The first symptoms of erosive antral gastritis, treatment regimen and prevention
Gastritis is an inflammatory disease of the stomach. The term antral refers to the location of this disease. Therefore, the source of the disease is in the last lower part of the stomach, called the antrum. And the term erosive indicates the presence of erosions and ulcers.
Thus, erosive antral gastritis is an inflammatory disease of the lower stomach, accompanied by the formation of erosions and ulcers. One of the causes of the disease is considered to be infection of the stomach by Helicobacter pylori bacteria. When it enters the stomach, the colony of these bacteria grows. Their waste products cause intoxication of the mucous membrane and lead to its thinning.
What it is?
Erosive gastritis or erosive-ulcerative gastritis is one of the forms of the inflammatory process in the gastric mucosa, which results in the formation of small surface defects in the form of erosions.
The erosive type differs from other types of gastritis by the appearance of extensive erosive areas against the background of an inflamed, reddened surface. Such damage sometimes covers the entire gastric surface. The development of erosive gastritis of the stomach begins with the formation of small wounds on the outer surface of the stomach and gradually covers a larger and larger area.
Candidate of Medical Sciences, Associate Professor Bedelbaeva G.G., Doctor of Medical Sciences, Prof. Turlanov K.M.,
Doctor of Medical Sciences, Prof. Izatullaev E.A., Doctor of Medical Sciences Tashenova L.K., Gridin I.O.
Department of LUTS, internal diseases No. 2 of the Kazakh National Medical University named after. S.D. Asfendiyarova, Kazakhstan
Modern ideas about erosive lesions of the stomach and duodenum
Erosive damage to the mucous membrane of the stomach and duodenum (duodenum) is one of the most frequently detected pathologies of the gastroduodenal zone (GDZ). This is a superficial defect in the mucous membrane of the stomach and duodenum, which does not penetrate the muscle layer and heals without scar formation. It is found in 2-15% of patients undergoing endoscopic examination. Erosion was first described by Morgagni in 1756. However, the opportunity to study erosions in detail appeared only after the introduction of endoscopic diagnostic methods into gastroenterological practice.
Currently, interest in the problem of erosive damage to the mucous membrane of the stomach and duodenum has increased significantly. This is due to the prevalence of this disease among people of working age. Severe, often profuse bleeding, the source of which was erosion, has been described; often the source of bleeding is erosion, even in patients with concomitant peptic ulcer disease (PU).
In most cases, a violation of the integrity of the mucous membrane is a consequence of a violation of the normally existing balance between the factors of aggression and defense. This thesis also applies to erosive lesions.
Erosive lesions occur as a result of stressful circumstances (surgery, trauma, etc.) and are often found in people who abuse hot, rough, spicy foods, coffee, and smokers. They complicate the course of various diseases (liver, kidneys, pancreas, heart, lungs, etc.), especially when they are decompensated. The appearance of erosions is often associated with the intake of alcohol and medications (corticosteroids, potassium chloride, non-steroidal anti-inflammatory drugs, etc.), with exposure of the mucous membrane to corrosive substances (acids, alkalis, etc.).
The question of the role of Helicobacter pylori in the occurrence of gastric erosions, whose aggressive effect on the mucous membrane has been objectively proven, is controversial. The frequency of detection of Helicobacter pylori in biopsies of the mucous membrane depends on the nature of the pathological process and, according to some data, ranges from 15 to 94.4% in patients with erosions. Studies have also shown that such patients often have antibodies to Helicobacter pylori, as well as sensitization of lymphocytes to the antigens of these bacteria.
Acid-peptic aggression is also considered an important factor in the formation of chronic erosions. However, in recent years, scientists have tended to believe that a high level of gastric acidity turns into a damaging factor only when the protective ability of the mucous membrane decreases. At the level of cell population kinetics, these factors are manifested by a change in the balance between cell formation and cell death. Consequently, an erosive defect in CO can occur even with normal or increased proliferation, if the processes of cell rejection increase to a greater extent.
More often there are works devoted to the pathogenetic role of disturbances in prostaglandin metabolism in the occurrence of erosions of the gastrointestinal tract. In particular, it is assumed that the decrease in the content of prostaglandins in the area of the erosive defect is due to the blocking of the key enzyme of prostaglandin biosynthesis, cyclooxygenase, by lipoperoxides.
