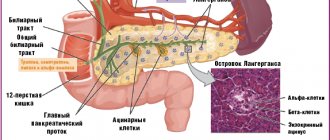
Pancreatitis is an acute or chronic inflammation of the enzymatic pancreas and peripancreatic tissues, manifested by low back pain and increased activity of pancreatic enzymes. About two-thirds of cases of acute pancreatitis (AP) are caused by long-term excessive alcohol consumption or gallstones.
The etiology of AP, recurrent and chronic pancreatitis (CP) is very diverse. Various combinations of genetic, epigenetic, metabolic and environmental factors can trigger the inflammatory process and lead to its effects in several systems that regulate and maintain pancreatic function.
When treating the patient and taking preventive measures, it is important to determine the etiological factors in order to prevent relapse of the disease. This article takes a closer look at the rarer causes of acute and chronic pancreatitis.
What is chronic pancreatitis?
Chronic pancreatitis is an inflammatory disease that damages the tissue of the pancreas. The diagnosis is quite common, it is given to people of any age and gender, but most often men from 40 to 55 years old suffer from pancreatitis.
Pancreatitis has two forms:
- Acute - occurs against the background of alcohol abuse, cholelithiasis, as a result of a viral disease, poisoning, or surgery on the gastrointestinal tract.
- Chronic pancreatitis is a long-term inflammatory disease of the pancreas. Acute pancreatitis can also become chronic.
Etiology
The etiological factors of pancreatitis are very diverse - metabolic, mechanical, infectious, vascular. Often the disease occurs as a result of the interaction of several factors. The etiology of AP is determined only in 75% of patients.
Chronic pancreatitis is classified according to etiology and risk factors according to the TIGAR-O classification (Table 1).
Table 1. Etiological classification of chronic pancreatitis (TIGAR-O)
| Toxic-metabolic |
| Alcohol; Tobacco, smoking; Hypercalcemia (hyperparathyroidism); Hyperlipidemia; Chronic renal failure; Drugs and toxins. |
| Idiopathic |
| Early start; Late start; Tropical calcific pancreatitis, fibrocalcular pancreatic diabetes. |
| Genetic |
Autosomal dominant
|
| Autoimmune |
| Autoimmune pancreatitis type 1 (IgG4 positive); Autoimmune pancreatitis type 2 (negative IgG4). |
| Recurrent (reversible) and acute |
| Ponecrotic (acute); Reversible sharp:
Ischemic (postoperative, hypotensive); Infectious (viral); Chronic alcoholism; Poradiative; Diabetes. |
| Obstructive |
Benign pancreatic duct stricture:
Malignant stricture; Periampullary carcinoma; Pancreatic adenocarcinoma. |
Table 2. Rare causes of pancreatitis
| Nosology | Characteristics | Diagnostics |
| Metabolic pancreatitis | Hypertriglyceridemia and hypercalcemia | OP or HP |
| Drug-induced pancreatitis | Azathioprine, 6-mercaptopurine, sulfonamides, estrogens, tetracycline, valproic acid, antiretroviral drugs | OP or HP |
| Autoimmune pancreatitis | Focal or diffuse enlargement of the pancreas, hypotensive pancreatic shunt, expansion of the papillary part due to lymphoplasmocytes p.
| HP |
| Hereditary pancreatitis | Usually occurs at a young age, gene mutations are detected | Acute recurrent pancreatitis |
| Pancreatitis after the procedure | Endoscopic retrograde cholangiopancreatography was recently performed | Most often OP |
| Pancreatitis with sedimentation of bile (sediment) | Bile deposits and small stones (microlithiasis) | Most often OP |
| Pancreatitis Paraduodeninio groove ( groove ) | Fibrous formations between the head of the pancreas and the thickened wall of the duodenum, leading to duodenal stenosis, cystic changes in the pancreaticoduodenal groove or duodenal wall, pancreatic and bile duct stenosis | Exclusively HP |
| Duodenal diverticulum | Periampullary diverticulum, wind deformation | OP>HP |
| Traumatic pancreatitis | Direct trauma to the pancreas, intrapancreatic hematoma, rupture of the pancreas with fluid around it | OP or HP |
| Infectious pancreatitis | Various infectious factors: viruses, bacteria, fungi. | Most often in OP |
| Ischemic pancreatitis | Pancreatitis due to circulatory disorders, arterial hypotension, cardiogenic shock | OP or HP |
Why is chronic pancreatitis dangerous?
