting the formula to the left, and increasing ESR. These are universal signs of inflammation. Hemoglobin falls, the number of red blood cells decreases. Due to blood thickening, its clotting is impaired.
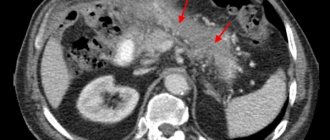
The main role is played by ultrasound of the abdominal cavity. It shows the primary localization of peritonitis, the affected organ and the degree of spread of the process throughout the peritoneum. The sooner a person with symptoms of peritonitis seeks help, the greater his chances of recovery. Therefore, if you have a disease that is accompanied by fever, uncontrollable vomiting, or abdominal pain, you must call a doctor. If he suspects peritonitis, he will urgently refer such a patient to the hospital.
Publications in the media
Peritonitis is an inflammation of the peritoneum, accompanied by both local and general symptoms. Frequency • Primary peritonitis occurs rarely, in approximately 1% of cases of acute abdomen • Secondary peritonitis - 15-20% of all cases of acute surgical diseases and injuries of the abdominal organs.
Classifications By reason • Primary: •• Hematogenous •• Lymphogenous •• Per continuitatem (through the fallopian tubes) • Secondary •• Infectious-inflammatory: ••• appendicular ••• with inflammatory diseases of the liver and extrahepatic biliary tract ••• with acute obstruction intestines ••• with thrombosis of mesenteric vessels ••• with acute pancreatitis ••• gynecological •• Perforated: ••• ulcers of the stomach and duodenum, as well as ulcers of the rest of the intestine (ulcerative-necrotizing enterocolitis, typhoid, dysenteric, tuberculosis, oncological and any other origin) ••• bedsores with obstructive intestinal obstruction, with foreign bodies in the gastrointestinal tract ••• strangulation grooves with strangulation intestinal obstruction, hernia strangulation ••• intestinal necrosis due to thromboembolism of mesenteric vessels •• Traumatic: with open and closed injuries to the abdominal organs cavity •• Postoperative: ••• failure of sutures after operations on the abdominal organs ••• infection of the abdominal cavity during surgery ••• defects in the application of ligatures to large areas of the omentum and mesentery with subsequent necrosis of tissue distal to the ligature ••• mechanical damage to the peritoneum, its drying out ••• hemorrhage into the free abdominal cavity with insufficiently reliable hemostasis.
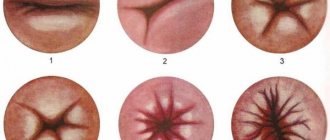
Clinical • Acute peritonitis is the most common and dangerous disease • Chronic peritonitis. By the nature of the exudate : serous, fibrinous, purulent, hemorrhagic, fecal, putrefactive, combinations of the above forms (for example, serous-fibrinous, fibrinous-purulent, etc.). According to the degree of spread of the inflammatory process along the surface of the peritoneum • Limited peritonitis (abscess or infiltrate) •• Appendiceal •• Subphrenic •• Subhepatic •• Pelvic •• Interintestinal • Diffuse peritonitis •• Local - in close proximity to the source of infection, occupies one anatomical area of the abdomen . Prone to generalization •• Widespread - occupies two anatomical areas of the abdomen or more •• General - total damage to the peritoneum. By development phases • Reactive (first 24 hours) - local symptoms prevail in the clinical picture • Toxic (24–72 hours) - phase of increasing intoxication. Corresponds to the concept of endotoxin shock • Terminal (over 72 hours) - equivalent to the concept of septic shock.