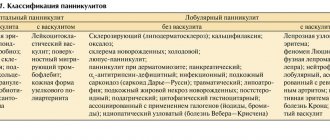
There are several classifications of erosions, which in most cases are based on the endoscopic picture. The most common is the classification proposed by V. Vodolagin (1996). According to this classification, a distinction is made between primary erosive defects, which are an independent pathology, and secondary ones, accompanying the underlying disease (severe damage to the liver, kidneys, cardiovascular system, etc.). In addition, erosions are distinguished as a manifestation of a malignant or systemic process in the gastric mucosa (malignant erosions in cancer, Crohn's disease, etc.). Benign erosions are divided into acute (hemorrhagic), chronic single and multiple, chronic erosive (lymphocytic) gastritis, erosive-hemorrhagic gastritis and duodenitis. Acute (superficial, flat, hemorrhagic, “incomplete”) erosions are superficial defects of various shapes and sizes, covered with blood, hemorrhagic and fibrinous plaque against the background of altered or unchanged mucous membrane. They are often multiple and localized mainly in the body and subcardial part of the stomach. Acute erosions epithelialize quickly (within 2-14 days), without leaving any significant (macroscopic) traces; sometimes in their place an area of mucosal hyperemia may remain. The main distinguishing feature for chronic (“complete”, elevated, varioliform) erosions is the presence of a polypoid formation with a diameter of 3-8 mm, at the top of which there is an area of eroded CO with an umbilical depression in its center. The bottom of the defect is made of fibrin or hydrochloric acid hematin and a thin unstable layer of granulation tissue. Around such erosions there are hyperplastic, elongated and convoluted gastric pits.
Chronic erosions are characterized by the presence of a highly prismatic, intensively mucus-producing epithelium of the marginal zone. At the same time, a network of subepithelial vessels is developed, and there is an elongation of the cervical parts of the gastric glands. The muscular plate is intact or hyperplastic. In the zone of chronic erosion, there is an alternation of large areas of fibrosis, cystic expansion of the gastric glands, solitary follicles and intense mixed polymorphic cellular infiltration of the mucous membrane.
Chronic erosions exist for a long time (from 4 weeks to several years). Based on the nature of histological changes, this type of erosion can also be divided into “mature” and “immature”. In the first case, chronic erosion is epithelialized, and the swelling of the mucous membrane remaining in its place completely disappears; in the second case, the bulging remains due to developed tissue fibrosis and pronounced productive inflammation.
It was believed that the clinical picture of erosive lesions corresponds to that of ulcerative disease and is not specific. However, if PU is accompanied by erosion, then the pain syndrome is particularly intense and persistent; in some patients it cannot be stopped even with treatment for 1.5-2 months. The exacerbation is more protracted than in patients with ulcer alone. Very often, the erosive process occurs under the guise of the disease against which it developed (cholecystitis, gastritis, etc.). In some cases, erosion lesions of the gastrointestinal tract are asymptomatic.
All complaints made by patients with erosive lesions of the gastrointestinal tract can be reduced to the following syndromes: ulcer-like, in which the pain syndrome is clearly associated with food intake, night, “hungry” pain often occurs, dyskinesia develops early, and the healing time is relatively prolonged; dyspeptic; without specific symptoms from the stomach and duodenum; hemorrhagic (clinically manifested by anemia and a positive reaction to occult blood in the stool). In some cases, in patients with peptic ulcer disease, the next exacerbation with a characteristic clinical picture is accompanied by the absence of a peptic ulcer, but there is hyperemia, swelling and erosion of the mucous membrane. Therefore, erosions should be regarded as a manifestation of disease activity.
The clinical course of the disease in the case of “complete” erosions has some features. The symptoms are scant: often heartburn, belching of air; rarely moderately severe fasting and early pain in the epigastric region after eating. Most chronic erosions generally proceed latently.
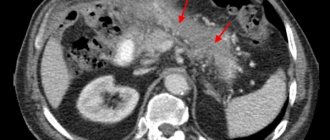
The leading method for diagnosing GDZ erosions is the endoscopic method, which makes it possible to distinguish two main types of erosions. Erosion of the stomach must be differentiated from the erosive-ulcerative form of cancer; for this purpose, a biopsy is necessarily performed, followed by a morphological assessment. Studies aimed at detecting Helicobacter pylori (Hp) using a urease test or other methods are also advisable.
