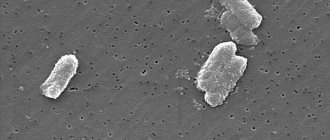
Enterobacters are gram-negative bacteria that are rod-shaped and covered with flagella. They do not form spores and develop under anaerobic conditions, but are able to survive in the presence of oxygen. Most of these microorganisms are part of the normal intestinal microflora of humans and animals, and some live in water, soil and food. Enterobacter under a microscope looks like a rod with flagella.
What are enterobacteria?
Enterobacteriaceae are a large group of microorganisms that live in various parts of the gastrointestinal tract and have a positive or pathogenic effect on the human body. All enterobacteria are divided into three groups: pathogenic, opportunistic and saprophytic.
- Most enterobacteria are representatives of the intestinal microbial biocenosis. These are Klebsiella, Enterobacter, Serration, Proteus, Citrobacter, Providence and Yersinia. They perform vital functions in the macroorganism, but under the influence of negative factors they become dangerous and cause various diseases.
- Absolute pathogens include Shigella, Salmonella and some species of Escherichia. These microbes, having entered the human body from the outside, cause acute intestinal infections and other pathologies that threaten the patient’s life.
- Saprophytic enterobacteria are not dangerous epidemiologically and are not important for practical medicine.
The Enterobacteriaceae family includes many genera and species that can cause serious disease in humans. One of the main representatives of this family is Enterobacter. It is considered a normal inhabitant of the human intestine, ensuring its adequate functioning.
Clepsiella
Clepsiella causes pneumonia.
Clepsiella is a collective name for strains of opportunistic microorganisms. They belong to facultative anaerobes.
That is, they can live both in the presence of oxygen and without it. Varieties of this microorganism can cause the following pathologies:
- lungs – causes pneumonia;
- conjunctivitis;
- digestive system;
- meningitis;
- genitourinary disease.
In 1 g of feces there should be no more than 10 * 5 microorganisms. Clepsiella are typical representatives of nosocomial infections. The source of infection is the carrier of the microorganism. It may take several weeks from the moment of infection to the first symptoms.
When the lungs are affected, an increase in temperature is observed, the cough is initially dry, then wet with the discharge of foul-smelling sputum with blood. Without treatment, sepsis develops. The mortality rate is 36%. When the lesion is localized in the nose, foul-smelling rhinorrhea, nasal congestion, and fever are observed. When the gastrointestinal tract is damaged, symptoms of acute colitis or enterocolitis develop.
Types of enterobacteria
The Enterobacteriaceae family is very large. It includes more than 100 varieties that are found everywhere: in water, soil, flowers, trees, food, in the bodies of living beings, including humans, in an environment that is nutritious for them (containing lactose).
Table. Types of enterobacteria
| Group | Characteristic |
| Pathogenic | Microbes located outside the human body. When ingested, they cause the development of acute intestinal infections and other pathologies that are life-threatening to the patient (salmonella, shigella, escherichia). |
| Opportunistic | They are present in the human body and under normal conditions are not dangerous; they play an important role in the functioning of the gastrointestinal tract. When negative factors occur, they change properties and become the cause of many diseases (enterobacter, yersinia, citrobacter, etc.) |
| Saprophytic | Epidemiologically safe bacteria are of no interest for practical medicine |
One of the main ones in this family is Enterobacter. Its presence in the intestines ensures its normal functioning. However, if Enterobacter invades other organs, it will cause serious problems. It is the leading cause of death in newborns.
Enterobacteriaceae. Characteristic.
Enterobacteriaceae (lat. enterobacteriaceae) are a family of gram-negative (like other proteobacteria), rod-shaped (bacilli), spore-forming bacteria, 1-5 microns long, with flagella for movement. These bacteria are facultative anaerobes and break down carbohydrates to form formic acid and other end products of formate fermentation. Some of them can decompose lactose.
Many members of the family are part of the intestinal microflora of humans and animals . They represent a large number of normal microflora of the human body and a significant number of pathogenic microbes: salmonella, E. coli, plague coli, etc. Enterobacteriaceae are determined in various parts of the gastrointestinal tract of a healthy person: in the jejunum - from 0 to 103 CFU/ml, in the ileum - from 102 to 106 CFU/ml. Normally, in the facultative intestinal microflora they should not exceed the amount of 104 CFU/g.
Another part of these bacteria is found in water and soil or parasitizes various plants and animals. Escherichia coli, a model organism used in molecular biology and genetics, has been well studied due to the knowledge of its genetics and biochemistry.
