Conjugation jaundice is not an independent disease. This is an external symptom indicating specific processes in the body.
Typically, this condition appears in newborns due to the immaturity of the digestive system, especially in premature babies. The yellow color of the skin is due to excess amounts of bilirubin (a breakdown product of hemoglobin).
In the first days of a baby’s life, his digestive system undergoes a restructuring to a new type of nutrition. Metabolism proceeds more slowly, so bilirubin does not have time to be excreted from the liver.
Conjugation jaundice is also called physiological jaundice; as a rule, it goes away after the first week of the child’s life. It should be differentiated from pathological, which can develop as a result of various diseases. This type of jaundice also occurs in adults suffering from liver disease.
What is it and what causes it?
If the yellowness does not go away within 2-3 weeks, then there is cause for concern.
Conjugative jaundice of newborns is a condition that arose during the process of adaptation of the child to new living conditions.
In the baby’s blood, fetal hemoglobin is replaced by hemoglobin A, which is formed as a result of the exchange; due to the immaturity of the liver, bilirubin accumulates in the tissues and turns the skin yellow.
The yellowness is most pronounced on the 3-4th day of life; gradually, as the enzyme systems work, the yellowness disappears on the 8-9th day. If jaundice does not go away within 2-3 weeks, then they speak of a protracted conjugative form.
This condition is dangerous, since excess bilirubin leads to disruption of the central nervous system.
Risk factors for the development of prolonged jaundice include:
- poor maternal nutrition during pregnancy;
- lack of iodine in the mother's body;
- bad habits of women;
- taking certain medications during pregnancy;
- poor environmental conditions;
- mother's diabetes.
Prolonged jaundice requires examination of the child by a specialist in order to differentiate it from pathological jaundice, which can be of the following types:
| Hemolytic | Occurs due to the accelerated breakdown of red blood cells in the child’s blood |
| Parenchymatous | Is a consequence of infectious liver diseases |
| Obstructive | Appears due to disruption of the bile outflow process |
If conjugation jaundice is a physiological condition and resolves within 10 days, then pathological jaundice requires immediate treatment.
Reasons for appearance
Conjugation jaundice may appear due to uncontrolled use of medications that lead to disruption of liver function. Also causes of jaundice in adults are:
- Gilbert-Meulengracht syndrome;
- liver tumors;
- gallstones.
The following pathologies contribute to the occurrence of prolonged jaundice in newborns:
- Kligler-Najjar syndrome. Characterized by hereditary deficiency of enzymes that process bilirubin.
- Breast milk jaundice. If breast milk contains an increased amount of estrogen and other substances that slow down the absorption of bilirubin. To normalize the child’s condition, it is recommended to stop breastfeeding.
- Congenital endocrine diseases associated with decreased synthesis of thyroid hormone.
- Incompatibility of the Rh factor of mother and child.
- Prescribing medications : chloramphenicol, vitamin K, salicylic acid.
Research
When evaluating a newborn with jaundice, consideration should be given to the pregnancy history, gestational age and postnatal age of the infant, as well as the initial physical examination. It is important to note whether any drugs or toxins may have contributed to its occurrence, as well as the race of the parents.
For any infant with jaundice, 2 questions need to be answered.
- Is it possible that unconjugated hyperbilirubinemia will cause neurological damage?
- Is there bound bilirubin?
Conjugated bilirubinemia is likely due to more serious causes, which in the case of biliary atresia should be quickly diagnosed and surgically treated early.
Repeat complete plasma bilirubin assessments should be performed in infants with rapid and early rises in (unconjugated) bilirubin so that treatment for hyperbilirubinemia can be instituted. Urine bilirubin indicates that the conjugated fraction of bilirubin should be evaluated in the laboratory, and the causes of conjugated bilirubinemia should be considered. Table 13.1 lists possible causes of jaundice that occur at different times during the neonatal period.
Table 13.1. Possible causes of jaundice occurring at different times in the neonatal period.
Day
| Unconjugated jaundice | Conjugated jaundice | |
| 1 | Hemolytic disease is suspected until proven otherwise | Neonatal Rubell's hepatitis CMV Syphilis |
| 2-5 | Hemolysis Physiological jaundice of prematurity G-6-P dehydrogenase deficiency Spherocytosis | Same as in point 1 |
| 5-10 | Sepsis Jaundice due to breast milk Galactosumia Hypothyroidism Drugs | Same as in point 1 |
| 10+ | Sepsis Urinary tract infection | Biliary atresia Neonatal hepatitis Choledochal cyst Pyloric stenosis |
The approach to diagnosing neonatal jaundice is shown in Fig. 13.3.
