Pancreatic juice and its enzymes
The pancreas (P) produces pancreatic juice, which, unlike gastric juice, has a pronounced alkaline reaction. Pancreatic juice contains amylase, lipase and protease, and other enzyme compounds. These substances are involved in the breakdown of proteins, fats and carbohydrates and help food to be absorbed. Enzymes are produced by the gland in the form of proenzymes, and their activation, that is, transformation into active enzymes, occurs in the intestinal lumen. This is necessary to avoid damage to pancreatic cells.
During normal functioning of the gland, pancreatic juice begins to be produced some time after eating. If a person is hungry, the pancreas does not secrete secretions. During meals, gastric digestion is activated and gastric juice is released. This signals the pancreas to begin its work. Its liquid enters the duodenum, where proenzymes are activated and the digestion process begins. Pancreatic juice production naturally decreases 9-10 hours after eating. At the next meal, this process is activated again.
The secretion of pancreatic juice is promoted by the consumption of acidic foods and drinks, and small portions of alcohol. The mucous membrane of the duodenum produces special hormones that are also involved in the regulation of the secretion of pancreatic juice. A decrease or increase in its production can be caused by the entry of certain drugs into the body or changes in the functioning of the nervous system.
With diseases of the pancreas or its partial removal due to pathology, the patient develops a deficiency of enzymes and hormones produced by the organ. In this case, replacement therapy, which includes insulin preparations and enzyme agents, helps normalize the condition.
Tablets "Creon": indications for use
The drug is used as part of a course of replacement therapy. The main indication is dysfunction of the pancreas due to various pathologies:
- cystic fibrosis;
- duct obstruction;
- chronic pancreatitis;
- pancreas cancer;
- the occurrence of neoplasms;
- cirrhosis of the liver;
- pancreatectomy;
- degenerative changes in old age;
- cholestatic hepatitis;
- complications after partial removal (resection) of the stomach;
- gastrostasis;
- duodenostasis;
- biliary obstruction;
- lesions of the terminal part of the small intestine;
- a sharp increase in the colony of bacteria in the small intestine.
Action
The pathological state of enzyme deficiency in diseases of the pancreas and gastrointestinal tract negatively affects digestive function, interferes with the normal breakdown of proteins, fats and carbohydrates, and the absorption of nutrients by the body. Outwardly, this manifests itself as signs of digestive dysfunction. Among them:
- pain;
- nausea, urge to vomit;
- increased gas formation;
- defecation disorder.
When ingested, Creon 10000 capsules quickly dissolve. Minimicrospheres are released and, together with food, enter the intestines, where they begin their therapeutic activity. In the small intestine, the acid-resistant membrane dissolves. This releases pancreatic enzymes, which are necessary to break down nutrients from food. They are then absorbed in the intestine or broken down by intestinal enzymes.
In terms of its structure, the active substance of the drug "Creon 10000" is of a protein nature. To exhibit therapeutic activity, it does not require absorption in the intestine. The drug works when it passes through the gastrointestinal tract. In the body, pancreatin, like other proteins, is broken down into amino acids and peptides.
Creon 10000 20 pcs. enteric capsules
pharmachologic effect
Digestive enzyme agent.
Composition and release form Creon 10000 20 pcs. enteric capsules
Capsules - 1 capsule:
- Active substance: pancreatin - 150 mg (which corresponds to 10,000 IU of Eur.F. lipase, 8,000 IU of Eur.F. amylase, 600 IU of Eur.F. protease.);
- Excipients: macrogol 4000 - 37.50 mg, hypromellose phthalate - 56.34 mg, dimethicone 1000 - 1.35 mg, cetyl alcohol - 1.18 mg, triethyl citrate - 3.13 mg;
- Hard gelatin capsule: gelatin - 60.44 mg, red iron oxide dye (E 172) - 0.23 mg, yellow iron oxide dye (E 172) - 0.05 mg, black iron oxide dye (E 172) - 0, 09 mg, titanium dioxide (E 171) - 0.07 mg, sodium lauryl sulfate - 0.12 mg.
20, 50 or 100 capsules in a white high-density polyethylene bottle with a polypropylene screw cap and tamper evident. A label is placed on the bottle. 1 bottle along with instructions for use in a cardboard box.
Description of the dosage form
Hard gelatin capsules No. 2, consisting of a brown opaque cap and a transparent colorless body.
The contents of the capsules are minimicrospheres of light brown color.
Directions for use and doses
Creon is taken orally. The dose of the drug depends on the age and degree of pancreatic insufficiency and is calculated in terms of lipase enzyme.
The average dose for adults is 150,000 units of lipase/day. In case of complete insufficiency of pancreatic function - 400,000 units/day, which corresponds to the daily requirement of an adult for lipase. The maximum daily dose is 15,000-20,000 units/kg of weight.
Children under 1.5 years of age are prescribed 50,000 units/day; over 1.5 years - 100,000 units/day. Capsules are taken with meals, swallowed whole with plenty of non-alkaline liquid (water, fruit juices).
Pharmacodynamics
An enzyme preparation that improves digestion processes. Pancreatic enzymes included in the drug facilitate the breakdown of proteins, fats, and carbohydrates, which leads to their complete absorption in the small intestine. Capsules containing enteric-coated mini-microspheres dissolve quickly in the stomach, releasing hundreds of mini-microspheres. The purpose of the multi-unit dose principle is to mix the mini-microspheres with the intestinal contents, and ultimately to better distribute the enzymes after their release within the intestinal contents.
Pharmacokinetics
When the mini-microspheres reach the small intestine, the enteric coating is destroyed, releasing enzymes with lipolytic, amylolytic and proteolytic activity, which ensure the breakdown of fats, starches and proteins.
Indications for use Creon 10000 20 pcs. enteric capsules
Creon is an enzyme preparation that improves digestion processes. Creon is used as replacement therapy for insufficiency of exocrine pancreatic function, for symptomatic treatment of digestive disorders in the following cases: conditions after cholecystectomy, partial resection of the stomach, total gastrectomy, duodeno- and gastrostasis, biliary obstruction, cholestatic hepatitis, cirrhosis of the liver, pathology of the terminal part of the small intestines, bacterial overgrowth in the small intestine.
Contraindications
Creon should not be taken in the early stages of acute pancreatitis, as well as in case of hypersensitivity to porcine pancreatin or to any other component of the drug.
Application Creon 10000 20 pcs. enteric capsules during pregnancy and breastfeeding
The use of Creon is possible under the supervision of a physician.
special instructions
In patients with cystic fibrosis who received high doses of pancreatin preparations, strictures of the ileum, cecum and colon (fibrosing colonopathy) have been described. As a precaution, if unusual symptoms or changes in the abdominal cavity occur, medical examination is necessary to rule out fibrosing colonopathy, especially in patients taking the drug at a dose of more than 10,000 lipase units/kg per day.
Impact on the ability to drive vehicles and operate machinery
The use of the drug Krson® 10000 does not affect or has an insignificant effect on the ability to drive a car and operate machinery.
Overdose
Symptoms: hyperuricuria, hyperuricemia. Treatment: drug withdrawal, symptomatic therapy.
