Pancreatic necrosis is a destructive disease of the pancreas, which is a complication of acute pancreatitis and leads to the development of multiple organ failure. Manifestations of pancreatic necrosis include acute girdling abdominal pain, persistent vomiting, tachycardia and encephalopathy. Laboratory diagnosis involves determining the level of alpha-amylase; instrumental – carrying out a survey radiography of the abdominal cavity, ultrasound, CT and MRI of the pancreas, RCCP, diagnostic laparoscopy. Treatment includes conservative measures (inhibition of proteolytic enzymes, restoration of the outflow of pancreatic juices, detoxification and pain relief) and surgery.
ICD-10
K85 Acute pancreatitis
- Causes of pancreatic necrosis
- Pathogenesis
- Classification
- Symptoms of pancreatic necrosis
- Complications
- Diagnostics
- Treatment of pancreatic necrosis Conservative therapy
- Surgery
General information
Pancreatic necrosis is the most severe complication of pancreatitis, affecting mainly young able-bodied people, accounting for 1% of all cases of acute abdomen. The pathogenesis of pancreatic necrosis is based on a failure of the mechanisms of internal protection of the pancreas from the destructive action of pancreatic enzymes.
Recently, the number of acute pancreatitis in Russia has been increasing - this pathology comes in second place after acute appendicitis in surgical hospitals. The number of destructive forms of pancreatitis, in particular pancreatic necrosis, is also growing - up to 20-25%. In different clinics, mortality due to destruction of the pancreas reaches 30-80%. The leading way to reduce mortality in pancreatic necrosis is timely diagnosis, hospitalization and early initiation of pathogenetic treatment.
Pancreatic necrosis
Causes of pancreatic necrosis
The causes of the development of both pancreatitis and pancreatic necrosis are usually diet disorders and occasional alcohol consumption. Research in the field of gastroenterology has shown that pancreatic necrosis usually affects people who are not prone to constant drinking of alcohol. However, in the vast majority of cases, the onset of pancreatic necrosis is preceded by an episode of drinking alcohol in large quantities. Patients suffering from chronic alcoholism almost always develop chronic pancreatitis, which is rarely complicated by pancreatic necrosis. The first signs of the disease may appear hours or days after the action of provoking factors.
Pathogenesis
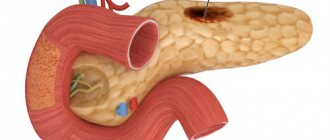
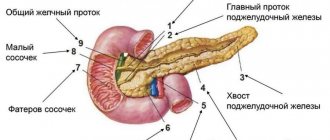
The pathogenesis of pancreatic necrosis is based on a violation of the local protective mechanisms of the pancreas. Large intake of food and alcohol leads to a significant increase in external secretion, overstretching of the pancreatic ducts, and disruption of the outflow of pancreatic juices. An increase in intraductal pressure provokes swelling of the parenchyma, destruction of the pancreatic acini, premature activation of proteolytic enzymes, which lead to massive necrosis of the gland tissue (self-digestion).
Activation of lipase causes necrosis of fat cells, and elastase causes destruction of the vascular wall. Activated enzymes and tissue breakdown products, due to the action of elastase, enter the bloodstream, causing a toxic effect on all organs and tissues. The liver, kidneys, heart, and brain are primarily affected.
Reasons for the development of necrosis
Pancreatic necrosis
Before starting treatment according to one scheme or another, it is necessary to establish the cause of this pathology. After all, if you treat only the consequences without eliminating the cause, the disease will recur.
Some diseases lead to necrosis. For example, cholecystitis, GIVP or cholangitis, manifested by impaired outflow of enzymes, often becomes such a cause. Infectious diseases lead to changes in pancreatic tissues.
The most common cause of this pathology is alcohol abuse and a diet based on junk food.
Problems with the pancreas also begin when people self-medicate and use medications uncontrollably. Only a specialist can know how the body will behave when using certain drugs. After all, the effect of medicinal components on the body is a very complex process. Stress and emotional overload also lead to necrosis of pancreatic tissue.
Classification
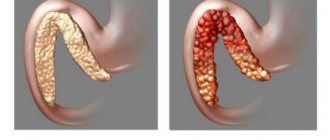
Depending on which damaging mechanisms lead in the pathogenesis, fatty, hemorrhagic and mixed forms of pancreatic necrosis are distinguished.
