Chronic pancreatitis is an inflammation of the pancreas that occurs over a long period of time with periodic exacerbations. Often this pathology is a consequence of the development of disturbances in the outflow of digestive fluid and other enzymes that are synthesized by the pancreas.
The disease poses a considerable danger to any person, as it can even cause death; as a result, it is important for every patient diagnosed with chronic pancreatitis to become familiar with the disease in more detail.
Today’s article on our resource will be an excellent help in this, because it examines a typical example of the history of this disease from the cases of a practicing gastroenterologist. Interested? Scroll below.
Medical history
Abdominal discomfort may be a sign of pancreatitis.
According to the patient, P.S. Klapovnikov, the disease appeared about 7 days ago. The first unpleasant manifestations of the disease appeared during meals.
There was no discomfort for several days. But within a day and directly on the day of admission to the clinic, the symptoms appeared again.
Life of a patient
There are no developmental problems. He ate 4-5 times a day and has no special food preferences. He was not seen by specialized specialists in the clinic.
The last time he was hospitalized was in 2006 due to acute appendicitis. The body systems function stably, there are no chronic ailments. The patient was completely healthy at the time of the last examination (March 1, 2016).
The patient's current condition
Abdominal discomfort when examined by a gastroenterologist will help make a diagnosis.
Condition category: mild severity. Consciousness: consistently clear. Body type: regular, hypersthenic. Patient activity: active. Parameters: height – 186 cm, weight – 97 kg, body temperature – 36.6 degrees Celsius. Lipid, epithelial and muscle tissues, as well as bone structures, are moderately and satisfactorily developed. There are no problems with any nodes in the body, with the exception of the gastrointestinal tract.
Inspection of the basic components of the body
Respiratory organs: the anatomy is normal, there are no pronounced disorders, the location and structure are symmetrical, the patient breathes through the nose and mouth, the type of breathing is mixed, the frequency of respiratory function is about 22 inhalations/exhalations per minute.
Epithelium: no problems, developed normally, good condition. Muscles and skeleton: no pathologies, well developed. Cardiovascular system: no pathologies were identified during the basic examination. Other body nodes: no pathologies were identified.
Profile examination by a gastroenterologist
Chronic pancreatitis can be examined using ultrasound.
The structure and anatomy of the ribs, gastrointestinal tract and nearby organs are not disturbed. The abdomen is slightly enlarged in size due to the presence of ascitic fluid, the appearance of which is caused by an attack of the disease.
The belly shape is “frog”. There is symmetry, complete. There are no hernias, ulcers or similar formations. The patient has his own teeth.
Etiology
Alcohol use is the most common cause of chronic pancreatitis in the United States. Factors that predispose some (but not all) heavy drinkers to the development of chronic pancreatitis remain unclear. A diet rich in fat and protein may be a predisposing factor. Smoking does not appear to play an important role in the development of alcoholic pancreatitis, but may increase the risk of developing calcifications in chronic pancreatitis [4]. In approximately 20% of cases of chronic pancreatitis, it is idiopathic in nature, and in the remaining cases it is associated with various other causes, including tropical pancreatitis, cystic fibrosis, hyperparathyroidism and hereditary pancreatitis[5].
There are no specific histological markers for various etiological types of pancreatitis. Consequently, it is difficult for a morphologist to distinguish between alcoholic and non-alcoholic chronic pancreatitis when examining biopsy specimens [2].
Surveys
To make an accurate diagnosis, the following types of examinations are prescribed:
- blood tests (clinical, biochemistry);
- examination of urine and stool;
- X-ray of the abdominal cavity without contrast;
- Ultrasound of adjacent organs to the gastrointestinal tract (liver, gallbladder, pancreas);
- ECG.