When the pancreas is damaged, the production of digestive enzymes is reduced and the functioning of the entire digestive system is disrupted. Due to inflammation, the cells degenerate and are replaced by dense fibrous (scar) tissue.
When treating a disease, correct identification of the cause is of great importance. In no case should chronic pancreatitis be treated at home; you should consult a doctor. Self-prescription of drugs and diet can lead to irreversible consequences.
On a note:
Dangerous complications of chronic pancreatitis are malabsorption syndrome, pseudocyst, diabetes mellitus, portal or splenic vein thrombosis, obstruction of the common bile duct, and tumors.
Chronic pancreatitis can occur with long-term remission. If the causes of occurrence are excluded and adequate therapy is carried out, the course of the disease slows down, which significantly improves the condition.
Calcific (hypercalcemic) pancreatitis
Calcific pancreatitis is very rare. The most common causes of hypercalcemia (about 90%) are hyperparathyroidism and malignancy. According to studies, hyperparathyroidism causes about 0.4% of cases of AP.
It is believed that calcium accumulated in the pancreatic duct activates trypsinogen in the pancreatic parenchyma. The low incidence of pancreatitis among patients with chronic hypercalcemia suggests that other factors (sudden increases in serum calcium levels) also influence OP.
Patients with hyperparathyroidism and associated hypercalcemia develop pancreatitis 10 to 20 times more often than the general population. The most common causes of hyperparathyroidism are:
- parathyroid adenoma (80%);
- hyperplasia of all 4 parathyroid glands (15–20%);
- thyroid cancer (2%).
Parathyroid adenoma
The most important principles of treatment are the correction of hypercalcemia and elimination of the underlying cause. In patients with asymptomatic mild hypercalcemia (calcium concentration 3.5 mmol/L), initial treatment is 200 to 300 ml/hour of isotonic sodium chloride solution based on a urine output of 100 to 150 ml per hour.
For immediate short-term treatment, patients who develop symptoms (lethargy, stupor) are given calcitonin, and for long-term treatment, an intravenous bisphosphonate is added. If bisphosphonates are contraindicated, zoledronic acid or denosumab can be used.
Diet in the treatment of chronic pancreatitis
The doctor chooses how to treat chronic pancreatitis in the stage of exacerbation or remission. The goal of therapy is pain relief, correction of impaired organ functions, and relief of concomitant disorders.
The key to successful therapy is the elimination of factors that led to the development or exacerbation of the disease, as well as strict adherence to nutrition and diet.
After treatment in a hospital, at home you must carefully follow the doctor’s recommendations regarding nutrition and lifestyle.
Carbohydrates
With pancreatitis, insufficient secretion of insulin and disturbances in carbohydrate metabolism are observed, so careful monitoring of carbohydrate intake is required.
It is necessary to limit the consumption of refined carbohydrates:
- Sahara
- honey
- sweets
- other sweets
Plant foods allowed:
- vegetable soups
- dishes from cereals and vegetables
It is advisable to limit vegetables containing coarse fiber:
- white cabbage
- legumes
- turnips
Give preference:
- zucchini
- pumpkin
- broccoli
- cauliflower
Fruits and berries are allowed, but not more than 200 g per day.
Fats
Control of fat intake is required due to decreased production of digestive enzymes. This primarily applies to animal fats.
Limit:
- fat meat
- fatty poultry (duck, goose)
- some varieties of fish salmon
- halibut
- sturgeon
- acne
It is undesirable to use:
- fatty dairy products
- aged cheeses
Squirrels
Particular attention is paid to products containing a sufficient amount of easily digestible proteins with complete amino acid composition.