- Fat form. If increased lipase activity predominates, destruction of pancreatic adipose tissue occurs. Lipase enters beyond the pancreatic capsule, causing the appearance of foci of necrosis in the greater and lesser omentum, peritoneal layers, mesentery, and internal organs. The fatty form of pancreatic necrosis usually ends in the development of severe chemical aseptic peritonitis and multiple organ failure.
- Hemorrhagic form. In the case of a predominance of microcirculatory disorders, a spasm of pancreatic vessels develops, leading to a rapid increase in parenchymal edema. Over the course of several hours or days, toxemia gradually leads to paresis of the vascular wall, dilation of blood vessels and slowing down of blood flow in the tissues of the gland. All this contributes to increased thrombus formation, and subsequently to the development of ischemic necrosis. Activation of elastase causes destruction of the vascular wall, first in the thickness of the pancreas, then in other organs. Ultimately, this leads to hemorrhagic penetration of the pancreas, hemorrhages into the internal organs and retroperitoneal tissue. A sign of hemorrhagic pancreatic necrosis is effusion into the abdominal cavity mixed with blood.
- Mixed form. If the activity of elastase and lipase is approximately at the same level, a mixed form of pancreatic necrosis develops. In this case, the phenomena of fat necrosis and hemorrhagic imbibition are expressed equally. With pancreatic necrosis, the level of alpha-amylase also increases significantly, but this fact does not play any role in the pathogenesis. Measuring amylase levels is of clinical significance only.
2. Causes of steatopancreatitis
Potentially dangerous factors that threaten pancreatic lipomatosis are conventionally divided into two groups: toxic and metabolic.
Toxic exposure, especially long-term, leads to the destruction of healthy pancreatic cells. To preserve the volume and maintain the geometry of the organ, a mechanism is activated to replace them with adipose tissue. The growth of fatty layers in the thickness of cells capable of functioning normally affects the activity of the entire organ, which gradually loses its functional viability.
The most common factors of toxic effects on the pancreas:
- long-term nicotine intoxication;
- systematic use of alcohol;
- taking certain medications that strain the pancreas.
Metabolic factors for the most part can be controlled and adjusted. These are excess weight, diet, food intake, nutritional balance, physical activity. The category of metabolic factors beyond human control includes chronic diseases of the gastrointestinal tract and liver, and diabetes mellitus. Steatopancreatitis can develop secondary to their background.
Recently, fasting and extreme diets have also been identified as risk factors. Sharp changes in the volume of incoming food stimulate the processes of fat accumulation in organs and tissues when conditions favorable for this occur.
Some types of medical care can also precipitate steatosis (eg, intravenous nutrition), but in most cases where intravenous nutrition is prescribed, there is no alternative.
Visit our Gastroenterology page
Symptoms of pancreatic necrosis
The development of the pancreatic necrosis clinic occurs in three stages. This condition may be preceded by purulent pancreatitis, acute alcoholic pancreatitis, biliary pancreatitis, hemorrhagic pancreatitis. At the first stage, the active proliferation of bacteria in the pancreas causes severe toxinemia and increased pancreatic enzymatic activity. The patient is worried about fever, vomiting, and stool instability. At the second stage of the disease, purulent and enzymatic melting of the gland tissue occurs with the formation of one or more cavities. At the last stage, the inflammatory process spreads to surrounding tissues, leading to multiple organ failure and death of the patient.
The disease has an acute onset; usually patients clearly associate the appearance of the first symptoms with errors in diet and alcohol intake. About 70% of patients are admitted to the hospital in a state of severe alcohol intoxication, which indicates a very rapid development of pathological changes in the pancreas.
The first symptom is usually acute girdling pain, radiating to the left half of the abdomen and lower back, and left shoulder. There are no painless forms of pancreatic necrosis. There is a direct relationship between the severity of pain and the severity of pancreatic necrosis. The spread of destructive changes to nerve endings leads to a gradual decrease in pain; in combination with persistent intoxication, this is a poor prognostic sign.
Some time after the onset of pain, uncontrollable vomiting develops, which is not associated with food intake and does not bring relief. The vomit contains bile and blood clots. Due to vomiting, dehydration develops, manifested by dry skin and mucous membranes, the tongue is coated, and the rate of diuresis gradually decreases. Intestinal flatulence develops, peristalsis is weakened, and gas and stool retention is noted. Intoxication and dehydration are accompanied by fever.