Enterobacteriaceae remain viable in water and soil for months, but die in a few minutes from disinfectants and in 1 hour at very high temperatures.
These bacteria produce saccharolytic, proteolytic and other enzymes , the determination of which is of taxometric significance. Indole is formed, and glucose, lactose, and mannitol are fermented to acid and gas.
Pathogenicity factors are:
- endotoxin, which is released after the destruction of microbial cells and adhesins,
- cytotoxin,
- exotoxin.
Bacteria can penetrate macrophages and multiply within them . The pathological process is aggravated by a decrease in the activity of phagocytosis and a decrease in the barrier function of tissues. A decrease in beneficial normal flora in the intestines and a violation of colonization and protective functions can lead to penetration into the lymph and blood . Colibacteriosis occurs when the amount of beneficial intestinal microflora and immunity decreases. After an illness, immunity does not develop.
Infections associated with bacteria
Escherichia coli is responsible for most enterobacterial infections. The non-invasive classes of E. coli are called enteropathogenic E. coli (EPEC), and enterotoxigenic E. coli (ETEC), which develop bacterial toxins that interact with digestive juices and cause dehydration. Invasive types of E. coli are divided into enterohemorrhagic E. coli (EHEC) and enteroinvasive Escherichia coli (EIEC).
These subtypes enter the gastric tissues directly, causing destruction of the structures and diarrhea (often with blood). EHEC also causes complications that lead to the destruction of red blood cell structures as well as kidney problems (kidney failure). EHEC is a growing problem worldwide due to frequent infectious outbreaks caused by contaminated food. A specific type of EHEC, known as O157:H7, was identified in 1982 in food chain products, unpasteurized milk and apple juice. Two to seven percent of O157:H7 infections cause serious complications.
Klebsiella and Proteus can in some cases cause urinary tract infections, pneumonia, which usually occurs in people who have a weakened immune system or are dependent on alcohol, and ear and sinus problems. Enterobacteriaceae and serration sometimes lead to bacterial blood infections (carbuncles), also more often in people with weakened immune systems.
Infection entering the body
Enterobacteriaceae are a class of saprophytes. These are gram-negative organisms that are unable to form spores. They adapt very quickly to any environment and are able to survive for a long time without oxygen.
Another distinctive feature of enterobacteria is their high survival rate. Most antiseptics have no effect on them; after minor deactivation, they continue their vital functions. Most antibacterial agents are also completely ineffective against them.
Enterobacteriaceae are a broad class of microorganisms, the classification of which includes several hundred names. Most of them live in the human body; they can penetrate it in the following ways:
- Oral-fecal;
- Contact;
- Domestic;
- Through medical instruments.
Most infections caused by enterobacteriaceae are nosocomial, since it is quite difficult to reduce their activity in large areas.
How to quickly recover from an infection?
Restoration and preservation of a sufficient amount of beneficial normal intestinal flora - lacto- and bifidobacteria, helps protect the intestinal mucosa from the penetration of pathogenic bacteria and their toxins into the blood and lymph, removes toxins, creates an environment in which pathogenic microorganisms cannot continue their vital activity and are eliminated from the human body . It is important that waste products of beneficial bacteria help the immune system remain active in the fight against harmful bacteria.
The synbiotic biocomplex Normoflorins - containing live active lacto- and bifidobacteria and their metabolites with anti-inflammatory, antiseptic, immunogenic and nutritional effects on mucous membranes has proven itself over many years as an active assistant and fighter against pathogenic bacteria for children and adults, pregnant women and patients with various diseases . Quite quickly, when using Normoflorins, intoxication is relieved and intestinal function and general well-being are restored.
It is recommended: as early as possible, start taking Normoflorin in age-specific dosages - L - 10-15 minutes before meals in the morning (+ lunch for constipation), D - lunch or evening 20 minutes before meals, B - at night or in a microenema. Duration of use is 3-4 weeks, until intestinal function is completely restored and overall well-being improves. It is advisable to take sorbents on an empty stomach for 10-14 days - to remove toxins - zosterin or pecto, they reduce putrefaction, fermentation processes, increased gas formation, and improve intestinal function.
It is important to consolidate the effect of microflora restoration, improve the functioning of the pancreas, liver, intestines, and immunity - for this it is good to use functional nutrition for a month - Harmony of Life. It also contains live beneficial lacto- and bifidobacteria, their metabolites and pectin. Tasty, healthy and effective!
Back to list Previous article Next article
Methods for diagnosing pathology
Enterobacterial infection requires laboratory diagnosis; instrumental research methods are not used in this case. First of all, it is worth analyzing the general condition of the patient and his living conditions. Patients in the following categories are at risk:
- Newborn babies;
- People of advanced age with a large number of chronic diseases;
- Patients with, who are often ill and have just had an illness;
- Patients who have been in a hospital for a long time;
- Tourists when switching to food from another region.