Side effects Creon 10000 20 pcs. enteric capsules
When using Creon, adverse reactions may occur, such as diarrhea, nausea, and allergic reactions.
Drug interactions
There are no reports of interaction with other drugs.
Indications for taking Creon 10000 in adults
The pancreas has hormonal and exocrine functions. The hormonal function is to produce insulin, which is necessary for the absorption of glucose by cells. Exocrine function is characterized by the production and release of pancreatic enzymes. They have enzymatic activity and participate in the breakdown of protein, fat and carbohydrate compounds.
In many diseases, there is a decrease in the secretion of pancreatin or its increased destruction in the intestinal lumen. This leads to symptoms of enzyme deficiency. Patients with the following diseases encounter this phenomenon:
- chronic pancreatitis and its complications;
- cystic fibrosis;
- disturbances in the functioning of the pancreas due to chronic cholecystitis, obstruction of the bile ducts;
- tumor diseases of the gland;
- surgical removal of part of an organ;
- gastrectomy.
Enzyme deficiency can occur in patients without pancreatic pathology in the event of improper nutrition. The secretion of enzymes worsens with overeating, an abundance of heavy fatty foods in the diet, and large gaps between meals.
Conservative treatment of chronic pancreatitis on an outpatient basis
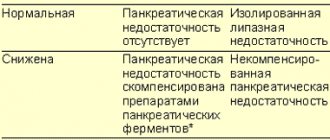
Chronic pancreatitis unites a heterogeneous group of diseases characterized by structural (morphological) and/or functional changes, despite the cessation of exposure to the etiological factor, with further progression of pancreatic damage and the development of exocrine and/or endocrine insufficiency. The morphological substrate of chronic pancreatitis is varying degrees of edema, inflammation and focal necrosis of acinar tissue, developing against the background of strictures along the pancreatic ducts, protein plugs and calcifications in small ducts; pseudocysts that occur during an attack of acute pancreatitis. All this leads to disruption of the flow of pancreatic juice, intraductal hypertension, progression of acinar tissue necrosis with subsequent atrophy of the acini; intralobular and perilobular fibrosis of the pancreas. With the loss of 90% of the functioning parenchyma, pancreatic insufficiency develops due to maldigestion syndrome.
In the later stages of the disease, with obvious exocrine pancreatic insufficiency or the development of diabetes mellitus, the diagnosis of chronic pancreatitis does not cause serious difficulties; certain obstacles arise in the early stages of the disease, when functional changes prevail, manifesting themselves most clearly during the action of the etiological factor. Diagnosis of chronic pancreatitis is based on the study of risk factors for its development, clarification of possible etiological factors, and assessment of the clinical picture of the disease. Often, the diagnosis of chronic pancreatitis is formed after long-term observation of a patient who has clinical signs suggesting the presence of chronic pancreatitis.
The etiological factors of chronic pancreatitis most often are 2 main causes - alcoholism and cholelithiasis, and 60-70% of all cases of chronic pancreatitis are caused by systematic, long-term (6-18 years) alcohol intake in a dose of more than 150 g per day before the development of obvious signs diseases (Table 1). The frequency of detection of chronic pancreatitis at autopsy in heavy drinkers reaches 45–50%. A high-protein diet and smoking exacerbate the damaging effects of alcohol. Alcohol-dependent pancreatitis develops predominantly in men and most often occurs between the ages of 35–45 years. A retrospective analysis of medical records and subsequent prospective observation of 372 patients made it possible to assess the course of chronic pancreatitis in idiopathic and alcoholic pancreatitis depending on the doses of alcohol consumed (less than 50 g/day and more than 50 g/day) [1]. It has been shown that in the group of patients with alcoholic pancreatitis, abdominal pain prevails at the onset of the disease. Patients from this group more often developed complications of chronic pancreatitis: fistulas, pseudocysts, abscesses, obstructive jaundice. It has been noted that in patients with the onset of chronic pancreatitis over the age of 35 years, drinking alcohol even in small doses (less than 50 g per day) leads to the early development of the disease, characterized by more frequent and intense abdominal pain, calcification of the pancreas and the presence of complications. Drinking large amounts of alcohol (50 or more grams per day) accelerates the formation of calcific pancreatitis and increases the incidence of fatal outcome in chronic pancreatitis.
Chronic pancreatitis, which develops with cholelithiasis (GSD), choledocholithiasis, is more common in women aged 50–60 years. As a rule, such patients show signs of metabolic syndrome: obesity, hyperlipidemia, a tendency to arterial hypertension, ischemic heart disease, impaired carbohydrate tolerance, hyperuricemia and/or hyperuricosuria, etc. In some patients with chronic pancreatitis, it is not possible to clarify the etiology of the disease - such pancreatitis is classified as to the group of idiopathic pancreatitis.
Recent studies have shown that the development of idiopathic pancreatitis may be caused by cholesterol microcrystals, bilirubinate granules and calcium microspherolites [2]. Dysfunction of the sphincter of Oddi (structural or functional) can also lead to the development of idiopathic pancreatitis, including due to the passage of microliths. Normally, the sphincter of Oddi performs 3 main functions: regulates the flow of bile and pancreatic juice into the lumen of the duodenum; prevents reflux of duodenal contents into the bile ducts and pancreatic duct; promotes filling of the gallbladder with hepatic bile. With dysfunction of the sphincter of Oddi, resistance to bile flow through the sphincter increases, as a result of which biliary colic develops in the absence of changes in the biliary system during a diagnostic examination (including ultrasound of the bile ducts (Fukuda, Aloka, Philips)); postcholecystectomy abdominal pain and chronic recurrent pancreatitis. Manometry (DSP-US, MTM-1, MA-4) of the sphincter of Oddi determines an increase in basal sphincter pressure in 15–57% of patients with a similar form of pancreatitis. The presence of biliary-type sphincter of Oddi dysfunction may be indicated by typical biliary-type pain, an increase in the level of aspartate aminotransferase and/or serum alkaline phosphatase by more than 2 times; prolongation of contrast transit time during endoscopic retrograde cholangiopancreatography (ERCP) by more than 45 minutes and dilatation of the common bile duct by more than 12 mm. With dysfunction of the sphincter of Oddi of the pancreatic type, there is a more than 2-fold increase in the level of pancreatic enzymes during successive attacks of pain, as well as an expansion of the pancreatic duct of more than 5 mm3.
Depending on the morphological changes in the pancreas, the following forms of chronic pancreatitis are distinguished (1989): calcifying, obstructive, fibrous-indurative pancreatitis, as well as cysts and pseudocysts of the pancreas. The group of calcifying pancreatitis includes alcoholic pancreatitis, pancreatitis that develops under the influence of organic solvents, certain chemical compounds, drugs, as well as pancreatitis that begins as a result of hyperlipidemia, hypercalcemia with hyperparathyroidism, chronic viral infections (including chronic HCV and HBV infections), congenital changes in the pancreatic ducts (doubling of the pancreatic duct - pancreas divisum). Hereditary pancreatitis with an autosomal dominant type of inheritance with incomplete penetration also belongs to the group of calcific pancreatitis and develops in children 10–12 years old or at the age of 30–40 years. It is indistinguishable from the usual forms of pancreatitis, is accompanied by recurrent attacks of abdominal pain; after 8–10 years, diabetes mellitus develops in 20% of patients and severe steatorrhea in 15–20% of patients. The absence of other etiological factors and indications of cases of pancreatitis in the family justify the suspicion of a hereditary form of chronic pancreatitis.