Recommended to use:
- Eggs
- Low-fat dairy products dietary cottage cheese
- kefir
- yogurt
- haddock
- rabbit
SBCS "Diso®" "Nutrimune" helps supplement the diet with easily digestible protein.
Conservative treatment
The goal of conservative treatment of patients with CP is to relieve symptoms and prevent the development of complications. There are 6 main objectives that must be achieved [2]:
1. Stop drinking alcohol and quit smoking.
2. Determining the cause of abdominal pain and trying to reduce its intensity.
3. Treatment of insufficiency of exocrine pancreatic function.
4. Detection and treatment of endocrine insufficiency in the early stages before complications develop.
5. Nutritional support.
6. Screening for pancreatic adenocarcinoma, especially in hereditary pancreatitis.
Behavior change (lifestyle modification) and nutritional therapy
Complete abstinence from alcohol consumption is recommended to reduce the incidence of serious complications and mortality. In addition, in conditions of abstinence, in some cases, a decrease in the severity of symptoms and relief of pain was noted, while continued alcohol consumption contributes to the progression of the disease [1, 2, 15]. Exocrine pancreatic insufficiency, as a rule, does not progress with abstinence from alcohol consumption [15]. Individuals who do not drink alcohol have a better response to pain management therapy [15–22]. However, stopping drinking alcohol does not always stop the progression of the disease. To stop drinking alcohol, it is necessary to involve narcologists and psychiatrists specializing in alcohol dependence, followed by the supervision of a psychologist [2].
In general, it is very difficult to identify the role of smoking in alcohol abuse as an etiological factor and a factor influencing the course of CP, since smoking often accompanies alcohol abuse [8, 23–30]. In addition, abstinence from alcohol consumption is often not associated with smoking cessation [1]. Retrospective data indicate the beneficial effects of smoking cessation in reducing/preventing pain and complications in CP [31, 32]. In any case, patients with CP are recommended to quit smoking as a significant and independent factor in the development of CP [16, 32].
Protein-energy malnutrition is common among patients with CP, and is multifactorial in nature due to abdominal pain syndrome, malabsorption, diabetes mellitus (DM), impaired intestinal motility and chronic alcoholism [33]. From the standpoint of science, based on evidence, there is no specific “diet for CP”, and we only have empirical experience in using the familiar “gentle nutrition”, or “table No. 5p”, which is familiar to everyone. In general, these recommendations boil down to eating low-fat, high-protein, and high-carbohydrate meals in smaller portions, especially for patients with steatorrhea. The degree of fat restriction is thought to depend on the severity of malabsorption. Patients usually tolerate a pure fat intake of <40–60 g per day. Specific recommendations include a daily energy diet of 2500–3000 calories, protein intake of 1.0–1.5 g/kg/day, and a fat intake of <30–40% of daily calories [2, 33]. However, there is no official data based on the results of randomized trials indicating the need to reduce fat intake in patients with pancreatogenic steatorrhea [1]. It is extremely important to remember that switching to a low-fat diet is challenging and can impair nutritional balance and lead to decreased vitamin levels. Since there have been no specific studies examining macronutrient intake patterns that can prevent the development of isolated complications of CP, it can be assumed that complex carbohydrates and dietary fiber may be useful in slowing the rate of development of diabetes.
Patients with CP may experience impaired absorption of fat-soluble vitamins (A, D, E and K) [1], which is accompanied by a decrease in their concentration in the blood serum [34]. However, clinical manifestations of hypovitaminosis rarely appear [2, 35–37]. Therefore, persons with uncontrolled exocrine pancreatic insufficiency and/or a long history of CP (more than 5 years) require biochemical screening of fat-soluble vitamins, and if they are reduced, parenteral administration of fat-soluble vitamins [1].
