Pancreatitis and cholecystitis are common diseases nowadays. Cholecystitis, a disease that affects the gallbladder, and pancreatitis, a disease that affects the pancreas, often accompany each other and therefore it is necessary to treat them together. The causes and symptoms of these diseases are largely similar to each other, and the treatment methods have a lot in common. How to treat cholecystitis and pancreatitis?
Causes and symptoms of cholecystitis
Proper nutrition is the key to healthy gastrointestinal tract
Cholecystitis is a disease that is characterized by the occurrence of inflammatory processes in the gallbladder. This organ is located next to the liver and is directly involved in digestion. When the functions of the gallbladder are impaired, the excretory ducts do not work properly and therefore bile accumulates inside the bladder, as a result of which the patient feels severe pain, and infections may develop inside the organ.
A number of different reasons can lead to the development of this disease, the most important of which is gallstone disease. Stones that appear in the bladder often clog the ducts, which leads to disruption of their excretory function.
Also, this disease can develop due to injury, or as a result of complications of other diseases, such as diabetes. In these cases, cholecystitis is not considered an independent disease, since it is a complication of another disease. All these reasons lead to the development of an acute form of cholecystitis. If the disease is left untreated for a long time, a chronic form of the disease may develop, resulting in hardening of the gallbladder walls.
Cholecystitis most often affects people over 50 years of age. The disease is characterized by the fact that at the beginning of its onset the patient begins to feel acute pain in the right side, just below the ribs. The pain is characterized by sudden onset and often develops after the duct is blocked by a stone. After this, the inflammatory process inside the organ begins.
After some time, the pain disappears on its own or after taking a painkiller. After some time, the pain returns with even greater intensity, and there is some regularity in its appearance. The disease worsens, the patient suffers from nausea and vomiting, and his temperature rises. His general condition is deteriorating.
As a result, the excretion of bile into the intestines stops altogether. The patient's skin becomes yellow, the tongue becomes dry, with a white coating. If these symptoms appear, the patient should consult a doctor as soon as possible, since the disease in its advanced form can provoke the development of peritonitis.
Cholecystitis is a disease of the gallbladder that can occur either as a result of other serious diseases or independently. The reason for its appearance is a violation of the excretory function of the bile ducts, as a result of which bile does not enter the intestines.
CHRONIC CHOLECYSTITIS
The most common chronic diseases of the gallbladder and biliary tract include chronic cholecystitis [1].
Chronic cholecystitis is an inflammatory disease that causes damage to the wall of the gallbladder, the formation of stones in it and motor-tonic disorders of the biliary system. Develops gradually, rarely after acute cholecystitis. In the presence of stones they speak of chronic calculous cholecystitis, in their absence - chronic acalculous cholecystitis. It often occurs against the background of other chronic diseases of the gastrointestinal tract: gastritis, pancreatitis, hepatitis. Women are more often affected [2].
The development of chronic cholecystitis is caused by bacterial flora (Escherichia coli, streptococci, staphylococci, etc.), in rare cases, anaerobes, helminthic invasion (opisthorchia, giardia) and fungal infection (actinomycosis), hepatitis viruses. There are cholecystitis of toxic and allergic nature.
Penetration of microbial flora into the gallbladder occurs by enterogenous, hematogenous or lymphogenous routes. A predisposing factor in the occurrence of cholecystitis is stagnation of bile in the gallbladder, which can be caused by gallstones, compression and kinks of the bile ducts, dyskinesia of the gallbladder and biliary tract, disturbances in the tone and motor function of the biliary tract under the influence of various emotional stress, endocrine and autonomic disorders, pathological reflexes of altered organs of the digestive system. Stagnation of bile in the gallbladder is also promoted by prolapse of the viscera, pregnancy, sedentary lifestyle, rare meals, etc.; The reflux of pancreatic juice into the bile ducts during dyskinesia with its proteolytic effect on the mucous membrane of the bile ducts and gallbladder is also important [1].
