Chronic pancreatitis
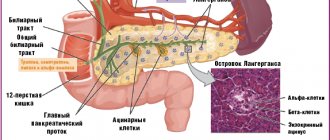
Chronic pancreatitis is a disease of the pancreas of inflammatory nature, in which periods of exacerbation of the inflammatory process lead to the replacement of the pancreatic parenchyma with fibrous connective tissue, which entails dysfunction of the pancreas.
Who is at risk?
- patients who abuse alcohol
- smokers,
- patients suffering from gallstone disease,
- patients who abuse high-calorie and spicy foods,
- patients with lipid and calcium metabolism disorders,
- patients who have close relatives suffering from chronic pancreatitis,
- patients with congenital developmental features of the pancreas,
- patients suffering from autoimmune diseases,
- patients who have suffered acute pancreatitis, pancreatic necrosis.
The disease can be suspected if the following symptoms occur:
- pain in the upper abdomen, which occurs or intensifies 20-30 minutes after eating, can radiate to the left shoulder, shoulder blade, and back.
- attacks of intense pain in the upper abdomen may be accompanied by nausea and sometimes vomiting.
- development of symptoms of dyspepsia (nausea, bloating, loose stools, etc.), especially in patients at risk, which may indicate a dysfunction of the pancreas - the development of exocrine insufficiency
- increased blood glucose, development of diabetes.
If one or more of these signs are detected, it is recommended to consult a doctor. The specialist will assess the situation and prescribe further examination.
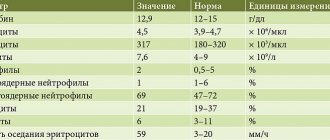
The diagnosis of chronic pancreatitis is established based on the combination of the clinical picture and the results of laboratory and instrumental studies. To diagnose chronic pancreatitis, laboratory tests : determining the level of leukocytes, inflammatory markers, pancreatic enzymes in the blood, urine and feces; as well as instrumental studies : ultrasound examination of the abdominal organs, if indicated - multislice computed tomography with intravenous bolus contrast, endoscopic ultrasonography, magnetic resonance imaging.
Conservative treatment of chronic pancreatitis consists of prescribing a special diet with the exception of fatty, fried, smoked, spicy foods and alcohol, pancreatic enzymes, proton pump inhibitors, painkillers, vitamins, etc.
The main indications for surgical treatment of chronic pancreatitis are the recurrent course of chronic pancreatitis, with frequent exacerbations and chronic pain syndrome, which significantly reduces the patient’s quality of life. In addition, one of the main indications for surgical treatment is the presence of post-necrotic cysts of the pancreas, the occurrence of jaundice, etc. The specialists of our center are proficient in the full range of operations on the pancreas, including laparoscopic methods.
At the Moscow Clinical Scientific and Practical Center named after. A.S. Loginova, treatment of chronic pancreatitis is carried out through the joint efforts of gastroenterologists , endocrinologists and surgeons . Do not delay your visit to the specialists of our Center. This will help to diagnose the disease in a timely manner and choose the right treatment tactics. Doctors of the State Budgetary Healthcare Institution MKSC named after A.S. Loginova DZM are always ready to help you.
Definition
The main insidiousness of the disease is its long asymptomatic course with periodic exacerbations (undulating course). Imperceptibly, the pancreas loses its functions. During exacerbations, the pathological process in the organ is activated.
As a result, the exocrine and intrasecretory functions of the organ suffer, and the parenchyma gradually becomes necrotic. If left untreated, the patient's condition becomes irreversible. In addition, the inflammatory process, as it progresses, affects neighboring organs, which threatens the development of dangerous complications.
The disease has a wide variety of forms and manifestations. In this regard, a rich classification of its types has been proposed.
Prohibited Products
Healthy carbohydrates
The list of foods prohibited for consumption in chronic pancreatitis is also quite large. Such products include:
- Any fried food, especially fish
- Fatty meats. Namely, the fatty part of pork and beef
- Eggs, namely scrambled eggs made from them. Sometimes in villages children, and even adults, are given a raw egg to drink. So, if a person has chronic pancreatitis, doing this is strictly prohibited
- Fatty soup, which is cooked in a very rich and boiled broth
- Fat cottage cheese and yoghurts
- Bread, especially wheat
- Legumes
- Cakes, pastries
- Margarine
- Alcohol. Even small amounts of alcohol are not allowed
- Dairy products, namely hard cheeses
Of course, it is very easy to eliminate some foods. Many people do this, remove certain dishes, but do not take any medications. So in this case, all actions will be in vain.
Causes
Chronic parenchymal pancreatitis is often an independent disease (primary form). Its main reason lies in external factors. But the disease can develop against the background of other pathologies. In this case, they speak of a secondary form of pancreatitis.
Primary pancreatitis is a common consequence of alcohol abuse (alcohol has a strong toxic effect on the parenchyma). Another common cause of a toxic type of pathology is the use of potent drugs such as corticosteroids, estrogens, and thiazide diuretics.
The cause of secondary pancreatitis is an advanced acute form of the disease. The condition of the pancreas can worsen if the functioning of various organs and systems is disrupted:
- disturbance of metabolic processes in the body (dysmetabolic pancreatitis);
- contact of a viral infection into an organ (viral pancreatitis);
- disruption of the autoimmune system or the release of antibodies in response to pancreatic cells (autoimmune pancreatitis);
- hereditary causes (genetically determined pancreatitis).