Chronic obstructive pancreatitis develops with obstruction of the main pancreatic duct by a pancreatic tumor, inflammation of the duodenal papilla or its stenosis, duodenitis due to Crohn's disease, closed abdominal trauma and surgical operations in the pyloroduodenal zone, the presence of pancreatic pseudocysts, congenital anomalies (pancreas divisum). Gallstone disease and choledocholithiasis, dysfunction of the sphincter of Oddi of the biliary and pancreatic types are the main causes of the formation of chronic obstructive pancreatitis.
Clarification of the etiological factor in the development of chronic pancreatitis allows for more effective prevention and treatment, which explains the appearance of the following classification of chronic pancreatitis according to the etiological principle, taking into account the morphological variant:
- alcoholic (calcific) pancreatitis;
- idiopathic juvenile and senile;
- tropical;
- hereditary;
- chronic obstructive pancreatitis.
Clinical signs of chronic pancreatitis are most clearly presented during the period of exacerbation (Table 2).
| Clinical signs of chronic pancreatitis |
Often the development of the painful form of chronic pancreatitis is preceded by a painless, latent stage of varying duration, masked by epigastric discomfort, flatulence, unstable stool with a tendency to diarrhea with the presence of undigested fiber in the stool or steatorrhea. Repeated attacks of the painful form of chronic pancreatitis form pancreatic insufficiency with predominant damage to exocrine or endocrine functions with the development of type 2 diabetes mellitus.
Pain syndrome - the most constant sign of acute and chronic pancreatitis - is observed in 70–80% of cases and has typical symptoms: localization in the epigastrium, “girdling” character with irradiation to the back, provoked and quickly intensifying after eating; the pain is relieved by sitting and bending forward. Often accompanied by nausea, vomiting, and fever. In 3–6% of patients, pain attacks can last several days; in 70–90%, episodes of pain are interspersed with a pain-free period. In some patients, the equivalent of epigastric pain may be back pain, sometimes comparable to the intensity of abdominal pain. In the genesis of abdominal pain syndrome in chronic pancreatitis, the main attention is paid to intraductal hypertension due to the persistent secretion of pancreatic enzymes by the inflamed gland under conditions of obstruction of the main or small ducts. Other factors - inflammation of the intrapancreatic nerve trunks, peripancreatic inflammation involving the duodenum, retroperitoneal space, stenosis of the distal common bile duct - also play a role in the development of pain. In 15% of patients, a painless form of the disease is observed, which manifests itself in 1/3 of patients with steatorrhea, most often this occurs with chronic calcific pancreatitis of alcoholic etiology. Endocrine function is most sensitive to the inflammatory process in chronic pancreatitis and is manifested in 2/3 of patients by impaired glucose tolerance and diabetes mellitus. In most cases, both exocrine and endocrine functions are affected; signs of pancreatic insufficiency develop with the loss of 80–90% of the functioning pancreatic parenchyma. In some cases, a progressive decrease in exocrine function leads to a decrease and even complete disappearance of pain.
Data on the effect of abstinence on the course of alcoholic pancreatitis are contradictory: in some patients, giving up alcohol leads to a decrease in the severity and frequency of pain attacks, signs of exo- and endocrine insufficiency, while others experience increased pain after 12–24 hours of abstinence. The course of chronic pancreatitis can be unpredictable - progressive, despite strict abstinence, and quite stable, regardless of continued alcohol intake. In one observation, 45% of patients who abused alcohol did not have clinical symptoms of pancreatitis, but had signs of chronic pancreatitis at autopsy.
Nausea, vomiting, anorexia, and weight loss are common in chronic pancreatitis. One of the main reasons for weight loss is a decrease in the caloric intake of food intake due to increased abdominal pain, as well as the developing malabsorption syndrome due to maldigestion and uncompensated diabetes mellitus. During chronic pancreatitis, malabsorption syndrome with diarrhea and steatorrhea develops relatively late, usually against the background of less than 20% of functioning acinar tissue. In some patients, malabsorption syndrome may occur with formed stool, which is explained by good absorption of water by the unchanged mucosa of the small intestine and a small amount of water in the stool. Sometimes patients note greasy spots on the surface of the water in the toilet, “greasy”, shiny feces that are difficult to wash off from the walls of the toilet, which usually indicates pancreatic steatorrhea. The absorption of fat-soluble vitamins A, D, E, K suffers little; significant deficiency is rarely detected in pancreatic insufficiency.
Although impaired glucose tolerance is common and presents early in chronic pancreatitis, clinically apparent diabetes mellitus occurs relatively late. In most patients, the diagnosis of chronic pancreatitis is established long before the development of hyperglycemia, however, in some of them suffering from a painless form of pancreatitis, diabetes mellitus may be the first and only manifestation of the disease. A feature of the course of diabetes mellitus in chronic pancreatitis should be considered the rare development of ketoacidosis, diabetic nephropathy and good tolerance of hyperglycemia levels up to 200 mg/dl, however, with long-term diabetes, retinopathy and polyneuropathy occur with the same frequency for different types of diabetes.
Other clinical manifestations of chronic pancreatitis include jaundice due to compression of the common bile duct by the enlarged head of the pancreas, ascites or pleural effusion due to leakage of pancreatic secretions from destroyed ducts; pseudocysts. Atypical variants of chronic pancreatitis with the development of liponecrosis of the subcutaneous tissue or “chemical” polyarthritis of small joints of the hands are rare.
The mortality rate for chronic pancreatitis reaches 50% with a 20-25 year duration of the disease. 15–20% of patients die from complications associated with exacerbations of pancreatitis; other deaths are caused by trauma, malnutrition, infection, smoking, which are often observed in patients with chronic pancreatitis.
Complications of chronic pancreatitis include malabsorption syndrome, diabetes mellitus, pseudocysts, portal or splenic vein thrombosis, pyloric stenosis, common bile duct obstruction, and tumor. Pancreatic adenocarcinoma develops in 4% of cases in individuals with more than a 20-year history of chronic pancreatitis.
Diagnosis of chronic pancreatitis is quite complex and is based on 3 main signs: a characteristic history (pain attacks, alcohol abuse), the presence of exocrine and/or endocrine insufficiency and identification of structural changes in the pancreas.
The level of amylase and serum lipase often remains normal or reduced during an attack of pancreatitis, which is explained by a decrease in the number of acinar cells producing these enzymes. When alcoholic pancreatitis is combined with alcoholic liver disease, abnormal liver function tests may be detected. In 5–10% of cases of chronic pancreatitis, there are signs of compression of the intrapancreatic part of the bile duct caused by edema or fibrosis of the head of the pancreas, which is accompanied by jaundice, increased levels of direct bilirubin and serum alkaline phosphatase.
Impaired glucose tolerance develops in 2/3 of patients, diabetes mellitus in 30% of patients with chronic pancreatitis.