The direct impetus for an outbreak of the inflammatory process in the gallbladder is often overeating, especially eating very fatty and spicy foods, drinking alcoholic beverages, or an acute inflammatory process in another organ (tonsillitis, pneumonia, adnexitis, etc.).
Chronic cholecystitis can occur after acute cholecystitis, but more often it develops independently and gradually, against the background of cholelithiasis, gastritis with secretory insufficiency, chronic pancreatitis and other diseases of the digestive system, obesity [3]. Risk factors for the development of chronic cholecystitis are presented in Table 1.
Chronic cholecystitis is characterized by a dull, aching pain in the right hypochondrium that is constant or occurs 1–3 hours after eating a large and especially fatty and fried meal. The pain radiates upward, to the area of the right shoulder and neck, right shoulder blade. Periodically, sharp pain resembling biliary colic may occur. Dyspeptic symptoms are common: a feeling of bitterness and a metallic taste in the mouth, belching of air, nausea, flatulence, defecation disorders (often alternating constipation and diarrhea), as well as irritability and insomnia.
Jaundice is not typical. When palpating the abdomen, as a rule, sensitivity and sometimes severe pain in the projection of the gallbladder onto the anterior abdominal wall and slight muscular resistance of the abdominal wall (resistance) are determined. Symptoms of Mussi-Georgievsky, Ortner, Obraztsov-Murphy are often positive. The liver is somewhat enlarged, with a dense and painful edge on palpation in case of complications (chronic hepatitis, cholangitis). In most cases, the gallbladder is not palpable, since it is usually wrinkled due to a chronic scar-sclerosing process. During exacerbations, neutrophilic leukocytosis, increased ESR and temperature reaction are observed. During duodenal intubation, it is often not possible to obtain cystic portion B of bile (due to a violation of the concentrating ability of the gallbladder and a violation of the gallbladder reflex) or this portion of bile has a slightly darker color than A and C, and is often cloudy. Microscopic examination of the duodenal contents reveals a large amount of mucus, desquamated epithelial cells, and leukocytes, especially in portion B of bile (the detection of leukocytes in bile is not given the same importance as before; as a rule, they turn out to be the nuclei of decaying cells of the duodenal epithelium). Bacteriological examination of bile (especially repeated) makes it possible to determine the causative agent of cholecystitis.
During cholecystography, a change in the shape of the gallbladder is noted, often its image is unclear due to a violation of the concentrating ability of the mucous membrane, sometimes stones are found in it. After taking the irritant - cholecystokinetics - there is insufficient contraction of the gallbladder. Signs of chronic cholecystitis are also determined by ultrasound examination (in the form of thickening of the walls of the bladder, its deformation, etc.).
The course in most cases is long, characterized by alternating periods of remission and exacerbation; the latter often arise as a result of eating disorders, drinking alcohol, heavy physical work, acute intestinal infections, and hypothermia.
The prognosis is favorable in most cases. Deterioration of the general condition of patients and temporary loss of their ability to work are typical only during periods of exacerbation of the disease. Depending on the characteristics of the course, latent (sluggish) forms are distinguished, the most common being recurrent, purulent-ulcerative forms of chronic cholecystitis.
Complications: addition of chronic cholangitis, hepatitis, pancreatitis. Often the inflammatory process is the “impetus” for the formation of gallstones.
Diagnosis of chronic cholecystitis
Diagnosis of chronic cholecystitis is based on the analysis of:
- medical history (characteristic complaints, very often there are other patients with biliary tract pathology in the family) and clinical picture of the disease;
- ultrasound data;
- results of computed tomography of the hepatopancreatobiliary zone, hepatoscintigraphy;
- clinical and biochemical parameters of blood and bile;
- indicators of scatological research.
A distinctive feature of the diagnosis of chronic cholecystitis is duodenal intubation followed by microscopic and biochemical studies of the composition of bile.