A common type of secondary parenchymal pancreatitis is biliary-dependent pancreatitis. It develops as a consequence of cholelithiasis, congenital defects of the biliary tract, spasm of the sphincter of Oddi, and blockage of the biliary tract with stones. If the outflow of bile is disrupted, it backflows into the glandular ducts. This leads to damage to the ducts and the onset of an inflammatory process in the gland.
Stages of the disease and complications
Vegetable soups are very healthy
Like any other disease, chronic pancreatitis has several stages of development, at each of which the symptoms will be different. Thus, it is customary to distinguish the initial and late stages.
- The initial stage of development of pancreatitis is characterized by the appearance of symptoms such as pain, which are localized in various areas, and diarrhea. This stage usually lasts from one to five years. It is during this period of time that the disease develops and causes harm to the body.
- The later stage is characterized by more serious symptoms, which are manifested by constant pain, constant stool disturbances, and digestive problems. This stage lasts from five to ten years.
In order to reduce the risk of chronic pancreatitis moving to a later stage, it is necessary to consult a doctor in time to avoid complications. Complications of chronic pancreatitis may be the following:
- Increased pressure in the biliary tract
- Formation of cysts in the pancreas
- Stagnation of bile, which is very dangerous
- Development of infectious diseases
- Development of bleeding
- Pleurisy
Depending on how advanced the disease was, complications will depend.
According to the nature of the flow
In the chronic form of pancreatitis, exacerbations have varying frequency and intensity. The classification according to this criterion is as follows:
- The parenchymal form itself is characterized by a long absence of symptoms, although the pathological process is actively developing. Treatment often begins late, which threatens to worsen the condition.
- The relapsing form is characterized by periodic recurrence of symptoms. The patient experiences severe pain and deterioration in general condition.
- If relapses occur quite often, then they speak of an indurative form of pancreatitis.
If treatment is incorrect or ineffective, the parenchymal tissue of the pancreas is replaced by non-functional fibrous tissue. This is an irreversible condition in which the organ gradually loses its functions.
Fibrous pancreatitis is a dangerous complication of the chronic form. Early diagnosis and adequate treatment help prevent its development.
Products recommended for consumption
During the diet, it is necessary to follow all the recommendations of the attending physician, since the patient’s health directly depends on this. So, a patient with chronic pancreatitis is recommended to include in the diet such foods as:
- Fish, and low-fat varieties. In addition, it is advisable to either steam it or simply boil it.
- Poultry, also steamed or simply boiled
- Eggs, and it is best to use them to make an omelet
- Fermented milk products, meaning cottage cheese and kefir, which contain a minimum of chemical additives. It should also be said that for pancreatitis it is better to purchase kefir without any flavoring additives
- Cereals, namely buckwheat, oatmeal, rice. Cereals can be used for simply cooking (when preparing a side dish) or you can cook porridge from them, which is very healthy for the stomach
- Vegetables, namely tomatoes, cucumbers, potatoes, broccoli
- Fruits, namely bananas, pears, strawberries, watermelon and others
- Marshmallows and marshmallows. These are exactly the sweets that people with chronic pancreatitis are allowed to eat. True, you need to eat them in moderation, in small quantities.
- Compotes
- Decoctions
Separately, it is necessary to say about the favorite drink of many people, this is coffee. In case of chronic pancreatitis, drinking coffee, even one cup per day, is prohibited.
Symptoms
The disease can occur in three morphological forms. Each has its own course and its own group of clinical signs. How the disease will proceed in this particular case depends on its causes, the state of the immune system, and concomitant pathologies.
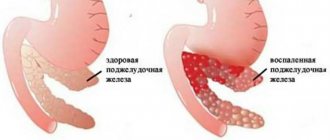
Edema form
Symptoms of pancreatic inflammation
In the edematous form, the pancreas is inflamed and significantly enlarged in size. This form is a common consequence of poor diet or abuse of low-quality alcohol.
The patient is accompanied by symptoms of severe intoxication. The first sign is a burning girdle pain, which is accompanied by dyspepsia (nausea, vomiting, unstable stool).
Conservative medical methods, without surgical intervention, are successfully used to treat the edematous form. The prognosis of the disease is favorable.
Sclerosing form
The sclerosing chronic form occurs against the background of obstruction (blockage) of the glandular ducts or other pathologies of the gastrointestinal tract. The parenchyma undergoes sclerotic transformation, the ducts significantly expand. The patient is in severe pain. This condition is complicated by polyuria and increased thirst, allergic manifestations on the skin are possible.
Calculous form
Calculous or biliary pancreatitis is the most severe. Stones are deposited in the glandular ducts of the organ, which threatens to completely close the lumen. In this case, the prognosis is much worse. The calculous form is also dangerous due to its transition to a malignant tumor process.
With this form of the disease, the patient’s body does not receive enough nutrients and vitamins, which causes severe loss of body weight. The patient feels a cutting pain in the left hypochondrium. The picture of the disease is complemented by symptoms of intoxication and weakness.
Diabetes mellitus often develops. Narrowing and obstruction of the ducts can provoke reverse reflux of bile, as evidenced by obstructive jaundice and a constant taste of bitterness.