Exocrine insufficiency becomes obvious and easily detected with the development of malabsorption syndrome, in which fat in the feces can be determined qualitatively (Sudan stain) or quantitatively. Secretory insufficiency is detected at earlier stages using pancreatic functional tests.
In recent years, an enzyme-linked immunosorbent method for determining elastase-1 in the blood serum and feces of patients has been introduced into clinical practice for the diagnosis of chronic pancreatitis, which makes it possible to assess the exocrine function of the pancreas [4].
Instrumental data to confirm the assumption of the presence of chronic pancreatitis can be considered quite informative. Ultrasound examination of the abdominal organs is used; endoscopic ultrasound, spiral computed tomography and magnetic resonance imaging of the pancreas. ERCP can detect duct stenosis, localization of obstruction, structural changes in small ducts, intraductal calcifications and protein plugs, but there is a high risk of developing acute pancreatitis [5, 6].
The goal of treatment of chronic pancreatitis can be considered to solve several problems: eliminating provoking factors (alcohol, drugs, obstruction); pain relief; correction of exo- and endocrine insufficiency; treatment of associated disorders. The main goals of conservative treatment are to stop or slow the progression of chronic pancreatitis and combat its complications. Depending on the severity of abdominal pain, a step-by-step treatment of chronic pancreatitis is used, including the following components (modified by Ihse et al., 1993).
- Diet, fractional meals, fats less than 60 g/day.
- Pancreatic enzymes (Pancreatin, Creon, Mezim, Panzinorm, Festal, Pensital, Enzistal) + H2 blockers (famotidine, ranitidine, cimetidine, nizatidine).
- Non-narcotic analgesics (acetylsalicylic acid, diclofenac, ibuprofen, piroxicam).
- Octreotide (Sandostatin).
- Endoscopic drainage (Olimpus, LOMO, Pentax, Fujinon).
- Narcotic analgesics (butorphanol, antaxone, fortal, tramadol, sedalgin-neo).
- Solar plexus block.
- Surgical intervention.
With mild pain syndrome, success can be achieved through a strict diet, small meals (every 3 hours) and limiting fat to 60 g per day, which helps reduce pancreatic secretion with a low-calorie diet. Given the fact that the main cause of pain is intraductal hypertension, it is advisable to use drugs that block stimulated pancreatic secretion. Normally, the release of cholecystokinin, the main stimulator of exogenous pancreatic function, is regulated by cholecystokinin-releasing peptide in the proximal small intestine, which is sensitive to trypsin and active in the intestinal lumen. The administration of pancreatic enzymes (mezim forte, pancreatin, panzinorm, pancitrate lycrease) provides significant relief of pain in some patients due to the inclusion of a feedback mechanism: an increase in the level of proteases in the lumen of the duodenum reduces the release and synthesis of gastrointestinal hormones (cholecystokinin), which leads to a decrease stimulation of exocrine pancreatic function, reduction of intraductal and tissue pressure and pain relief [7, 8].
One should be aware of the possibility of inactivation of exogenous digestive enzymes by stomach acid and pancreatic proteases. To prevent this effect, a combination of enzymes (Pancreatin, Creon, Mezim, Panzinorm, Festal, Penzital, Enzistal) with H2-histamine blockers (famotidine, ranitidine, cimetidine, nizatidine) is widely used. Doses of enzyme preparations for pain relief must be adequate; in a placebo-controlled, double-blind study, pancreolipase at a dose of 6 tablets 4 times a day for 1 month significantly reduced pain in 75% of patients with moderate to severe pancreatitis. Pancreatic enzymes in encapsulated form containing acid-resistant mini-microspheres (Creon) are currently the first choice drugs in the treatment of abdominal pain in exocrine pancreatic insufficiency. Microgranular dosage forms (Creon 10,000 or 25,000) are characterized by rapid (after 45 minutes) release of more than 90% of enzymes at a pH of duodenal and small intestinal contents of 5.5 and above. At very low pH values in the gastrointestinal tract, adjuvant therapy with H2 antagonists or proton pump inhibitors (lansoprazole, omeprazole, pantoprazole, rabeprozole) is used. In addition, enzyme replacement therapy has been shown to improve the transit of food through the gastrointestinal tract, affecting the motor function of the gastrointestinal tract and thereby helping to reduce malabsorption. Pancreatic enzymes are prescribed in all cases of chronic pancreatitis to correct the exocrine function of the pancreas. Taking these drugs reduces intestinal distension and diarrhea caused by malabsorption of fats, and therefore reduces pain. Enzyme preparations reduce the intensity of pain in moderate chronic pancreatitis, especially in women with obstructive pancreatitis; against the background of pancreas divisum. In men with alcoholic calcific pancreatitis, these drugs are significantly less effective. To relieve steatorrhea in chronic pancreatitis, film-coated drugs with a high lipase content are indicated; for pain relief - drugs with a high content of proteases without a coating.
If there is no effect of enzyme replacement therapy in combination with H2-histamine blockers, it is necessary to prescribe analgesics; for this purpose, paracetamol (daleron, prodol, efferalgan), non-steroidal anti-inflammatory drugs: diclofenac (apo-diclo, voltaren, diclofenac, ortofen), ibuprofen (apo -ibuprofen, ibuprofen, ibufen, solpaflex), piroxicam (piroxicam, piroxifer, felden, erazon), celecoxib (celebrex), lornoxicam (xefocam), meloxicam (meloxicam, movalis), nimesulide (mesulide, nise, niculid), naproxen (apo -naproxen, nalgesin, naproxen). To relieve pain in chronic pancreatitis, octreotide (Sandostatin) is prescribed. As a potent inhibitor of neuroendocrine hormones of the gastrointestinal tract, sandostatin inhibits exogenously stimulated and endogenously stimulated exocrine pancreatic secretion by direct action on exocrine tissue and reduces the release of secretin and cholecystokinin. In a multicenter study, sandostatin at a dose of 200 mcg subcutaneously 3 times a day for 4 weeks reduced the severity of pain in 65% of patients with chronic pancreatitis. The drug is also effective in the treatment of pseudocysts, pancreatic ascites and pleurisy. We use small doses: 50–100 mcg subcutaneously 2 times a day for 1 week to treat painful chronic pancreatitis.
If the pain syndrome persists, it is necessary to perform ERCP to morphologically clarify the nature of the lesion of the ducts and exclude dysfunction of the sphincter of Oddi. In this case, the possibility of using invasive treatment methods is discussed: endoscopic drainage and bypass, solar plexus blockade with steroids, pancreaticojejunostomy and pancreatic resection.
The greatest difficulties are associated with the treatment of dysfunction of the sphincter of Oddi, one of the causes of the development of chronic pancreatitis, which is difficult to diagnose. With dysfunction of the sphincter of Oddi, there is increased sensitivity of the wall of the pancreatic and bile ducts to changes in volume and pressure. It is necessary to exclude drugs that have a choleretic effect (bile acids, including those contained in enzyme preparations - festal, enzistal, etc.; decoctions of choleretic herbs, synthetic choleretic agents). To relieve spasm of the smooth muscles of the sphincters of Oddi and the cystic duct, nitrates are used: nitroglycerin for quick pain relief, nitrosorbitol for a course of treatment (under drug tolerance monitoring).