Rice. 13.3 Diagram demonstrating the diagnostic approach to neonatal jaundice. (Modified from Maisels 1994).
Signs and manifestations
Conjugation jaundice is usually limited to yellow discoloration of the skin and sclera. This does not pose a danger to the child and goes away on its own.
Too high a level of bilirubin can cause deterioration of the child’s condition, which manifests itself in:
- Weak sucking reflex.
- Increased sleepiness.
- Vomiting.
- Cramps.
- Throwing back the head.
In this situation, a complete examination of the baby is required. Increased bilirubin levels can lead to kernicterus (bilirubin encephalopathy). This condition poses a danger to the newborn, as it provokes serious developmental defects: deafness, mental retardation, paralysis.
If pathological jaundice develops, the child will experience the following symptoms:
- darkening of urine;
- stool lightening;
- enlarged liver;
- abdominal pain when pressed;
- the appearance of hematomas on the baby’s skin.
These symptoms require immediate examination and specific treatment.
Research
In cases where prolonged jaundice is observed, lasting more than 14 days in a full-term infant and 14 days in a premature infant, additional studies should be performed. An initial investigation should be conducted to distinguish conjugated from non-conjugated causes. Table 13.3 lists studies for long-term unconjugated hyperbilirubinemia.
Table 13.3. Studies conducted in an infant with long-standing unconjugated hyperbilirubinemia.
| Direct and indirect bilirubin Hemoglobin Blood smear for the morphology of red blood cells Blood type of mother and baby Direct Coombs test Maternal hemolysis in case of ABO incompatibility Screening for infection Substances that reduce urine volume Action of galactose-uracil transferase of erythrocytes, if there is a possibility of galactosemia Glucose-6 analysis -phosphate T4 and TSH plasma |
Diagnostics
In order to determine what type of jaundice the baby has, the doctor prescribes a differential diagnosis. Usually the child is given:
- general analysis of blood, urine, feces;
- study of bilirubin concentration in the blood;
- determination of osmotic resistance of erythrocytes;
- measuring the level of total protein in the blood;
- proteinogram.
To compare bilirubin concentrations, you can use the following table:
An ultrasound of the liver and spleen is also done to determine the size of the organs and the presence of pathological changes in them.
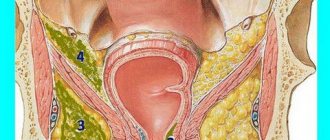
Parenchymal jaundice
It develops when liver cells are damaged by infectious or toxic agents, which leads to a decrease in their ability to bind bilirubin. In the first place in this series are intrauterine infections: cytomegalovirus (it is the cause of approximately 60% of all cases of prolonged jaundice in infants), toxoplasmosis, listeriosis, rubella, viral hepatitis. As a rule, the idea of an intrauterine infection arises with the development of prolonged jaundice (when its duration exceeds 2-3 weeks in full-term newborns and 4-5 weeks in babies born prematurely), as well as in the presence of other symptoms (enlargement of the liver, spleen and peripheral lymph nodes , anemia (decrease in the level of hemoglobin in the blood), darkening of urine and discoloration of feces, signs of inflammation in a general blood test (increased number of leukocytes, increased ESR), increased levels of liver enzymes in a biochemical blood test. To make a diagnosis, serological reactions are used (detection in the blood antibodies to viruses or bacteria), detection of RNA or DNA of the pathogen using PCR (polymerase chain reaction is a method that allows you to “recreate” DNA or RNA from small fragments that are found in biological fluids or tissues of the body. After this, the resulting RNA or DNA is examined for species (i.e. determine the type of pathogen).
Treatment
This is what the phototherapy procedure looks like
In the case of physiological jaundice, no specific treatment is required. If the baby is breastfed, then gradually his digestive tract begins to work normally, the level of bilirubin returns to normal and the skin acquires a soft pink tint.
If the tests reveal that the level of bilirubin is too high , the child can be helped to cope with this condition with the help of:
- phototherapy, that is, irradiation with an ultraviolet lamp. With its help, bilirubin is converted into another enzyme, which is excreted much more easily;
- infusion therapy (intravenous administration of saline solutions);
- taking barbiturates that promote accelerated excretion of bilirubin.
