According to statistics, about 5 million cases of cholera are recorded annually in the world, of which about 130 thousand are fatal.
In which countries can you get cholera?
There is an increased risk of infection with Vibrio cholerae in people living or on long-term business trips in the following countries:
- Yemen.
- Iraq.
- Iran.
- India.
- Nigeria.
- Uganda.
- Mexico.
- Tanzania.
- Brazil.
Symptoms of cholera
Most people infected with Vibrio cholerae do not become ill and do not even know they have been infected. But they shed bacteria in their stool for 7-14 days, which means they can still infect others through contaminated water.
Cholera patients suffer from dehydration. Photo: PHIL CDC
As a rule, the clinical manifestations of cholera are represented by moderate or severe diarrhea, which is not much different from stool disorders of other origins. It is less common for more severe symptoms to develop. As a rule, this occurs suddenly, 1-3 days after infection.
Symptoms of cholera infection may include:
- Severe diarrhea. As a rule, it is the first symptom of the disease. It occurs most often at night or in the morning against the background of normal body temperature and in the absence of abdominal pain. Initially, the stool looks like normal diarrhea, but then quickly takes on the specific appearance of “rice water” - cloudy white, transparent stool with whitish inclusions and impurities in the form of flakes. There is no smell. The volume of discharge can reach 3 liters per day.
- Vomit. Appears soon after diarrhea. Vomiting has the appearance of cloudy white water without an odor, sometimes occurring in a “fountain”. Often occurs without previous tension in the abdominal wall muscles and nausea or abdominal pain. Associated symptoms include rumbling and discomfort in the navel area.
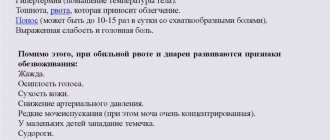
- Dehydration (dehydration). As a result of severe loss of fluid along with stool and vomit, dehydration develops. In the early stages, it manifests itself as general weakness and lethargy, but quickly progresses to more serious symptoms (Table 1).
Table 1. Degrees of dehydration in cholera
| Degree of dehydration | Percentage of fluid loss relative to body weight | Symptoms |
| I | 1-3 % | Moderate thirst Dry mouth mucous membranes Moderate white coating on the tongue |
| II | 4-6 % | Extreme thirst The skin is pale and dry, its firmness and elasticity are reduced Sharp general weakness Hoarseness of voice, decreased volume Cramps in the calf muscles Increased heart rate and drop in blood pressure |
| III | 7-10 % | Blue color of the skin and mucous membranes Pointed facial features, sunken eyes, wrinkled skin on the hands - “washerwoman’s hands” A person can only speak in a whisper Muscle cramps throughout the body Urination stops partially or completely |
| IV | More than 10% | The previously mentioned symptoms develop very quickly Systolic blood pressure drops below 60 mmHg. Art. Hiccups occur instead of vomiting Body temperature decreases Dark circles around the eyes Retraction of the abdomen General tonic spasms Hypovolemic shock develops |
“Knowing the enemy by sight”: how to avoid cholera
Until 1817, this infection raged only in the Ganges delta, taking the lives of millions of people. Changes in climate and the development of trade relations between Europe and Asia led to the disease spreading beyond India. About a hundred countries around the world annually register outbreaks of this disease. Despite all the efforts of the medical community, it is still not possible to completely defeat it.
We're talking about cholera.
What is hidden behind the diagnosis of cholera?
Classified as an acute intestinal infection, the disease occurs when food or water enters the body, contaminated with the bacterium Vibrio cholerae, which is the direct cause of the development of cholera. A characteristic feature of the disease is severe diarrhea and repeated vomiting, as a result of which dehydration of the body rapidly increases. WHO (World Health Organization) classifies cholera as a quarantine infection, as it tends to spread epidemically and is accompanied by high mortality.
Transmission of the cholera pathogen is usually caused by poor living conditions: lack of adequate access to clean water and unsanitary conditions. That is why almost every developing country today faces outbreaks or the threat of cholera epidemics.
A typical clinical picture with signs of severe dehydration develops in one person out of five patients. In other cases, it is almost impossible to distinguish from other forms of acute diarrhea.
It is noteworthy that not all persons infected with the cholera pathogen become ill.
Transmission of the cholera pathogen is usually due to
low level of living conditions:
lack of adequate access to clean water and unsanitary conditions
How cholera spreads
The reservoir and source of infection is a sick person or a transient carrier of infection, releasing bacteria out through vomit and feces. Transmitted by household, water and food routes. The risk of developing cholera significantly increases when swimming in dirty water, drinking contaminated water and raw seafood. Persons suffering from gastritis with low acidity are also susceptible to infection.
You can read more about gastritis in our article
Social cataclysms, natural disasters, and military operations are usually accompanied by a lack of drinking water in the region and the destruction of sewage systems, and this is ideal soil for the activation of Vibrio cholerae.
How to recognize cholera
An intense urge to defecate, accompanied by abdominal discomfort, diarrhea, and vomiting are the first symptoms of cholera. Cholera is characterized by repeated loose stools (often without abdominal pain, up to 20 times a day or more) in the form of “rice water” - a clear liquid with white loose flakes. Often diarrhea and vomiting occur against the background of normal or even low body temperature. Patients complain of a feeling of dry mouth and thirst. The loss of a large volume of fluid leads to a decrease in the amount of urine. With severe dehydration (dehydration), patients experience painful cramps of all skeletal muscles.
Violation of the water-electrolyte balance as a result of massive fluid loss leads to changes in blood composition, an increase in heart rate and pulse, and increased breathing. From the first hours, patients experience a feeling of lethargy and irritability, which is explained by the influence of dehydration and toxins on the functioning of the nervous system.
Diagnosis of cholera involves laboratory testing of the following materials:
- vomit and feces;
— presumably contaminated food, water;
— washouts from dishes and furniture.
To confirm the diagnosis, research methods such as:
— microscopy of the material;
— bacteriological inoculation on nutrient media;
— agglutination reaction with anticholera O-serum;
— immunofluorescence analysis;
— detection of Vibrio cholerae DNA by PCR, etc.
Treatment and prevention of cholera
Patients are subject to mandatory hospitalization in the infectious diseases department and placement in an individual box. All the patient’s secretions are collected in a special container and their volume is assessed. These data allow the doctor to calculate the required amount of saline solutions used to replenish the deficiency of fluid and electrolytes. Depending on the degree of dehydration, patients take such solutions orally in small sips, or they are administered intravenously by drip (stream).
Antibacterial therapy for cholera involves the use of tetracycline antibiotics, cephalosporins, nitrofurans for 3-5 days.
What was the situation with the treatment of cholera at a time when there were no antibiotics well known today, nitrofurans? Read about one of these methods here
There is no specific diet for cholera. In the first days of the disease, table No. 4 is prescribed; after restoration of intestinal activity, it is recommended to increase the amount of potassium-containing foods in the diet (dried apricots, bananas, citrus fruits).
With timely and adequate treatment, the prognosis is favorable. Working capacity is fully restored within approximately 30 days. In the absence of adequate medical care, the likelihood of rapid death is high.