Chronic erosions, unlike acute ones, can exist for a long time (weeks, months, in some cases even years). Their outcome may be the appearance of focal hyperplasia followed by the development of hyperplastic polyps. The possibility of malignancy of this type of erosion cannot be excluded.
Literature:
1. Maev I.V., Kucheryavyi Yu.A., Gadzhieva M.G. New approaches to the diagnosis and treatment of chronic gastric erosions // Russian Journal of Gastroenterology, Hepatology, Coloproctology, 2003, No. 1, pp. 43-49.
2. Vodolagin V.D., Lebedev S.P., Tsodikov G.V. Clinical and morphological criteria for chronic gastric erosions // Therapeutic archive, 1983, T.55, No. 4, pp. 123-125.
3. Zimmerman Ya.S., Vedernikov V.E. Chronic gastroduodenal erosions: clinical and pathogenetic characteristics, classification, differentiated treatment // Clinical Medicine, 2001, No. 6, pp. 30-36.
4. Demirturk L., Yazgan Y., Izci O. et al. The effect of Helicobacter pylori eradication on gastric juice and blood ammonia concentrations and on visually evoked potentials in cirrhotics// Helicobacter. – 2001. – V. 6, No. 4. – P. 325–330.
Causes
The etiology of this disease is quite well studied. The formation of erosions occurs as a result of the pathological effect of gastric juice on the mucous membrane. If this process is not stopped, ulcers may develop, which are dangerous due to their perforation.
Gastritis of the antrum of the stomach can develop in the presence of the following predisposing factors:
- the bacterium Helicobacter pylori is the most common etiological factor, up to 85% of cases of erosive antral gastritis;
- infectious or inflammatory disease in the gastrointestinal tract;
- gastroenteritis;
- poisoning with toxic substances;
- previous gastric surgery;
- unhealthy diet – abuse of fatty, spicy and fried foods;
- alcoholism, smoking;
- long-term use of medications that violate the integrity of the gastric mucosa.
According to statistics, the bacteria Helicobacter pylori and poor nutrition most often lead to the development of this disease.
STOMACH EROSION
STOMACH EROSION
(Latin erosio corrosion) is a superficial defect of the gastric mucosa that does not reach the muscular plate and heals without scar formation.
It was first described by G. Morgagni in 1756.
Karvonen (AL Karvonen, 1981) during endoscopy of the stomach revealed erosions in 10.5% of patients. Martinoli and Gantner (E, Martinoli, J. Gantner, 1970) on sectional material found acute erosions in the stomach and duodenum in 6.1% of all autopsy cases.
In most existing classifications of gastric erosions, depending on the characteristics of the course and morphological signs, it is customary to divide them into acute and chronic. V. X. Vasilenko and his colleagues (1978) also include in the concept of “stomach erosion” defects of the mucous membrane that occur as a result of malignant or systemic pathological processes (stomach cancer, gastric lymphoma, Crohn’s disease, etc.), however, this opinion is not shared by all researchers .
Etiology and pathogenesis
gastric erosions have not been studied enough. They are often diagnosed in shock, burns, sepsis, after various operations (so-called stress injuries). The occurrence of gastric erosion may be associated with taking medications (acetylsalicylic acid, brufen, indomethacin, corticosteroids, etc.). Sometimes erosive lesions of the stomach (usually the antrum) can be an early stage of peptic ulcer (see). Often, gastric erosions accompany colon tumors, chronic liver diseases, diseases of the cardiovascular system, respiratory system, and blood (secondary erosions). Thus, erosions are a heterogeneous lesion of the gastric mucosa and are the result of its uniform reaction to various (general or local) pathological influences.
According to modern concepts, ischemia of the gastric mucosa, which occurs as a result of various pathological influences and leads to an increase in its permeability, is of primary importance in the development of gastric erosion. Due to impaired permeability of the gastric mucosa, reverse diffusion of hydrogen ions increases, which contributes to the release of histamine and pepsin, the occurrence of edema of the mucous membrane, and increased capillary permeability. The result of these changes is damage such as erosions and ulcers. There is an assumption that increased secretion of hydrochloric acid and pepsin, bile reflux (see Reflux), as well as increased autoimmune processes contribute to the transition of the process to chronic.
