Pancreatitis (pancreatitis - lat.) is an acute or chronic inflammatory disease of the pancreas, accompanied by its self-digestion and progressive tissue destruction (necrosis).
If pancreatitis , treatment with integral medicine methods includes:
1) anti-inflammatory therapy (to eliminate the inflammatory process)
2) restorative therapy (to restore pancreatic tissue at the cellular level).
The third component of the treatment of pancreatitis is the elimination of the cause that caused the disease - biliary dyskinesia, cholelithiasis, cholecystitis or another cause. As pancreatitis is treated using integral medicine methods, pain (pain in the left hypochondrium and upper abdomen) subsides, and other symptoms of pancreatitis gradually disappear. At the same time, the production of pancreatic enzymes (pancreatic juice) is normalized, digestion is improved, and the development of diabetes mellitus is prevented.
Symptoms of chronic pancreatitis
When diagnosed with pancreatitis, the symptoms depend on what type of disease occurs: acute pancreatitis, acute recurrent, chronic pancreatitis or exacerbation of chronic pancreatitis.
In addition, when pancreatitis is diagnosed, symptoms depend on the location of the inflammation. If the inflammatory process occurs in the head of the pancreas, pancreatitis is manifested by pain in the right upper abdomen, if in the body of the pancreas - in the upper abdomen on the left, and if the inflammatory process has affected the tail of the pancreas, pain is felt in the left hypochondrium. Widespread pancreatitis is manifested by girdle pain.
Acute pancreatitis has symptoms such as acute pain in the left hypochondrium and upper abdomen, acute pain in the left side above, in the upper abdomen on the right, girdle pain, nausea, vomiting, foamy mushy stools.
Symptoms of chronic pancreatitis are constant or paroxysmal pain in the left hypochondrium, pain in the left side above and in the epigastric region, pain in the upper abdomen on the right, girdle pain radiating to the back, belching, diarrhea, flatulence, rumbling in the abdomen, the appearance of red spots on chest, stomach and back.
Symptoms of exacerbation of chronic pancreatitis are of the same nature as the symptoms of acute pancreatitis .
Causes of abdominal pain
Acute pancreatitis
Inflammation of the pancreas is the main cause of abdominal pain.
A painful attack manifests itself suddenly, mainly after eating a large amount of fatty or spicy food. The pain is localized in the upper abdomen, radiating to the lower back and interscapular area. The pain is sharp, burning. Patients may describe it as a feeling of a tight belt. The pain syndrome is constantly present, intensifies in the supine position. Against the background of pain, repeated vomiting develops, which does not bring relief to the patient. Vomit contains bile. In addition to the girdle pain, discomfort is felt throughout the abdomen, which is caused by flatulence. Purulent pancreatitis is characterized by debilitating pain accompanied by high fever. With biliary pancreatitis, a painful attack is accompanied by jaundice of the skin and mucous membranes.
Chronic duodenitis
The presence of girdle pain is possible with a pancreatic-like variant of duodenitis. The pain is constant and is described by patients as sharp, burning or squeezing. They are provoked by errors in diet and alcohol consumption. The pain is localized in the upper abdomen like a belt. The pain radiates to the back, to the left shoulder blade. The pain syndrome is combined with dyspeptic disorders: nausea, diarrhea, flatulence.
Pancreatic abscess
The condition mainly occurs with pancreatitis. After 10-15 days from the onset of the disease, the intensity of the girdle pain intensifies, it takes on a paroxysmal or pulsating character. Pain in the abdomen worsens with the slightest movements, in a position on the left side and back. The symptom is accompanied by febrile or hectic fever, severe weakness, and increased sweating. Protective muscle tension is detected in the left hypochondrium.
Pancreatic necrosis
The sudden onset of unbearable girdling pain is a typical sign of organ destruction. The pain radiates to the left abdomen, interscapular region and left shoulder. The intensity of the pain attack depends on the degree of damage to the pancreas. In 70% of cases, pain occurs after an episode of poor diet and alcohol abuse. Within a few days, the pain decreases, which indicates the death of the nerve endings.