Myotropic antispasmodics (bendazole, bencyclane, drotaverine, mebeverine, papaverine) reduce the tone and motor activity of smooth muscles. The main representatives of this group are papaverine, drotaverine (no-shpa, no-shpa forte, vero-drotaverine, spasmol, spakovin), bencyclane (halidor).
The most effective myotropic antispasmodic is duspatalin (mebeverine) - a muscletropic, antispastic drug that has a direct effect on smooth muscles. By selectively acting on the sphincter of Oddi, it is 20-40 times more effective than papaverine in terms of its ability to relax the sphincter of Oddi.
It is important that duspatalin does not affect the cholinergic system and therefore does not cause side effects such as dry mouth, blurred vision, tachycardia, urinary retention, constipation and weakness. It is actively metabolized when passing through the liver, all metabolites are quickly excreted in the urine. Complete excretion of the drug occurs within 24 hours after taking a single dose; as a result, it does not accumulate in the body; even elderly patients do not require dose adjustment. Duspatalin is prescribed 1 capsule (200 mg) 2 times a day, it is better to take it 20 minutes before meals.
Another myotropic antispasmodic with selective properties is hymecromone (odeston), a phenolic derivative of coumarin that does not have anticoagulant properties and has a pronounced antispasmodic and choleretic effect. Hymecromone is a synthetic analogue of umbelliferone, found in anise and fennel fruits, which were used as antispasmodics. The drug provides one or another effect depending on the characteristics of its action at various levels of the biliary tract. Odeston causes dilatation of the gallbladder, reduces intraductal pressure and, thus, is an antagonist of cholecystokinin. At the level of the sphincter of Oddi, it acts synergistically with cholecystokinin, reduces basal pressure and increases the duration of opening of the sphincter of Oddi, thereby increasing the passage of bile through the bile ducts. Being a highly selective antispasmodic, odeston also has choleretic properties. Its choleretic effect is due to the acceleration and increase in the flow of bile into the small intestine. An increase in the flow of bile into the lumen of the duodenum helps to improve digestion processes, activate intestinal motility and normalize stool.
Odeston is prescribed 400 mg (2 tablets) 3 times a day 30 minutes before meals, which ensures a relatively constant drug concentration in the serum exceeding 1.0 mcg/ml. The duration of treatment is individual - from 1 to 3 weeks. Odeston is low-toxic and is usually well tolerated.
If there is no effect from conservative therapy for sphincter of Oddi dysfunction and there is evidence of its stenosis, restoration of the patency of the sphincter of Oddi is carried out surgically (sphincterotomy).
Replacement therapy for exocrine pancreatic insufficiency as a result of chronic pancreatitis is carried out in the presence of steatorrhea of more than 15 g of fat per day, progressive loss of body weight and dyspeptic disorders. A single dose of enzymes must contain at least 20,000–40,000 units of lipase, so it is prescribed 2–4 capsules with main meals and 1–2 capsules with additional small amounts of food. With clinically significant pancreatic insufficiency, it is often not possible to eliminate steatorrhea completely. An increase in body weight, normalization of stool, and a decrease in flatulence indicate the adequacy of the selected dose of digestive enzymes. The ineffectiveness of replacement therapy requires the exclusion of other causes of malabsorption syndrome - Crohn's disease, celiac disease, thyrotoxicosis. To correct nutritional deficiencies, medium chain triglycerides (trisorbon) and fat-soluble vitamins A, D, E, K are prescribed.
For questions regarding literature, please contact the editor.
T. N. Lopatkina , Candidate of Medical Sciences, Associate Professor of MMA named after. I. M. Sechenova, Moscow
How to take Creon
The dosage of Creon 10,000 in adults is determined by the patient’s health condition and the degree of enzyme deficiency. Gelatin capsules with pancreatin are taken with or immediately after meals. This applies not only to full meals, but also to snacks.
Capsules must be swallowed whole with plenty of water. If the medicine is taken by an elderly person, a bedridden patient who has difficulty swallowing, you can open the shell and mix the contents of the capsules with soft food. Here you need to follow some rules:
- Food should not be hot.
- You can use products with a sour taste. Kefir or yogurt, sour fruit juice, fruit or vegetable puree are suitable for mixing.
- After stirring the minimicrospheres, the contents should be taken orally immediately. Enzymes mixed with food cannot be stored, including in the refrigerator.
- It is not advisable to chew minimicrospheres during administration. Chewing leads to the destruction of the protective shell of the granules and the release of active components into the mouth. This reduces the effectiveness of the drug and can lead to irritation of the oral mucosa.
- When taking enzyme preparations, you should monitor your drinking regime. If there is a lack of fluid, taking Creon 10000 can cause constipation.
The use of enzyme preparations for digestive disorders in children
Digestion is a single, holistic process due to the close relationships between the activities of various parts of the digestive tract. Dysfunction of one part of the gastrointestinal tract, as a rule, leads to dysfunction of other organs. Different processes of absorption of nutrients occur in different parts of the digestive tract. In the stomach - protein breakdown, secretion of internal factor, oxidation of iron ions; in newborns - the breakdown of fats (formation of diglycerides under the action of gastric lipase). In the duodenum - entry of bile acids, emulsification of fat, breakdown of triglycerides, formation of mono- and diglycerides, breakdown of starch and disaccharides, breakdown of protein, absorption of monosaccharides, amino acids, iron, calcium, zinc, magnesium. In the jejunum - breakdown of disaccharides; absorption of monosaccharides, monoglycerides, bile acids, fat-soluble vitamins, folate, calcium, iron, magnesium, zinc, vitamin B12. In the ileum - absorption of bile salts, water, sodium, and the main amount of vitamin B12. In the large intestine - absorption of water, potassium, sodium, calcium, bile salts.
An important digestive organ in the body is the pancreas (PG), which performs an exocrine function. When food enters the gastrointestinal tract, the pancreas secretes into the small intestine not only pancreatic enzymes, but also bicarbonates, which neutralize hydrochloric acid and maintain an alkaline environment in the duodenum, necessary for the normal functioning of pancreatic enzymes. Under physiological conditions, the pancreas produces from 50 to 2500 ml of secretion per day, depending on the age of the person and the nature of the incoming food. Pancreatic juice is a colorless liquid with an alkaline reaction (pH 7.8–8.4). It contains organic substances (proteins) and inorganic components (bicarbonates, electrolytes, trace elements), as well as mucus of the excretory ducts. The enzymatic part of the secretion is formed in acinar cells, and the liquid (water-electrolyte) part - mucin and bicarbonates - by the ductal epithelium. With the help of pancreatic enzymes (lipase, amylase and proteases), which play a key role in the exocrine function of the pancreas, the breakdown of nutrients occurs. Most of them are in an inactive form - these are proenzymes that are activated in the duodenum by enterokinase. Lipase, amylase and ribonuclease are secreted in active form. This mechanism determines the activity of pancreatic juice in the intestinal cavity, which, in turn, protects pancreatic tissue from autolysis.