Toxemia, fluctuations in blood glucose levels, and hyperfermentemia lead to brain damage and the development of encephalopathy, which is expressed by confusion, agitation, disorientation, and even the development of coma (in about a third of patients).
The progression of the inflammatory process leads to a significant increase in the pancreas in size and the formation of an infiltrate in the abdominal cavity. Already by the fifth day from the onset of the disease, the infiltrate can not only be palpated, but also visible with the naked eye. Skin hyperesthesia appears in the projection of the pancreas.
Material and methods
This comparative prospective study included 152 patients aged 23 to 59 years who were treated in the Department of Surgery of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency of Russia in the period from 2001 to 2012 with a clinical diagnosis of PN.
The main group consisted of 92 patients. In the early stages of the disease, the main goal of the interventions was sanitation and drainage of the abdominal cavity and (or) limited fluid accumulations of the retroperitoneal space as a method of surgical detoxification when conservative therapy was ineffective (endovideosurgical or percutaneous puncture-drainage techniques were used). Identification of infected PN and parapancreatic abscesses served as an absolute indication for their drainage, which was performed percutaneously or lumboscopically (mini-access). If minimally invasive techniques were ineffective, traditional open interventions were performed.
Depending on the stage of PN and types of complications, patients underwent various options and combinations of surgical interventions. Minimally invasive operations were the final type of surgical treatment in 39 (42.4%) patients; these patients underwent a total of 128 minimally invasive surgical interventions, including diagnostic operations (diagnostic video laparoscopy, diagnostic punctures under radiation control). In 47 (51.1%) patients, combined surgical treatment was performed, namely: a combination of minimally invasive techniques and open operations. Open operations, without the use of minimally invasive techniques, were performed in 6 (6.5%) patients. Indications in these cases were widespread purulent peritonitis and retroperitoneal phlegmon.
In the phase of pancreatogenic toxemia and sterile PN, minimally invasive surgical interventions were performed in 79 (91.9%) patients. Indications for surgery were the progression or persistence of symptoms of intoxication and MODS in accordance with the SAPS scale. In the phase of infected pancreatic necrosis, minimally invasive interventions were performed in 7 (8.1%) patients; the remaining patients in this stage of pancreatitis were operated on in an open manner.
In the complex treatment of patients in the main group, in addition to minimally invasive surgical methods, a device for prolonged regional anesthesia Smartinfuser Pain Pump, an ultrasonic cavitator Sonoca-190, a Prizma Flex device for low-flow hemofiltration, and a Rematerp device for conducting sessions of structural resonance therapy (SRT) were used.
The comparison group included 60 patients. Of these, 42 underwent video laparoscopy and traditional open surgery, and 18 underwent laparotomy only. Both study groups were comparable in terms of gender, age, duration of the disease and main clinical and laboratory parameters.
In the main group there were 69 men (75%) and 23 women (25%), average age - 47.3±3.8 years. The comparison group consisted of 41 (68.3%) men and 19 (31.7%) women, average age - 52.4±4.7 years. In the main group (92 patients), 31 patients were admitted to the hospital within the first 3 days from the onset of the disease, 48 from 3 to 7 days, 9 from 7 to 14 days, and 4 after 14 days. In the comparison group, patients over the above time periods were distributed as follows: 22, 29, 6 and 3, respectively. The etiological factors that caused PN in patients of the main group were nutritional (error in diet, alcohol consumption) - 64 (69.6%) and biliary (pathology of the biliary tract) - 28 (30.4%). In the comparison group - 39 (65%) and 21 (35%), respectively.
The clinical diagnosis was established on the basis of anamnesis, clinical picture of the disease, data from instrumental and laboratory examinations, as well as video laparoscopy or laparotomy.
Of the instrumental diagnostic methods, all patients in both groups used chest radiography and plain radiography of the abdominal organs, ultrasound of the abdominal cavity and retroperitoneal space, computed tomography (CT) with bolus contrast enhancement, and electrocardiography. According to indications, esophagogastroduodenoscopy (EGDS) and endoscopic interventions on the major duodenal papilla and common bile duct (papillosphincterotomy, endoscopic lithextraction, nasobiliary drainage), and videolaparoscopy were performed. Radiation diagnostics and minimally invasive surgeries were performed using a Philips IU 5000 device and a General Electric 64-slice High Speed computed tomograph. Videolaparoscopic interventions were performed using a video complex and instruments. In all observations, in addition to general laboratory research methods, the levels of C-reactive protein and procalcitonin were determined over time.