A couple of hours after the onset of pain, uncontrollable vomiting begins, containing streaks of blood and bile. There is retention of stool and gases. The general condition of the person is serious or extremely serious; there may be hemodynamic disturbances. According to the clinical picture, pancreatic necrosis resembles the abdominal form of myocardial infarction and requires differential diagnosis.
Girdle pain in the abdomen
Pancreas cancer
Malignant tumors initially manifest themselves as constant dull pain in the left upper quadrant of the abdomen, but as the tumor grows, the pain syndrome becomes encircling in nature. Irradiation of pain to the back and lower back is typical. Pancreatic pain increases sharply when the body bends forward and to the left. With malignant degeneration of an organ, patients quickly lose weight, up to anorexia and cachexia.
Diaphragmatic hernia
The occurrence of girdle pain in the upper abdomen occurs with 2-3 degrees of hiatal hernia. The pain syndrome has a burning or squeezing character. Patients report that pain bothers them after eating, during intense physical activity or straining. To reduce abdominal pain, a person takes a vertical position, takes deep breaths, and induces vomiting. Excruciating girdle pain is observed when a hernia is strangulated.
Intercostal neuralgia
Abdominal pain of a girdle nature develops with damage to the nerves passing in the 10-11 intercostal spaces, as well as with pathology of the subcostal nerves. Patients report that the pain spreads in a circle from the spine to the sternum. For such girdling pain, a sudden onset is typical, lasting from a few seconds to 3-5 minutes. During an attack, a person freezes and holds his breath.
Complications of pharmacotherapy
Girdle pain in the abdomen is characteristic of drug-induced pancreatitis. To alleviate the attack, patients take a forced position: lie on their side, pulling their knees to their chest. Soreness is accompanied by dyspepsia and weakness. Drug-induced pancreatitis can occur during treatment with certain antibiotics, antiretroviral drugs, cytostatics and corticosteroids.
Chronic pancreatitis. Pain in left side
Of all the symptoms of pancreatitis, the most characteristic and typical is pain. However, pain in the left side does not necessarily indicate pancreatitis.
Thus, pain in the left side and hypochondrium may be associated with a disease of the spleen, in which it enlarges and stretches the fibrous capsule. Another cause of pain in the left side and upper abdomen can be gastritis.
However, pain in the left side is highly likely to indicate pancreatitis, especially if it radiates to the back and under the shoulder blade. Therefore, if you are experiencing pain in the left hypochondrium or pain in the upper left side, it is necessary to undergo diagnostics as soon as possible in order to find out the cause of the pain and undergo appropriate treatment to avoid complications of pancreatitis.
Acute pancreatitis and chronic pancreatitis
There are two main types of the disease - acute pancreatitis and chronic pancreatitis . In most cases, acute pancreatitis occurs due to alcohol abuse, cholelithiasis (up to 30% of cases), as well as due to poisoning (intoxication), viral disease or surgery on the gastrointestinal tract. Acute pancreatitis can also occur as an exacerbation of chronic pancreatitis .
In turn, without proper treatment, acute pancreatitis can develop into chronic pancreatitis . However, chronic pancreatitis can also occur as an independent disease, without a preliminary acute phase. In this case, the causes of chronic pancreatitis can be, first of all, diseases of the biliary tract - cholecystitis (inflammation of the gallbladder), biliary dyskinesia, cholelithiasis.
As a result of these diseases, part of the bile is thrown into the pancreas, preventing the outflow of pancreatic juice, stagnation of pancreatic juice occurs and self-digestion of the pancreas begins, which leads to its inflammation.
In such cases, we speak of reactive pancreatitis, which often develops against the background of cholecystitis (cholecystopancreatitis). Factors contributing to the development of the disease are abuse of alcoholic beverages, spicy, fatty and fried foods, as well as nervous stress.