Treatment of pathological jaundice depends on the cause of its occurrence. If the child's condition is serious, a blood transfusion is required.
In adults, therapy consists of treating the primary disease. If jaundice has developed as a result of taking medications, these medications should be discontinued and the patient’s condition will return to normal. In case of gallstones or tumor processes, the issue of surgical intervention is resolved.
Bilirubin production
During the day, most bilirubin is produced from aging cells. Red cells are destroyed in the reticuloendothelial system and heme is converted to free bilirubin. One gram of hemoglobin yields 600 m mol (35 mg) of unbound bilirubin. Hemolysis may increase with maternal intake of drugs such as salicylates, sulfonamides, phenacytin and furadantin. Twenty-five percent of daily bilirubin production comes from sources other than red cells, such as hemoprotein and free (tissue) heme.
Prognosis and prevention
Conjugation jaundice has a favorable prognosis. After applying therapeutic methods, the symptoms disappear. The prognosis of the pathological form depends on timely diagnosis and correct therapy. If left untreated, the child may develop serious pathologies:
- liver dysfunction;
- deterioration of vision and hearing;
- developmental delay;
- increased risk of developing liver cirrhosis;
- state of intoxication.
It is impossible to prevent the appearance of physiological jaundice, since it develops as a result of the process of establishing metabolism.
To prevent the appearance of pathological jaundice, a woman during pregnancy should give up bad habits, eat right, control the amount of antibodies in the case of different Rh factors, and take special vitamins for pregnant women.
Remember that treatment is the work of doctors. Don't self-medicate
Research
Treatment of obstructive jaundice in newborns depends on the diagnosis. The diagnostic dilemma is to distinguish biliary atresia from neonatal hepatitis. Table 13.5 lists the studies that are relevant in distinguishing between these conditions. Liver biopsy, radionuclide scan and further treatment should be carried out in a specialized pediatric liver center.
Table 13.5. Studies to discover the causes of neonatal conjugated hyperdilirubinemia.
| Liver enzymes Alkaline phosphatase Serial bilirubin levels Alpha ferroprotein Alpha1 and phenotype screening I Rose Bengal excretion test Abdominal ultrasound Sugar stress test Amino acid screening Percutaneous liver biopsy Radionuclide (HIDA) scan |
What is the nature of jaundice in newborns?
Jaundice or, scientifically speaking, unconjugated hyperbilirubinemia in newborns occurs due to physiological or pathological reasons. More than 75% of cases of neonatal jaundice are due to physiological reasons. Physiological jaundice is also called non-pathological jaundice because it is mild and disappears spontaneously. This occurs due to the peculiarities in the metabolism of bilirubin in the neonatal period. Increased bilirubin load in newborns occurs due to its increased production, which is caused by a higher mass of red blood cells (RBCs) with a decrease in the duration of their existence in newborns. At the same time, a newborn’s liver is still very inactive, and it processes water-soluble bilirubin into conjugated bilirubin, which is water-insoluble, 100 times slower than in an adult.
Physiological jaundice usually occurs between days 2 and 4 of life, peaks between days 4 and 5, and resolves within 2 to 3 weeks. Physiological jaundice never occurs in the first 24 hours of a newborn's life.
Publications in the media
Jaundice is a symptom of various diseases: yellow discoloration of the mucous membranes, sclera and skin, due to the deposition of bile pigments in them.
Classification • Suprahepatic • Hepatic (hepatocellular) • Subhepatic (cholestatic).
Bilirubin metabolism • Indirect bilirubin (unbound, unconjugated) is formed during the breakdown of Hb in the cells of the reticuloendothelial system (80%) and other heme-containing proteins (myoglobin, cytochromes, etc.) in the liver (20%) •• Indirect bilirubin is insoluble in water, lipotropic, not excreted by the kidneys, toxic, bound to albumin in the blood •• Liver cells absorb indirect bilirubin from the blood and conjugate it with glucuronic acids (using the enzyme uridine diphosphate glucuronyltransferase [UDPGT]) to form direct (bound, conjugated) bilirubin •• Direct bilirubin water-soluble, insoluble in fat, non-toxic, can be excreted by the kidneys (when circulating in the blood in high concentrations) •• Direct bilirubin is excreted in bile •• In the intestine, under the influence of bacterial enzymes, direct bilirubin is converted into urobilinogens, which give the characteristic color to stool. Urobilinogens are partially absorbed and enter the liver through the portal vein, where they are destroyed by hepatocytes to di- and tripyrroles. Through the middle and lower rectal veins, anastomosing with the inferior vena cava system, urobilinogens enter the systemic circulation and are then excreted by the kidneys •• In healthy individuals, total serum bilirubin is mainly represented by indirect bilirubin (no more than 20 µmol/l), direct bilirubin is not more than 25% of the total, the feces are colored, traces of urobilin are present in the urine.