As the first stage of surgical treatment, videolaparoscopy was performed in 73 (79.3%) patients in the main group and 42 (70%) patients in the comparison group. In addition to the diagnostic factor, laparoscopy was of a therapeutic nature, including sanitation and removal of toxic effusion from the abdominal cavity and omental bursa, installation of drains in the abdominal cavity, catheterization of the round ligament of the liver and subsequent administration of analgesic solutions. In addition, in 16 patients, percutaneous transhepatic drainage of the gallbladder was performed during laparoscopy to eliminate biliary hypertension.
The severity of PN upon admission to the hospital was assessed using the integral scales Ranson, Apache-II, as well as according to computed tomography data in the Balhtasar system. Heavy P.N. in the main group it was established in 34 (37%) patients, moderate severity - in 58 (63%). In the comparison group - in 23 (38.3%) and 37 (61.7%) patients, respectively.
Complex conservative treatment in both groups included individual treatment tactics for the disease depending on its etiology (autonomic or biliary), pain relief (epidural anesthesia), intubation and aspiration of gastric contents, nutritional support, intensive therapy (aimed at restoring hemodynamics, rehydration, correction disorders of the acid-base state, maintaining an optimal level of oxygen delivery), blockade of the secretory function of the pancreas (octreotide), antibacterial and antiulcer therapy, methods of extracorporeal detoxification (Fig. 1).
Rice. 1. Scheme of therapeutic tactics for pancreatic necrosis depending on the etiology of the disease. AP - acute pancreatitis; Ultrasound - ultrasound examination; EGDS - esophagogastroduodenoscopy; CT - computed tomography; MRCP—magnetic resonance cholangiopancreatography; MSDPC - major duodenal papilla.
The effectiveness of treatment of patients with PN in the main group was assessed by comparing the duration of clinical manifestations, the dynamics of laboratory and instrumental parameters, the number of complications and deaths, and the length of the patient’s stay in the hospital relative to those in the comparison group.
All digital material was processed statistically using the Statistica 6.0 software package (Stat-Soft, 2001). The results were considered significant at p
<0,05.
Complications
These pathological changes in the body lead to the formation of multiple organ failure against the background of severe toxic hepatitis, nephritis, carditis, and respiratory disorders. Pancreatic necrosis can be complicated by shock, peritonitis, abdominal abscess, and gastrointestinal bleeding.
Local complications often include abscess, cyst or false cyst of the pancreas, enzyme deficiency, fibrosis of the pancreas, phlegmon of the retroperitoneal tissue, gastrointestinal ulcers, thrombosis of the portal and mesenteric veins.
Diagnostics
The patient should be examined jointly by a gastroenterologist, surgeon, and resuscitator. The presence of pancreatic necrosis implies extreme severity of the patient's condition, therefore, in all cases, hospitalization in the intensive care unit is recommended. The department constantly determines pancreatic enzymes in the blood and urine. A poor prognostic sign is a progressive increase in amylase levels or a sharp jump in this indicator.
On physical examination, abdominal distension is noted, bluish spots appear on the lateral surfaces of the anterior abdominal wall and lower back (manifestation of internal hematomas, hemorrhages into soft tissues). The skin is earthy-pale or icteric, marbled, cold. Tachycardia, arterial hypotension, rapid shallow breathing are a sign of severe intoxication. The diagnosis is confirmed using:
Differential diagnosis is carried out with intestinal obstruction, acute inflammatory diseases of the appendix, gallbladder, biliary colic, perforation of a hollow organ, thrombosis of mesenteric vessels, myocardial infarction, rupture of an abdominal aortic aneurysm.
CT OBP. Pancreatic necrosis. Diffuse edema and disruption of the structure of the pancreas, lack of accumulation of contrast in its parenchyma.