Compliance with sanitary and hygienic standards in populated areas, at food establishments, and in areas where water is collected for the needs of the population helps prevent the development of cholera.
You can protect yourself from cholera by following simple rules:
- It is necessary to wash your hands promptly and thoroughly with soap;
- eat only good-quality, thoroughly washed, cooked foods;
- drink boiled or industrially disinfected water;
— for those traveling to areas with a high risk of infection with Vibrio cholerae, specific prevention measures have been developed with cholera vaccine and cholera toxoid. The cholera vaccine has a short (3 - 6 months) period of action.
Follow the rules of hygiene and be healthy!
Sevil Ibraimov
The article was prepared with the information support of specialists from Clinic Expert Voronezh
The editors recommend:
Viruses and bacteria - what is the fundamental difference?
Russia or Britain: who actually discovered penicillin?
Live according to your dreams. The great discovery of Louis Pasteur
When to see a doctor?
The risk of a cholera outbreak in industrialized countries is low. Even in regions where it exists, the likelihood of infection is minimal if food safety recommendations are followed. However, cases of cholera occur throughout the world.
Therefore, if a person develops severe diarrhea after visiting an area with recent cases of cholera, it is time to seek immediate medical attention².
Features of cholera in children
At the age of under 3 years, the dehydration characteristic of cholera is much more severe. Because of this, children quickly develop signs of dysfunction of the nervous system in the form of severe general lethargy, convulsions and even loss of consciousness. Moreover, unlike adults, the body temperature of children with cholera often rises to 37.5-38.0°C.
Treatment of cholera
Treatment of patients with cholera is carried out in hospitals of the infectious diseases department, in an isolated box. In most cases, patients require bed rest. The basis of treatment is correction of water-salt balance and antibacterial therapy. The duration of treatment depends on the severity of cholera and is 3-5 days.
Restoring water-salt balance
An important role in treatment is the restoration of water-salt balance, which must begin from the first hours of the development of the disease. It is necessary to compensate for the loss of fluid in the body: the volume of incoming fluid should be 1.5 times greater than its loss (vomit, stool).
It is important to start rehydration and correction of water-salt balance as early as possible. Photo: belchonock/Depositphotos
For 1-2 degrees of dehydration, water-salt solutions are used, which are taken orally. With 3-4 degrees of dehydration, patients lose the ability to drink on their own, which is why saline solutions are administered intravenously in a stream during the first few hours, after which their administration is continued intravenously by drip.
How to make a rehydration solution at home
In some cases, it is not possible to purchase a ready-made oral rehydration solution. As a temporary measure, you can use a homemade analogue. To do this you need to mix:
- 1 liter of bottled or boiled water.
- 6 level teaspoons (about 30 grams) table sugar.
- 1/2 level teaspoon (about 2.5 grams) table salt.
Antibacterial therapy
Antibiotics are prescribed to combat the pathogen directly. For cholera, effective remedies are:
- tetracyclines: tetracycline, doxycycline;
- fluoroquinolones: ciprofloxacin;
- macrolides: erythromycin;
- if antibiotics are intolerant, drugs from the nitrofuran group (furazolidone) are prescribed.
Historical reference
In the 19th century, cholera began to spread throughout the world from its original reservoir, the Ganges River delta in India. Six subsequent pandemics took the lives of many millions of people on all continents of the planet. The last (seventh) pandemic began in South Asia in 1961, reached Africa in 1971, and America in 1991. Cholera is now endemic in many countries¹.
The causative agent of cholera
This infection is caused by the enteropathogenic Vibrio cholerae. Today, more than 150 different strains of this bacterium have been discovered, which differ in their microbiological characteristics. They are divided into two groups - option A or B. The causative agent of cholera is strains of type A. This is a mobile gram-negative bacterium, which, when it enters the lumen of the digestive system, releases toxins - heat-stable endotoxin and heat-labile cholerogens (enterotoxin).
Vibrio cholerae: Vibrio cholerae under a microscope. Photo: wikipedia.org
The bacterium is quite resistant to unfavorable environmental conditions, can easily survive in running water for several months, and lives in wastewater for up to 30 hours or more. The breeding ground for vibrio is meat or milk. But the bacterium dies under the influence of boiling, disinfectants, sunlight, and drying. Sensitive to antibiotics from the group of fluoroquinolones and tetracyclines.
Risk factors
Everyone is susceptible to cholera, with the exception of infants who have received immunity from nursing mothers who have previously had cholera. However, certain factors can make a person more vulnerable to the disease or cause the infection to become more severe. These include:
- Poor sanitary conditions. Unsanitary living conditions are common in refugee camps, poor countries, and areas affected by famine, war, or natural disasters.
- Decreased or absent stomach acid. Cholera bacteria cannot survive in an acidic environment, and regular stomach acid often serves as a defense against infection. But people with low stomach acid levels (such as children, the elderly, and people taking medications to reduce stomach acid secretion) do not have this protection.
- I (0) blood group. The reasons are not yet fully understood, but the likelihood of developing cholera in people with the first blood group is twice as high as in others².
Diagnostics
Diagnosis is made based on a combination of medical history, clinical manifestations and laboratory results. When collecting an anamnesis, possible routes of cholera infection are clarified (consumption of potentially contaminated water or seafood) and risk factors - for example, a business trip to disadvantaged countries, regions, areas several days before the onset of symptoms.
The following tests are used in the laboratory diagnosis of cholera:
- Complete blood count (CBC). It shows a moderate increase in the level of red and white blood cells, including neutrophils. The saturation of red blood cells with hemoglobin and the erythrocyte sedimentation rate (ESR) also increase. At the same time, the level of monocytes may drop.
- General urinalysis (UCA). In addition to a general decrease in the volume of urine excreted, as dehydration increases, there may be an increase in the level of pathological casts and protein.
- Bacteriological culture. If cholera is suspected, in order to identify the pathogen, a sample of vomit or feces is sown on a nutrient medium. After 1-2 days, colonies grow. If cholera is suspected, the test is repeated twice more.
- Rapid tests with monoclonal antibodies. Allows you to confirm within 5 minutes the fact of human infection with cholera vibrios.
- Indirect blood hemagglutination reaction (IRHA). Makes it possible to detect the presence of specific antibodies in the blood. Their diagnostic titer of 1:160 is considered a positive result. The test is informative only from the 5th day of the disease.
- Polymerase chain reaction (PCR). Allows you to identify the genetic material (in this case, DNA) of the pathogen. In addition to the patient's secretions, water or food, which are a potential source of infection, can also be used for research.
Culture for cholera is one of the diagnostic methods.
Photo: Nathan Reading / Flickr (CC BY-NC-ND 2.0) Differential diagnosis of cholera is carried out with other diseases, which in the early stages may be accompanied by similar symptoms. These include:
- Acute intestinal infections: salmonellosis, typhoid fever, escherichiosis (dysentery), rotavirus infection. They are also accompanied by diarrhea and vomiting. However, unlike cholera, they cause fever, abdominal pain, and often mild or no dehydration.