Duodenal intubation is performed in the morning on an empty stomach. The best choleretic agent used to obtain portions B and C during duodenal intubation is cholecystokinin, when used, duodenal bile contains much less impurities of gastric and intestinal juices. It has been proven that it is most rational to perform fractional (multi-stage) duodenal intubation with an accurate account of the amount of released bile over time. Fractional duodenal intubation allows you to more accurately determine the type of bile secretion.
The process of continuous duodenal intubation consists of 5 stages. The amount of bile released for every 5 minutes of probing is recorded on the graph.
The first stage is the time of the common bile duct, when light yellow bile flows from the common bile duct in response to irritation of the duodenal wall by the olive probe. Collect 3 portions, 5 minutes each. Normally, the rate of bile secretion in portion A is 1-1.5 ml/min. At a higher rate of bile flow, there is reason to think about hypotension, at a lower rate - about hypertension of the common bile duct. Then, a 33% solution of magnesium sulfate is slowly (over 3 minutes) injected through the probe (in accordance with the patient’s return - 2 ml per year of life) and the probe is closed for 3 minutes. In response to this, a reflex closure of the sphincter of Oddi occurs, and the flow of bile stops.
The second stage is the “time of closed sphincter of Oddi.” It begins from the moment the probe opens until bile appears. In the absence of pathological changes in the biliary tract system, this time for the specified stimulus is 3–6 minutes. If the “closed sphincter of Oddi time” is more than 6 minutes, then a spasm of the sphincter of Oddi is assumed, and if it is less than 3 minutes, its hypotension is assumed.
The third stage is the time of release of bile portion A. It begins from the moment the sphincter of Oddi opens and the appearance of light bile. Normally, 4–6 ml of bile flows out in 2-3 minutes (1-2 ml/min). A higher speed is observed with hypotension, a lower speed is observed with hypertension of the common bile duct and sphincter of Oddi.
The fourth stage is the time of release of bile of portion B. It begins with the release of dark cystic bile due to relaxation of the Lutkens sphincter and contraction of the gallbladder. Normally, about 22–44 ml of bile is secreted in 20–30 minutes, depending on age. If the emptying of the gallbladder occurs faster and the amount of bile is less than specified, then there is reason to think about hypertonic-hyperkinetic dysfunction of the bladder, and if emptying is slower and the amount of bile is greater than specified, then this indicates hypotonic-hypokinetic dysfunction of the bladder, one of the reasons for which may be hypertension of the Lütkens sphincter (with the exception of cases of atonic cholestasis, the final diagnosis of which is possible with ultrasound, cholecystography, and radioisotope studies).
The fifth stage is the time of release of bile of portion C. After the gallbladder is emptied (outflow of dark bile), bile of portion C is released (lighter than bile A), which is collected at 5-minute intervals for 15 minutes. Normally, portion C bile is secreted at a rate of 1-1.5 ml/min. To check the degree of emptying of the gallbladder, the irritant is reintroduced, and if dark bile “comes out” again (portion B), then it means that the bladder has not contracted completely, which indicates hypertensive dyskinesia of the sphincter apparatus.
If it was not possible to obtain bile, then probing is carried out after 2-3 days while preparing the patient with atropine and papaverine. Immediately before probing, it is advisable to use diathermy, faradization of the phrenic nerve. Bile microscopy is performed immediately after probing. The material for cytological examination can be preserved for 1-2 hours by adding a 10% solution of neutral formaldehyde (2 ml of a 10% solution per 10-20 ml of bile).
All 3 portions of bile (A, B, C) must be sent for culture.
Microscopy of bile. Leukocytes in bile can be of oral, gastric and intestinal origin, therefore, during duodenal intubation, it is better to use a two-channel probe, which allows you to constantly suck out gastric contents. In addition, with unconditionally proven cholecystitis (during surgery in adults), in 50–60% of cases, the content of leukocytes in the bile of portion B is not increased. Leukocytes in bile are now given relative importance in the diagnosis of cholecystitis.