Pathophysiology
The pathophysiology of chronic pancreatitis remains unclear and there are separate theories of its development under different etiological factors. Hereditary pancreatitis and cystic fibrosis, leading to chronic pancreatitis, develop at an early age and are characterized by severe calcification. Obstructive chronic pancreatitis develops as a result of congenital or acquired stricture of the pancreatic duct, for example, as with bifurcation of the pancreas. The latter leads to compression of the lumen of the dorsal duct. Acquired stricture, on the other hand, may be the result of trauma, pseudocyst, necrotizing pancreatitis, or tumor. When the obstruction is removed, the dilation of the duct may disappear. The pathophysiology of chronic pancreatitis is based on basal hypersecretion of pancreatic proteins with a simultaneous decrease in protease inhibitors. The latter alters the biochemical structure of pancreatic juice and predisposes individuals to the formation of protein plugs and the formation of pancreatic stones. Blockage of small ducts causes premature activation of pancreatic enzymes, which leads to the development of acute pancreatitis, which, over time, causes permanent structural damage to the glands [6].
Much attention has been directed to the mechanism of the effect of alcohol on the development of chronic pancreatitis. One theory says that its chronic use leads to the secretion of protein-rich pancreatic juice. A diet rich in protein and lipids is thought to alleviate protein hypersecretion (which includes digestive enzymes) and ultimately blockage of the ducts and the formation of protein plugs. The discovery of the genetic code for hereditary pancreatitis has contributed to our understanding of the pathogenesis of chronic pancreatitis [7].
Test results
A blood test is a very important procedure for making a correct diagnosis.
Based on the results of the surveys, the following results were obtained:
- clinical blood test – indicators are normal;
- biochemical blood test – the indicators are normal;
- X-ray of the abdominal cavity is normal, there are no free gases;
- Ultrasound of the underlying organs to the gastrointestinal tract - the liver is in a “normal” state, the pancreas is moderately enlarged, the gallbladder is in an irregular shape and has no stones.
Conclusion based on the results of the diagnostics: diffuse disorders of adjacent organs to the gastrointestinal tract. The results of the examinations are discussed in more detail in the appendices to the medical history.
Biliary-dependent pancreatitis (case report)
The article discusses the main causes of acute and chronic biliary-dependent pancreatitis and the features of its treatment. A clinical case of acute biliary pancreatitis that developed during treatment for cholelithiasis, with further development of chronic pancreatitis as a result of persistence of biliary sludge, was analyzed.
Table 1. Clinical blood test
Table 2. Biochemical blood test
Putty-like bile in the terminal portion of the common bile duct
As shown by the results of a retrospective (20-year period) study devoted to the analysis of the causes of acute pancreatitis, biliary-dependent pancreatitis occurs in 26.9% of patients [1]. The main cause of its development is cholelithiasis (GSD). Acute pancreatitis is considered one of the main complications of cholelithiasis [2].
In recent decades, there has been a worldwide trend toward an increase in the incidence of biliary pancreatitis as a result of an increase in the incidence of cholelithiasis [3]. Thus, according to various authors, the incidence of biliary pancreatitis in patients with cholelithiasis is 25–90% [4].
The leading factor in the pathogenesis of biliary pancreatitis is an increase in pressure in the bile ducts due to the occurrence of a mechanical obstruction (calculus, biliary sludge, stricture, tumor, etc.), especially distal to the junction of the common bile duct with the main pancreatic duct, or dysfunction of the sphincter of Oddi. The development of pathological biliopancreatic reflux against this background and impaired outflow of pancreatic secretions can lead to acute biliary pancreatitis [5].
Biliary-dependent pancreatitis differs from pancreatitis of other etiologies (alcoholic, nutritional, post-traumatic) in that the etiological factor, as a rule, is not eliminated. Its effect continues against the background of a developing process in the pancreas (P) and parapancreatic tissue [6].
Particular importance in the development of biliary pancreatitis is given to biliary sludge. The frequency of its detection in patients with idiopathic pancreatitis is 30–75%. When examining bile within the first day from the onset of a pancreatic attack, biliary sludge is detected in 80% of cases [7].