ETIOLOGY
• Suprahepatic jaundice is caused by increased hemolysis of red blood cells •• Poisoning with substances that cause hemolysis (for example, snake venom, sulfonamides, arsenic hydrogen) •• Transfusion of incompatible blood •• Large hematomas •• Hemolytic disease of the newborn •• Autoimmune hemolytic anemia •• Hereditary hemolytic anemia ( microspherocytic anemia of Minkowski–Choffard, sickle cell anemia, thalassemia, etc.).
• Hepatic jaundice •• Damage to hepatocytes: infectious, toxic (drugs, alcohol) hepatitis, liver cirrhosis •• Low activity of UDPHT in newborns (transient jaundice of newborns) •• Hepatic jaundice can be hereditary ••• Impaired transport of bilirubin from hepatocytes to bile ( Dubin-Johnson syndrome) ••• Absence of UDFGT - Crigler-Nayar syndrome type I ••• Significant deficiency (less than 10% of the norm) UDFGT - Crigler-Nayar syndrome type II ••• Insufficient activity of UDFGT (Gilbert-Meulengracht syndrome).
• Subhepatic jaundice develops when there is an obstruction to the outflow of bile into the duodenum •• Stones in the bile ducts •• Cancer of the biliary tract and cancer of the head of the pancreas •• Parasitic lesions of the liver •• Atresia of the biliary tract.
PATHOGENESIS • All types of jaundice are united by one symptom - hyperbilirubinemia, on which the brightness of the skin color depends: from a light lemon tint to orange-yellow and green or olive-yellow •• Yellowing of the skin and sclera begins when the bilirubin concentration is more than 26 mmol/l • • Impregnation of the skin with pigment takes time: during experimental ligation of the common bile duct, hyperbilirubinemia increases after 24 hours, but the skin becomes colored only 5–8 days later • There are 4 main mechanisms for the development of jaundice •• Increased formation of indirect bilirubin (hemolysis) •• Impaired uptake of indirect bilirubin hepatocytes and its transport inside the hepatocyte •• Impaired conjugation of indirect bilirubin in hepatocytes •• Impaired excretion of direct bilirubin from the hepatocyte into the bile capillary or obstruction at the level of larger biliary tracts.
• Hemolysis •• The concentration of indirect bilirubin in the blood serum is moderately increased (usually 2-3 times), because. liver functions are not impaired •• The stool is very intensely colored (a lot of direct bilirubin is formed and it is excreted into the bile) •• The concentration of urobilin is increased in the urine (because urobilinogen is absorbed in large quantities through the rectal veins and filtered into the urine).
• Hepatitis •• In the blood serum, the concentration of indirect (impaired uptake, transport and conjugation) and direct (impaired excretion, destruction of hepatocytes, impaired outflow due to compression of the bile ducts in the portal tracts by inflammatory infiltrates) bilirubin is increased •• In most cases, the concentration is increased to a greater extent direct bilirubin (intrahepatic cholestasis); an increase in the concentration of indirect bilirubin indicates the predominance of necrosis of hepatocytes •• Feces are usually discolored, but may not be changed •• Urine is dark due to direct bilirubin (filtered into urine) and urobilinogen (not destroyed in the liver, enters the systemic circulation and is filtered into urine ).
• Cholestasis •• The concentration of direct bilirubin is increased in the blood serum •• The feces are discolored •• The urine is dark (due to the filtration of direct bilirubin into the urine), there is no urobilin in the urine (since direct bilirubin does not enter the intestine).
• Isolated disorders of conjugation or excretion of bilirubin are characteristic of hereditary syndromes. Pathomorphology in cholestasis • Bile pigment in hepatocytes • “Bile lakes” • Dilation of bile canaliculi • Signs of damage to the bile ducts • Formation of new bile ducts.