In modern gastroenterology, diagnostic significance is not attached to the detection of a portion of B leukocytes and cellular epithelium of the biliary tract in bile. The most important criterion is the presence in portion B of microlites (accumulation of mucus, leukocytes and cellular epithelium), cholesterol crystals, lumps of bile acids and calcium bilirubinate, brown films - deposition of mucus in the bile on the wall of the gallbladder.
The presence of Giardia and opisthorchia can support various pathological (mainly inflammatory and dyskinetic) processes in the gastrointestinal tract. Giardia does not live in the gallbladder of healthy people, since bile causes their death. The bile of patients with cholecystitis does not have these properties: Giardia settles on the mucous membrane of the gallbladder and contributes (in combination with microbes) to maintaining the inflammatory process and dyskinesia.
Thus, Giardia cannot cause cholecystitis, but can cause the development of duodenitis, biliary dyskinesia, i.e. aggravate cholecystitis, contributing to its chronic course. If vegetative forms of Giardia are found in the patient’s bile, then, depending on the clinical picture of the disease and the results of duodenal intubation, either chronic cholecystitis or biliary dyskinesia is made as the main diagnosis, and intestinal giardiasis is made as a concomitant diagnosis.
Of the biochemical abnormalities of bile, signs of cholecystitis are an increase in protein concentration, dysproteinocholia, an increase in the concentration of immunoglobulins G and A, C-reactive protein, alkaline phosphatase, and bilirubin.
The results of probing should be interpreted taking into account the history and clinical picture of the disease. Computed tomography has diagnostic value for identifying cervical cholecystitis.
In addition to those presented above, the following risk factors for the development of cholecystitis are identified: heredity; previous viral hepatitis and infectious mononucleosis, sepsis, intestinal infections with a prolonged course; intestinal giardiasis; pancreatitis; malabsorption syndrome; obesity, obesity; a sedentary lifestyle combined with poor nutrition (in particular, abuse of fatty foods and canned industrial products); hemolytic anemia; association of pain in the right hypochondrium with eating fried, fatty foods; clinical and laboratory data that persists for a year or more, indicating biliary dyskinesia (especially diagnosed as the only pathology); persistent low-grade fever of unknown origin (with the exception of other foci of chronic infection in the nasopharynx, lungs, kidneys, as well as tuberculosis, helminthiasis). Detection of typical “vesical symptoms” in a patient in combination with 3-4 of the risk factors listed above makes it possible to diagnose cholecystopathy, cholecystitis or dyskinesia without duodenal intubation. Ultrasound confirms the diagnosis.
Echographic (ultrasound) signs of chronic cholecystitis:
- diffuse thickening of the walls of the gallbladder more than 3 mm and its deformation;
- compaction and/or layering of the walls of the organ;
- reduction in the volume of the organ cavity (wrinkled gallbladder);
- “inhomogeneous” cavity of the gallbladder.
In many modern guidelines, ultrasound diagnostics is considered decisive in identifying the nature of gallbladder pathology.
As already mentioned, biliary dyskinesia cannot be the main or only diagnosis. Long-term biliary dyskinesia inevitably leads to excessive contamination of the intestine, and that, in turn, to infection of the gallbladder, especially with hypotonic dyskinesia.
In case of chronic disease of the biliary tract, cholecystography is performed to exclude malformations. An X-ray examination of patients with hypotonic dyskinesia reveals an enlarged, downward expanding and often prolapsed gallbladder; its emptying is slow. There is gastric hypotension.
With hypertensive dyskinesia, the shadow of the gallbladder is reduced, intense, oval or spherical in shape, emptying is accelerated.
Instrumental and laboratory data
- Blood test during exacerbation: neutrophilic leukocytosis, accelerated ESR to 15–20 mm/h, appearance of C-reactive protein, increase in α1- and γ-globulins, increased activity of liver spectrum enzymes: aminotransferases, alkaline phosphatase, γ-glutamate dehydrogenase, and also the level of total bilirubin.