Discussion
Our experience in the surgical treatment of PN confirms the data of other authors [2, 4, 6, 12], that when determining indications for surgery, it is necessary to be guided by the entire complex of clinical, laboratory and especially instrumental visualization (ultrasound, CT, laparoscopy) data on the dynamics of the disease and conservative treatment. Sterile forms of PN, complicated by the development of enzymatic peritonitis, serve as an absolute indication for laparoscopic sanitation and drainage of the abdominal cavity. Laparotomic surgical intervention undertaken on an emergency basis for enzymatic peritonitis in the pre-infectious phase of the disease should be considered an erroneous and unjustified therapeutic measure [1, 5, 16].
When an infected PN is formed in combination with an abscess, when the area of destruction in the retroperitoneal space is comparable to the liquid component of the purulent-necrotic lesion, at the first stage of surgical treatment, minimally invasive technologies can be used in the form of percutaneous drainage of the purulent-necrotic lesion under ultrasound or CT control (Fig. 7). This tactic makes it possible to perform laparotomy intervention in a delayed manner (at 2-3 weeks of the disease and even later), when optimal conditions are created for delimiting zones of necrosis, sequestration and viable tissues [10, 17].
Rice. 7. Fistulogram of a parapancreatic abscess after percutaneous drainage under ultrasound guidance.
Percutaneous drainage of pancreatogenic abscesses of various locations in the retroperitoneal space seems to be the optimal method for their surgical treatment in situations where the volume of necrosis is minimal or absent, and the abscess cavity does not contain putty-like detritus that provokes constant obstruction of the drains. Methods of minimally invasive surgical interventions also have undoubted advantages in cases where limited fluid formations are formed at various times after laparotomy operations, especially after repeated sanitation interventions [6, 10, 18].
At the same time, we consider it necessary to note the danger of exaggerating the importance of percutaneous drainage interventions as the main method of treatment for those forms of infected PN in which there is long-term and extensive sequestration. In such situations, in order to achieve a therapeutic effect, in our opinion, one should lean in favor of traditional laparotomy intervention.
In recent years, methods of laparoscopic pancreatomentobursoscopy and sanitation of the omental bursa have been actively used [7, 19]. Using endoscopic technology, laparoscopy, decompression of the pancreas, sanitation and drainage of the abdominal cavity are performed, and then, using specially designed instruments from a minilaparotomy access, the pancreas is examined, its abdominization, necro- and sequestrectomy and a pancreatomentobursostomy and/or lumbostomy is formed. Subsequently, staged sanitation is performed, and between operations, flow-through or fractional lavage of the cavity of the omental bursa is performed through drainages (Fig. 8). The obtained results of treatment of patients in the main group prove the effectiveness of ultrasonic cavitation of purulent cavities (Fig. 9). As an acoustic medium, it is preferable to use 0.02% chlorhexidine solution, 0.9% sodium chloride solution, 0.25-0.5% novocaine solution and mixtures thereof. The bactericidal effect of the method is due to the damaging effect of the ultrasonic wave on the microbial cell, the formation of chemical compounds that have a detrimental effect on microorganisms, and a decrease in the antibiotic resistance of wound infection pathogens. Ultrasound stimulates intracellular biosynthesis and regenerative processes, causes dilation of blood vessels and an increase in regional blood flow by 2-3 times, initiates favorable changes in the microvasculature and vascular adventitia, the development of collaterals, which is very important in inflammatory and purulent-destructive processes [5, 15] .
Rice. 8. Areas of the retroperitoneal space drained through various mini-accesses. 1 - bursostomy (parapancreatic, mesocolon), 2 - lumbostomy (parapancreatic, mesocolon, retrocolytic), 3 - retroperitoneostomy (retrocolytic).
Rice. 9. Ultrasonic cavitator Sonoca-190 for treating purulent cavities.
Adequate sanitation and drainage of pathological foci, combined with low surgical aggression of access during these interventions, provide advantages compared to treatment with traditional methods.
Another factor determining a more favorable course of the postoperative period was the minimal destruction of anatomical and physiological barriers around pathological foci, which entails a lesser increase in endogenous intoxication compared to that during open operations.
An important role in adequate pain relief, stimulation of intestinal motility, and earlier activation of patients belongs to the Smartinfuser Pain Pump infusion device, which provides prolonged slow administration of a local anesthetic solution through an irrigation catheter directly into the wound (Fig. 10). Of the numerous methods of extracorporeal detoxification, in our opinion, low-flow hemofiltration using the Prizma Flex device turned out to be the most effective (Fig. 11).
