PANCREATITIS – REVOLT OF THE PANCREAS
24.Dec.2019
With regular abuse of fatty and spicy foods, strong alcoholic drinks, one “fine” day you will definitely experience pain and heaviness in the abdomen, nausea, and indigestion. This will mean that the pancreas is “tired”, indicating its dissatisfaction with the manifestations of the first signs of pancreatitis
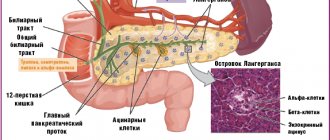
Despite its relatively small weight (80-90 grams), the pancreas plays a huge role in the functioning of the body. One of the most important functions is the production of special digestive enzymes and ensuring the digestion of proteins, fats and carbohydrates in the intestines. At the same time, the pancreas produces hormones (including insulin) that regulate blood glucose levels and the functioning of other body systems.
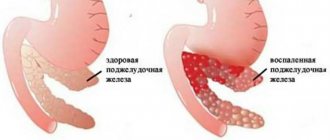
Sometimes, under the influence of various factors, the movement of digestive juices is disrupted. Liquids stop entering the small intestine and begin to corrode the tissue of the gland itself, causing severe inflammation of the latter - acute pancreatitis. Normal pancreatic tissue is gradually replaced by scar tissue. In the case when the endocrine parts of the gland are involved in the process, and subsequently are affected and die, then the person develops diabetes mellitus and the metabolism in the body is disrupted.
The first sign of acute pancreatitis is attacks of cutting pain in the pit of the stomach, intensifying after eating, the duration of which can take quite a long time. Often the pain radiates to the back, to the left and right hypochondrium, and can be girdling or simulating heart pain. The pain worsens if you lie on your back and gets better if you sit and lean forward. In addition, dry mouth, nausea, hiccups, belching, frequent vomiting, and diarrhea appear. In severe cases, the general condition quickly deteriorates: the temperature rises, the pulse quickens, shortness of breath appears, and blood pressure drops. In such a condition, you cannot do without medical help.
Risk factors
Doctors believe that the main causes of pancreatitis are alcohol consumption and gallbladder diseases, primarily cholelithiasis, in which the ducts of the gland become “clogged.” But there are other factors, including: diseases of the duodenum (gastroduodenitis, peptic ulcer), excessive food load (fatty and spicy foods), taking certain medications (antibiotics, paracetamol, sulfonamides, etc.), injuries, infections (hepatitis , mumps), obesity. In older people, the disease can appear when the blood circulation of the pancreas is impaired as a result of atherosclerosis. In addition, hereditary predisposition cannot be ruled out.
Diagnose and treat
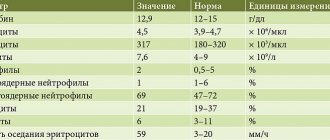
Diagnosing pancreatitis in the early stages is not always easy. This requires laboratory and instrumental studies. In some cases, abdominal x-rays, computed tomography and laparoscopy will also be required.
It is very important to start treatment as quickly as possible to stop the progression of the disease. As a rule, in the first days, patients are prescribed medications that reduce inflammation and pain, suppress the activity of the pancreas, are prescribed a strict diet (sometimes even several days of fasting) and bed rest. In severe cases, surgical treatment is necessary.
When the disease cannot be curbed, the disease becomes chronic. And periodically, especially after culinary and alcoholic excesses, it makes itself felt with attacks of pain and unpleasant sensations in the abdomen. To get rid of them, various digestive enzymes are used (Mezim, Festal, Creon, etc.). These drugs should be taken with meals, Moreover, the required dose directly depends on what the person will eat. In addition, all patients need to promptly treat cholelithiasis and cholecystitis, and keep blood sugar levels under control.
The best prevention is the right food
A person who has experienced attacks of pancreatitis naturally does not want a repetition of the latter. Therefore, in order to enjoy life in the future, you have to follow some rules. First, train yourself to eat small portions 5-6 times a day (fractional meals). The menu should be dominated by protein products - lean boiled meat and fish, dairy products, egg whites. Secondly, you can’t overeat at night. Thirdly, it is important, despite the temptations, to give up fatty, spicy, fried, smoked foods and alcohol.
If you adhere to these principles, attacks of chronic pancreatitis will occur much less frequently.