- Duodenal intubation: the time of appearance of portions and the amount of bile are taken into account. If flakes of mucus, bilirubin, and cholesterol are detected, they examine it microscopically: the presence of leukocytes, bilibirubinates, and lamblia confirms the diagnosis. The presence of changes in portion B indicates a process in the bladder itself, and in portion C indicates a process in the bile ducts.
- Ultrasound of the hepatobiliary zone will reveal diffuse thickening of the walls of the gallbladder of more than 3 mm and its deformation, compaction and/or layering of the walls of this organ, a decrease in the volume of the gallbladder cavity (wrinkled bladder), and an “inhomogeneous” cavity. In the presence of dyskinesia, there are no signs of inflammation, but the bladder will be greatly stretched and empties poorly or very quickly.
The course of chronic cholecystitis can be recurrent, hidden latent or in the form of attacks of hepatic colic.
With frequently recurrent cholecystitis, cholangitis may develop. This is an inflammation of the large intrahepatic ducts. The etiology is basically the same as for cholecystitis. Often accompanied by increased body temperature, sometimes chills, and fever. The temperature is well tolerated, which is generally characteristic of coli-bacillary infection. The liver is characterized by enlargement, its edge becomes painful. Yellowness often appears, associated with a deterioration in the outflow of bile due to blockage of the bile ducts with mucus, and itchy skin. Blood tests revealed leukocytosis, accelerated ESR.
Treatment
During exacerbations of chronic cholecystitis, patients are hospitalized in surgical or therapeutic hospitals and treated as for acute cholecystitis. In mild cases, outpatient treatment is possible. Prescribe bed rest, dietary nutrition (diet No. 5a) with meals 4–6 times a day [1].
Etiotropic treatment is prescribed, as a rule, in the phase of exacerbation of the process. Among antibiotics, it is recommended to prescribe broad-spectrum drugs that enter the bile in fairly high concentrations - macrolides, the latest generation clarithromycin (synonyms: Klacid, Fromilid) 250 mg, 500 mg 2 times a day and the more well-known erythromycin 250 mg 4 times a day, long-acting tetracyclines doxycycline 100 mg, Unidox Solutab 100 mg according to the regimen on the first day 200 mg in 2 doses, then 100 mg with meals for 6 days. All drugs are prescribed in usual therapeutic doses in courses of 7–10 days. For giardiasis of the biliary tract, metronidazole 200 or 400 mg, daily dose 1200 mg (synonyms: metrogil, trichopolum, Klion) or tinidazole 500 mg, daily dose 2 g for 2-3 days are effective. For opisthorchiasis of the biliary tract, the antiparasitic drug praziquantel 600 mg 25 mg/kg 1–3 times a day is effective.
To eliminate biliary dyskinesia, spastic pain, and improve bile flow, symptomatic therapy is prescribed with one of the following medications.
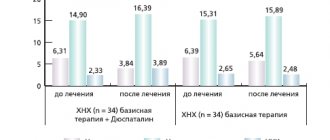
Selective myotropic antispasmodics: mebeverine (duspatalin) 200 mg 2 times a day (morning and evening, course of treatment for 14 days).
Prokinetics: cisapride (Coordinax) 10 mg 3-4 times a day; domperidone (Motilium) 10 mg 3-4 times a day; metoclopromide (cerucal, raglan) 10 mg 3 times a day.
Systemic myotropic antispasmodics: no-spa (drotaverine) 40 mg 3 times a day; nikoshpan (no-spa + vitamin PP) 100 mg 3 times a day.
M-anticholinergics: buscopan (hyocinabutyl bromide) 10 mg 2 times a day.
Comparative characteristics of systemic and selective antispasmodics are reflected in Table 2.
Advantages of the selective antispasmodic mebeverine (duspatalin)
- Duspatalin has a dual mechanism of action: it eliminates spasm and does not cause intestinal atony.
- It acts directly on the smooth muscle cell, which, due to the complexity of the nervous regulation of the intestine, is preferable and allows one to obtain a predictable clinical result.
- It does not affect the cholinergic system and therefore does not cause side effects such as dry mouth, blurred vision, tachycardia, urinary retention, constipation and weakness.