Nervous stress plays a special role in the development of chronic pancreatitis, as it causes spasms of the bile and pancreatic ducts and, as a consequence, stagnation of pancreatic juice and progressive inflammation of the pancreas - chronic pancreatitis.
The danger of chronic pancreatitis is that as the pancreas self-digests, its cells are destroyed, which leads to a decrease in the production of digestive enzymes, as well as the hormone insulin, which can cause the development of diabetes. In addition, chronic pancreatitis is fraught with sudden exacerbation, which poses an immediate threat to life and requires immediate hospitalization.
Content:
- Why is pancreatitis dangerous?
- Causes
- Manifestation
- Diagnosis of pancreatitis
- Treatment of exacerbations of pancreatitis
Why is pancreatitis dangerous?
Chronic pancreatitis is a progressive inflammatory disease of the pancreas, which can be caused by various etiological factors, but in the final stage it always leads to the development of exocrine and endocrine insufficiency of the gland. Early complications of pancreatitis include subhepatic jaundice syndrome, abscesses, cysts and pseudocysts, pleurisy and pneumonia, as well as gastrointestinal bleeding, and late complications are the actual consequences of insufficient secretion of pancreatic enzymes and hormones.
Causes
The pancreas is an endocrine and exocrine gland; it produces digestive enzymes, biologically active molecules that regulate the digestion process, as well as the hormones insulin and glucagon, which regulate blood glucose levels. Among the most common causes of inflammation of the pancreas are alcohol intoxication, various diseases of the biliary tract and the area of the major duodenal papilla (the ducts of the pancreas and bile ducts flow into it). There are two main types of chronic inflammation of the gland - obstructive and calcifying. The first option is due to the fact that one or another obstacle (obstruction) is formed in the path of the outflow of pancreatic secretions - in case of cholelithiasis, injuries, developmental anomalies, or damage to the place where the duct enters the duodenum (DDS). Calcifying pancreatitis develops with alcohol abuse, hereditary pathologies, or hyperparathyroidism, when calcium deposits impair the flow of pancreatic juice into the ducts. Due to the fact that the pancreas produces enzymes capable of digesting proteins and fats, as a result of a disruption in the flow of pancreatic juice into the duodenum, its components from high pressure in the ducts begin to flow and become activated in the tissues of the gland itself, “self-digestion” (necrosis) occurs. , chemical damage to the pancreas.
Manifestation
The clinical picture of exacerbation of chronic pancreatitis includes three main symptom complexes:
- inflammatory-destructive syndrome, which is caused by the actual necrosis of part of the gland - pain in the left hypochondrium of a girdle nature, signs of intoxication (fever, joint pain, weakness, loss of appetite), yellowness of the skin and mucous membranes;
- syndrome of impaired external secretion: steato- and creatorrhea - frequent loose stools with a high content of undigested fats and elastic fibers, pain and bloating in the abdomen, nausea, rapid satiety, hypovitaminosis, deterioration of the skin and nails, weight loss;
- insufficiency syndrome: decreased insulin levels with the development of carbohydrate intolerance or diabetes mellitus.
Diagnosis of pancreatitis
The diagnosis and treatment of chronic pancreatitis is carried out by general practitioners, gastroenterologists, and, if there are indications for surgery, by surgeons.