Pathological picture
. Gastric erosion is a small (up to 10-15 mm in diameter) defect of the gastric mucosa of a round, jagged or triangular shape that does not reach the muscular plate. Erosion of the stomach can be single (1-3) or multiple (more than three in different parts of the stomach). Damage to the mucous membrane of the entire stomach or most of it is classified as erosive-hemorrhagic gastritis.
Acute erosions are often located in the fundus and body of the stomach. They are characterized by the absence of surface epithelium; in the area of the bottom of the defect - moderate infiltration of lymphocytes and fibrin overlay; in the area of the edges - flattening of epithelial cells and hyperchromicity of their nuclei, the presence of a large amount of DNA in the nuclei.
Chronic erosions are most often localized in the antrum (pyloric cave, T.) of the stomach. Histological examination reveals granulation tissue, dilation of blood vessels in the bottom area, dystrophic changes and atrophy of the pyloric glands in the area of the bottom and edges of erosion, as well as focal hyperplasia of the surface epithelium in the area of its edges. In addition, in the zone of acute and chronic erosions, there is a pronounced cellular reaction of the lamina propria of the mucous membrane, predominantly of a lymphoplasmic nature. With erosive-hemorrhagic gastritis in the mucous membrane, along with erosions, multiple hemorrhages with rejection of the surface epithelium are noted.
Clinical picture
gastric erosion often manifests itself as ulcer-like or hemorrhagic syndromes. An ulcer-like syndrome can be observed in individuals with acute or chronic erosions. Patients are concerned about pain in the epigastric region associated with eating, sometimes “hungry”, nausea, belching, heartburn. Hemorrhagic syndrome is observed more often in patients with acute erosions and erosive-hemorrhagic gastritis, manifested by gastric bleeding and posthemorrhagic anemia (see). The process is often asymptomatic; with secondary erosions, the symptoms of the underlying disease may predominate.
Diagnosis.
The leading diagnostic method is gastroscopy (see). During endoscopic examination, acute erosions are superficial defects of the mucous membrane (flat erosions), covered with blood, hemorrhagic or fibrinous plaque. After 2-4 weeks, they are completely healed by epithelialization without scar formation. In some cases, acute erosions become chronic. Chronic erosions look like small bulges with a deepening in the erosion). Their outcome is focal hyperplasia of the mucous membrane, sometimes polyps (see Stomach, tumors). The question of the transition of chronic gastric erosions to a chronic ulcer or cancer remains controversial. To exclude a malignant tumor of the stomach with infiltration, hyperemia, or changes in the relief of the gastric mucosa around the erosion, a targeted biopsy is performed.
If gastric erosion is detected, it is necessary to conduct a comprehensive examination of the patient and monitor him in order to timely identify the underlying disease (usually colon tumors, chronic liver diseases).
Treatment
similar to the treatment of peptic ulcer (see). Patients are prescribed an appropriate regimen, a gentle diet, antacids (calcium salts, magnesium, almagel), enveloping agents (bismuth preparations, etc.); anticholinergics (atropine), as well as metronidazole (see), which promotes the healing of defects in the gastric mucosa. The antipsychotic dogmatil (sulpiride, eglonil), the H2-histamine blocker cimetidine (belomet, tagamet), as well as gastrozepine, which reduces the secretion of gastric juice, have a good effect.
For gastric erosions occurring with hemorrhagic syndrome, which is more common in acute gastric erosions, treatment in the surgical department of a hospital is indicated. Patients are transfused with blood and plasma, aminocaproic acid and fibrinogen are administered intravenously, Vicasol is administered intramuscularly, and the stomach is washed with cold water or a cold isotonic sodium chloride solution. If conservative treatment is ineffective, gastroscopy is used to perform diathermocoagulation (see) or laser photocoagulation of bleeding vessels. In case of severe bleeding, sometimes they resort to surgical intervention, including gastric resection (see Stomach, operations). For chronic erosions, in case of ineffectiveness of other means and due to the possibility of polyp formation, diathermocoagulation is used.
Forecast
, as a rule, favorable; in patients with secondary erosions, it depends on the underlying disease.