To confirm the presence of infection, a number of laboratory tests are performed. These include stool, urine and blood tests. A blood test can determine the presence of an inflammatory process. A urine test can rule out infection of the genitourinary system. The key is to examine the stool, and doctors are able to identify the nature of the infection and the specific pathogen. Stool culture is also actively used to determine sensitivity to a particular type of drug.
Symptoms
It is impossible to independently determine that the causative agent of the infection is some kind of enterobacteria. Therefore, you should always contact your pediatrician if your baby’s condition changes. You need to pay attention to the following signs:
- restlessness and constant crying;
- refusal to eat;
- frequent bowel movements or constipation;
- change in the nature of stool - watery, foul-smelling, mixed with mucus, blood or greens;
- increased body temperature;
- crying when urinating;
- change in urine odor;
- vomiting and nausea;
- redness of the eyes;
- difficulty breathing or cough;
- decreased overall activity;
- excessive sleepiness or prolonged agitation.
In these cases, you should consult a doctor immediately. It is always advisable to remember that inflammation in children of the first year of life develops like a fire, every minute of timely provision of assistance is valuable.
What danger do enterobacteria pose?
The quantitative significance of enterobacteria that a person encounters is very difficult to determine: they are capable of mutating and under normal conditions may not manifest themselves. Typically, diseases caused by these microbes develop as complications of other pathologies. Therefore, the risks are first of all:
- people with weak immune systems;
- Senior citizens;
- newborns;
- people with chronic gastrointestinal pathologies;
- patients staying in hospital for a long time.
Most people believe that enterobacteria only harm the digestive process, but their effect can extend to absolutely any organ.
Thus, bacteria of this family can cause pathologies such as:
- infection of the female reproductive organs;
- respiratory diseases (pneumonia);
- brain abscess, meningitis;
- inflammatory diseases of the urinary tract (cystitis, pyelonephritis);
- blood diseases (sepsis, bacteremia);
- inflammation of the liver and gallbladder;
- salmonellosis, dysbacteriosis, dysentery.
The main danger of such microorganisms is their detrimental effect on beneficial microflora: they destroy positive bacteria, thereby disrupting the functioning of infected organs.
Hafnia or Hafnia
Haphnia are microorganisms belonging to the class of Enterobacteriaceae. Currently, only 1 species of N. alvei has been described. It belongs to facultative anaerobes and rarely exhibits pathogenic properties. Can cause exacerbation of chronic diseases of the gastrointestinal tract, urinary system, and septic pathologies.
This microorganism is difficult to diagnose, and it is rarely the sole cause of the disease. Signs of hafnia infection are similar to the symptoms of salmonellosis - high fever, pain. This pathogen is often confused with E. coli.
Treatment of diseases caused by hafnia is difficult, since the microorganism is resistant to the latest generation of antibiotics, including cephalosporins.
Symptoms of enterobacteriosis
Enterobacteriosis, as a rule, does not have any special symptoms, so they can be identified by the type of pathogen and the location of the affected area. Common manifestations of the disease may be:
- digestive problems, stool disorders (up to the appearance of impurities in the feces);
- nausea, heartburn, increased gas formation, vomiting;
- weakness, feeling of weakness, decreased performance;
- intense pain in the affected area;
- pale skin, chills, lack of appetite, fever, elevated temperature;
- high indicators in test results.
Diseases caused by enterobacteriaceae develop rapidly, and if they are not treated immediately, they can lead to serious complications. Therefore, it is necessary to diagnose the disease in time.
Diagnosis of enterobacteriosis
The presence or absence of infection in the body can only be confirmed by laboratory diagnostics. Based on the patient’s complaints, his medical history, general condition, and lifestyle, the doctor can draw conclusions and refer the person for tests.
Thus, enterobacteria can be found in feces, urine, smears, and pharynx. Each of these tests is the most reliable way to identify the causative agent of pathology of certain organs and begin to fight it.
Enterobacteriaceae in urine
To isolate the bacteria that cause problems with the urinary organs, urine culture is performed. It can be prescribed when there are signs of inflammation of the excretory organs, during pregnancy, diabetes, or a history of chronic cystitis or urethritis. Before collecting urine, you need to take care of genital hygiene.
A week before donating urine, you must give up spicy, fatty and salty foods, and alcoholic beverages.
So, if a microscopic examination reveals more than 105 microbial bodies in 1 ml of urological fluid, inflammation of the urinary organs and kidneys occurs.