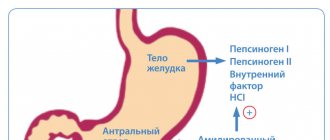
Patients with CP may develop deficiency of vitamin B12, which is absorbed in the terminal ileum and forms a complex with intrinsic Castle factor. When vitamin B12 enters the stomach, it binds to haptocorrin (R-protein, or Castle factor). Haptocorrin is broken down in the small intestine by pancreatic enzymes, thereby releasing B12. In patients with pancreatic dysfunction, vitamin B12 may remain bound to haptocorrines and not be absorbed in the terminal ileum. Patients who continue to abuse alcohol are also at risk of developing thiamine (vitamin B1), riboflavin (vitamin B2) and pyridoxine (vitamin B6) deficiencies. If insufficient levels of vitamins in the blood serum are detected, vitamin replacement therapy should be carried out.
Osteoporosis is an established complication of CP; It is recommended to perform a one-time assessment of bone mineral density (using X-ray densitometry) [37].
Treatment of abdominal pain syndrome
Pain is the most common and most significant symptom in CP. The mechanism of pain is not precisely established and is likely multifactorial; additional examination is often required to establish it [4].
Factors that determine the development of pain in CP include [2]:
• formation of false cysts;
• stenosis of the duodenum (DU);
• strictures of the biliary tract;
• pancreatic cancer;
• other concomitant diseases (for example, peptic ulcer).
If the above factors are excluded, consistent conservative treatment is carried out [2]. Despite the fact that pain in CP may subside over time, especially in alcohol-related pathology, its duration cannot be predicted [38]. Initial therapy consists of periodic or course use of simple non-narcotic analgesics (paracetamol or non-steroidal anti-inflammatory drugs - NSAIDs) along with a low-fat diet. The drugs should be taken 30 minutes before meals to minimize postprandial pain [1, 2].
In Russia, the recommendations of a number of foreign associations [1–5] on trial replacement therapy with high doses of pancreatic enzymes for 6 weeks (in the form of tablets without a protective coating) [4, 38–40] are not available for implementation due to the lack of such drugs on the pharmacological market in Russia . However, there is insufficient evidence of the effectiveness of such therapy in controlled studies [1, 2].
A possible mechanism for pain relief with enzyme replacement therapy (ERT) is to reduce the stimulation of the pancreas by cholecystokinin released in response to food intake. When exogenous pancreatic enzymes enter, releasing factors undergo proteolysis, which leads to a decrease in the release of cholecystokinin in response to food intake, a decrease in the secretory tension of the pancreas and, accordingly, pain. Clinical trials examining the validity of this hypothesis have yielded conflicting results [39, 40]. Enteric-coated tablet pancreatin, registered in Russia, has no evidence of effectiveness at all, since it has not been tested in any placebo-controlled study.
In studies using non-enteric-coated tablets, a decrease in pain was observed compared with placebo. It should be remembered that the effects of drugs based on pancreatic enzymes without a protective coating were enhanced by therapy that suppresses acid production (H2 blockers or proton pump inhibitors), which prevents the inactivation of enzymes under the influence of acid in the stomach and increases the level of proteases reaching the duodenum [ 38, 41]. When combining microtablets or minimicrospheres of pancreatin, coated with an enteric coating, with antisecretory drugs, early opening of the membranes and activation in the initial parts of the duodenum are possible, where the principle of negative feedback can be implemented. There are no experimental studies confirming this hypothesis, but there are individual randomized [42] and non-randomized [43] studies that indirectly confirm this fact, which has long been reflected in the practice of Russian gastroenterologists and surgeons.
It is assumed that ERT for CP with pain is most effective in the absence of duct dilatation or with minimal changes in the pancreatic parenchyma [44]. Octreotide is also effective in suppressing pancreatic secretion, but currently it is not recommended for use in the treatment of chronic pain [38] due to the ambiguity of the available scientific data and the impossibility of long-term use (high cost, adverse events) [2].