Prevention
the same as for peptic ulcer disease: rational nutrition, gentle regimen, exclusion of alcohol and smoking. In order to prevent relapses, the patient is monitored for 2-3 years.
Bibliography:
Vasilenko V. X. and Grebenev A. L. Diseases of the husk and duodenum, p. 65, M., 1981; Struchkov V.I. et al. Gastrointestinal bleeding and fibro-endoscopy, p. 154, M., 1977; Atlas of diseases of the upper gastrointestinal tract, ed. by R. Ottenjann a. K. Elster, Philadelphia, 1980; P ranzin G. ao Chronic erosions of the stomach, Endoscopy, v. 16, p. 1, 1984; R o es with h W. Erosions of the upper gastrointestinal tract, Clin^ Gastroent., v. 7, p. 623, 1978.
V. D. Vodolagin.
Symptoms of antral erosive gastritis
Among the signs of antral erosive gastritis are the following:
- Sharp pain in the abdomen;
- Periodic pain in the lower abdomen, especially after eating;
- Feeling of tightness in the stomach area;
- Increased secretion of gastric juice;
- Belching;
- Heartburn;
- Vomiting, nausea.
With chronic erosive antrum gastritis, the symptoms are more muted or absent altogether. Possible signs:
- belching;
- flatulence;
- unpleasant sensation or dull pain in the epigastrium;
- prostration;
- heaviness in the stomach;
- diarrhea;
- heavy sweating.
To diagnose the disease, you will need to undergo: x-ray of the stomach, gastrofibroscopy, targeted biopsy.
Diagnostics
To determine the type of gastritis, the first step is endoscopy. Then blood and stool tests are mandatory. When diagnosis is difficult, X-ray examination is sometimes used.
Diagnosis of gastritis should only be carried out by a gastroenterologist. You cannot independently diagnose yourself or someone else, unless, of course, you have special education. Self-medication and self-diagnosis without medical education often leads to deaths.
Description
Hemorrhoidal gastritis is an inflammation that affects the mucous membrane in the stomach. At the initial stage, microcirculatory vascular dysfunction occurs in the near-surface layer, which leads to hemorrhages of blood-soaked mucous tissues or thrombosis of small vessels. The mucous membrane becomes inflamed due to hemorrhagic changes occurring and disruption of the blood supply to the tissues. Infiltration of leukocytes occurs with the formation of small near-surface hemorrhages. They can be single or multiple.
Hemorrhagic gastritis is often accompanied by gastric bleeding of varying intensity due to the pathological weakness of the blood vessels. When defects are localized on the anterior, posterior wall, or fundus of the stomach, the risk of bleeding is minimal. When the area of the lesser curvature with large vessels is affected, bleeding develops more often. The muscle tissue is not affected, so superficial hemorrhages with proper treatment tend to heal without scarring. Hemorrhagic gastritis occurs in acute or chronic form. Hemorrhagic gastropathy does not depend on the secretory activity of the digestive organ. Predisposing factors:
- Uncontrolled use of non-steroidal anti-inflammatory drugs.
- Any viral infections.
- Severe stress.
- Mechanical internal irritation of the stomach.
- Crohn's disease is a granulomatous inflammation of the gastrointestinal tract.
- Any blood lesions.
Return to contents
How to treat erosive antral gastritis?
Therapeutic measures to combat erosive antral gastritis are aimed at:
- stopping the activity of pathogenic bacteria;
- elimination of inflammation processes;
- relief from pain syndrome;
- stopping bleeding;
- reduction of acid levels and restoration of enzyme composition.
The most effective is a two-stage treatment aimed at combating pathogens and restoring damaged tissue structures:
- At the first stage, therapy with potent medications is used.
- The second stage of treatment is aimed at restoring tissues affected by erosions.
The duration of the therapeutic course is two weeks. Antibacterial drugs are used, as well as antacid drugs, which help reduce the acidic effect on the affected gastric mucous membranes.
Severe disease is treated by intravenous administration of antacids in liquid form. Painful sensations are relieved with analgesics.
Diet is important in successfully getting rid of the disease: preference should be given to low-fat foods that should be consumed warm. This therapy will help avoid worsening the inflammation process.