- Poisoning. Symptoms of chemical intoxication directly depend on the specific reagent. However, in most cases they also present with vomiting, diarrhea and signs of central nervous system dysfunction. In this case, dehydration, as a rule, does not occur.
- Botulism. An acute infection that also leads to disruption of the central nervous system. In addition to skeletal muscle cramps, vision and breathing suffer. Unlike cholera, constipation often occurs. The cause of infection is most often the consumption of spoiled canned food or smoked meats.
What is cholera
This is a particularly dangerous infection that affects the entire body. Particularly pathogenic Vibrio cholerae affects the digestive tract at the level of the stomach and small intestine, causing severe gastroenteritis and severe dehydration, which leads to the formation of dehydration shock.
Cholera is an extremely contagious infection, it provokes epidemics, has a high percentage of deaths, and therefore is classified throughout the world as quarantine and highly pathogenic.
Today, cholera outbreaks occur in Africa, Southeast Asia or Latin America. Up to 5 million people suffer from this infection every year, and about 100 thousand people die.
Pathogen and routes of infection
The causative agent of cholera is Vibrio cholerae, namely its two serogroups O1 and O139. Of these, the main biotypes that cause outbreaks of the disease are: O1 classica – classic biotype. O1 El Tor – currently predominant. O139 Bengal - known since 1992, the cause of a major epidemic in Bangladesh, India and nearby countries.
The source of infection is a sick person or a carrier of the bacteria. People are most contagious in the first 7 days after the development of cholera - during this time they actively release Vibrio cholerae into the environment. Insects and animals are not carriers of this disease.
Transmission of infection most often occurs through the fecal-oral route. Infection can occur in the following ways:
- Surface or well water. Contaminated public wells are a common cause of large-scale cholera outbreaks. People living in crowded conditions with poor sanitation are particularly at risk.
- Seafood. Eating raw or undercooked seafood, especially shellfish, can lead to cholera.
- Raw fruits and vegetables. Raw, unpeeled fruits and vegetables are a common source of infection in endemic regions. Undecomposed fertilizers or irrigation water containing untreated wastewater can contaminate produce in the field.
- Grains. In regions where cholera is widespread, rice and millet that are contaminated after cooking and stored at room temperature for several hours can provide a breeding ground for cholera bacteria.
The risk of developing a cholera epidemic is highest in unsanitary conditions. Photo: Olgatribe/Depositphotos
Publications in the media
Cholera is an anthroponotic, especially dangerous acute quarantine infectious disease that occurs with severe diarrhea and vomiting, leading to dehydration.
Etiology . The causative agent is the mobile gram-negative bacterium Vibrio cholerae (Vibrio cholerae, or Koch's comma). There are 3 types of pathogens - V. cholerae asiaticae (the causative agent of classical cholera), V. cholerae eltor (the causative agent of El Tor cholera) and serovar O139 (Bengal) (the causative agent of cholera in Southeast Asia). The mobility of bacteria is very pronounced, and its determination (by the hanging or crushed drop method) is an important diagnostic sign. Cell division occurs very quickly and in alkaline peptone water the pathogen produces growth visible to the naked eye within 6 hours. It quickly dies when boiled in an acidic environment.
Epidemiology . Cholera is a typical intestinal infection. The only natural reservoir is patients and bacteria carriers, the main routes of transmission are water and food, less often household contact. Transmission factors: food, water, environmental objects. A certain role is played by flies that can transfer the pathogen from feces to food products. Despite the fact that the release of the pathogen into the environment occurs within a short time, a large number of latent forms maintain the circulation of the pathogen. The only historical endemic focus of cholera is the Ganges-Brahmaputra delta. There are 2 types of cholera epidemics: outbreak epidemics with a single source of infection and routes of spread, characterized by the simultaneous appearance of a large number of patients, and sluggish epidemics with a low constant incidence and difficult to identify routes of transmission of the pathogen. In most cases, an increase in incidence is observed in the warm season.
Pathogenesis . In the human body, most of the vibrios die under the influence of the acidic environment of the stomach, and only a small part of them reaches the small intestine. In response to the penetration of bacteria, the intestinal epithelium secretes an alkaline secretion saturated with bile (bile is an ideal environment for pathogen reproduction). Clinical manifestations of cholera are caused by the formation of exotoxins • Exotoxin (cholerogen) is a heat-labile protein, the toxin molecule includes 2 components: component B interacts with the monosialic ganglioside receptor, which causes the penetration of component A into the cell. Component A consists of subunit A1 (active center) and subunit A2, connecting both components. Subunit A1 catalyzes the ribosylation of the guanyl-dependent component of adenylate cyclase, leading to an increase in the intracellular content of cyclic 3,5-adenosine monophosphate and the release of fluid and electrolytes from the cells of the Lieberkühn glands into the intestinal lumen. The toxin is not able to realize its effect on any other cells. Bacteria serovar O139 also produce an exotoxin with similar properties, but in smaller quantities; toxin formation is encoded by both chromosomal and plasmid genes • Hemolysins play a certain role in the lesions caused by the El Tor biotype.
Clinical picture
• The incubation period lasts from several hours to 5 days (usually 2–3 days).
• Most infected individuals are asymptomatic or may experience mild diarrhea. The ratio of severe lesions to the number of erased manifestations for classical cholera is 1:5–1:10, for El Tor cholera is 1:25–1:100.
• Clinically severe cases are characterized by general malaise, vomiting and the development of severe diarrhea syndrome, lack of intoxication (body temperature does not rise). The latter is characterized by the release of a significant amount (up to 10 l/day) of watery, colorless feces. Another characteristic feature is the sweetish, fishy (but not fecal) odor of the stool.
• Severe cases of the disease are caused by the development of dehydration: in patients, diuresis sharply decreases with the development of acute renal failure. Hoarseness of voice or aphonia is characteristic. The leading pathogenetic factor is hypovolemia and electrolyte deficiency. As a consequence, arterial hypotension, coronary insufficiency, impaired consciousness and hypothermia develop. A similar condition is defined as cholera algid (Algid is a symptom complex caused by dehydration of the body (loss of sodium chloride, potassium, bicarbonates): hypothermia, hemodynamic disorders, anuria, tonic convulsions, severe shortness of breath). A characteristic manifestation is noted - facies hippocratica (sunken eyes, pointed facial features with sharply protruding cheekbones). The duration of manifestations depends on timely initiation and adequate treatment and varies from several hours to several days. In the absence of treatment, the mortality rate of patients in the algid stage can reach 60%.
• Recovery is accompanied by the development of short-term immunity; cases of re-infection are often noted.
Research methods • Isolation and identification of the pathogen; The goals of the research are to identify patients and bacteria carriers, establish a final diagnosis when examining the dead, monitor the effectiveness of treatment of patients and sanitization of carriers, control over environmental objects and the effectiveness of disinfection measures. Materials for research - feces, vomit, bile, sectional material (fragments of the small intestine and gall bladder), bed and underwear, water, sludge, wastewater, hydrobionts, swabs from environmental objects, food products, flies, etc. The most objective results are obtained by examining samples taken before the start of antibacterial therapy • Blood test - signs of dehydration (acidosis, hypokalemia, hyponatremia, hypochloremia, hypoglycemia, polycythemia, slight neutrophilic leukocytosis).