In one study, researchers followed 104 patients with biliary sludge for 630 days (21 months). 25 (24%) patients developed complications such as cholelithiasis, cholecystitis, choledocholithiasis and pancreatitis. At the same time, 12 patients had non-calculous cholecystitis, and two had acute calculous cholecystitis. Six cases of cholecystolithiasis, one case of choledocholithiasis, and four cases of pancreatitis were registered [8].
Thus, the clinical significance of biliary sludge is difficult to overestimate, since it:
- serves as a source of stone formation: gallstones form in 5–20% of patients over a 1–3-year period;
- promotes the development of strictures of the terminal part of the common bile duct and/or stenotic papillitis;
- can lead to the development of acute cholecystitis, cholangitis, shutdown of the gallbladder (in the presence of putty-like bile);
- is the cause of biliary pancreatitis.
In addition, biliary sludge containing microliths can freely pass through the ductal system and cause unexplained pain in the right hypochondrium in 83% of patients [9].
Biliary sludge is formed in the gallbladder as a result of destabilization of the physicochemical state of bile and precipitation of its main components.
Factors contributing to the persistence of biliary sludge include hypotension of the gallbladder and hypertonicity of the sphincter of Oddi. The constant passage of sludge through the bile ducts leads to damage to the mucous membrane, mainly in the area of the sphincter of Oddi. Trauma to the mucous membrane is caused by microliths, which make up the main part of biliary sludge. As a consequence, secondary dysfunction of the sphincter of Oddi first develops, then stenotic papillitis forms [4].
In addition to stones and biliary sludge, exacerbations of pancreatitis can be caused by dysfunction of the sphincter of Oddi [10], including in patients after cholecystectomy [11]. Thus, in 18.8% of patients with at least one episode of acute pancreatitis or chronic idiopathic pancreatitis, the pancreatic type of sphincter of Oddi dysfunction is detected [11].
Pharmacotherapy of biliary-dependent pancreatitis can be etiological and pathogenetic. If there are indications (gastrointestinal tract disease, bile flow obstruction), endoscopic or surgical treatment is performed.
Etiological therapy involves the use of ursodeoxycholic acid (UDCA) drugs. Pathogenetic depends on the type of prevailing disorders. For hypomotor disorders, prokinetics (domperidone, itopride) are prescribed; for hypermotor disorders, antispasmodics (mebeverine) are prescribed. Combination drugs that simultaneously have both choleretic and antispasmodic effects are also used.
According to the mechanism of action, antispasmodics are divided into neurotropic and myotropic. Neurotropic block the process of transmission of nerve impulses in the autonomic ganglia and nerve endings that stimulate smooth muscle cells. They block M1, M2 and M3 cholinergic receptors of smooth muscle cells. Among the neurotropic antispasmodics there are:
- natural: atropine, hyoscyamine, belladonna preparations, platiphylline, scopolamine;
- synthetic central: adiphenine, aprofen, aprinal, cyclosyl;
- semi-synthetic peripheral: hyoscine butyl bromide.
Myotropic antispasmodics reduce muscle tone through a direct effect on smooth muscle cells. These antispasmodics include ion channel blockers, phosphodiesterase (PDE) type 4 inhibitors, and nitrates. Myotropic antispasmodics are divided into:
- to selective: calcium channel blockers (pinaverium bromide, otilonium bromide);
- sodium channel blockers (mebeverine) and nitric oxide donors (isosorbide dinitrate, nitroglycerin, sodium nitroprusside);
As for pathogenetic therapy, the drug of choice for patients with functional diseases of the biliary tract are drugs that selectively relax the smooth muscles of the gastrointestinal tract. Drugs of this group, in particular mebeverine, have relaxing selectivity for the sphincter of Oddi, 20–40 times greater than the effect of papaverine. At the same time, mebeverine has a normalizing effect on the intestinal muscles, eliminating functional duodenostasis, hyperperistalsis, spasm and without causing unwanted hypotension [13].