Yulia Gudkova, general practitioner, Nyagan City Clinic
Abdominal pain and chronic pancreatitis
Vladimir Trofimovich Ivashkin , academician of the Russian Academy of Medical Sciences, Doctor of Medical Sciences:
– We will talk about discussing abdominal pain. This is a classic question in clinical medicine. There was medicine, and there will be medicine, and there will always be abdominal pain, and abdominal pain will always lead to difficult thoughts for clinicians and, unfortunately, rash decisions. Quite recently, I looked at a patient who periodically had abdominal pain, but who did not show signs of an acute abdomen during the same period - there was no defence, tension, there was no positive Shchetkin-Blumberg, and so on, and so on. And now, apparently, one of the young surgeons finally decided that the patient’s complaints alone were enough with an absolutely soft abdomen. A soft abdomen, a woman allows her hand to reach any posterior surface. However, one of our surgeons decided that it was acute appendicitis, they entered and so on, well, and then the consequences were not very rosy.
Therefore, when we talk about abdominal pain, of course, we always need, before I give the floor to highly professional, respected lecturers, to ask ourselves the question: this pain is combined with the clinical picture of an acute abdomen, with classic symptoms - defence, tension, rebond, that is, positive Shchetkin - or not? And the second question: is this pain combined with one or another form of intestinal obstruction, with ileus or obstructive intestinal obstruction or not? Here is a triangle: pain - acute abdomen - intestinal obstruction. This triangle must always be kept in mind, then we will make fewer mistakes when interpreting abdominal pain. Now I am pleased to give the floor to Yuri Aleksandrovich Kucheryavyi, the representative of the glorious clinic headed by Igor Veniaminovich Mayev. Yuri Alexandrovich, please.
Yuri Aleksandrovich Kucheryavyi , associate professor, candidate of medical sciences:
– Dear Vladimir Trofimovich, Tatyana Lvovna, dear colleagues! Of course, I am glad to meet you and I am very pleased to open such an important representative symposium today. In anticipation of this report, I would like to ask one question both here in the audience and to everyone who is watching our symposium interactively today. If there is abdominal pain and there is no diagnosis yet, what should you use to try to relieve pain in this situation? Is it necessary to do this to alleviate our patient’s condition and make his examination more comfortable? If this answer is “yes,” then what will we consider as a means of choice in the future? If we look at the epidemiological situation in our country, it is quite understandable, because we have learned to treat the incidence and, accordingly, prevalence, including peptic ulcer disease, by introducing eradication therapy into routine practice.
We see a decrease - there are fewer and fewer patients with stomach ulcers and duodenal ulcers, and this is certainly reflected in the official statistics of the Ministry of Health. But at the same time, some diseases, such as, as we see, are included here - gastritis, duodenitis, pancreatic diseases, mainly pancreatitis, of course, and infectious enteritis and colitis - are characterized by growth. How can this be explained? If most, say, forms of chronic gastritis are associated with Helicobacter pyloricus, and we are coping with this infection, which has already affected the incidence of peptic ulcer disease, why is this nosology growing? Well, because we're probably just coding and recognizing diagnoses incorrectly. Unfortunately, reflux disease, dyspepsia, and a combination of these diseases are probably hidden behind the official diagnosis of “chronic gastritis.”
The situation with chronic pancreatitis can be assumed similarly – the incidence is more than 100 cases, which is approximately 10 times more than in Europe. Why? Because most of these cases are probably not pancreatitis, and this is also probably a functional pathology, irritable bowel syndrome, which can occur, so to speak, under the guise of pancreatitis or to some extent resemble girdle pain, as if specific to this disease. Of course, today, speaking about pain and chronic pancreatitis, we understand that chronic pancreatitis is a long-term non-infectious disease of the pancreas, the most important symptom of which is the inflammatory process, and, of course, pain characterizes the majority of patients with chronic pancreatitis. And over time, during this disease, irreversible morphological changes in the pancreatic parenchyma progress and signs of deficiency of pancreatic endocrine and exocrine function increase.