Rice. 10. Device for prolonged regional anesthesia Smartinfuser Pain Pump with an irrigation catheter placed in the retroperitoneal space.
Rice. 11. General view of the Prizma Flex device for low-flow hemofiltration.
Promoting the widespread use of minimally invasive operations in the treatment of patients with destructive pancreatitis, we believe that if they are ineffective, open interventions are reserve operations. At the same time, the use of minimally invasive technologies in combination with conservative therapy in patients of this category makes it possible to enhance the detoxification effect, stabilize the condition of patients and perform open operations in more favorable conditions, which once again emphasizes the need for the use of the considered methods, especially at the initial stage of treatment of the disease.
We agree with the opinion of E. Bradley (USA, 1992) that “there are not many other diseases that require the doctor to have the same flexibility in diagnosis and treatment that is necessary for a clinician caring for a patient with acute pancreatitis.” Therefore, its treatment must be comprehensive and proactive, and effective surgical techniques must be combined with adequate conservative therapy and rehabilitation.
Considering the main links in the pathogenesis and phases of the course of PN, as well as taking into account the proven capabilities of the CRT method in relieving edema, improving microcirculation, normalizing intestinal tone and function, restoring the normal (genetically determined) functioning of the autonomic nervous system, we can recommend the use of the CRT method in complex treatment patients with PN [20].
The CRT technique for this disease is pathogenetically justified (promotes earlier resolution of intestinal paresis and reduces the pathological effect of intestinal microflora on the pancreas) in acute pancreatitis, is simple to perform, safe and does not require large financial costs (Fig. 12).
Rice. 12. Rematerp device for conducting structural resonance therapy sessions.
Currently, the process of revising diagnostic and treatment programs for PN continues, which is due to the emergence of modern highly informative diagnostic methods, new medications and effective minimally invasive surgical techniques.
Treatment of pancreatic necrosis
Conservative therapy
Treatment of pancreatic necrosis begins with providing complete rest to the inflamed pancreas. Physical activity and enteral nutrition are excluded, and gastric lavage with cool solutions may be prescribed. The main areas of treatment are pain relief, neutralization of proteolytic enzymes, and detoxification therapy.
- Analgesia. Adequate pain relief includes the administration of analgesics (narcotics if necessary), antispasmodics, dissection of the pancreatic capsule, and novocaine blockades. Reducing the swelling of the gland under the influence of diuretics leads to the fading of the pain syndrome (as it leads to a weakening of the tension of the pancreatic capsule).
- Infusion therapy. Detoxification is carried out with a large number of infusion solutions under the control of diuresis. Aprotinin is added to the infusion solution. Antihistamines are required.
- Antibiotic therapy. In order to prevent purulent complications, antibacterial therapy with broad-spectrum antibiotics is carried out. Symptomatic treatment includes anti-shock measures, restoring the function of other organs and systems.
Surgery
In almost all cases of pancreatic necrosis, surgical treatment is required to restore the outflow of pancreatic juices and remove necrotic masses (pancreatic necrectomy). In the first five days from the onset of the pathological process, surgical intervention is not recommended, since during this period it is still impossible to assess the level of necrosis, but the risk of secondary infection and postoperative complications increases.
At the stage of purulent inflammation in the abdominal cavity, various techniques (puncture, laparoscopic, laparotomic) can be used to restore the outflow from the pancreatic ducts; elimination of necrotic masses, inflammatory and hemorrhagic exudate; stopping intra-abdominal bleeding. To improve the condition of the internal organs, abdominal drainage may be required.
results
Of the 92 patients with PN in the main group, complex treatment using minimally invasive techniques turned out to be effective and sufficient in 39 (42.4%); 47 (51.1%) patients underwent open surgery after minimally invasive interventions. In the comparison group, only video laparoscopic interventions were performed in 11 (26.2%) patients out of 42, and 31 (73.8%) underwent combined surgical treatment (video laparoscopy + laparotomy or lumbotomy).
Upon admission of patients with a clinical picture of PN, the treatment and diagnostic algorithm, depending on the nature of the course of the disease, consisted of the following stages: 1) determination of the prevalence of the destructive process in the pancreas, the presence or absence of peritonitis; 2) identifying the degree of involvement of parapancreatic tissue and retroperitoneal space in the inflammatory process; 3) determination of the severity of MOF syndrome; 4) detection of infection.