Etiology . The main cause of peritonitis is infection. Microbial (bacterial) peritonitis • Nonspecific, caused by gastrointestinal microflora •• Aerobes: ••• gram-negative: Escherichia coli, Pseudomonas aeruginosa, Proteus, Klebsiella, Enterobacter, Acinetobacter, Citrobacter; ••• gram-positive: Staphylococcus, Streptococcus •• Anaerobes: ••• gram-negative: Bacteroides, Fusobacterium, Veillonella; ••• gram-positive: Clostridium, Eubacterium, Lactobacillaceae, Peptostreptococcus, Peptococcus • Specific, caused by microflora not related to the gastrointestinal tract: Neisseria gonorrhoeae, Streptococcus pneumoniae, Streptococcus pyogenes, Streptococcus viridans, Mycobacterium tuberculosis. Aseptic (abacterial, toxic-chemical) peritonitis becomes microbial within a few hours due to the penetration of infection from the intestinal lumen • Exposure of the peritoneum to aggressive agents of a non-infectious nature: blood, bile, gastric juice, chylous fluid, pancreatic juice, urine • Aseptic necrosis of internal organs . Special forms of peritonitis • Carcinomatous • Parasitic • Rheumatoid • Granulomatous. Pathogenesis. Intoxication, hypoxia, gastrointestinal motility disorders, hemodynamics, metabolism, immune defense and multiple organ failure. Pathological anatomy . Characterized by hyperemia, a decrease in the luster of the peritoneum (to the point of its complete absence), fibrinous deposits, exudation, the development of edema and infiltration of the omentums, mesenteries, and intestinal walls. At first, these changes are most pronounced near the source of peritonitis, then gradually spread to other parts or to the entire peritoneum.
Clinical picture • Pain (the earliest and most constant symptom) •• First, the pain is localized in the area of the source of peritonitis, gradually spreads throughout the abdomen, becomes constant, poorly localized •• As intoxication increases, paralysis of the nerve endings of the peritoneum occurs, leading to a decrease in the intensity of pain • • With perforation, the pain is sudden and intense (dagger pain) •• Radiation of pain to the shoulders or supraclavicular areas (Elecker symptom). • Tension of the muscles of the anterior abdominal wall •• Reactive phase - plank tension •• Toxic phase - muscle relaxation. • Symptoms of peritoneal irritation •• Shchetkin-Blumberg - when palpating the abdomen, sharp abduction of the hand from the anterior abdominal wall leads to acute pain (positive symptom). With plank-like tension in the muscles of the anterior abdominal wall, it is not always clearly expressed •• Mendel - identification of percussion pain with sequential tapping with a bent finger along the entire abdominal wall (determining the presence and localization of pain) •• Voskresensky (shirt symptom) - pain when quickly moving the palm along the anterior abdominal wall wall (on top of the shirt). • Nausea and vomiting at the beginning of the disease are reflexive in nature, and later become a consequence of intestinal paresis. An admixture of bile is added to the vomit, then the contents of the small intestine (fecal vomiting). • Paralytic intestinal obstruction rarely occurs at the onset of the disease, more often it occurs as a consequence of severe intoxication.
Diagnostics • Digital examination of the rectum and vaginal examination - severe pain in the anterior wall of the rectum or vaginal vaults (Kulenkampff's symptom) • Laboratory tests: •• Positive result of culture of peritoneal exudate •• Leukocytosis, neutrophilia, shift of the leukocyte formula to the left, increase in ESR •• Increase residual blood nitrogen •• Blood thickening according to Ht indicator •• Metabolic acidosis •• Respiratory acidosis • X-ray examination •• Free gas under the dome of the diaphragm (sickle symptom) with perforations or ruptures of hollow organs •• Kloiber cups, intestinal arcades, significantly dilated intestinal loops if it is obstructed • Ultrasound: presence of free fluid, abscesses • Abdominal puncture (laparocentesis). Contraindicated in case of extensive adhesions in the abdominal cavity due to the risk of damage to internal organs • Laparoscopy • Diagnostic laparotomy is indicated if the above set of measures does not eliminate doubts about the diagnosis. Differential diagnosis • Diseases of the lungs and pleura (pneumonia, pleurisy, lung and rib injuries, hemo- and pneumothorax) • Cardiovascular diseases (angina pectoris, MI, aneurysm of the abdominal aorta and its branches) • Damage to the spine and spinal cord, tuberculous spondylitis, tumors and osteomyelitis of the spine • Endocrine diseases and metabolic disorders (DM, thyrotoxicosis, acute adrenal insufficiency, hypercalcemia, hypokalemia, uremia) • Infectious diseases (foodborne diseases, viral hepatitis, influenza, tonsillitis, scarlet fever, diphtheria, dysentery, typhoid fever) • Genitourinary diseases organs (mobile kidney, urolithiasis, acute pyelonephritis, apostematous pyelonephritis, paranephritis, hydronephrosis, tumors and amyloidosis of the kidneys) • Diseases and injuries of the anterior abdominal wall (hematomas, abscesses, tumors).