Digestive enzymes of the pancreas have their own targets: amylase - α-1,4-glycosidic bonds of starch, glycogen; lipase - triglycerides (formation of di-monoglycerides and fatty acids); phospholipase A - phosphatidylcholine (formation of lysophosphatidylcholine and fatty acids); carboxylesterase - cholesterol esters, esters of fat-soluble vitamins, tri-, di-, monoglycerides; trypsin - internal protein bonds (basic amino acids); chymotrypsin - internal protein bonds (aromatic amino acids, leucine, glutamine, methionine); elastase - internal bonds of proteins (neutral amino acids); carboxypeptidase A and B - external bonds of proteins, including aromatic and neutral aliphatic amino acids (A) and basic (B) amino acids from the carboxyl end.
The last four enzymes are secreted by the pancreas in an inactive form (proenzymes) and are activated in the duodenum.
Exocrine pancreatic dysfunction is observed in various hereditary and acquired diseases and may be caused by impaired formation of pancreatic enzymes or their activation in the small intestine. Due to pancreatic dysfunction, accompanied by enzyme deficiency, a disorder of food digestion (maldigestion) and absorption of nutrients (malabsorption) in the intestine develops.
Maldigestion in children is caused by a number of disorders.
- Decreased activity of pancreatic enzymes. It can be caused by chronic or acute pancreatitis, cystic fibrosis, congenital pathology of the pancreas - morphological anomalies of the pancreas (abberant pancreas, ring-shaped pancreas, stenosis of the papilla of Vater or sphincter of Oddi, cysts, bifurcated pancreas), hereditary syndromes accompanied by congenital pancreatic insufficiency (Shwachman syndrome). Diamond, pancreatic insufficiency syndrome with multiple anomalies, deafness and dwarfism (Iohanson-Bizzard), pancreatic insufficiency syndrome with vacuolation of bone marrow cells and sideroblastic anemia (Pearson); isolated enzymatic deficiency (lipase - Sheldon-Rey syndrome; amylase, trypsin, enterokinase) , as well as pancreatic trauma, pancreatic carcinoma, primary sclerosing cholangitis.
- Bile acid deficiency in the small intestine associated with functional disorders of the biliary tract, hepatitis, liver cirrhosis, biliary obstruction.
- Violation of cholecystokinin synthesis caused by damage to the duodenal bulb (chronic duodenitis, chronic gastroduodenitis).
- Inactivation of pancreatic enzymes in the small intestine as a result of intestinal dysbiosis or rapid passage of food.
- Impaired mixing of enzymes with food chyme associated with gastro- and duodenostasis.
The cause of malabsorption is a violation of the activity of the secretion of intestinal enzymes, caused by disaccharidase deficiency, a gastrointestinal form of food allergy, a violation of intracellular digestion (celiac disease, Crohn's disease, enteritis, etc.), a violation of the transport of absorbed substances (exudative enteropathy, lymphoma, tumors, tuberculosis).
It is known that the pancreas has great compensatory capabilities, and disorders of pancreatic secretion appear only in cases of severe damage to the gland. There is an opinion that severe steatorrhea and creatorrhea in adults develop in cases where the secretion of pancreatic lipase and trypsin decreases by more than 90%. However, such a threshold has not been established in children.
The causes and mechanisms of development of exocrine pancreatic insufficiency are varied. There are absolute pancreatic insufficiency, caused by a decrease in the volume of functioning pancreatic parenchyma, and relative, which can be associated with various diseases of the gastrointestinal tract.
If symptoms indicating exocrine pancreatic insufficiency are identified, it is necessary to begin replacement therapy with pancreatic enzymes as early as possible, before malabsorption begins to develop.
Clinical signs of exocrine pancreatic insufficiency are:
- stomach ache,
- loss of appetite,
- flatulence,
- unstable chair,
- steatorrhea,
- nausea,
- recurrent vomiting,
- general weakness,
- weight loss,
- decreased physical activity,
- growth retardation (in severe forms).
There are quite a large number of methods for assessing the digestive capacity of the gastrointestinal tract.
- Determination of the content of pancreatic enzymes in the blood and urine. In acute pancreatitis, the level of amylase in the blood and urine can increase 5-10 times; the level of amylase and lipase in the blood during exacerbation of chronic pancreatitis can be normal or increase for a short time by 1-2 times (from several hours to several days), determination of elastase-1 in the blood plasma, the level of its increase reflects the severity of pancreatitis. The development of hyperenzymemia depends on the period and severity of pancreatitis.
- Scatological research. It should be recognized that scatological research has not lost its relevance to this day and is the most accessible method. It should be carried out before prescribing pancreatic enzymes to the patient. However, the accuracy of this method is also influenced by the state of intestinal motility, the volume of bile secreted into the intestinal lumen, its qualitative composition, the presence of inflammatory processes in the intestine, etc.
In case of digestive disorders, the following symptoms are identified: steatorrhea - the presence of neutral fat in the stool (type 1 steatorrhea); fatty acids, soap (type 2 steatorrhea); both (steatorrhea type 3); creativeorrhea - may be a sign of a violation of the exocrine function of the pancreas. Normally, there are very few muscle fibers in feces; amilorrhea - the presence of a large number of starch grains in the stool - indicates a violation of the breakdown of carbohydrates; It is rarely detected in patients with pancreatic insufficiency, since starch hydrolysis is practically not impaired due to the high activity of intestinal amylase. The earliest sign of exocrine pancreatic insufficiency is steatorrhea; creatorrhoea appears somewhat later. Amilorrhea is rarely observed in exocrine pancreatic insufficiency.
- Study of the content of pancreatic enzymes in duodenal secretions. The method allows you to determine the type of secretion: normosecretory, hypersecretory, hyposecretory or obstructive. The identified types of secretion reflect different degrees of functional and morphological changes in the pancreas, which allows differentiated treatment measures.
- Quantitative determination of fat in feces (stool lipid profile). This method makes it possible to summarize the total amount of fat in feces, taking into account fat of exogenous (food) origin. Normally, the amount of fat excreted in feces should not exceed 10% of the fat introduced with food. In diseases of the pancreas, the amount of fat excreted in feces sometimes increases to 60%. The method can be used to clarify the nature of steatorrhea and assess the effectiveness of enzyme therapy.
- Determination of elastase-1 content in feces. Elastase-1 is a proteolytic enzyme of the pancreas. It is known that human pancreatic elastase does not change its structure as it passes through the gastrointestinal tract. This method has certain advantages over those used today in the diagnosis of exocrine pancreatic insufficiency (fecal lipidogram, coprogram, determination of chymotrypsin in feces) due to the high specificity of the method (93%), its non-invasiveness and the lack of influence of enzyme preparations on the results of the elastase test.
Enzyme preparations were first used in gastroenterological practice about 100 years ago. Digestive enzymes are currently widely used for various gastroenterological pathologies. Despite the variety of manifestations of enzymatic digestive disorders, the main direction of treatment for such patients is enzyme replacement therapy. Currently, a large number of enzyme preparations are used in clinical practice, characterized by different combinations of components, enzyme activity, production method and release form. When choosing an enzyme preparation in each specific case, the doctor must first of all pay attention to its composition and the activity of its components.