Enterobacteriaceae in feces
This study is prescribed if the patient has a high temperature (+38°C), frequent diarrhea and vomiting, and the presence of blood in the feces. The norm for the content of these bacteria in 1 gram of feces will be less than 104 CFU (colony-forming units). Exceeding this norm means the presence of dysbacteriosis. Once the pathogen is detected, researchers test to see how the bacteria respond to antibiotics. It is better to submit feces for testing within an hour.
Enterobacteriaceae in the throat
Most often, microbes disrupt the activity of the gastrointestinal tract. But, having parasitizing properties, they can multiply in neighboring organs, and even in the pharynx. The presence of Enterobacter in the throat can be dangerous: if it enters the respiratory tract, it causes severe pneumonia. Purulent inflammation of the tonsils may also develop. As a rule, the doctor takes part of the material (pus or sputum) for examination. The presence of harmful bacteria in the throat in quantities exceeding 104 CFU indicates the development of inflammation. It is necessary to begin restoring the microflora of the throat mucosa, following all the doctor’s recommendations.
How dangerous are enterobacteriaceae?
Enterobacteriaceae is the general name for a collective group of microorganisms. In clinical practice, lactose-negative ones are important, namely:
- Klebsiella;
- proteas;
- serrations;
- hafnia;
- morganella;
- providence;
- Citrobacter;
- Enterobacter.
These microorganisms are always present in the normal microflora, and if the “good” components are active, the activity of enterobacteria is limited. In a situation where normal microflora is suppressed, opportunistic flora gets a chance to reproduce and increase the size of its population.
Bacteria exhibit their pathogenic properties in different ways:
- Klebsiella - can cause urogenital infections, pneumonia, acute indigestion, inflammation of the meninges, conjunctiva and sepsis in newborns;
- Proteus - produces a toxin that has hemolytic properties, causes acute intestinal infection, damage to the urinary tract up to kidney failure, wound infections, anemia, inflammation of the ear, meninges, hemolytic syndrome or breakdown of red blood cells, sepsis, purulent inflammation of the umbilical wound;
- serrations – cause purulent-inflammatory processes in any organs and tissues;
- hafnia – in weakened children they cause inflammation of the gastrointestinal tract and genitourinary system, as well as a source of nosocomial infection;
- Morganella - causes infectious diarrhea;
- Providence - 5 species were found, causing diarrhea, wound suppuration, septicemia;
- Citrobacter - there are 11 types of these bacteria; when weakened, the organisms are capable of initiating inflammation of the intestines, gall bladder, bones, ear, respiratory tract, and brain abscesses;
- Enterobacter - has 13 species, most often causing various organ damage in those who were previously treated with antibiotics.
Detection of bacteria in a smear
If E. coli is present in the smear, treatment is not required if there are no symptoms of inflammation. Otherwise, antibiotics are prescribed. The drug is selected depending on the results of the culture test. Antibacterial therapy is carried out over a course of 5 days to 2 weeks. After a month or 2, a control smear is done to ensure the effectiveness of the treatment and the absence of the pathogen. If a relapse occurs and inflammation resumes, treatment is repeated.
A course of antibiotics is the first stage of treatment, followed by the second, consisting of probiotics, antimycotic agents and restorative drugs. To normalize the composition of the vaginal microflora, Vagilak, Gynoflor, Laktogin are prescribed. Immunomodulators - Viferon, Likopid, Kagocel - will help strengthen the immune system. Maintaining the health of the intimate area is facilitated by a diet with a sufficient amount of dairy and fermented milk products and limiting sweets.
Treatment
Therapy in the case of enteroviral diseases should be as prompt as possible, since the development of bacterial infections is accelerated and is fraught with complications. It is best to start treatment no later than in the first three days of illness.
There have been many treatments for infections caused by Enterobacter aerogenes. The persistence of these Gram-negative bacteria has been well documented by the scientific community, even though antimicrobial therapy is indicated for virtually all Enterobacter infections. With some exceptions, the main classes of antibiotics used to treat E. aerogenes bacterial infections are: beta-lactams, aminoglycosides, fluoroquinolones, and trimethoprim-sulfamethoxazole.
For treatment to be effective, it is important to follow a diet!
The patient's diet should consist of:
- steamed dishes (omelettes, rabbit, veal, turkey);
- pureed vegetable soups;
- biscuits, white crackers;
- jelly, decoction of dried fruits (without sugar), green tea;
- baked apples;
- liquid mashed potatoes;
- porridge on the water.