TREATMENT Diet. Parenteral nutrition. In the postoperative period, as peristalsis is restored, diet No. 0 is prescribed. Surgical (local) - laparotomy or relaparotomy. • Preoperative preparation. It is better to postpone the operation for 2-3 hours for targeted preparation than to start it on an unprepared patient •• Infusion therapy •• Catheterization of the bladder •• Preparation of the gastrointestinal tract ••• In the early stages of peritonitis - a single emptying of the stomach using a tube ••• In the later stages stages of peritonitis, the probe should be inserted for a long period of time •• Broad-spectrum antibiotic i.v. • Anesthesia - multicomponent balanced anesthesia using muscle relaxants and mechanical ventilation •• Spinal anesthesia •• Intraoperative novocaine blockade of reflexogenic zones and the root of the mesentery of the small, transverse colon and sigmoid colon. • Surgical tactics •• Surgical access: median laparotomy with hardware correction of access according to the Segal technique •• Elimination or reliable isolation of the source of peritonitis •• Intraoperative sanitation of the abdominal cavity: use solutions pre-cooled to a temperature of 4–6 ° C (intraoperative local abdominal hypothermia) •• Intestinal decompression : nasogastrointestinal intubation of the small bowel according to Abbott-Miller. The colon is drained through the anus •• Drainage of the abdominal cavity: vinyl chloride or rubber tubes, multi-channel vinyl chloride drainage, drainage from a semi-permeable hydrated cellulose membrane •• Completion of the operation: closed method, semi-open method (planned relaparotomy), open method (peritoneostomy).
Conservative therapy in the postoperative period . • Adequate pain relief. • Balanced infusion therapy. • Prevention and treatment of multiple organ failure syndrome •• Adequate pulmonary ventilation and gas exchange with early mechanical ventilation •• Stabilization of blood circulation with restoration of blood volume •• Normalization of microcirculation •• Correction of metabolic changes •• Removal of toxins using efferent surgery methods: hemosorption, hemodialysis, ultrafiltration, therapeutic plasmapheresis, lymphosorption, floor-by-floor sorption hemoperfusion of the abdominal cavity, enterosorption, xenosplenperfusion, quantum hemotherapy, extracorporeal oxygenation •• Prevention and treatment of renal and liver failure •• Maintaining the immune status of the patient •• Parenteral nutrition. • Antibacterial therapy. The most adequate regimen of empirical antibacterial therapy (until the results of bacteriological examination of blood or peritoneal fluid are obtained) is a combination of cephalosporins (cefamandole), aminoglycosides (gentamicin) and metronidazole. Routes of administration: •• Into the abdominal cavity through irrigators, drainages •• Intravenous, intraarterial (intra-aortic), intramuscular, intraportal, endolymphatic anterograde, endolymphatic retrograde, lymphotropic interstitial. • Immune therapy •• Pyrogenal or prodigiosan (no more than 1 time every 3-5 days) •• immunoglobulin •• antistaphylococcal -globulin •• leukocyte mass •• antistaphylococcal plasma •• levamisole •• thymogen.