Today we have somewhat overestimated the contribution of available and previously understood etiological factors and we understand today that most cases of pancreatitis are of unknown etiology, it is idiopathic, because for one person one may be a pancreatotoxic dose of alcohol and smoking history, and for another it is completely different, and The basis of this variability is, of course, genetics. What is important to know today about chronic pancreatitis and pancreatic pain? That, of course, in the early stages of the disease, pancreatitis is characterized by either persistent, continuous pain, fairly long episodes, or acute episodes similar to attacks of acute pancreatitis. Of course, pain in chronic pancreatitis can be caused by its complications and signs of exocrine insufficiency, but I will allow myself to illuminate these mechanisms a little later. The situation today is that conservative pancreatology has remained a little behind other, more studied nosological forms of reflux disease, H. pylori associated diseases, irritable bowel syndrome, inflammatory bowel diseases and so on, and we find ourselves in a situation where We have very little evidence-based research to date.
Therefore, if we pay attention to both international and Russian recommendations, which are at the approval stage and are about to be published, then we will not see many old, seemingly familiar and reliable drugs there, because, unfortunately, many of them did not show their worth, and time, rather, dotted the i's that we cannot use them today, so some of the medicines have completely left the arsenal of doctors dealing with chronic pancreatitis in the world. Well, and, of course, I am proud to present the project, which is ending its existence today. It was published exactly a year ago, in the first issue of the Russian Journal of Gastroenterology, Hepatology, Coloproctology. We have been collecting information for a whole year, and I would like to thank all my colleagues, all members of the Russian Gastroenterological Association, practicing doctors, chief specialists who found the strength to study this document and sent us all their comments, critical reviews, many of which formed the basis the basis for the formation of an updated document, which will be called the new recommendations of the Russian Gastroenterological Association or “Protocols for the treatment of chronic pancreatitis”.
However, both the draft and the final version are based only on evidence from large international studies, meta-analyses and some of the largest Russian studies. According to this document, conservative treatment of chronic pancreatitis in the context of pain treatment is based on the exclusion of alcohol and tobacco smoking. In any case, regardless of what doses, what frequency and what length of experience of using these toxic substances a particular patient has, because today a large number of cohort epidemiological studies show us that these risk factors are quite significant. They cannot guarantee the development of chronic pancreatitis, but the risk of its development and unfavorable course increases significantly. The second most important element of pain relief is the use of analgesics, non-steroidal anti-inflammatory drugs, and the emphasis is on paracetamol, as the most tested in the world, at a dose of 500 mg per dose, and up to three doses per day, a maximum of this drug can be used.
With a treatment duration of 4 to 8 weeks, in some cases this therapy can be prolonged under strict monitoring of the patient’s condition, because we know about the possibility of adverse events with long-term therapy with such drugs. In the event that paracetamol has an insufficient effect, we can adjust the therapy, expanding it through the use of antidepressants that potentiate the action of analgesics, or use narcotic analgesics, but this is a very complex problem, and not only in Russia, and in the world in general, because it is very a high risk of developing addiction and large methodological, logistical, let’s say, restrictions on outpatient treatment with these drugs in principle. But if, after all, we have justified the prescription of narcotic analgesics, and the patient has an effect, then in this case we must predict a fairly rapid development of addiction, and in this case we must understand that this is not a very favorable scenario, and consider the help of our fellow endoscopist surgeons regarding the use of alternative methods of pain relief, including surgical treatment, because the development of addiction is very serious, and we cannot systematically approach this issue in this way.
At the second stage or on the second line, so to speak, an attempt to relieve pancreatic pain is, of course, the use of modern pancreatin preparations in sufficient doses, which can be combined with vitamin-mineral antioxidant complexes. There is a sufficient number of evidence-based studies indicating that both monotherapy with these drugs and their combination, respectively, gives a good analgesic effect, the only question is that the duration of use is quite long. It is many months of treatment with these drugs that can actually lead to a reduction in pancreatic pain, rather than just a few days or weeks of use, so we do not currently have high expectations for a quick effect in this combination. And the question remained open beyond these recommendations about the correction of motor impairment. Why did this happen? Because there are no randomized controlled trials on the use of antispasmodics in patients with chronic pancreatitis. It is very difficult to study motor disorders.