Patients with persistent pain may require the use of narcotic analgesics [1,2] due to the lack of effectiveness of NSAIDs [23, 29, 45–48]. It is believed that tramadol should be initially preferred over morphine due to its less pronounced effect on the functions of the gastrointestinal tract [48]. Narcotic analgesics in different dosage forms have similar effectiveness [46]. You should start with drugs with the least activity, followed by a transition, if necessary, to potent drugs. Initially, it is recommended to prescribe narcotic analgesics only as needed (as required for severe pain). In general, regular use of opioids is only required when endoscopic or surgical treatments fail and symptoms persist [2].
Tricyclic antidepressants reduce the manifestations of concomitant depression, can reduce the severity of pain and potentiate the effect of analgesics. These drugs can change the sensitivity of the central nervous system and visceral nerves, the role of which is assumed in the development of pain in CP [2, 44].
Chronic intake of antioxidants may be effective in preventing attacks of pain in CP [1]. Only one randomized controlled trial has demonstrated the effectiveness of oral antioxidants (selenium, beta-carotene, ascorbic acid, tocopherol, and methionine) as adjunctive therapy for the prevention of attacks of pain. Overall, antioxidant supplementation resulted in a significant reduction in the number of pain days per month, a reduction in the need for oral analgesics, and a reduction in hospitalizations. By the 3rd month, a statistically significant beneficial effect of antioxidants on pain relief was already noted [49]. The results of this study require confirmation [1, 2] to adapt such tactics to routine clinical practice.
Treatment of pain in CP should be carried out jointly with qualified surgeons and endoscopists who can offer minimally invasive techniques for relieving/reducing pancreatic pain (blockades, stenting, etc.) and/or surgical treatment.
Treatment of insufficiency of exocrine function of the pancreas
Clinically significant impairment of the absorption of fats and proteins occurs only when the functional activity of the pancreas decreases by more than 90% [38]. Steatorrhea usually precedes protein deficiency [38] and occurs in the late stages of CP (approximately 50% of patients, on average 10–12 years after the onset of the disease) [50]. It may be more common than previously thought [51]. The main clinical consequences of CP are wasting and steatorrhea caused by impaired fat digestion [52].
Pancreatic enzyme replacement therapy improves fat absorption in patients with CP and exocrine pancreatic insufficiency [53] and can normalize nutritional status, such as the level of fat-soluble vitamins, prealbumin and ferritin, including in patients without overt steatorrhea [50, 52] , prevent the development of osteoporosis caused by vitamin D malabsorption [36, 37].
Indications for PRT [2]:
• severe steatorrhea;
• weight loss;
• diarrhea;
• long-term course of CP (more than 5 years of history) [1, 51].
Adequate and timely treatment helps to avoid the development of serious complications and reduce mortality due to malnutrition.
For patients with clinically significant steatorrhea (unformed, greasy, foul-smelling stool in large quantities), it is possible to prescribe pancreatic enzymes only on the basis of clinical data [1]. In CP with signs of nutritional deficiency (weight loss, muscle wasting, osteoporosis, signs of hypovitaminosis), ERT can be indicated even without diagnosing steatorrhea using the method of quantitative assessment of excreted fat and normal stool appearance [1, 51].
A standard coprological study with the detection of neutral fat is characterized by low sensitivity, therefore, when using it to verify steatorrhea and evaluate its effectiveness, it is necessary to carry out the test three times and take into account the patient’s diet and stool frequency. A 72-hour stool collection to determine the fat absorption coefficient (neutral fat quantification), although the gold standard for diagnosing steatorrhea, is used only in clinical trials [50].
Minimicrospheres containing the pancreatin enzyme are coated with an enteric coating (Creon). They are much more effective than any tablet drugs in the treatment of steatorrhea, since lipase is not inactivated in the stomach by acid. Thus, improved pharmacokinetics results in a more likely contact of enzymes with chyme and a larger contact area [54]. Minimicrospheres with a diameter of 1.0 to 1.2 mm are evacuated simultaneously with food. Their effectiveness is 25% higher compared to microtablets measuring 1.8–2.0 mm [52, 55].