Let's consider a clinical example demonstrating the result of successful treatment of biliary-dependent pancreatitis through the administration of etiological and pathogenetic therapy.
Patient K., 76 years old, was hospitalized in the department of pathology of the pancreas and biliary tract of the Moscow Clinical Scientific and Practical Center named after. A.S. Loginova for examination and treatment for repeated exacerbation of chronic pancreatitis.
Upon admission, complaints of pain in the upper abdomen radiating to the back and chest, worsening after eating, nausea, belching, weight loss of 16 kg over two years.
From the anamnesis it is known that abdominal pain first appeared several years ago. The patient was hospitalized with pain. Choledocholithiasis and obstructive jaundice were diagnosed. Endoscopic papillosphincterotomy and extraction of common bile duct stone, complicated by pancreatic necrosis, were performed. Conservative treatment was carried out. Six months later, repeated deterioration was noted - intense pain. The patient was readmitted to the hospital. Diagnosis: chronic pancreatitis, exacerbation. Two years later, laparoscopic cholecystectomy was performed. The pain did not bother me for a year, but a year later it returned. For the next six months, the patient with a diagnosis of “exacerbation of chronic pancreatitis, transient choledocholithiasis” was hospitalized.
Upon objective examination, the condition is satisfactory, the skin and visible mucous membranes are clean and of normal color. Turgor is reduced. There is no swelling. In the lungs there is vesicular breathing, no wheezing. Heart sounds are muffled, the rhythm is correct. Heart rate – 76 beats/min. Blood pressure – 120/80 mm Hg. Art. The tongue is moist and covered with a white coating. The abdomen is of a normal configuration, with star-shaped scars in the epigastric region and right hypochondrium. On palpation, the abdomen is soft, painful in the epigastric region. The liver is at the edge of the costal arch, the spleen is not palpable.
Laboratory and instrumental research.
Clinical blood test without pathological abnormalities (Table 1).
The biochemical blood test showed moderate cholestasis (Table 2). Fecal elastase – over 200 mcg/g. Esophagogastroduodenoscopy.
Parapapillary diverticulum. Condition after papillotomy.
Ultrasound examination of the abdominal organs.
Signs of diffuse liver disease. Biliary hypertension. Expansion of hepaticocholedochus. Choledocholithiasis cannot be excluded, although the stone is not visualized. Diffuse changes in the pancreas (signs of chronic pancreatitis).
To determine further treatment tactics, endosonography of the pancreatobiliary zone was performed. Putty-like bile is visualized in the common bile duct (Figure).
Probably, it was the putty-like bile in the terminal part of the common bile duct that became the cause of frequent exacerbations of chronic biliary-dependent pancreatitis.
To reduce the lithogenicity of bile, the patient was prescribed the drug UDCA Exchol® 500 mg in divisible tablets at a dose of 750 mg/day in three doses. Thanks to this form of release, Exchol® 500 mg can be dosed flexibly, reducing the number of tablets taken [14]. This is very important when choosing UDCA drugs. An equally significant factor is the economic component. The choice of drug in this case was determined by the availability of long-term course treatment.
In order to relieve pain, eliminate spasms and improve the passage of bile into the intestine, Sparex® 200 mg was prescribed in two doses before meals. After three months of treatment, positive dynamics were noted in the form of complete relief of pain and normalization of biochemical parameters. Observation of the patient over the next six months showed no relapses of biliary-dependent pancreatitis.
According to N.A. Agafonova et al. [14], the Russian drug mebeverine Sparex® not only relieves pain, but also improves the rheological properties of bile in cholelithiasis.
The safety and tolerability of mebeverine were assessed in studies that included over 3500 patients [13]. All studies showed good tolerability of the drug without the development of side effects, including with increasing doses. Mebeverine does not cause hematological and biochemical changes, does not have typical anticholinergic effects, and therefore can be prescribed to patients with prostatic hypertrophy and glaucoma [13], which is important for elderly patients.