- Can be prescribed to patients suffering from prostate hypertrophy.
- Selectively acts on the intestines and biliary tract.
- There are no systemic effects: the entire administered dose is completely metabolized when passing through the intestinal wall and liver to inactive metabolites and mebeverine is not detected in plasma in the blood.
- Extensive clinical experience.
- If there is reflux of bile into the stomach, antacid drugs are recommended, 1 dose 1.5-2 hours after eating: Maalox (algeldrate + magnesium hydrochloride), phosphalugel (aluminum phosphate).
Disturbances in the outflow of bile in patients with chronic cholecystitis can be corrected with choleretic drugs. There are choleretic drugs with choleretic action, which stimulate the formation and secretion of bile by the liver, and cholekinetic drugs, which enhance muscle contraction of the gallbladder and the flow of bile into the duodenum.
Choleretic drugs:
- oxafenamide, cyclone, nicodine - synthetic agents;
- hophytol, allohol, tanacechol, pumpkinol, cholenzyme, lyobil, flamin, immortelle, holagon, odeston, hepatofalk planta, hepabene, herbion choleretic drops, corn silk - of plant origin;
- festal, digestal, cotazim are enzyme preparations containing bile acids.
Cholekinetic drugs: cholecystokinin, magnesium sulfate, sorbitol, xylitol, Carlsbad salt, sea buckthorn and olive oil.
Choleretic drugs can be used for the main forms of cholecystitis, in phases of subsiding exacerbation or remission, usually prescribed for 3 weeks, then it is advisable to change the drug.
Cholekinetics should not be prescribed to patients with calculous cholecystitis; they are indicated for patients with non-calculous cholecystitis with hypomotor dyskinesia of the gallbladder. Therapeutic duodenal intubation, 5-6 times every other day, is effective in patients with non-calculous cholecystitis, especially with hypomotor dyskinesia. In the remission phase, such patients should be recommended “blind duodenal intubation” once a week or 2 weeks. To carry them out, it is better to use xylitol and sorbitol. In patients with calculous cholecystitis, duodenal intubation is contraindicated due to the risk of developing obstructive jaundice.
Patients with noncalculous cholecystitis with disturbances in the physicochemical properties of bile (discrinia) are prescribed wheat bran and enterosorbents (Enterosgel 15 g 3 times a day) for a long period of time (3–6 months).
Diet: limiting fatty foods, limiting high-calorie foods, excluding poorly tolerated foods. Regular 4-5 meals a day.
If conservative treatment fails and frequent exacerbations occur, surgical intervention is necessary.
Prevention of chronic cholecystitis consists of following a diet, playing sports, physical education, preventing obesity, and treating focal infections.
For questions regarding literature, please contact the editor.
T. E. Polunina, Doctor of Medical Sciences E. V. Polunina “Guta-Clinic”, Moscow
What do these diseases have in common and how to treat them?
Cholecystitis and pancreatitis have similar symptoms
Both the gallbladder and the pancreas have similar functions - they produce enzymes that contribute to the normal digestion process. The first organ is responsible for dosing the bile produced by the liver so that it arrives in the right quantities, and the second organ produces pancreatic juice. If the functions of one of the organs are impaired, disturbances in the functioning of the other are observed.
Pancreatitis and cholecystitis, as is customary, are treated with medications. Therapy is often supplemented by the use of traditional medicine, as well as the prescription of a variety of diets. The main requirement for food intake in these diseases is frequent split meals. It promotes more effective action of medications used during therapy.
It is recommended to limit the consumption of foods that are too fatty and eat more healthy foods, such as steamed vegetables. It is also useful to drink a glass of kefir before bed. Typically, diseases are treated with the complex use of various drugs aimed at combating the main symptoms of the disease. Properly thought out treatment helps restore the functions of the gallbladder and pancreas. The main medications used for pancreatitis:
Treatment of reactive pancreatitis
Treatment of reactive pancreatitis includes eliminating inflammation of the pancreas, removing intoxication and restoring normal secretion of pancreatic juice. The treatment process must certainly take place under the supervision of a doctor.