Thus, the prediction of the effectiveness of TRT will definitely be influenced by the choice of drug. It is important to remember that in different pancreatin preparations the content of lipase, protease and amylase is not the same. The patient should receive at least 25–40 thousand units of lipase for the main meal and 10–25 thousand units of lipase for an intermediate meal [1, 2, 56], which should be at least 100 thousand units per day.
Treatment usually results in clinically significant weight gain and symptomatic relief.
Serological (retinol binding protein, transthyretin) and general clinical (absolute lymphocyte count in the absence of other causes of lymphocytopenia) markers can be used to monitor nutritional status. The use of an average of 40 thousand units of lipase per meal for one year leads to normalization of fat absorption, a significant increase in body weight, normalization of the level of retinol-binding protein and prealbumin in the majority of patients with CP [50]. For patients with no effect of treatment, laboratory methods for assessing fat absorption can be used - dynamic determination of neutral fat in the stool and C13 breath tests [35, 50]. Despite clinical improvement, malabsorption may persist in some patients, which requires the use of higher doses of Creon (up to 60 thousand lipase units per meal or more) [50].
Patients with persistent symptoms despite taking high doses of enteric-coated enzyme preparations should be prescribed therapy that suppresses acid production [54], due to a sharp decrease in bicarbonate secretion in the pancreas with insufficient neutralization of chyme acidity in the duodenum [52, 57]. The preferred drugs are proton pump inhibitors in standard doses [1, 2], which are prescribed only for persistent steatorrhea. With persistent steatorrhea, it is necessary to exclude other causes of diarrhea, in particular those associated with bacterial overgrowth in the small intestine, which often occurs in CP [58], protozoal infections, and celiac disease.
Adequate replacement therapy with Creon significantly improves the quality of life of patients with newly diagnosed and never treated CP and patients who received FPP in insufficient doses. A significant relationship has been established between improvements in quality of life indicators and body weight or a decrease in the excretion of fat in feces [59].
Long-term treatment with pancreatic enzymes in daily doses of up to 200 thousand units of lipase is absolutely safe, as evidenced by the results of numerous studies of children with cystic fibrosis, adult patients with CP and those who underwent extensive resections of the pancreas [60]. At the same time, a common misconception among patients and doctors is the so-called. harm of long-term treatment with pancreatic enzymes. There are no scientific explanations for this assumption. It is based only on the opinion expressed by someone unknown about “addiction of the pancreas,” “atrophy of the pancreas,” and the fact that “your pancreas will stop working altogether.” On the one hand, studies conducted in which extremely high pancreatin levels were used (360 thousand units of lipase per day) did not show any effect on pancreatic secretion [61]. On the other hand, leaving a CP patient with pancreatic insufficiency without vital replacement therapy is criminal and tantamount to canceling replacement therapy with levothyroxine, antihypertensive and hypoglycemic drugs for hypothyroidism, arterial hypertension and diabetes, respectively.
Treatment of endocrine insufficiency
70% of patients with CP develop impaired glucose tolerance over time. The likelihood of endocrine insufficiency begins to gradually increase 10 years after the onset of the disease [38]. Pancreatogenic diabetes differs from diabetes types 1 and 2 by a higher risk of hypoglycemia and a reduced incidence of ketoacidosis due to worsening glucagon secretion [62] and concomitant liver dysfunction in individuals with alcohol-related CP [2]. Complications such as macro-/microangiopathy, nephropathy, neuropathy and retinopathy are as common as in type 1 diabetes [62]. They largely depend on the duration of the disease, rarely affecting life expectancy, since the determining factors of prognosis for patients with CP are the outcomes of alcohol and nicotine addiction (cardiovascular diseases, malignant tumors).
Diagnosis of endocrine insufficiency should be timely and thorough, based on the results of regular determination of the concentration of glycosylated hemoglobin (HbA1c), fasting blood glucose level or glucose loading test. The optimal form of screening remains controversial [2]. An international expert committee with members nominated by the American Diabetes Association, the European Association for the Study of Diabetes Mellitus, and the International Diabetes Federation recommended using HbA1c (at a level ≥ 6.5) rather than blood glucose concentration to diagnose diabetes [63]. The advantages of HbA1c include the lack of a strict fasting determination and the lower variability of blood glucose results [2].