The main indications for videolaparoscopic interventions were enzymatic peritonitis, the presence of free fluid in the abdominal cavity and according to radiological diagnostic methods; sterile pancreatic necrosis with progressive MODS on the background of adequate intensive therapy.
In both groups, laparoscopic sanitation with drainage of the abdominal cavity was performed in 115 (75.7%) of 152 patients (Fig. 2). The main areas of drainage were the right hypochondrium and the pelvic cavity. In 42 (36.5%) cases, the presence of pathological exudate in the cavity of the lesser omentum necessitated its opening, followed by aspiration of the effusion and drainage. Due to the spread of the pathological process to the retroperitoneal tissue, in 22 (19.1%) patients there was a need to open and drain the retroperitoneal space with mobilization of the colon.
Rice. 2. Laparoscopic transhepatic cholecystostomy, sanitation and drainage of the abdominal cavity for pancreatic necrosis (endophoto).
In the presence of biliary hypertension, a tense and enlarged gallbladder, and without signs of choledocholithiasis, laparoscopic cholecystostomy was performed during surgery in 26 (22.6%) patients (Fig. 3). In other cases, if necessary, percutaneous transhepatic cholecysto- or cholangiostomy was performed under ultrasound guidance. There were no complications directly related to videolaparoscopic operations.
Rice. 3. Intraoperative view of percutaneous transhepatic cholecystostomy performed during laparoscopy.
In the main group, minimally invasive technologies using radiation navigation were carried out at all stages of treatment of PN and in all phases of the disease in order to reduce the factor of surgical trauma. Diagnostic percutaneous puncture intervention made it possible to determine the presence of bacterial contamination, assess the extent of the destruction process and did not aggravate the endotoxin shock present in patients.
Indications for puncture and drainage therapeutic percutaneous interventions for PN were considered: 1) limited fluid accumulations in the abdominal cavity, omental bursa, and retroperitoneal space; 2) developing postnecrotic pseudocysts with a diameter of more than 5 cm; 3) abscesses of the abdominal cavity and retroperitoneal space; 4) signs of biliary hypertension.
The experience gained shows that the combination of controlled percutaneous drainage of necrotic foci with multiple large-diameter drains with regular replacement of drains with an increase in their diameter, aggressive irrigation of foci and necrectomy through the lumen of retroperitoneostomy makes it possible in most cases to avoid open operations (Fig. 4). The use of minimally invasive procedures makes it possible to eliminate septic manifestations and subsequently choose a more appropriate time for open surgical intervention in the context of demarcation of necrotic tissues of the pancreas and retroperitoneal space.
Rice. 4. Sanitation and drainage of retroperitoneal tissue through burso- and lumbostomies. a — computed tomogram in the sagittal plane, widespread lesion of the retroperitoneal tissue (arrows); b — general view of the same patient after the formation of burso- (1) and lumbostomy (2).
If fluid was detected in the cavity of the lesser omentum, parapancreatic, paracolar tissue, or in the abdominal cavity, a diagnostic puncture was performed, the purpose of which is to determine contamination and remove toxic exudate. To assess the degree of infection of the exudate, a bacterioscopic and bacteriological study was carried out with an assessment of sensitivity to antibacterial drugs.
In the case of limited fluid accumulations in the cavity of the lesser omentum or retroperitoneal space of more than 5 cm, short-term drainage was used for a period of 2 to 3 days, with a drainage lumen of 12-15 Fr (4-5 mm). The condition of the abdominal cavity and retroperitoneal space was monitored daily using ultrasound, and in case of difficult visualization - X-ray computed tomography (X-ray computed tomography) or magnetic resonance imaging.
When performing drainage percutaneous operations, the following methods were used: stylet-catheter (one-stage), two-stage, trocar. The choice of drainage technique was carried out depending on the topography, size and nature of the pathological focus. Primary drainage was performed with 12-15 Fr drains. On days 3-4, drains were replaced with a clearance of 16-18 Fr and then up to 30 Fr.
To drain the retroperitoneal space without contact with the abdominal cavity, the trocar method was preferred, which allows for the immediate installation of large-diameter drains and retroperitoneostomy “sleeves”. Laparoscopic examination, sanitation of the retroperitoneal space and removal of sequesters were performed through the retroperitoneostomy openings. This type of surgical intervention was performed in 27 (29.3%) patients from the main group, while in 9 patients the intervention was performed 2 to 4 times.