There are two directions of action of enzyme preparations:
- primary - hydrolysis of food substrates, which is the basis for prescribing enzymes as replacement therapy for exocrine pancreatic insufficiency;
- secondary - reduction of abdominal pain syndrome (with pancreatitis), dyspepsia (feeling of heaviness, flatulence, belching, stool disorders, etc.).
Indications for prescribing enzyme therapy are:
- impaired secretion of pancreatic enzymes;
- maldigestion and malabsorption syndrome;
- motility disorders of the gastrointestinal tract.
Classification of enzyme preparations
The following groups of enzyme preparations are distinguished.
- Preparations containing pancreatin (pancreatin, penzital, mezim forte, panzinorm forte - N, creon, pancitrate).
- Preparations containing pancreatin, bile components, hemicellulase and other components (festal, digestal, enzistal, panzinorm forte).
- Herbal preparations containing papain, rice fungus extract and other components (pepphys, oraza).
- Combined enzymes containing pancreatin in combination with plant enzymes, vitamins (wobenzym, phlogenzyme).
Despite the fact that there are currently many pancreatic enzyme preparations in the doctor’s arsenal, it is still not always possible to select adequate enzyme replacement therapy in patients with severe forms of pancreatic insufficiency. The instability of many enzymes in an acidic environment remains a serious problem.
Products containing pancreatin include lipase, amylase, proteases. The raw material for the preparation of these drugs is the pancreas of pigs and cattle. When choosing enzyme preparations, it is necessary to take into account the level of enzymes included in their composition (Table 1).
Preparations containing pancreatic enzymes can be used either continuously, as replacement therapy, or once, with a high food load. The dose is selected individually and depends on the severity of clinical and laboratory parameters of exocrine pancreatic function. The effectiveness of the dose is judged by clinical (disappearance of abdominal pain, normalization of stool frequency and character) and laboratory indicators (disappearance of steatorrhea and creatorrhoea in the coprogram, normalization of triglycerides in the stool lipidogram).
Enzyme-containing preparations, along with pancreatin, may contain bile acids, hemicellulase, plant choleretic components (turmeric), simethicone, etc. (Table 2). The main indication for the use of drugs in this group in children is dysfunction of the biliary tract (hypomotor dyskinesia). Bile acids and salts increase the contractile function of the gallbladder, normalize the biochemical properties of bile, and also regulate the motility of the large intestine in children with constipation. They should be used during or immediately after meals (without chewing) 3-4 times a day in courses of up to 2 months. Enzymes of this group are not used for pancreatitis, as they contain bile components that enhance intestinal motility.
Bile acids included in the preparations increase pancreatic secretion and choleresis; stimulate intestinal and gallbladder motility.
Under conditions of microbial contamination of the intestine, deconjugation of bile acids occurs, and cyclic adenosine monophosphate of enterocytes is activated with the development of osmotic and secretory diarrhea. Bile acids enter the enteropathic circulation and are metabolized in the liver, increasing the load on it. In addition, bile acids can have a direct damaging effect on the intestinal mucosa.
Hemicellulase ensures the breakdown of polysaccharides of plant origin (digestible fiber) and reduces gas formation.
Contraindications to the use of enzyme preparations containing bile components:
- acute pancreatitis;
- chronic pancreatitis;
- acute and chronic hepatitis;
- diarrhea;
- peptic ulcer of the stomach and duodenum;
- inflammatory bowel diseases.
Enzyme preparations of plant origin containing papain, rice fungus extract and other components can be used to correct exocrine pancreatic insufficiency. They are made from plant materials.
The group of enzyme preparations of plant origin includes:
- Nigedase - plant lipase (Nigella damascene) - 20 mg; the drug, due to the absence of proteo- and amylolytic enzymes in its composition, is prescribed in combination with pancreatin;
- orase - a complex of amylolytic and proteolytic enzymes of fungal origin - Aspergillus oryzae (lipase, amylase, maltase, protease);
- pepphys - fungal diastase - 20 mg, papain - 60 mg, simethicone - 25 mg;
- solizym - lipase produced by the fungus Penicillum solution (20,000 units);
- somilase—solizim and fungal L-amylase;
- unienzyme - fungal diastase - 20 mg, papain - 30 mg, simethicone - 50 mg, activated carbon - 75 mg, nicotinamide - 25 mg;
- Wobenzym - pancreatin - 100 mg, papain - 60 mg, bromelain - 45 mg, trypsin - 24 mg, chymotrypsin - 1 mg, rutoside - 50 mg;
- merkenzyme - pancreatin - 400 mg, bromelain - 75 units, bile - 30 mg;
- phlogenzyme - bromelain - 90 mg; trypsin - 48 mg, rutoside - 100 mg.
The preparations pepphys, unienzyme, wobenzym, merkenzyme and phlogenzyme contain bromelain - a concentrated mixture of proteolytic enzymes from the extract of fresh pineapple fruits and its branches. The effectiveness of bromelains does not depend on the amount of hydrochloric acid in the stomach (pH 3-8.0).
All of the listed enzyme preparations of plant origin are contraindicated in patients with fungal and household sensitization, and with bronchial asthma (A. A. Korsunsky, 2000). Solizim and somilase should not be prescribed if you are allergic to penicillin antibiotics.
Enzymes based on plant materials can be used to correct exocrine pancreatic insufficiency, especially in cases where the patient cannot tolerate pancreatic enzymes (allergy to pork, beef).
It should be noted that data have appeared in the literature indicating the low enzymatic activity of enzymes of plant and fungal origin (75 times less effective than drugs of animal origin), and therefore they have not found widespread use in pediatric practice.
Simple enzymes (betaine, abomin) do not belong to the group of pancreatic enzymes. The following drugs with proteolytic activity are currently registered:
- abomin (combined preparation from the gastric mucosa of calves and lambs);
- acidin - pepsin (the tablet contains 1 part pepsin and 4 parts betaine hydrochloride; when it enters the stomach, betaine hydrochloride is hydrolyzed and hydrochloric acid is released);
- pepsidil (contains pepsin and peptones);
- pepsin (a proteolytic enzyme obtained from the mucous membrane of pigs and lambs).
These drugs are obtained from the gastric mucosa of pigs, calves or lambs. The presence of pepsin, cathepsin, peptidases, and amino acids in the preparations promotes the release of gastrin, which is a regulatory polypeptide, and therefore drugs of this group can be prescribed for functional disorders of the gastrointestinal tract, for gastritis with secretory insufficiency, which is relatively rare in older children. These drugs are prescribed orally with meals.
These drugs should not be prescribed for exocrine pancreatic insufficiency.
The success of therapy for exocrine pancreatic insufficiency depends on many reasons. Recent studies have not found significant differences in effectiveness when taking enzyme preparations hourly and using them with meals. However, the most convenient and physiological for the patient is to take enzyme preparations with meals.
In the case of an adequately selected dose and form of the enzyme preparation, a significant improvement in the patient’s condition occurs. The criteria for the effectiveness of treatment are the disappearance of polyfecal matter, reduction or elimination of diarrhea, increase in body weight, disappearance of steatorrhea, amilorrhea and creatorrhoea. Creatorrhoea is usually the first to disappear during enzyme therapy. This may be due to the fact that the secretion of pancreatic protease persists slightly longer than lipase.