History • Compounded family history of anemia, any manifestations of liver and biliary tract diseases • Contact with patients with infectious hepatitis, stay in hepatitis endemic regions during the last 2 months, parenteral interventions, drug administration, casual sexual intercourse during the last 6 months • Working with hepatotoxic substances • Alcohol abuse • Treatment with hepatotoxic drugs • Biliary colic, cholelithiasis • Deterioration of general condition, weight loss.
CLINICAL MANIFESTATIONS
• Onset of the disease: from the prodromal period (intoxication syndrome, nausea, vomiting, dyspepsia - with infectious hepatitis), after biliary colic (with cholelithiasis), gradual (with tumors), after infection or hypothermia (with hemolytic anemia) • Jaundice with hemolysis dim, the patient is more pale than jaundiced, with obstruction the jaundice has a green tint, with hepatitis - with an orange tint (with cholestatic forms - with a green tint).
• Suprahepatic jaundice •• Splenomegaly predominates over liver enlargement •• Intense coloring of stool •• Manifestations of anemia.
• Hepatic jaundice •• Enlargement and hardening of the liver from the onset of the disease •• Skin itching is possible •• The spleen is sometimes enlarged •• In severe forms there may be manifestations of hemorrhagic syndrome, hepatic encephalopathy •• Feces are discolored at the height of the disease, urine is dark •• With chronic hepatitis and liver cirrhosis - extrahepatic signs (telangiectasia, hepatic palms), signs of portal hypertension, ascites.
• Subhepatic jaundice •• Skin itching, as a rule, is pronounced •• The gallbladder is enlarged and painless with tumors; in case of cholelithiasis, it may not be palpable, but a pain point is found in its projection •• The liver is enlarged •• Feces are discolored, urine is dark • • Signs of the underlying disease.
LABORATORY RESEARCH
• CBC • Liver function tests • Determination of direct bilirubin and urobilin in urine • Proteinogram • Reticulocyte count, determination of osmotic resistance of erythrocytes, blood smear examination, Coombs test, bone marrow puncture are indicated for suspected hemolytic anemia • Markers of viral hepatitis in hepatic jaundice.
• Suprahepatic jaundice •• The concentration of bilirubin in the blood serum is increased mainly due to indirect bilirubin •• Other indicators of liver function tests are not changed •• Reticulocytosis •• Osmotic resistance of erythrocytes may be reduced •• Possible changes in the shape and size of erythrocytes •• Signs of bone marrow irritation .
• Hepatic jaundice •• The concentration of bilirubin in the blood serum is increased mainly due to direct bilirubin •• The activity of ALT in the blood serum is significantly increased in acute hepatitis, slightly or moderately in chronic hepatitis •• In cholestatic forms of acute hepatitis, the concentrations of cholesterol, -glutamyl transpeptidase are increased , alkaline phosphatase •• In severe forms of acute hepatitis, liver cirrhosis, the albumin content, prothrombin index, and the results of the sublimate test are reduced •• The concentration of immunoglobulins and the results of the thymol test may be increased.
• Subhepatic jaundice •• The concentration of bilirubin in the serum is increased mainly due to the direct fraction •• The concentrations of cholesterol, alkaline phosphatase, g-glutamyl transpeptidase in the blood serum are significantly increased •• The activity of ALT in the blood serum is not changed, with prolonged cholestasis it is moderately increased •• PTI may be reduced, after the introduction of menadione sodium bisulfite it increases •• The concentration of a2- and b-globulins is increased.
INSTRUMENTAL STUDIES • Ultrasound, CT of the liver, biliary tract, pancreas allows you to diagnose obstructive jaundice, as well as identify an empty gallbladder (no mechanical obstructions) in the cholestatic form of acute viral hepatitis • Plain radiography of the chest allows you to identify tumors and their metastases • With FEGDS you can assess the condition of the major duodenal papilla and the possibility of bile outflow through it • Endoscopic retrograde cholangiopancreatography or percutaneous transhepatic cholangiography is indicated for questionable ultrasound results in cases where blockage of the extrahepatic bile ducts is suspected.
TREATMENT is determined by the etiology of the disease that caused jaundice - see Hemolytic anemia, Autoimmune hemolytic anemia, Sickle cell anemia, Acute viral hepatitis, Chronic viral hepatitis, Liver cirrhosis, Gallstone disease.