Differential diagnosis is carried out with various severe diarrhea (for example, caused by Salmonella species, E. coli or enteropathogenic viruses), mushroom poisoning, arsenic.
Treatment • Etiotropic therapy •• Adults and children over 8 years old - doxycycline 300 mg 1 time / day, or 100 mg 2 times / day or tetracycline 50 mg / kg / day for 3 days. As an alternative drug, it is possible to use ciprofloxacin in an average therapeutic dosage •• For children under 8 years of age - co-trimoxazole (4 mg/kg trimethoprim and 20 mg/kg sulfamethoxazole every 12 hours) or furazolidone 5–10 mg/kg/day in 4 divided doses after 6 hours for 3 days •• For pregnant women - furazolidone 100 mg 4 times a day for 7-10 days • Replacement of loss of fluid and electrolytes in accordance with the degree of dehydration of the patient •• For mild and moderate forms - oral rehydration (r- r rehydration salt [sodium chloride 3.5 g, potassium chloride 1.5 g, glucose 20 g, trisodium citrate 2.9 g in 1 liter of water], glucosolan or citraglucosolan) •• In severe form - introduction of saline solutions into /in (sodium acetate + sodium chloride + potassium chloride).
Synonyms • Asiatic cholera • Epidemic cholera • Rice water diarrhea
ICD-10 • A00 Cholera
Classification
Several classifications of cholera are used in clinical practice. This is due to differences in the symptoms of the disease and treatment approaches in different cases. Also, some forms of the disease may have a course uncharacteristic of classical cholera.
Depending on the developing symptoms, cholera is divided into the following forms:
- Typical or gastrointestinal. The classic form of cholera, accompanied by gastrointestinal disorders.
- Atypical. It includes several subspecies that differ significantly from the typical variant of the disease. Atypical forms of cholera include:
- Lightning fast. It is characterized by extremely rapid development with pronounced vomiting and diarrhea, due to which severe dehydration quickly develops, and dehydration shock occurs within 3-4 hours.
- Dry. It is characterized by a sharp deterioration in the general condition of a person. Even before the onset of diarrhea, a coma may develop.
- Erased. It has relatively mild symptoms: the frequency of bowel movements per day ranges from 1 to 3 times, and the stool is not modified. The general condition is often satisfactory; the diagnosis is established only at the stage of laboratory tests.
- Asymptomatic. A variant of infection that occurs without any clinical manifestations. It is detected only after laboratory diagnostics.
It is customary to distinguish vibration carriers separately. This is a condition in which an infected person releases Vibrio cholerae into the environment, but does not show signs of illness. He may have the following options:
- Convalescent. It is observed in people who are recovering from cholera.
- Transitional. Characteristic for people who are in the center of a cholera outbreak. They become infected, but their body successfully fights off the infection. As a rule, it lasts no more than 3 months.
- Chronic. A condition in which cholera vibrios remain active in the body and a person continues to release them into the environment for more than 3 months.
Depending on the patient’s condition, the severity of damage to the gastrointestinal tract and the degree of dehydration, the following degrees of severity of cholera are distinguished:
- Easy. It is characterized by the accumulation of Vibrio cholerae toxins in the body. Defecation is repeated 3-5 times a day, general health remains satisfactory. There are minor feelings of weakness, thirst, dry mouth. The illness lasts 1-2 days.
- Average. Intoxication of the body is moderate. In this case, diarrhea is accompanied by vomiting, which is not accompanied by nausea. There is intense thirst and other signs of dehydration. Stool up to 15 times a day, copious. Single muscle cramps may be observed. The duration of the disease is 4–5 days.
- Heavy. Pronounced consequences of severe intoxication of the body. There are pronounced signs of dehydration due to copious (up to 1–1.5 liters per bowel movement) stool with a frequency of up to 35 times a day. Repeated vomiting in a fountain. Painful muscle cramps in the limbs and abdomen. The skin of the hands and feet becomes wrinkled (“washerwoman’s hand”). The face takes on a characteristic appearance: sharpened features, sunken eyes, cyanosis of the lips, ears, earlobes, nose.
“Washerwoman’s hands” is a characteristic symptom of cholera. Photo: PHIL CDC
Cholera
Cholera (cholera) is an acute intestinal anthroponotic infection with a fecal-oral transmission mechanism, which is characterized by the development of acute gastroenteritis with water-electrolyte imbalance with the rapid development of dehydration. Refers to particularly dangerous conventional diseases.
History and distribution. Cholera has existed since ancient times. Until the beginning of the 19th century. the disease was recorded within the Hindustan Peninsula and did not spread to other regions. But with the development of trade and transport relations and tourism from the middle of the 19th century, cholera began to spread beyond its historical focus. From 1817 to 1925, six cholera pandemics were recorded. In 1872, the causative agent of cholera Vibriocholerae was discovered by E. Niedzwiecki, but he did not obtain it in pure culture. In 1883, R. Koch described the causative agent of the disease and isolated it in pure culture. From 1926 to 1960, cholera was reported in India and Pakistan and rarely spread to other regions. Since 1961, the beginning of the seventh cholera pandemic has been noted, which is associated with the emergence of a new pathogen Vibrioeltor, which was isolated by F. Gottschlich at the El Tor quarantine station among pilgrims in 1905. Since 1961, WHO began to consider cholera caused by the El Tor vibrio , as a disease that, according to clinical and epidemiological data, does not differ from classical cholera. In the 90s, some researchers predicted the possibility of the beginning of the 8th cholera pandemic, which was associated with the registration of large epidemics and outbreaks caused by Vibrio cholerae serogroup O139 (a synonym for Bengal, indicating its first isolation in the coastal areas of the Bay of Bengal), in the countries of South and South-East Asia. However, WHO experts expressed the view that the threat of the spread of infection is unlikely. After the first publications about Bengal cholera in India, vibrio was isolated in a number of Asian countries: Bangladesh, China, Hong Kong, Malaysia, Burma, Nepal, Singapore and Thailand. 3487 cases of cholera caused by this pathogen were registered; no further large outbreaks were observed. Imports of Bengal cholera without further spread to the USA, Germany, England, Denmark, Estonia, Russia, Japan, Kyrgyzstan, Uzbekistan, Kazakhstan and China were recorded. It is difficult to predict the further development of the spread of the disease, but it is known that epidemic outbreaks of Bengal cholera occur in India and Bangladesh.
Morbidity, mortality. From 1961 to 1992, according to WHO, 2,826,276 cases of cholera were reported worldwide, most of which were caused by Vibrio El Tor. Including 48.1% of cases were noted in Asian countries, 25.7% in America, 26.8% in Africa, 0.2% in Australia, 0.2% of cases in European countries. The mortality rate for cholera in the world (1989–1998) was from 1.8% to 4.7%, with maximum rates in Asia - 5.7%, in Africa - 9.1%, in America - 2.1% and in Europe - 1.7%.