• Restoration of gastrointestinal functions •• Aspiration of toxic contents through probes inserted into the small and large intestines •• Bilateral perinephric novocaine blockade according to A.V. Vishnevsky •• Anticholinesterase drugs (neostigmine methyl sulfate, distigmine bromide), ganglion blockers (dimecolony iodide, hexamethonium benzosulfonate); anticholinergics (atropine), replenishment of potassium deficiency •• Various types of enemas •• Physiotherapeutic stimulation of intestinal motility. • Hyperbaric oxygen therapy. It is advisable to combine it with drug treatment. Course and prognosis • Mortality with widespread purulent peritonitis is 25–30%, with the development of multiple organ failure — 85–90%.
ICD-10 •• K65.0 Acute peritonitis
Treatment methods for peritonitis
Peritonitis is treated surgically. The operation is prescribed urgently, after appropriate preparation of the patient. The surgeon will open the abdominal cavity, eliminate the cause of peritonitis, suture the diseased organ, perform an inspection, and wash the internal organs and peritoneum with an antiseptic and saline solution. If peritonitis has affected a large part of the peritoneum, the wound is not tightly sutured, but additional lavage of the abdominal cavity is performed on the second and third days.
Complications
Peritonitis in children and adults is dangerous due to the development of multiple organ failure and intoxication of the body. Among the complications of the acute process:
- dehydration;
- renal failure;
- toxic shock;
- pulmonary pathologies;
- liver failure;
- secondary inflammatory processes.
Peritonitis after surgery may be accompanied by the formation of fistulas and abscesses of internal organs, and suppuration of postoperative sutures. The appearance of a number of complications is possible far beyond the abdominal cavity - occlusion of deep veins, inflammation of the lungs and pleura, mediastinitis.
Preoperative preparation and monitoring
- For successful surgical intervention, it is necessary to carry out preoperative preparation.
- The patient must have a peripheral and central vein and bladder catheterized and premedicated.
- Midazolam (5 mg) and 10–20 mg of cerucal are administered on the operating table. Atropine administration is contraindicated, as there is a high probability of developing bradycardia.
- Medicines are administered that help reduce the acidity of gastric juice (about 40 mg of omeprazole or famotidine/ranitidine 50 mg into a vein).
- During the operation, infusion therapy is carried out in an amount of at least 1.5 liters of physiological solution, and plasma and blood products are added if necessary.
- Perform artificial ventilation and administer oxygen.
In the case when the patient lies on the operating table and there is more than 25 ml of contents in the stomach, there is a real threat of aspiration. This is the name for the entry of stomach contents into the lumen of the bronchial tree. Gastric juice can cause a burn to the mucous membrane of the bronchi and trachea. Complications of aspiration include multiple pulmonary atelectasis, bronchospasm, respiratory failure, and pulmonary edema.
Aspiration of small amounts of gastric juice can subsequently lead to aspiration pneumonia.
Therefore, in anesthesiological practice in patients with peritonitis, ganglioblockers and anticholinergics - drugs that can reduce the tone of the lower esophageal sphincter - are not used.
Antibacterial therapy is carried out with a combination of antibiotics that act on both Gram-plus and Gram-minus bacteria. For community-acquired peritonitis, this is intravenous administration of cefotaxime and metronidazole. For in-hospital use - cefepime and metronidazole. If peritonitis develops in the hospital during antibiotic therapy, carbapenems are used.
Postoperative period
Antibiotic therapy for peritonitis is mandatory
In the postoperative period, some problems may arise related to the normal functioning of the intestines, severe pain, and the development of purulent complications. Recommended:
- observation of the patient, hourly assessment of respiratory rate, pulse, diuresis, central venous pressure, drainage discharge;
- infusion therapy with colloid and crystalloid solutions is carried out;
- to warm patients, infusion media are heated to body temperature;
- the lungs are ventilated for 72 hours to ensure sufficient oxygen supply to organs and tissues;
- a glucose solution is administered through a nasogastric tube;
- early restoration of intestinal motility;
- prevention of pain syndrome. Narcotic analgesics are used in combination with non-steroidal anti-inflammatory drugs. Fentanyl, morphine, ketorolac are used.