ICD-10 • P58 Neonatal jaundice due to excessive hemolysis • P59 Neonatal jaundice due to other and unspecified causes • D58 Other hereditary hemolytic anemias • D59 Acquired hemolytic anemia • A27.0 Leptospirosis icteric-hemorrhagic •• E80 Disorders of porphyrin and bilirubin metabolism • P55 Hemolytic disease of the fetus and newborn • B15 Acute hepatitis A • B16 Acute hepatitis B • B17 Other acute viral hepatitis • B18 Chronic viral hepatitis • B19 Viral hepatitis, unspecified
APPLICATIONS
Familial jaundice of newborns is a transient hereditary (r) form of hyperbilirubinemia, starting with jaundice 4 days after birth and developing due to a transient defect of glucuronyl transferase associated with the presence of inhibitors of its activity in the mother’s blood; may lead to bilirubin encephalopathy and cerebral palsy. Treatment: timely replacement blood transfusions and phototherapy. Synonyms: non-hemolytic transient jaundice of newborns, Lucea-Driscoll syndrome, Lucea non-hemolytic jaundice. ICD-10. P59 Neonatal jaundice due to other and unspecified causes.
Jaundice during breastfeeding (jaundice from mother's milk) is a spontaneously transient hyperbilirubinemia of unknown etiology in healthy children in the neonatal period. It can be early (appears within 3–4 days after birth) or late (within 4–5 days after birth) with maximum manifestations at 10–15 days. The maximum concentration of bilirubin can reach 20–30 mg% (340–510 µmol/l). No cases of bilirubin encephalopathy have been described. Diagnostic test: temporary cessation of breastfeeding for 24–48 hours. Treatment: phototherapy, phenobarbital, bilirubin adsorbents. ICD-10. P59 Neonatal jaundice due to other and unspecified causes.
Nuclear jaundice is a severe form of jaundice in newborns with a high concentration of unconjugated bilirubin in the blood, deposition of bilirubin in the basal ganglia and nuclei of the brain stem, occurring with severe impairment of brain functions. Etiology: excessive levels of indirect bilirubin in the blood (over 320 µmol/l in full-term infants and 150–250 µmol/l in premature infants). Causes of hyperbilirubinemia: incompatibility of mother and fetus by blood groups; hereditary spherocytosis, non-spherocytic hemolytic anemia, hemolysis caused by a lack of vitamin K3, taking nitrofurantoin, sulfonamide drugs, etc., hemorrhages, pyloric stenosis, Hirschsprung's disease; metabolic and endocrine disorders, obstructive disorders (Dabin-Johnson-Rotor syndrome, cystic fibrosis, tumors), sepsis, intrauterine infections, neonatal respiratory distress syndrome, severe fetal erythroblastosis. Clinical picture • Yellow-colored amniotic fluid • From birth, moderate jaundice, progressing hourly • Arterial hypotension • Motor restlessness, convulsions • Enlargement of parenchymal organs • Opisthotonus, drowsiness, poor sucking, distorted or absent Moro reflex; late manifestations (after 6 months of life): deafness, paralysis, mental retardation. Diagnosis, treatment, prevention, prognosis - see Erythroblastosis fetalis; additionally treat the underlying disease. Synonym: bilirubin encephalopathy. ICD-10. P57 Kernicterus.
Gilbert's syndrome (#143500, defects of the UGT1A1 UGT1A1 gene, 1q21 q23, B) is a benign unconjugated hyperbilirubinemia of moderate severity. Prevalence is 5–7%, the syndrome more often develops in males in adolescence • In the blood serum, the concentration of indirect bilirubin periodically increases to 17–85 µmol/l. Jaundice is not constant, it can appear or intensify after infections, fasting and decrease after taking phenobarbital (tests with phenobarbital and fasting are used in diagnosis). Liver function is not impaired, the histological picture is not changed. The prognosis is favorable, no treatment is required. Synonyms: Gilbert–Meulengracht syndrome, Meulengracht jaundice, congenital hyperbilirubinemia, constitutional hyperbilirubinemia, Gilbert–Lerbouyer syndrome. ICD-10. E80.4 Gilbert's syndrome
Crigler–Nayjar syndrome (type I, 218800, r; type II, 143500, Â) is a rare hereditary disorder associated with UDPG deficiency and manifested by unconjugated hyperbilirubinemia.