Drug therapy
Drugs to improve gastric motor function A number of well-known experts have recommended a special method for the treatment of erosive gastritis, approved by WHO. The duration of this course of therapy is 14-15 days. Aggressive treatment is carried out with proton pump inhibitors, histamine receptor blockers and prokinetics. In the first stage, a triple regimen is used, consisting of one drug such as a proton pump inhibitor and two antibacterial substances: amoxicillin and clarithromycin.
If the first regimen does not radically change the situation, then a course of therapy is prescribed according to the second regimen, which includes a complex of 4 drugs: bismuth dicitrate, proton pump inhibitor, tetracycline and metronidazole. Antisecretory drugs and antacids reduce the activity of oxidized gastric juice, reduce total acidity and stop tissue erosion and erosion of the mucous membrane. The drugs Maalox, Almagel, Gelusil, Renicidin, Omeprazole, Gaviscon and some others have shown sufficient effectiveness in this direction. Digestion can be stabilized by using enzyme-type products: mezim, festal, panzinorm, etc.
For patients with a severe stage of the disease, intravenous administration of liquid antacids and blockers such as cimetidine, famotidine is provided; blood replacement drugs are used. Painful symptoms of a spasmodic nature are relieved with the help of antispasmodics: no-shpa, papaverine.
Stages of esophageal erosion
09.10.2021
Indications for esophageal begin with symptoms of heartburn . With proper treatment and care, the next stage of erosion can be avoided. Otherwise, erosion of the esophagus can cause serious health problems.
Esophageal erosion refers to the gradual destruction of the esophagus , the tube that carries food from the mouth and into the stomach . Although it sounds quite simple, it is not. The point is not that food, when swallowed, simply falls from the esophagus into the stomach . When food reaches the esophagus from the mouth , a series of muscle movements gradually transfer the food to the stomach . It is always recommended to eat food slowly, chew properly and swallow slowly.
How and why does esophageal erosion occur?
In most cases, wear and tear on the esophagus is caused by digestive problems. The most common digestive problem is gastroesophageal reflux disease ( GERD ). In this condition, the contents of the stomach back up into the esophagus because the valve that closes the opening between the esophagus and the stomach does not function or close properly. This constant accumulation of gastric acid in the esophagus causes damage to the esophagus , resulting in persistent erosion of the esophageal . This erosion causes many problems.
Gastric juice
The acid present in the stomach is mainly responsible for the digestion of food. To protect the stomach from this acid, nature creates a special lining for the stomach . This gives an idea of how strong stomach acid actually is. Now that this acid penetrates the esophagus , which does not have the luxury of a special lining, one can imagine the destruction it will cause to the esophagus . When this happens rarely, it is tolerable, but when it becomes a daily occurrence, the esophageal gives way and begins to collapse.
Causes of GERD
Dysfunction of the muscles of the lower esophageal . The opening of the esophagus to the stomach is protected by a set of muscles that act as a covering. Its main function is to prevent food from entering the stomach into the food tube. When this valve weakens, food from the stomach passes freely back into the esophagus , causing serious problems.
Other reasons:
- Improper stomach
- Abnormalities of the esophagus
- Hiatal hernia
- Genetic problems
- Diabetes
- Gastrointestinal disorders
- Lymphomas
Stages of esophageal erosion
Inflammation. In the initial stages, when stomach acid begins to flow into the esophagus , the result is swelling of the esophagus . The lining of the esophagus becomes red and bruised, causing a burning sensation in some parts or along the entire length of the esophagus . This condition is called acid indigestion or heartburn .
Stricture. Swelling of the esophagus can cause the lining of the esophagus . This tumor narrows the passage of the esophagus , making it difficult to swallow food and even saliva. This swelling can occur anywhere in the esophagus .
Ulcers . In addition, the constant presence of gastric juice in the digestive tract leads to ulcers. This usually occurs at the base of the food tube, which always takes the first hit and therefore suffers the most.
Bleeding. The next stage is bleeding from bruises of the esophagus . When blood in the victim's stool or vomit, this is a dangerous sign.
Published in Gastroentorology Premium Clinic
Folk remedies
Traditional medicine can be a good help for drug therapy in restoring tissue and normalizing stomach functions, but if used correctly. It is best if folk remedies are agreed upon with your doctor. The following folk methods are widely used:
- Potato juice is taken 3 times a day before meals, and the dose is gradually increased from 25 ml to 100 ml, the course of treatment is 15 days.