According to the WHO, there are 3–5 million cases of cholera and 100,000–120,000 deaths from cholera each year. Incidence for the period 2004–2008. increased by 24% compared to 2000–2004. In 2008, 190,130 cases of the disease were reported in 56 countries, including 5,143 deaths. However, many cases of the disease remain unreported due to limited surveillance capacity and fears of travel and trade bans. The number of cholera cases annually is estimated at 3–5 million cases and 100,000–120,000 deaths.
The risk of cholera epidemics increases during natural and human-caused disasters, as well as in overcrowded refugee camps. In such conditions, explosive outbreaks of diseases with high mortality rates often occur. For example, in 1994, in refugee camps in Goma, Congo, there were 48,000 cholera cases and 23,800 deaths in one month. Cholera incidence of this magnitude is rare, but it remains a public health problem and causes significant economic and life losses. In 2001, WHO and its Global Outbreak Alert Network partners reported 41 cholera outbreaks in 28 countries.
Cholera outbreaks continue to this day. Classic cholera is recorded in India, Pakistan, Bangladesh, El Tor cholera - in Thailand, Indonesia and other countries of Southeast Asia. Thus, in 2010, 60,240 cases of the disease were detected in Haiti, of which 1,415 were fatal. Pakistan reported in October 2010 99 cases of cholera caused by Vibrio cholerae 01. Currently (2011) in Haiti with 426,785 people turned up with cholera symptoms, 6,169 died, hospital mortality was 1.7%. In the Dominican Republic, the number of cases of cholera is 15.8 thousand people, with 109 deaths. In Ukraine, 33 cases of cholera and 24 cases of vibrio carriage have been registered. Vibrio 01 El-Tor Ogawa was isolated from all patients. Cholera cases were registered in 2011 in Venezuela, Pakistan, Nepal, India, Iran, Nigeria, Somalia, Cameroon, Uganda, the Democratic Republic of the Congo, Afghanistan, and Niger.
In Russia, there has been a stabilization of the epidemic process since 1988, and cholera diseases are mainly imported and sporadic. Over the past 20 years, more than 100 cases of importation have been identified in seven regions of the country. The cholera epidemic in Dagestan in 1994 was severe, when 2,359 people fell ill as a result of the introduction of the disease by pilgrims who performed the Hajj to Saudi Arabia.
Etiology . The causative agent of cholera Vibrio cholerae - belongs to the genus Vibrio, family Vibrionaceae, serogroup 01 of biovars cholerae (classical and eltor). In recent years, up to 80% of all cholera cases have been caused by Vibrio El Tor. Based on their antigenic structure, cholera vibrios are divided into three serovars: Inaba, Ogawa and Gikoshima. Vibrio cholerae has the shape of a comma, due to the presence of a flagellum it has good mobility, is aerobic, does not form spores, is gram-negative, capable of very rapid reproduction, the optimal growth temperature is 37 ° C. It grows well on nutrient media that have a slightly alkaline reaction, liquefies gelatin, decomposes starch, forms indole, reduces nitrates to nitrites, and is lysed by specific phages. Of the pathogenicity factors, the most important is the exotoxin - cholerogens. The pathogen also contains endotoxin, which has a leading role in the development of post-infectious immunity. Vibrio dies when boiled and tolerates low temperatures and freezing. Under the influence of light, air and drying, cholera vibrios die within a few days. Vibrio cholerae is sensitive to chlorine-containing disinfectants. In the water of surface reservoirs, silt and in the body of some hydrobionts, the pathogen not only persists for a long time, but also multiplies. Strains that circulate in the external environment are weakly virulent. On food products, vibrios persist for 2–5 days; on tomatoes and watermelons, when exposed to sunlight, vibrios die after 8 hours. Infection is possible by consuming fish, crayfish, shrimp, oysters caught in polluted waters and not subjected to heat treatment. Vibrios persist for a long time in open reservoirs into which sewage water flows and when the water warms up to more than 17 °C.
In recent years, outbreaks of diarrheal diseases have been recorded that are caused by Vibrio cholerae not of O1, but of O139 serogroup. The course of the disease in its clinical and epidemiological characteristics does not differ from cholera. WHO experts believe that the spread of diseases caused by Vibrio cholerae O139 is becoming a real threat, identical to what happened with Vibrio El Tor in 1961. Vibrios, in relation to cholera phages, are divided into five main phagotypes. There are vibrios that are not agglutinated by polyvalent cholera serum O, the so-called NAG-vibrios, which, by morphological and cultural characteristics, as well as by enzymatic activity, do not differ from cholera vibrios, have the same H-antigen, but belonging to other O-groups . Currently, over 60 serological O-group NAG vibrios have been identified. These vibrios can cause cholera-like diseases.
Epidemiology . The source of infection are patients with a typical or erased form of cholera, vibrio carriers (convalescent, acute, chronic). The pathogen is released into the environment with feces, especially by persons with a typical form of the disease in the first 4–5 days. Patients with erased, atypical forms of the disease are dangerous due to their active lifestyle and contact with others. This is also the epidemic danger of vibrio carriers, but chronic carriage is extremely rare.
The transmission mechanism is fecal-oral, the main route of transmission is water, less often food and household contact. It is important not only to drink water contaminated with the pathogen, but also to use it for washing dishes, vegetables, fruits, and swimming in contaminated water bodies. Cholera has a tendency to spread epidemically. Outbreaks occur more often during the warmer months.
Human susceptibility to cholera is high. People with low acidity of gastric juice, some forms of anemia, helminthic infestations and alcoholism are more often susceptible to the disease. After an illness, type-specific antimicrobial and antitoxic immunity is formed, which persists for one year.