• Type I •• UDFGT activity is completely absent in the liver •• Very high concentration of indirect bilirubin in the blood serum, kernicterus develops •• Patients usually die in the 1st year of life •• Phenobarbital is ineffective, plasmapheresis has a temporary effect •• Phototherapy can reduce the concentration of indirect bilirubin is 2 times •• Encephalopathy (kernicterus) can develop at any time during the first 10–20 years of life •• Liver transplantation leads to normalization of bilirubin metabolism, the prognosis improves • Transplantation should be performed at a young age, before the development of kernicterus . • Type II •• UDFGT activity is reduced to 10% or lower compared to normal •• The concentration of indirect bilirubin is high, but usually lower than in Crigler-Nayjar syndrome type I •• Phenobarbital is effective •• Sometimes the combined use of phenobarbital and phototherapy is necessary • • Patients survive to adulthood.
Abbreviations: UDPGT—uridine diphosphate glucuronyl transferase. Synonyms: congenital non-hemolytic jaundice type I, non-hemolytic hyperbilirubinemia with kernicterus. ICD-10. E80.5 Crigler–Najar syndrome.
Dubin-Johnson syndrome (*237500, defect in the gene for the tubular transporter of organic anions CMOAT, 10q24 [*601107], r) is a hereditary pigmentary hepatosis caused by impaired transport of bilirubin from hepatocytes to bile due to a mutation in the protein gene responsible for the hepatobiliary transport of various organic anions; clinically manifested by jaundice with a moderate increase in the content of direct bilirubin in the blood and its appearance in the urine; During a liver biopsy, a dark, brown-orange pigment (lipochrome) is found in hepatocytes. Treatment: reduction of bilirubinemia with phenobarbital. Synonyms: Dubin-Johnson jaundice, non-hemolytic constitutional jaundice with lipochromic hepatosis, conjugative hyperbilirubinemia type II. ICD-10. E80.6 Other disorders of bilirubin metabolism.
Rotor syndrome (*237450, conjugated hyperbilirubinemia type I, r) is clinically similar to Dubin-Johnson syndrome; Unlike the latter, with Rotor syndrome there is no accumulation of pathological pigment in liver cells, oral cholecystography is often normal, and an increase in urinary excretion of coproporphyrin is noted. ICD-10. E80.6 Other disorders of bilirubin metabolism.
Cholestasis rare • Cholestasis with gallstones, ataxia and visual impairment (214980, r). Clinically: congenital cholestasis, gallstones, cerebellar ataxia, bilateral ptosis, retinal damage, optic nerve atrophy, camptodactyly, jaundice, prurigo. Laboratory: giant cell hepatitis according to the results of liver biopsy • Intrahepatic cholestasis with impaired metabolism of trihydroxycoprostanoic acid (*214950, r). Clinically: congenital jaundice, intrahepatic cholestasis, bile duct insufficiency. Laboratory examination: absence of bile acids in bile, detection of trihydroxyprostanoic acid in bile. Synonym: alligator defect. Note. Typically, bile acids are synthesized in the liver by hydrogenation and hydroxylation of the steroid core of cholesterol with oxidation of the side chains. In some lower vertebrates, side chains are oxidized without hydroxylation (in alligators, trihydroxycoprostanic acid is the main component of bile) • Progressive intrahepatic cholestasis type 2 (*601847, 2q24, defect in the PFIC2, r gene) is a form of severe cholestatic liver disease; manifests in infancy with intermittent jaundice and cholestasis and rapidly progresses to end-stage liver failure and death in childhood. Clinically: progressive familial intrahepatic cholestasis, intermittent jaundice.
How common is jaundice in newborns?
Almost all newborns will have a total bilirubin level above the upper limit of normal for adults and older children of bilirubin of 1.5 mg/dL with less than 5% total conjugated bilirubin. Up to 60% of full-term infants and 80% of newborns at 35 weeks' gestation or more will have jaundice, which occurs when plasma bilirubin levels exceed 5 mg/dL. Neonatal jaundice is more common in people living at high altitudes and in people living around the Mediterranean Sea, especially in Greece.
Jaundice due to infectious diseases
Systemic infections such as toxoplasmosis, syphilis, varicella, rubella, cytomegalovirus and herpes simplex, and systemic conditions such as sepsis, shock and birth asphyxia may also present as jaundice caused by conjugated hyperbilirubinemia. Neonatal urinary tract infections and long-term use of parenteral nutrition in preterm infants are also known causes of conjugated hyperbilirubinemia.