We understand that there are objective reasons for the lack of these studies, and, of course, there are a number of contradictions that I must talk about. Therefore, when discussing our draft recommendations, we encountered a large number of objections from practicing doctors and even researchers regarding the fact that many believe that there is still a place for antispasmodics in the treatment of chronic pancreatitis, because they are justified pathogenetically, we have been using these drugs for a long time in routine practice, they are even included in medical and economic standards, and we sometimes see the result, they also talk about this, and antispasmodics are characterized by a good safety profile when we are talking about modern and not outdated drugs. At the same time, one can object quite categorically as follows: if antispasmodics are used in the world, then only neurootropic ones, that is, m-cholinergics, and most definitely drugs of newer generations. On the other hand, pancreatitis is not an official indication for the use of these drugs, and their use will be justified, well, let’s say, pathogenetically or symptomatically. These drugs are not included in any standard for the management of chronic pancreatitis, excuse me, guidelines or recommendations; we will not find antispasmodics in any of them today, because there are no studies, and the recommendations are based only on evidence-based data. And, of course, the safety profile varies widely, from older drugs that have a very high incidence of adverse events to new drugs that have an extremely high safety profile. And, of course, it should be noted that almost all antispasmodics, both neurotropic and myotropic, reduce spasm only of intestinal smooth muscles, predominantly acting on this localization, and, of course, they are able to produce an effect, rather, in this segment.
While discussing the project, we came across several aspects that make sense to discuss, because there is a dissonance between evidence-based medicine and routine practice. Of course, we assume motor disorders in chronic pancreatitis, analyzing hypotheses of pathogenesis - duodenal hypertension, sphincter of Oddi dysfunction, and duodeno-pancreatic reflux, for example, where it would be appropriate to use the correction of motor disorders. However, there is actually too little real evidence today; we have indirect facts. If we are talking about dysfunction of the sphincter of Oddi, then today it is clear that it is not absolutely a risk factor for the development of chronic pancreatitis, and moreover, if we are talking about hydraulic theories and hypotheses of intrapancreatic activation of proteases, there is more substantiated data. Opie's theory, which is more than 100 years old today, is destroyed by one argument, which suggests that the pressure in the main pancreatic duct is significantly higher, almost an order of magnitude, than in the common bile duct and duodenum, which practically excludes bile or duodenal reflux with activation of proteases intrapancreatic. On the other hand, there is evidence regarding acute pancreatitis of an increase in intra-abdominal pressure by only 1 mm Hg. Art., accompanied by a more than twofold increase in the risk of developing severe acute pancreatitis, for example, or a connection with intra-abdominal pressure and complications of acute pancreatitis. But whether this is associated with intraduodenal pressure or is associated with some other factors, obesity, for example, or microcirculation disorders that can be caused by increased abdominal pressure, we do not know today.
On the other hand, I would like to note the validity of clinicians’ comments that signs of motor disorders are quite clearly manifested clinically during an attack of pancreatitis, especially with pancreatitis of biliary pathology, with pancreatic insufficiency, and, of course, these arguments are very, very fair. Moreover, even during examination, we observe that in some patients it is possible to identify certain indirect signs indicating the presence of motor disorders in chronic pancreatitis. Another important argument from practicing doctors is that empirical approaches such as the use of a variety of antispasmodics and prokinetics in the treatment of attacks of pancreatitis, biliary pancreatitis and pancreatic insufficiency can be effective, but in some cases we combine these drugs and use antibacterial agents , and infusion therapy, and many other means.
How can you tell if any one component of this circuit is actually working? This is very, very difficult, and, of course, unfortunately, we do not have studies that are devoted to the study of motility disorders and the effect of, say, antispasmodics on these motor disorders of the pancreatic ducts and their clinical effect. Therefore, if we look - perhaps not very timely in the logic of presentation of the material - at the mechanisms of pain, we will see that they are multifaceted. We know this: we are talking about obstruction of the ducts, and inflammation in the pancreatic parenchyma, especially perineural, and ischemia of the exocrine parenchyma, because complications of chronic pancreatitis such as pseudocysts can be characterized by large sizes and the formation of independent pancreatic pain, and, of course and secondary intestinal motility disorders. In addition, we understand that the etiology of pancreatitis may also influence the type and characteristics of pancreatic pain. Alcoholic pancreatitis is one situation, autoimmune pancreatitis is completely different, as many studies indicate today. Therefore, if we consider the presence of a spasm and the possibility of stopping it, it turns out that the niche for the use of antispasmodics is not so great.