Pathogenesis and pathomorphology. The pathogen enters the human body with contaminated food or water, overcomes the acid barrier, which is facilitated by stomach diseases, which are accompanied by low acidity. Cholera is most severe in people who abuse alcohol or have undergone gastric resection. In the slightly alkaline environment of the small intestine, the vibrio adheres to the border of epithelial cells and multiplies. By adhering to enterocytes, cholera vibrios use the enzyme units of the latter to generate energy for the synthesis of their own structures. It is still controversial whether adhesion itself leads to intestinal secretion. Studies with recombinant, attenuated strains of Vibrio cholerae developed to produce oral vaccines have shown that these strains adhere well but do not cause diarrhea. Vibrio cholerae multiply and produce cholera toxin. There are three toxic substances: 1) endotoxin (lipopolysaccharide); 2) exotoxin (cholerogen); 3) permeability factor. Other toxins of Vibrio cholerae have also been described: zot, which affects the tight junctions of cells and regulates their permeability, as well as the additional toxin ace, which causes an increase in the short circuit current in the Ussing chamber. This is probably the sodium pump blocking toxin reported by Phillips back in the 60s. The location of the genes for these toxins on a chromosome fragment has been revealed. The clinical manifestations of cholera are based on electrolyte diarrhea syndrome. The development of diarrhea consists of hypersecretory processes, which are caused by activation of the enzyme adenylate cyclase in the epithelial cells of the small intestine under the influence of cholerogens and the accumulation of cAMP, leading to increased secretion of water and electrolytes into the intestinal lumen. Studies (D. Powelletal., 1994; CSeurs. G. Kaper., 1996) describe in detail the biochemical properties and biological effects of cholera toxin. Through a system of cyclic nucleotides, it stimulates the secretion of chlorine, inhibits the absorption of electrically neutral sodium chloride by epithelial cells and modulates their cytoskeleton (microtubules), and causes the accumulation of intracellular calcium. This, in turn, determines an increase in the secretory response, since calcium stimulates the formation of cyclic nucleotides. Calcium and the protein calmodulin activate phospholipase, which causes phosphorylation of proteins with an increase in the permeability of the apical membranes of crypt enterocytes, which leads to hypersecretion of water and electrolytes. Bradykinin, kallidin, and vasoactive intestinal peptide influence the increase in the synthesis of cyclic nucleotides. It has been proven that diarrhea also occurs due to the release of serotonin, which in turn stimulates the formation of prostaglandin E2. The role of serotonin as the most important mediator of hypersecretion in the small intestine under the action of cholera toxin is proven by the successful use of serotonin receptor antagonists. In cholera, isotonic dehydration occurs. According to modern concepts, cholera diarrhea is caused by increased secretion of intestinal juice (sodium ions, bicarbonate, potassium chlorine, water), accelerated physiological desquamation of enterocytes, increased membrane permeability, as well as slower reabsorption of sodium, chlorine and water ions. Patients experience: severe metabolic acidosis, blood thickening, increased specific gravity, deterioration of the rheological properties of blood, hypokalemia, increased protein content, etc. Fluid losses with feces and vomit in a short period of time can reach volumes that do not occur with diarrhea of other etiologies . As a consequence of dehydration, significant hemoconcentration, hypovolemia, hypoxia, thrombohemorrhagic syndrome and acute renal failure develop. Additional mechanisms of protection against dehydration and loss of electrolytes are included:
a) a decrease in body temperature - this leads to a decrease in natural perspiration (about 1.5 liters of sweat are lost per day along with sodium, potassium and other electrolytes); b) dryness of the mucous membranes of the mouth, eyes, and genitourinary organs appears (secretion of all glands is reduced); c) oliguria develops up to anuria.
However, these defense mechanisms do not save, since the insidiousness of Vibrio cholerae is that its toxin (cholerogen), when combined with epithelial cell receptors, causes prolonged hypersecretion of fluid and electrolytes from the crypts of the small intestine for 18–24 hours. During this period, the body dies without treatment (rehydration).
The dead often exhibit a “Hippocratic face”: sunken eyes, sharpened facial features, sallow skin color with a bluish tint. The “wrestler or boxer pose” and the “washerwoman’s hand” are often observed. Cadaveric spots are purple-violet in color. The blood has a tar-like consistency that resembles currant jelly. Redistribution of blood and its accumulation in large veins, desolation of the capillary network are revealed. The kidneys decrease in size, the glomeruli are filled with blood, and degeneration of the convoluted and proximal tubules is noted. The intestines are full of fluid. An exudative process is observed throughout the digestive tract, but no signs of inflammation are observed. There are dystrophic changes in the liver and myocardium.
The method of optical and electron microscopy revealed functional changes in the structures of the heart, kidneys, adrenal glands, hypothalamic nuclei and pituitary gland. However, all these changes are secondary, regulatory, protective and are aimed at restoring water-salt homeostasis. These disturbances in cholera are in no way connected with a direct toxic effect on the structures of internal organs, but are caused by dehydration.
It is this approach to understanding the pathogenesis of cholera - recognition of the primacy of dehydration and electrolyte imbalance - that made it possible to develop pathogenetic rehydration therapy, which is aimed at eliminating the main cause of the pathology.
Clinical picture. The incubation period lasts from several hours to 5 days, most often 1–3 days. The disease begins acutely in the middle of full health, often at night with the appearance of rumbling, flatulence and loose stools. The body temperature is often normal, but in some patients it is low-grade. The stool is watery, a cloudy white liquid with floating flakes and resembles “rice water” or “meat slop” in appearance. The act of defecation is painless. Then vomiting of gastric contents follows, soon it becomes watery and also resembles rice water. Cholera is characterized by dehydration, desalination and metabolic acidosis; there are no symptoms of intoxication. In regions with hot climates, where there is a significant loss of fluid and electrolytes through sweat, as well as when water consumption is reduced due to damage to water supplies, cholera is severe due to the development of a mixed mechanism of dehydration, which occurs due to a combination of extracellular (isotonic) dehydration with intracellular (hypertonic) dehydration. In such cases, the frequency of stool does not always correspond to the severity of the disease. Clinical symptoms of dehydration develop with infrequent bowel movements, and in a short time a significant degree of dehydration develops, which threatens the patient’s life.
In 80% of people, cholera occurs in mild or moderate form. 10–20% of people develop severe watery diarrhea with signs of dehydration. In accordance with the classification of cholera by V.I. Pokrovsky, four degrees of dehydration are distinguished: I degree involves fluid loss of up to 3% of body weight, II degree - 4-6%, III degree - 7-9%, IV degree (decompensated dehydration) - 10% or more.
Dehydration of the first degree is detected most often, while many symptoms of the disease are not expressed and the disease is abortive in nature. Some patients experience a prodromal period lasting about a day, which is characterized by dizziness, malaise, weakness, and nausea. The first symptom of the disease is abnormal stool, which is watery in 2/3 of patients and mushy in 1/3. In 5% of patients, the stool may be formed. The frequency of diarrhea is from 5 to 10 times a day. The duration of the disease is no more than 3 days. The bowel movements are not profuse. Vomiting may occur in about half of patients. The skin is moist, turgor is preserved. In 2/3 of patients, dryness of the oral mucosa is detected. There are no hemodynamic disturbances.
Dehydration of the second degree is recorded in approximately 20% of patients. In most cases of the disease, the prodromal period is either not pronounced or short-lived. The disease is characterized by the appearance of loose stools, which quickly become watery and in half of the patients resemble rice water. Vomiting occurs in the first hours of illness, its frequency reaches up to 10 times a day. The total loss of fluid with stage II dehydration averages 5–6 liters. Symptoms of dehydration develop quickly. Characterized by weakness, dizziness, fainting, dry mouth, thirst, hoarseness, decreased skin turgor. A quarter of patients have cyanosis and acrocyanosis. Body temperature is normal or subnormal. An increase in body temperature is rarely detected. The tongue is dry. Half of the patients have tachycardia, a quarter have arterial hypotension, and in some cases oliguria. Some patients experience cramps in the calf muscles, hands and feet. When examining blood, signs of hemoconcentration are minimal (Ht = 0.46–0.50) due to compensatory blood thinning. Electrolyte changes are compensated. Most often, compensated or subcompensated metabolic acidosis (pH 7.36–7.40; BE = -2.0–5.0 mmol/l), hypokalemia, and hypochloremia are observed.