The dose of the enzyme preparation is selected individually during the first week of treatment, depending on the severity of exocrine pancreatic insufficiency. It is advisable to calculate the dose of the enzyme preparation based on lipase, starting with small dosages (1000 IU of lipase per kg of body weight per day). If there is no effect, the dose of the drug is gradually increased under the control of scatological studies. For severe exocrine insufficiency, 4000–5000 IU of lipase per kg of body weight per day is used in 3–4 doses. The duration of therapy is determined individually. Enzyme intake is stopped if clinical and scatological signs of maldigestion and malabsorption disappear.
Reasons for lack of effect with enzyme therapy:
- insufficient dose of the drug;
- loss of enzyme activity in the drug due to violation of shelf life;
- inactivation of the enzyme in the stomach;
- destruction of enzymes during intestinal dysbiosis with high colonization of the stomach and duodenum;
- inactivation of enzyme preparations due to high “acidification” of the duodenum (to prevent this phenomenon, antacids and H2-histamine receptor blockers are prescribed);
- incorrect diagnosis (type 2 steatorrhea; giardiasis, etc.);
- violation of the drug regimen.
Despite the fact that with the help of enzyme preparations the degree of steatorrhea can be significantly reduced, its complete and permanent disappearance cannot always be achieved.
Factors that prevent the disappearance of steatorrhea:
- malabsorption syndrome;
- low micellar concentration of bile acids due to the fact that they are deposited in the pathologically acidic contents of the duodenum;
- non-simultaneous release of enzymes from the stomach with food (microtablets or microspheres with a diameter of no more than 2.0 mm are transported from the stomach faster than tablets or dragees of large diameter);
- sensitivity of lipase to the acidic contents of the stomach (up to 92% of the lipase included in “ordinary” enzymes is easily destroyed by hydrochloric acid).
Ways to overcome enzyme inactivation by gastric juice:
- increasing the dose of the drug;
- prescribing antacids (it must be remembered that antacids containing calcium or magnesium weaken the action of enzymes);
- prescription of H2-blockers of histamine receptors.
Contraindications to the use of enzyme preparations:
- acute pancreatitis (first 7-10 days);
- exacerbation of chronic pancreatitis (during the first 3-5 days);
- allergy to pork and beef products.
Currently, thanks to a large selection of pancreatic enzyme preparations, there is a real possibility of individual correction of digestive disorders in children with exocrine pancreatic insufficiency, functional disorders of the stomach, and biliary tract. Prescribing enzyme preparations requires a differentiated approach from the doctor in each specific case - it is necessary to take into account the mechanisms of development of the disease that led to disruption of the digestive processes.
N. A. Korovina , Doctor of Medical Sciences, Professor I. N. Zakharova , Doctor of Medical Sciences, Professor of RMAPO, Moscow
Dosage
Replacement therapy with enzyme preparations requires medical supervision. The doctor pays attention to the cause of enzyme deficiency, the patient’s age and body weight. The dosage of Creon 10000 is measured in lipase units. For example, at the beginning of treatment for cystic fibrosis, adult patients require 500 units of lipase per kilogram of body weight per meal. In the future, the dosage should not exceed 10,000 units/kg body weight per day with regular monitoring of steatorrhea.
Since patients with cystic fibrosis receive increased dosages of the drug, constant monitoring of the condition of the intestines is necessary due to the risk of developing fibrosing colonopathy. In medical practice, there are cases where, against the background of regular intake of large doses of pancreatin, a person developed strictures of certain sections of the intestine. In this condition, the intestinal lumen narrows, making it difficult for food to pass through. To avoid complications, it is important for patients with cystic fibrosis to undergo regular medical examinations and take timely measures if there are signs of intestinal obstruction.
As for other diseases that are accompanied by a decrease in pancreatin production, here it is necessary to take into account not only the severity of the disease, but also the characteristics of the patient’s diet. Typically, for adults, the dosage ranges from 25,000 to 80,000 units per meal. These dosages are suitable for a full meal, and for snacks it is enough to take half the dose. The need for lipase increases if the diet contains a lot of fatty foods.
If the patient does not have gastrointestinal diseases, and enzyme deficiency is caused by an improper diet, 10,000 to 20,000 units of pancreatin are required per meal. It is important to remember that the prescription and dosage of the drug should be agreed with your doctor.
Instructions for use "Creon"
The drug is taken orally, and a single dose is selected individually, depending on the patient’s age, condition, diet, and concomitant diseases. Before starting therapy, a doctor's consultation is recommended.
General recommendations for admission:
- Single dose in the amount of 1/2 or 1/3 at the beginning of the meal.
- The rest - after a few minutes (but during the meal).
Typically, the capsules are swallowed and washed down with water. But if swallowing is difficult (infants, seriously ill people, elderly patients), the capsules should be carefully opened and the contents poured into water, soup or other liquid food. At the same time, it should not have a high temperature (preferably up to 35-37 degrees) so that the enzymes do not collapse. You cannot chew or gnaw the capsules. It is best to drink them with water at room temperature.
For diagnosed cystic fibrosis, the dose is prescribed depending on the patient’s body weight and age:
- Up to 4 years inclusive - in the amount of 1000 lipase units per kilogram of body.
- From 5 years - in the amount of 500 lipase units per kg.
Also, the dosage depends on the nature of the disease and the stage of its development. The maximum amount of product received per day should not be more than 10,000 lipase units per 1 kg.
For the treatment of other diseases of the pancreas, the dosage is determined depending on the degree of insufficiency of digestive processes and the proportion of fats in the food taken. Moreover, the amount of the drug during the main dose ranges from 20,000 to 75,000 units, and during a snack – from 5,000 to 25,000 units.
At the initial stage, the dosage should be less - the optimal value is considered to be in the range from 10,000 to 25,000 units. To reduce steatorrhea and improve well-being, the dosage is increased gradually. In general, the daily amount of the drug is from 20,000 to 50,000 lipase units.
Side effects and contraindications
"Creon 10000" has no contraindications except in cases of hypersensitivity to the components of the product. As for side effects, unwanted reactions most often occur from the digestive system. Some patients experience the following symptoms:
- nausea and vomiting;
- abdominal pain;
- bowel dysfunction (diarrhea or constipation);
- strictures (narrowing of the lumen) of the intestine (with prolonged treatment with high doses);
- flatulence.
Taking Creon 10000 in adults can lead to rashes, itching, and redness of the skin. The frequency of allergic reactions is low.
As a rule, if the dosage is correctly chosen and the patient follows the rules of administration, the drug is well tolerated.
How to use Creon 10000 during gestation and lactation
At the moment, there are no results of clinical trials on the treatment of pregnant women with drugs based on pancreatic enzymes. Testing of these drugs on animals has confirmed their safety for the fetus and a breastfed child.
At the same time, experts advise avoiding independent uncontrolled use of enzyme products by pregnant and lactating women. The appointment should be made by a doctor, taking into account the physiological state of the patient and the characteristics of her health. The expected benefit of taking the drug for the mother must exceed the potential risk to the fetus or newborn.