Thus, despite the papillosphincterotomy performed, the outflow of bile was impaired, which in turn provoked exacerbations of chronic pancreatitis. No data on the formation of strictures were obtained. In this regard, surgical intervention was inappropriate. The situation was resolved by using the drug UDCA (Exhol®) and a selective myotropic antispasmodic (Sparex®).
Diagnosis
Based on the observed history of the patient’s pathology, the results of examinations and medical practice, with the maximum guarantee, a diagnosis can be made - chronic pancreatitis at the acute stage (not an advanced type of pathology). There are no associated diseases, with the exception of mild gastritis.
You can learn more about chronic pancreatitis from the video:
https://www.youtube.com/watch?v=YkefLGAvbKg&t=1459s
Incidence rate
Although the actual incidence of chronic pancreatitis is unknown, estimates range from 0.04% to 5% of the general population. In developed countries, the development of this disease is associated with alcohol abuse in approximately 60-70% of cases. Chronic pancreatitis is most common in men, with a peak incidence occurring between 35 and 45 years of age. Idiopathic pancreatitis, accounting for 30% of all cases of chronic pancreatitis, occurs in two specific groups of patients: young individuals 15-30 years old and older individuals 50-70 years old. A rarer form of the disease, tropical pancreatitis, occurs in children in parts of Africa and Asia [2].
Prescribed treatment
Papaverine is a drug for normalizing the functioning of the pancreas.
In accordance with the patient's history of pancreatitis, he was prescribed the following treatment:
- the first 7 days - observation by a specialist, leave to go home, daily regimen: bed, diet: moderate fasting, medications: Diphenhydramine, Papaverine, Glucose, Novocaine (intravenously, intramuscularly) and Enap tablets (orally);
- 7-30 days after hospitalization - observation by a specialist, special diet, taking preventive medications prescribed by a specialist based on the results of observations;
- after 30 days – maintaining gastrointestinal health according to the recommendations of a specialist.
More precise dosages of drugs, their list and other elements of treatment are discussed in the appendices to the medical history.
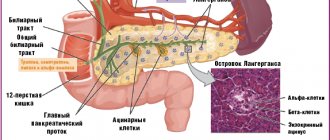
Anatomy and physiology
The pancreas is a retroperitoneally located organ, approximately 12-20 cm long and weighing 70-120 grams. The head of the pancreas is located in the horseshoe of the duodenum (duodenum), then the gland is located in an oblique direction, crosses the spinal column and its tail ends at the gate of the spleen. The pancreas has a very rich blood supply, blood flows through the branches of the celiac trunk, superior mesenteric and splenic arteries. Venous drainage from the pancreas goes into the portal vein system. Both sympathetic and parasympathetic efferent nerve fibers from the vagus nerve and visceral nerves innervate the pancreas through the hepatic and celiac plexuses.
The functional unit of the pancreas is the acinus. The acini consists of acinar and ductal cells. Acinar cells are equipped with a rich and highly specialized intracellular matrix for the synthesis, storage and secretion of a large number of proteins, mainly in the form of inactive digestive enzymes. Ductal cells primarily secrete water and electrolytes.
There are three phases of pancreatic secretion: central, gastric and intestinal. The central phase is stimulated by the thought of, sight, taste or smell of food through the cholinergic innervation of the vagus nerve. The gastric phase occurs in response to gastric dilation and is also produced through the vagal cholinergic reflex. The main period of pancreatic secretion after eating occurs in the intestinal phase. This phase is responsible for 70-80% of pancreatic secretion and is regulated by the release of secretin or cholecystokinin (CC). Secretin, which enters the circulation from the duodenum, is responsible for the secretion of bicarbonate and water by the ductal cells of the pancreas. CC is mainly responsible for the secretion of enzymes (proteases) in acinar cells [3].