Dehydration of the third degree is detected in 10% of cholera patients during outbreaks. The onset of the disease is acute, and symptoms of dehydration develop quickly - after 10–12 hours. The frequency of stools is up to 20 times a day, bowel movements look like rice water. Vomiting is profuse, more than 20 times a day, the vomit resembles rice water. Patients experience increasing weakness, dry mouth, thirst, agitation, irritability, and muscle cramps in the extremities (most often the calf muscles). A third of patients have subnormal body temperature. The skin is dry, pale. The facial features are pointed, the eyeballs are sunken, and the symptom of “dark glasses” is observed. A decrease in skin turgor is detected in the vast majority of patients.
The voice is changed, hoarse and weakened, speaking in a whisper is typical. Heart sounds are muffled, tachycardia and arterial hypotension are noted. In 3/4 of cases, oliguria occurs, in 1/4 - anuria. Hemoconcentration is moderately pronounced (Ht = 0.50–0.55), decompensated metabolic acidosis (pH 7.30–7.36; BE = -0.5–10.0 mmol/l), hypokalemia, and hypochloremia are noted. In the absence of intensive care, the condition of patients worsens and can lead to death.
Dehydration of the IV degree is the most severe form of cholera, which is called algid. It is more appropriate to call this form of the disease decompensated dehydration, since the body is not able to independently maintain water-salt balance and the activity of functional systems. The disease is characterized by a rapid course, continuous profuse stool and vomiting, with the development of hypovolemic shock, which is one of the manifestations of the disease. Sometimes, with the development of intestinal paresis, diarrhea and vomiting may stop and fluid accumulates in the intestinal lumen. The patients are in a state of prostration, consciousness is preserved. Convulsions, general cyanosis, decreased skin turgor, dry mucous membranes are detected in all patients. Hypothermia, absence of peripheral pulse and blood pressure, tachypnea, anuria and aphonia are noted. The skin is cold and sticky to the touch. Cyanosis becomes purple-black in color. The patient's facial features are pointed, the eyes are sunken, there are bluish circles under the eyes (a symptom of “dark glasses”), the eyeballs are turned upward, and the cheeks are sunken. The nose, cheekbones and chin protrude sharply forward - faсies cholerica. The patient's face and appearance express suffering. Muscle cramps become frequent, periods of relaxation are almost not pronounced. With cramps of the fingers, a spasm in the form of an “obstetrician’s hand” is observed. In some patients, “horse foot” is detected or the foot freezes in a sharply extended position. Spasms of the diaphragm muscles cause painful hiccups.
Patients have hypothermia, body temperature drops to 34.5 °C, the skin loses elasticity - “washerwoman’s hands”. The outcome of the disease is determined by hemodynamic disturbances. The pulse is thready or undetectable, heart sounds are barely audible, heartbeats are arrhythmic. Breathing is rapid, shallow, arrhythmic, 40–60 per minute. In some cases, Kussmaul-type breathing is observed. Anuria is detected in all patients. IV degree dehydration is characterized by hemoconcentration (Ht > 0.55), decompensated metabolic acidosis (pH < 7.30; BE exceeds -10 mmol/l), hypokalemia (up to 2.5 mmol/l). When examining the hemostatic system, increased phases I and II of coagulation, increased fibrinolysis, and thrombocytopenia are revealed. Peripheral blood is characterized by erythrocytosis (up to 7 × 106 in 1 μl), leukocytosis (up to 30–60 × 103 in 1 μl with neutrophilia and a shift of the leukocyte formula to the left). The level of urea and creatinine increases. The ECG reveals signs of pulmonary hypertension with diastolic overload of the right heart and tachycardia.
Sometimes even more rapid development of dehydration is possible. In these cases, dehydration shock develops within several hours (one day), and this form of the disease is called fulminant.
Dry cholera occurs without diarrhea and vomiting, but with signs of rapid development of hypovolemic shock - a sharp drop in blood pressure, the development of tachypnea, shortness of breath, convulsions, aphonia, anuria.
The most severe course of cholera is observed in children under 3 years of age. Children tolerate dehydration worse, and they experience secondary damage to the central nervous system (lethargy, clonic convulsions, convulsions, impaired consciousness up to the development of coma). In children, it is difficult to determine the initial degree of dehydration. It is impossible to rely on the relative density of plasma due to the relatively large extracellular volume of fluid. Therefore, it is advisable to weigh children upon admission to most reliably determine their degree of dehydration. The course of cholera in children has some features: frequent increases in body temperature, more pronounced apathy, adynamia, and a tendency to epileptiform seizures, as hypokalemia quickly develops. The disease lasts from 3 to 10 days, its subsequent manifestations depend on the adequacy of rehydration therapy. When the loss of fluid and electrolytes is replaced, normalization of physiological functions occurs quite quickly and deaths are rare. The main causes of death in case of inadequate treatment of patients are dehydration shock, metabolic acidosis and uremia as a result of acute tubular necrosis.
Along with the severe course of the disease, erased and subclinical forms of the disease are possible, which are revealed during a detailed examination of carriers. Such patients have a history of short-term diarrhea, stool 1-2 times a day. Patients with a subclinical form of the disease are identified in foci of cholera when the pathogen is detected in the feces; they do not have clinical symptoms of the disease, but a blood test reveals an increase in the titer of vibrioid antibodies.
Complications . Among the complications caused by regional circulatory disorders: myocardial infarction, thrombosis of mesenteric vessels, acute cerebrovascular accident. A frequent complication is pneumonia, focal or segmental, in elderly people - hypostatic. Complications include acute renal failure with a predominance of the prerenal form. Exicosis contributes to the development of abscesses, phlegmon and erysipelas. Phlebitis and thrombophlebitis are caused by long-term intravenous rehydration therapy.
Diagnostics . In typical cases of the disease in endemic foci of cholera, the diagnosis does not cause difficulty. Diagnosis becomes difficult when cholera is recorded in an area where it was not previously present and must be confirmed bacteriologically. In areas where cases of cholera have already been registered, patients with cholera and acute intestinal diseases should be actively identified at all stages of medical care, as well as through door-to-door visits by medical workers and sanitary commissioners. If a patient is identified with symptoms of gastrointestinal damage, urgent measures are taken to hospitalize him.
The main method of laboratory diagnosis of cholera is bacteriological examination of stool and vomit in order to isolate the pathogen. If it is impossible to deliver the material to the laboratory in the first 3 hours after collection, then use preservative media (alkaline 1% peptone water, etc.). The material is collected in individual vessels, washed from disinfectant solutions, at the bottom of which a smaller vessel or sheets of parchment paper are placed, disinfected by boiling. The secretions (10–20 ml) are collected using metal spoons into sterile glass jars or test tubes, closed with a tight stopper. In patients with gastroenteritis, material can be taken from the rectum using a rubber catheter. For active collection of material, rectal cotton swabs and tubes are used.