- Sea buckthorn in the form of berries.
- Sea buckthorn oil is taken 3 times a day, 1 tbsp. l.
- Cabbage juice is taken 100 ml 3 times a day for 20-30 days.
- A mixture of flaxseeds with water (2 tablespoons per 0.5 liters of water), consumed 60-70 ml 3-4 times a day before meals for 15-25 days.
- Honey can be used separately or added to any composition.
- Sea buckthorn infusion: the berries are poured with boiling water (in a ratio of 1:5) and infused for 2 hours, honey is added to the cooled composition, and drunk in a volume of 0.8-1 liters during the day.
Erosive gastritis is a fairly dangerous disease and is one of the most severe types of gastritis. The effectiveness of treatment largely depends on the timely initiation of treatment. At the first signs, you should consult a doctor, since self-diagnosis is very difficult due to the similarity of symptoms with many other diseases.
Journal "Internal Medicine" 3(3) 2007
Among the many diseases of the upper gastrointestinal tract (GIT), gastroduodenal erosions are among the most common and least studied.
Gastroduodenal erosions are superficial defects of the mucous membrane of the stomach and duodenum, not extending beyond its own muscular plate, which form in foci of superficial necrosis and heal without the formation of a connective tissue scar.
Erosion of the mucous membrane of the stomach and duodenum was first described by the Italian anatomist Morgagni back in 1761 in his work “On the location and causes of diseases identified by the anatomist,” based on the study of extensive sectional material. Subsequently, the study of the process of erosion of the mucous membrane of the gastroduodenal zone, mainly as a pre-ulcerative condition, was reflected in the works of K. Rokitansky (1842).
Much attention to the problem of superficial destructive changes in the mucous membrane of the gastroduodenal zone was paid by major researchers of the domestic therapeutic school in not so distant times (Yu.M. Lazovsky, V.Kh. Vasilenko). An increase in interest in this pathology has been noted in the last 10–20 years due to the widespread introduction of endoscopic research methods into clinical practice. According to most authors, with esophagogastroduodenoscopy, erosion of the mucous membrane of the stomach and duodenum can be detected in 10–25% of cases. However, a significant part of erosions is not diagnosed intravitally, as evidenced by the detection of erosive changes in the stomach and duodenum in sectional material in 6–28% of cases. In addition, recent studies have shown a clear trend towards an increase in the frequency of erosive lesions of the gastric mucosa and their complications. Erosive changes in the gastric mucosa today remain the second most common cause of gastrointestinal bleeding after duodenal ulcers.
However, this pathology remains one of the most poorly understood diseases of the gastroduodenal organs. Many aspects of the etiology and pathogenesis of gastric erosions have not been resolved, which complicates not only approaches to adequate therapy, but also the systematization of available scientific data. Thus, gastric erosions are not included in the International Classification of Chronic Gastritis (Sydney System, 1990); only its endoscopic section mentions the visual differences between acute and chronic erosions. Erosion of the stomach and duodenum is not included in the ICD 10th revision (1997), which once again confirms the lack of clear ideas about the place and significance of erosions of the stomach and duodenum in the structure of gastroduodenal pathology.
As suggested by K. Kawai et al. 30 years ago they began to distinguish between acute (superficial, flat) and chronic (complete, raised, smallpox-like - varioliform) erosions.
Acute erosions are superficial defects of the gastric mucosa, mainly in its distal section, the diameter of which does not exceed 1–2 mm.
Chronic erosions are raised (raised) areas of the gastric mucosa with a diameter of 3–7 mm, having a rounded shape, resembling a papule with an umbilical depression in the center, often with a small ulceration at their top (“mature” complete erosions).
Etiology and pathogenesis
Among the main causes of acute erosions, the following play an important role:
1) taking medications, including non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, digitalis preparations, nitrofurans, tolbutamide, veroshpiron, ethacrynic acid;
2) alcohol intoxication;
3) stressful effects (burns and frostbite, shock, wounds, polytrauma, psycho-emotional stress);
4) severe somatic pathology (decompensated circulatory failure, chronic renal and hepatocellular failure, blood diseases, chronic nonspecific lung diseases);
5) diseases of the endocrine system (hyperparathyroidism, diabetes mellitus, sepsis).