Separately, it is worth mentioning about fluid consumption, since during illness there is a high risk of dehydration and intoxication of the body due to frequent bouts of vomiting and diarrhea.
During the day, the patient should drink little by little, but often (every half hour) and no less than 2 liters of water per day. It is better that the liquid is warm. The same applies to food: dishes should be at the optimal temperature, neither hot nor cold. Meals are fractional: 5-6 meals in small quantities. Under no circumstances should you eat:
- fatty, spicy, salty, smoked, fried foods;
- fresh vegetables and fruits;
- dairy products.
In each specific case, the doctor gives separate recommendations regarding nutrition, which must be strictly adhered to!
Such a diet should be followed for quite a long time (3-4 weeks after illness). Together with prescribed medications, maintaining proper nutrition will have a quick and positive effect, significantly speeding up the healing process.
Enterobacteriaceae in a child's stool
Enterobacteriaceae are opportunistic microorganisms, an integral part of the normal intestinal microflora. If their total number does not exceed 5% of the total, then the intestines are functioning normally. In a stool test, the normal number of enterobacteriaceae is indicated as 103. The acceptable increase is 106, corresponding to the state before illness or minor digestive disorders.
Enterobacteriaceae live in the intestines of every person, so the main route of transmission is fecal-oral. Microorganisms enter the baby’s intestines as they move along the birth canal, and with the first sip of mother’s milk, the previously sterile intestines are “populated” with normal microflora. Enterobacteriaceae belong to the so-called facultative group, the reproduction of which is activated under unfavorable conditions.
On the 3-5th day of life, almost every baby experiences transient dysbiosis - a temporary condition caused by uneven reproduction of bacteria from different groups. This is manifested by upset stool, mucus, and green stool. The general condition suffers, but with proper feeding it goes away quickly
Video - Symptoms of infection in children
If you have one or more signs, you should immediately contact your pediatrician!
Under no circumstances should you try to cure a child yourself. As a rule, the doctor prescribes the same drugs as for adults, but with a difference in dosage, depending on the weight and age of the small patient.
Parents are advised to disinfect all objects that the child comes into contact with. During illness, it is better to protect him from pets. You can’t overheat the baby or wrap him up. The best is fresh air in the room (regular ventilation) and a room temperature of about 22-23 °C.
Children's diet
If it is important for sick adults to follow all the points of treatment prescribed by the doctor, then for small patients this is a hundredfold important. It is necessary to help the fragile body that has become a victim of infection to get rid of it as quickly as possible. Therefore, you should strictly adhere to the following points:
- Water is the main thing. Dehydration occurs many times faster in children than in adults. With enteroviral diseases, the likelihood of dehydration in a small patient is very high, so parents should give him water every half hour (more than 2 liters of warm, clean water per day).
- Food temperature – 33-35 °C.
- In addition to water, you need to give your child a decoction of dried fruits, chamomile tea, fruit drinks, and jelly.
- Water and feed the baby only in small portions, fractionally, at certain intervals (food - 5-6 times a day).
- Light food. Feed your child during illness with vegetable and mashed potato soups, porridge with water (without milk!).
Hemolyzing Escherichia coli
E. coli can cause peritonitis.
Escherichia coli is the collective name for a group of more than 100 varieties of this microorganism. This microorganism can only live in an oxygen-free environment. Certain strains are human symbionts.
They live in the intestines and participate in the processes of food digestion. Some species of Escherich's bacillus are pathogens.
Prevention of pathology
The main requirement for recovery. The baby does not have the ability to resist many infections because his immune system is not yet developed enough. It is necessary to protect the baby from collisions with environmental factors that are dangerous for him. It is necessary to keep everything that the baby comes into contact with clean. This is a pacifier, toys, his own hands and body. If your baby has diarrhea, then after each bowel movement you need to not only wash him, but also wash his hands with soap. You need to swaddle and dress in such a way that the baby cannot get dirty with his secretions.
Pacifiers and chewing toys should be boiled several times a day as they are used. If this is not done, the baby will become re-infected with his own bacteria. It is better to remove pets during illness; the microbes that live in them are much more aggressive than human ones.
The air temperature in the baby's room should be between 22-23 ° C; anything higher or lower makes it difficult for the baby to thermoregulate. Optimal humidity is 40-60% (determined by a hygrometer, which is sold in every pharmacy). Overheating and stuffiness are the main mistakes of young parents.
In the modern world, being healthy is no longer just a necessity, it is fashionable and stylish, it means being in trend. That is why an increasing number of citizens are trying to lead a healthy lifestyle, instill appropriate habits in their children and regularly monitor the condition of their body by undergoing various examinations.