When examining convalescents and healthy individuals who have been in contact with sources of infection, a saline laxative (20–30 g of magnesium sulfate) is first given. All samples for research are delivered in sterile sealed containers with an accompanying person. Each sample is accompanied by a direction in which the first and last name of the patient, the name of the sample, the place and time of collection, the intended diagnosis and the name of the person who took the material are indicated. The indicative test is microscopy of fixed stained smears of stool and vomit. Clusters of vibrios look like schools of fish. Accelerated research methods are immunofluorescence microscopy and the crushed drop method. The research materials are feces, vomit, portions B and C of bile, sectional material, water, food and other environmental objects. To isolate and identify pure culture, enrichment media, selective and differential diagnostic media are used. The results of the express study are obtained after 2–6 hours (approximate answer), accelerated analysis after 8–22 hours (preliminary answer), and full analysis after 36 hours (final answer). Immobilization and microagglutination of vibrios with cholera serum are used as accelerated diagnostic methods; the answer is obtained in a few minutes. All these studies are carried out comprehensively. Serological blood tests (neutralization reaction, enzyme immunoassay) are used in patients with a typical clinical picture of cholera, if Vibrio cholerae is not isolated from feces and vomit. The titers of agglutinins, vibriocidal antibodies and antitoxins are determined. If there are antibody titers (agglutinins 1:40, vibriocidal antibodies 10–4, antienterotoxins - 30 antitoxic units, antimembranotoxins - 50 antitoxic units), cholera should be suspected. The result is positive when the antibody titers in paired sera increase by 4 times. Serological research methods are secondary and are used for retrospective diagnosis.
The presence of Vibrio cholerae in stool is confirmed by laboratory tests. The use of a new rapid diagnostic test (RDT) allows patients to be tested quickly. RDT is currently in the WHO approval process for inclusion in the list of prequalified products. At the same time, in case of positive RDT results, WHO suggests retesting all samples using classical laboratory methods for confirmation. If an outbreak is confirmed, clinical diagnosis based on the WHO standard case definition, with additional testing of selected cases at regular intervals, is sufficient.
Read the end of the article (“Treatment”) in the next issue.
G. K. Alikeeva, Candidate of Medical Sciences N. D. Yushchuk, Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Medical Sciences N. Kh. Safiullina, Candidate of Medical Sciences A. V. Sundukov, Doctor of Medical Sciences, Professor G. M. Kozhevnikova, Doctor medical sciences, professor
MGMSU, Moscow
Contact information for authors for correspondence
Complications
Without proper treatment, cholera can quickly become fatal. In the most severe cases, loss of large amounts of fluid and electrolytes can cause death within hours. In other cases, people who do not receive the necessary care may die from dehydration and dehydration shock 1-2 days after the first symptoms of cholera² appear.
Although severe dehydration is considered the most dangerous complication of cholera, other problems can occur with this pathology:
- Low blood sugar (hypoglycemia). Low levels of sugar (glucose) in the blood - the main source of energy for the body - are characteristic of severe forms of cholera. Hypoglycemia can be accompanied by convulsions, loss of consciousness and lead to death. Children are most susceptible to low glucose levels due to cholera.
- Low potassium levels (hypokalemia). Patients with cholera, due to diarrhea, lose a large amount of electrolytes, including potassium, as a result of which the functioning of the heart and nervous system is disrupted, which poses a threat to the patient’s life.
- Kidney failure. When the kidneys lose their filtering ability, excess fluid, some electrolytes and metabolic products accumulate in the body, which is also life-threatening.
- Secondary infection. Against the background of cholera, the body becomes more susceptible to other bacteria. This can lead to complications such as pneumonia, abscesses, and sepsis.
Forms of cholera
Doctors distinguish several forms of cholera depending on the key classification criterion.
Based on the characteristics of the clinical picture, the following forms can be distinguished:
- typical cholera with damage to the gastrointestinal tract;
- atypical form (possible in those suffering from alcoholism, during pregnancy, against the background of immunodeficiency, taking antibiotics, vaccination against cholera, fasting).
With atypical forms, we can distinguish:
- fulminant course - begins quickly, vomiting and stool are very frequent, shock from dehydration can occur in the first 3 - 6 hours of illness;
- dry form with a rapid onset and the onset of coma and toxicosis even before the onset of diarrhea;
- erased form - begins smoothly, gradually, diarrhea 1-3 times a day with mushy stools, mild weakness and malaise (diagnosis in this case can only be made based on laboratory data, or during an epidemic based on data on contact with a sick person);
- asymptomatic form - there are no clinical signs of infection, but cholera vibrios are detected in tests.
Vaccination against cholera
Specific prevention of cholera is represented by a vaccine that is taken orally. Currently, three drugs have been developed and approved for use⁴:
- WC/rBS. The composition includes killed whole cells of Vibrio cholerae.
- CVD 103-Hg-R. Developed from live, attenuated, genetically modified Vibrio cholerae.
- Vaxchora is an attenuated live vaccine. Currently not registered in Russia.
Vaccination against cholera is given to people living in endemic regions and at high risk of infection. It is also recommended for people planning to travel to countries where cholera outbreaks have recently been reported. In this case, immunization is carried out at least 10 days before travel.
The complete vaccination program depends on the drug and the age of the person and may include 2-3 doses, administered at intervals of 1-2 weeks. A full course of vaccination provides protection against cholera for three years, while a single dose provides short-term protection.
No cholera vaccine provides 100% protection, and vaccination does not replace standard prevention and control measures, including food and water precautions⁴.
Modes of transmission of cholera in adults
The main source of pathogens is considered to be sick people or carriers of bacteria. A person excretes a lot of cholera vibrios during the first days through vomiting and stool. It is especially difficult to identify those people who easily carry cholera, since they are especially dangerous in terms of spreading the disease. Therefore, in outbreaks where infection is detected, all people who have been in contact with the patient are examined, even if they do not have a single symptom. The degree of contagiousness of patients gradually decreases; by the third week of infection, the body is cleared of bacteria and the person recovers. But for some people who have recovered from the disease, carriage of the bacteria continues for about a year or more. This is usually facilitated by existing diseases.
Cholera pathogens can be transmitted through dishes and household items, dirty hands, as well as through contaminated water and food. In addition, these bacteria are actively spread by flies.
People of any age are susceptible to the disease, but it can be especially severe in children, people with anemia, those who drink alcohol, and those who have parasitic diseases.
Prognosis and prevention
With mild and moderate forms of the disease, the prognosis is relatively favorable. However, even in such cases, without timely assistance, complications can develop that lead to death. After an illness, a person has a strong immune system.
Although cholera is rare in Europe, the risk of infection still exists. You should also take additional precautions when visiting countries with active cholera outbreaks among the population. For this purpose, specific and nonspecific prevention is used.
The main measures for nonspecific prevention of cholera include:
- Compliance with personal hygiene rules. You should wash your hands frequently with soap and water, especially after using the toilet and before handling food. If soap and water are not available, an alcohol-based hand sanitizer should be used.
- Drink only high-quality water. It is important to drink only safe water, including bottled, boiled or disinfected water. It can even be used to brush your teeth. Hot drinks, drinks in cans or bottles are generally safe, but the outside of the package must be disinfected before opening. Also, you should not add ice to drinks unless you are sure that it is made from clean water.
- Eating only proven food. You should give preference to home-cooked and hot food, and if possible avoid food from street vendors. It is recommended to avoid sushi, as well as any raw or improperly prepared fish and seafood. It is important to eat fruits and vegetables that you can peel yourself, such as bananas, oranges and avocados.