In abscesses with a volume of more than 100 ml, 2 or more drains were usually installed. Most patients underwent drainage immediately from various points, which were selected taking into account the greatest possible coverage of the drained volume and the adequacy of drainage (Fig. 5). Subsequent replacement of drains with a larger diameter allowed maintaining adequate drainage. In the presence of sequesters, they were replaced with drainages with a lumen of up to 30 Fr, which made it possible to remove large fragments of necrotic tissue.
Rice. 5. Appearance of patient K., 48 years old, after puncture and drainage interventions for left-sided type of purulent parapancreatitis.
Despite the advantages of the method (no need for general anesthesia, minimal surgical aggression, the possibility of performing interventions through hollow organs), the implementation of such operations in cases of predominance of the tissue (or solid) component over the fluid part of the cavity was limited. Complications in this group of patients occurred in 6 (4.8%) patients: external and internal intestinal fistulas - in 3, dislocation of cholecystostomy - in 1, and intraperitoneal bleeding - in 2 (Fig. 6).
Rice. 6. Fistulograms. a — communication of the parapancreatic purulent cavity with the descending colon; b — communication of the parapancreatic purulent cavity with the duodenum.
The main problem limiting the use of minimally invasive techniques was the massive involvement of retroperitoneal tissue in the infiltrative process, sequestration in destruction cavities, and the formation of hourglass-type cavities, which in some cases did not allow adequate drainage or replacement of drains through a guidewire under X-ray control. In such a situation, the technique of flexible fiber fistuloscopy of drained cavities was used. Under visual and radiological control in 14 patients (after percutaneous and lumboscopic drainage), fragmentation and removal of sequesters, bougienage of external and internal fistula tracts with more adequate installation of drains were carried out using an endoscope. The operation was performed under local anesthesia using a fistuloscope with a diameter of 7 mm. In all cases, the technique was effective and no additional drainage surgery was required.
In 13 (16.8%) patients with formed foci of destruction, an original minimally invasive technique was used - lumboscopic opening, sanitation and drainage with wide-lumen drainages under ultrasound control and using laparoscopy. This operation made it possible to fully inspect the retroperitoneal space, open, sanitize and adequately drain pathological foci under instrumental and visual control. In 4 patients, the cavities were localized in the area of the head of the pancreas—accordingly, the operation was performed through the right lumbar region; in the remaining 9 patients, destructive foci were located in the area of the tail and body of the gland—access through the left lumbar region. In all cases of opening the cavities, purulent contents were obtained; in 5 patients, the source of destruction was infected pancreatic necrosis with a large amount of detritus and large sequestration; in 8 patients, the operation was performed for peripancreatic abscesses.
After drainage, active local and general treatment was carried out. Preserving the integrity of the parietal peritoneum excluded the spread of the purulent process into the abdominal cavity, which had a positive effect on the course of the postoperative period in the form of less intoxication, rapid cleansing of destruction cavities, and the absence of specific complications (adhesive intestinal obstruction, small intestinal fistulas, abdominal abscesses). Control over the dynamics of the condition of the drained cavities and their sizes was carried out using ultrasound, dynamic fistulography with replacement and more adequate installation of drains on demand. In the postoperative period, incomplete external colonic fistulas formed in 2 patients, which did not require repeated surgical interventions.
The general results of treatment of patients with PN are presented in the table.
The main results of complex treatment of patients with pancreatic necrosis
Analysis of the results showed that the main reason for the ineffectiveness of minimally invasive treatment was the total spread of infected PN in the retroperitoneal space with a predominance of the dense tissue component, and this made it difficult to perform adequate sanitation using minimally invasive techniques. In all cases, the main cause of death in both groups was the progression of MODS against the background of purulent-septic complications.
Prognosis and prevention
Making a prognosis for patients with pancreatic necrosis is a very difficult task, as it depends on many circumstances. The prognosis is significantly worsened in the presence of one or more of the following factors: age over fifty-five years, leukocytosis more than 16x109/l, hyperglycemia, hypocalcemia, metabolic acidosis, arterial hypotension, increased levels of urea, LDH and AST, significant loss of fluid from the bloodstream into the tissue . The presence of seven of these criteria ensures 100% patient mortality. Prevention of pancreatic necrosis involves timely seeking medical help and early initiation of treatment, including surgery.