The diet for pancreatogenic diabetes corresponds to that for type 1 diabetes, with the exception of the need to correct malabsorption, deficiency of vitamins and microelements, and prevent hypoglycemia using fractional nutrition [1]. Most patients with secondary diabetes and ineffective diet require insulin. With the development of diabetes, oral hypoglycemic agents do not play a significant role in the outcome of severe fibrosis of the pancreatic parenchyma [64].
When prescribing insulin therapy, the target glucose level should correspond to that for type 1 diabetes, with the exception of a slight increase during episodes of severe hypoglycemia. To prevent severe hypoglycemia, patients are advised to stop drinking alcohol, increase physical activity, and eat smaller meals. Commitment to the TFT is of great importance. Patients on insulin therapy should avoid hypoglycemia.
What happens to the pancreas during this disease?
When the first acute attack of pancreatitis occurs, the gland becomes inflamed, digests its own tissues and can no longer fully perform its functions, which are to secrete hormones and aid in digestion. During these processes, the affected tissues are replaced by other structures, and the full functioning of the organ becomes impossible.
Early consultation with a doctor during an attack is mandatory and largely determines the future prognosis of the disease. Only in this way can further spread of organ tissue damage be prevented. If the disease has not affected most of the tissues, then it is possible to talk about a complete cure of the disease.
Is it possible or not?
To understand whether pancreatitis can be cured forever, we need to talk a little about the mechanism of development of this disease. So, pancreatitis is characterized by inflammation of the cells of the pancreas, due to which their integrity is disrupted and they cease to function as before.
In this case, the inflammatory process covers the pancreatic ducts, through which pancreatic juice is released into the duodenum. As a result of this, spasms periodically occur in them, due to which the lumen of the ducts narrows significantly and pancreatic juice, containing digestive enzymes, begins to accumulate inside the gland, triggering self-digestion processes in it. The result of this is even greater damage to the cells of the organ and disruption of its functionality.
During inflammation, pancreatic cells die and are no longer restored.
And speaking about whether it is possible to cure pancreatitis completely, it should be noted that all cells of the human body have the property of self-healing. However, with the development of this disease, the destruction of pancreatic cells occurs much faster than their restoration. At the same time, metabolism in the gland is disrupted and regeneration processes slow down significantly. As a result of this, areas appear in the pancreas that completely cease to function, and, unfortunately, it is impossible to restore them.
There is no clear answer to the question of whether the pancreas can be cured. However, this does not mean that when this disease occurs, a person should forget about his usual life once and for all. If you make some adjustments to it, then you can lead a normal life with pancreatitis. You will now find out how to do this.
How does the development of pancreatitis manifest?
Pancreatitis causes severe pain in the left hypochondrium.
Most patients may not notice that inflammatory processes in the form of pancreatitis are present in the body.
Only sometimes there may be problems with defecation or minor pain in the left hypochondrium.
However, it is very difficult to miss the first signs of this disease. At the first manifestations, the following usually happens:
- An aching or dull pain appears on the left side. Sometimes it radiates to the back or under the shoulder blade;
- Diarrhea appears, while the feces contain undigested food and also have a greasy sheen;
- There is a bitterness in the mouth, nausea and lack of appetite may be tormented;
- There is a white coating on the tongue;
- A person loses weight sharply.
These manifestations may appear one at a time or all together. When the pain is too strong, it means there is a dyspeptic disorder. Some patients may not feel severe pain, but only occasionally suffer from nausea, problems with bowel movements, and lack of appetite.
Sometimes this condition can last for about a month. When the patient is in a dyspeptic state, he begins to vomit, loses his appetite, and suddenly loses weight - up to 8 kg in two weeks. If, on the contrary, you constantly want to eat, your hunger is not satisfied, then it is worth checking for diabetes.