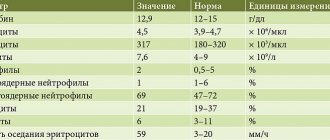
At the first stage of diagnosis, complaints and medical history are collected. The nature of the pain syndrome and its location may indicate the lesion: if the tail of the pancreas is affected, pain occurs in the left hypochondrium, if the body is affected - in the epigastrium, above the navel, if the head is affected - in the right hypochondrium. Girdle pains that spread from the hypochondrium to the back indicate total defeat. The pain can be paroxysmal, constant or combined. During an exacerbation of chronic recurrent pancreatitis, the pain is sharp, cutting, as in an acute attack, but resolves on its own, and in the chronic painful version, it is constant aching. Diarrhea during exacerbation of pancreatitis usually turns into constipation when inflammation subsides. A physical examination may reveal a rash on the skin of the chest and abdomen, pain on palpation of the pancreas area, and positive symptoms of irritation. The decisive stage in the diagnosis of pancreatitis is a laboratory and instrumental examination. In a general clinical blood test, signs of inflammation are noted, but the increase in pancreatic enzymes in the biochemical analysis of blood and urine (amylase, lipase) is of particular importance. When examining stool, a high content of undigested muscle fibers and fats (steato and creatorrhea) is detected; a decrease in elastase-1 is of great diagnostic importance. When performing duodenal intubation, stimulation of external secretion is used - secretin-pancreozymin test (if the exocrine function is impaired, the volume of secretion and the number of enzymes decreases). Intrasecretory function is assessed using a glucose tolerance test, insulin or c-peptide levels. Instrumental methods include ultrasound, CT or MRI, as well as retrograde cholangiopancreatography.
Treatment of exacerbations of pancreatitis
Treatment of exacerbations is aimed at suppressing pancreatic secretion, reducing gastric acid production, direct suppression of secretion, stopping enzyme autoactivation and correcting intoxication. Patients are advised to fast, gastric contents are evacuated, and medications are prescribed (proton pump inhibitors, histamine receptor blockers, antacids, somatostatin, octreotide, enzyme inhibitors, and others). Severe exacerbation is an indication for hospitalization. In the remission phase, it is recommended to follow a diet, avoid alcohol, and enzymatic preparations and painkillers can be used.
Treatment of chronic pancreatitis
When pancreatitis is diagnosed, treatment using integral medicine methods is complex and is carried out taking into account all factors in the development of the disease.
Treatment of pancreatitis includes reflexology methods on the bioactive points of the meridians of the pancreas, liver and gallbladder using acupuncture and acupressure.
The most important part of the treatment of pancreatitis is herbal medicine. used to treat pancreatitis have an anti-inflammatory effect, improve the functions of the pancreas and biliary tract, normalize the production and flow of bile, as well as the enzymatic activity of the pancreas (production of pancreatic enzymes), promote the restoration of pancreatic tissue at the cellular level and eliminate the inflammatory process.
Treatment
Help before diagnosis
In most cases, the appearance of girdle pain is a sign of a serious pathology of the digestive system, so self-medication is unacceptable. The patient should seek medical help as soon as possible. Before the doctor arrives, you should not take painkillers or other medications, so as not to blur the clinical picture. To alleviate the patient's condition before identifying the causes of the pain syndrome, doctors can use analgesics and infusion therapy.
Conservative therapy
Treatment is carried out in a hospital setting. In the acute period, strict bed rest is recommended; after the condition improves, the restrictions are removed. A diet and ice on the area of the pancreas projection are indicated. For all forms of pancreatitis, therapy is aimed at relieving pain, for which antispasmodics and novocaine blockades are prescribed. For diseases that are accompanied by abdominal pain, the following groups of drugs are effective:
- Antibiotics
. They are used as etiotropic treatment for pancreatic abscess, for the prevention of purulent complications in pancreatic necrosis. - Infusion therapy
. Intravenous administration of electrolyte and protein solutions is necessary for detoxification of the body. - Enzyme inhibitors
. The drugs neutralize the damaging effects of pancreatic enzymes, which are released into the blood in large quantities. - Anti-inflammatory drugs
. Used for intercostal neuralgia to relieve pain.
Diet for chronic pancreatitis
If chronic pancreatitis , treatment will be more successful the more strictly the diet is followed. The diet for pancreatitis is prescribed individually and at the same time includes a number of general rules.
In particular, a diet for pancreatitis involves avoiding alcoholic beverages, rich meat and fish broths, fatty meats, spicy, sour and fried foods, strong coffee and tea.
You can learn more about the integral method of treating chronic pancreatitis at CONSULTATION.
Detailed information by phone: (495) 789-41-53.
We are ready to answer your questions from 9:00 to 21:00, seven days a week. Call!