Therapeutic fasting can help relieve inflammation, especially in the acute period. It relieves stress from the inflamed pancreas and the entire digestive tract. After the acute phase has passed, it is allowed to eat in small portions, eating crushed foods. But under no circumstances should you adjust your diet on your own. Only a doctor can prescribe a correct and healthy diet, based on the characteristics of your body.
As a rule, those foods that can provoke re-activation of pancreatic enzymes and intensify the inflammatory reaction in tissues are excluded from the patient’s diet for several months.
For reactive pancreatitis, the following are prohibited:
- alcohol;
- fatty and fried foods;
- legumes;
- sour juices;
- fresh baked goods;
- smoked meats, sausages;
- corn;
- mushrooms;
- sauces, seasonings, spices.
It is recommended to steam or boil the meat. It is advisable to prefer lean poultry, beef or rabbit. In the treatment of pancreatitis, it is very important to strictly follow the diet: regular eating disorders can provoke an exacerbation of the disease.
Drug therapy for pancreatitis includes taking enzyme preparations and antispasmodics that eliminate spasm of smooth muscles and relieve pain. The doctor may also prescribe medications that improve intestinal microflora and increase the content of live bacteria in the body.
To learn more
An important stage of treatment is taking enzyme agents based on pancreatin. An inflamed pancreas does not secrete enzymes in the required quantities to ensure high-quality digestion of food and the correct course of digestive processes. Medicines containing enzymes compensate for the lack of natural digestive elements and prevent the occurrence of fermentation and rotting of food in the intestines.
An example of an enzyme preparation used in the treatment of reactive pancreatitis is Creon®. A modern drug of the latest generation, produced in the form of capsules with active minimicrospheres of pancreatin, enclosed in a gelatin shell. Once in the stomach, the capsule quickly dissolves2, and the minimicrospheres are mixed with food and enter the intestines with it, helping the breakdown process and absorption of nutrients. More information about the drug Creon® can be found here.
How to treat cholecystitis and pancreatitis using traditional methods
Often, herbal medicine is used in the treatment of cholecystitis and pancreatitis. Specially selected herbs are effective helpers in the fight against diseases. When choosing these herbs, you should pay attention to their individual tolerance, and also to the fact that many of them can increase or decrease blood pressure, are laxatives, and some of them cause constipation.
Most often, herbs are prescribed that can stop the inflammatory process. These include: dandelion root, calendula, chamomile. If there are stones in the gallbladder or gallstones, then herbs are used that will help dissolve these stones and also change the composition of bile. Together with them, herbs are used that normalize the peristalsis of the bile ducts.
Sometimes stomach enzymes affect the pancreas, stimulating it even when it should be at rest. For this reason, herbs are used to reduce the production of gastric juice. There are some ready-made recipes that can be used for pancreatitis and cholecystitis:
- Method one. Mix one part of chamomile, two parts of hawthorn berries and immortelle flowers, and three parts of mint leaves and dill seeds and pour boiling water over it all. A spoonful of the mixture should be poured into a glass of boiling water and, after it has infused, drink a quarter of the glass before meals.
- Method two. Three tablespoons of string, elecampane and mint, mixed in equal amounts, pour one and a half glasses of boiling water and, after boiling them for a couple of minutes on the fire, let it brew for an hour, then drink a third of a glass twice a day, before meals.
- Method three. Pour boiling water over a tablespoon of calendula flowers and leave for eight hours. Drink a third of a glass half an hour before meals.
Traditional medicine is also effective in combating diseases such as pancreatitis and cholecystitis. It should be used in combination with drug treatment and diet: this contributes to a more effective fight against diseases.
Cholecystitis and pancreatitis are diseases of the gallbladder and pancreas. They are similar in many ways, have similar symptoms and causes, and can appear simultaneously. For this reason, their therapy is carried out using similar methods.