Yes, theoretically, we can facilitate the outflow of pancreatic secretions, perhaps somehow influence the ischemia of the pancreatic parenchyma, and we can definitely influence secondary motility disorders, and it is in connection with this that today our standards do not contain antispasmodics. If we look at the same issue in the context of the use of analgesics, we will see that the effectiveness of these drugs will potentially be much greater, especially in terms of the effect on inflammation in the pancreatic parenchyma, which today many experts give leading importance in the development of long-term pancreatic pain . What restrictions are possible? This is one of the main critical points on the part of practicing doctors. This is the toxicity of these drugs, the potential hepatotoxic effect, the ulcerogenic effect, and, accordingly, we, of course, offer possible solutions. This is a combination with potentiating analgesics and drugs, these can be neurotropic antispasmodics, and antidepressants, this is also the use with proton pump inhibitors, off label today, but, nevertheless, with the aim of at least gastroprotection and, maybe maybe hopes for an indirect reduction of pain.
Well, and, of course, careful monitoring of the patient’s condition is necessary. If we prescribe 1.5, 2, 3 g of paracetamol, it is necessary to monitor blood biochemistry, at a minimum, and, of course, other indicators. If we ask ourselves which drug from the group of antispasmodics is appropriate to use to potentiate the action of analgesics or expect an independent effect, then we must understand that this drug should have a complex effect, with a pronounced antispasmodic effect, with a fast-acting effect, with a proven ability to potentiate and analgesics, and influence the sphincter of Oddi, and, of course, be characterized by high safety, because in any case we will be talking about combination therapy. And today there is only one answer to this question - hyoscine butyl bromide. Let's find out why. Firstly, there is a complex, combined mechanism of action - blockade of M-3 receptors, a ganglion-blocking effect, and another feature of the drug - the ability to reduce the secretion of the digestive glands. We do not currently know the real niche and ability to act on pancreatic secretion of this drug. This is worth studying in the future, but this property of reducing gastric secretion and pancreatic secretion may be quite beneficial.
Moreover, no other drug from the group of antispasmodics has such a comprehensive mechanism of action. Open studies that help us imagine a patient with pain syndrome, but without a diagnosis, who is prescribed Buscopan, paracetamol, their combinations or placebo, show us a serious difference between any regimen of use relative to placebo, a statistically significant difference in pain relief according to subjective and objective assessment . The study is quite large; we see more than 1.5 thousand patients included. Extrapolating the data obtained, we can assume that these studies open up certain prospects for us: potentiation of the action of paracetamol and tetracyclic antidepressants with the help of Buscopan and its combined use, perhaps the ability to reduce the daily doses of these drugs and the risk of drug intolerance.
Today we can safely say that there are only a few studies, and hyoscine butyl bromide is the only drug whose antispasmodic effect on the sphincter of Oddi has been proven using manometry of the sphincter of Oddi, and this is a very serious argument in favor of the use of this drug for pancreatitis. Well, answering the question that was announced in the debut of the lecture, what to use to try to relieve pain when there is no diagnosis yet, we have in our arsenal “Buscopan”, which provides quick action, a high probability of a positive effect in functional pathology, if it is the reason for treatment, a more comfortable examination of the patient, if this effect of pain relief or pain reduction is actually achieved, and, of course, this drug has absolutely no effect on somatic pain, which allows us to more correctly diagnose somatic surgical pathology in contrast to the use of analgesics. And if we look at the prospects, then Buscopan is a drug that may be promising for a number of patients in whom, perhaps, behind the picture of pancreatitis there will be a functional pathology of the intestine, this drug will be the most effective.
Even if we diagnose pancreatitis, then this drug, both in monotherapy and especially in combination with paracetamol, will be very successful. But if we are talking about functional dyspepsia, then, of course, here you need to choose other drugs, prokinetics, they will be more effective. Therefore, in conclusion, I would like to note the following that if we are talking about visceral abdominal pain syndrome, then the drug of choice today is hyoscine butylbromide, with an emphasis on the fact that this can be both a functional pathology and chronic pancreatitis. In chronic pancreatitis, motor disorders definitely occur, but their features have not been sufficiently studied, and, of course, if you choose drugs that affect motor skills, antispasmodics are more reasonable drugs for chronic pancreatitis, and this needs to be studied and proven in controlled studies. And if we supplement the therapy of chronic pancreatitis with neurotropic antispasmodics, we hope that they can have an additional positive effect. Thank you very much for your attention, and, of course, freedom to everyone from pancreatic pain.