According to etiology, chronic erosions are divided into primary and secondary. Primary ones arise, as a rule, in practically healthy young people without concomitant diseases under the influence of unfavorable socio-climatic or psychotraumatic factors and are capable of undergoing involution as the influence of the latter is eliminated.
Secondary chronic erosions arise as the equivalent of a syndrome of generalized circulatory-hypoxic disorders, altered immune reactivity and metabolic processes against the background of diseases of the cardiovascular system and liver, associated with complete erosions with a frequency of up to 75%.
According to L.I. Aruina, in 19.1% of patients, erosions occur against the background of chronic gastritis, in the rest they are combined with other diseases of the digestive system, primarily with duodenal ulcer (51%) and chronic cholecystitis (13%).
Among the factors that are important in the development of erosions, the role of Helicobacter pylori (Hp), duodenogastric reflux, hydrochloric acid, a decrease in the cytoprotective properties of the gastric mucosa gel, microcirculatory disorders in the gastric mucosa, immune disorders, and some hormones is being studied.
Risk factors for erosion of the mucous membrane of the stomach and duodenum
1. HP infection. According to the results of modern studies, contamination of the mucous membrane with Hp is 66–85% when erosions are localized in the stomach. Some authors believe that the important role of HP in the occurrence of erosions is confirmed not so much by the high level of contamination of the gastric mucosa, but by the pronounced effect of eradication therapy, which clearly correlates with the frequency of elimination of erosive lesions.
However, most researchers do not consider this microorganism to be the main pathogenetic factor in the development of a chronic erosive process. There is no clear answer yet to the question of its possible participation in the development of acute erosions of the gastric mucosa.
The relationship between HP and microcirculatory disorders is interesting. There is evidence that Hp, causing alteration of the epithelium of the mucous membrane of the stomach and duodenum, promotes the entry of tissue thromboplastic and fibrinolytic agents into the general bloodstream, as evidenced by a direct correlation between the degree of contamination of the mucous membrane of the gastroduodenal zone with Hp and the activity of plasminogen activators in the peripheral blood. In studies by C. Atuma et al. the inhibitory effect of HP cytotoxins (VacA, CagA) on blood flow in the gastric mucosa is shown.
2. Most researchers attach great importance to microcirculation disorders in the pathogenesis of erosions of the gastric mucosa. With recurrent erosive gastritis in the remission phase, disturbances of local and general microcirculation are observed in 62 and 40% of cases, respectively, compared to 38 and 24% in patients with chronic gastritis without erosion, and especially pronounced changes were revealed when studying terminal blood flow.
With chronic erosions, intravascular aggregation, perivascular sclerosis and arteriovenous shunting develop, which leads to long-term microcirculatory disorders and the formation of chronic hypoxia of the mucous membrane. According to I.V. Maeva et al., changes in tissue blood flow in the distal part of the stomach are detected in 91.8% of cases, in the antrum - in all patients. Histological examination of biopsy specimens of the gastric mucosa in all patients with chronic erosions revealed morphological signs of microcirculation disorders, most pronounced in the antrum of the stomach: congestion of the microvasculature (capillaries and venules), perivascular hemorrhages, perivascular edema and stasis of erythrocytes.
Many authors have shown that during erosion, significant changes in the hemostatic system develop. In patients with erosive gastritis, duodenitis and duodenal ulcer, the antithrombogenic properties of the vascular endothelium are impaired, its antiaggregation, anticoagulant and fibrinolytic functions are reduced, especially in chronic gastric erosions.
3. Duodenogastric reflux is of great importance in the formation of acute and chronic erosions. According to various authors, gastric erosions are combined with the latter in 22.9–85% of cases.
Components of duodenal contents, primarily salts of deconjugated bile acids and lysolecithin, in high concentrations have a damaging effect on the gastric mucosa. Lysolecithin, which is formed in the duodenum during the hydrolysis of lecithin and bile by phospholipase A produced by the pancreas, has an extremely high degree of toxicity to the cell membranes of the gastric mucosa. The relationship between duodenogastric reflux and Hp infection is very interesting. There is evidence that HP in duodenogastric reflux and reflux esophagitis is less common than in chronic gastritis associated with HP.
4. Many researchers provide data on disturbances in the motor function of the stomach and an increase in intracavitary pressure, which first causes functional and then organic damage to the organ with the formation of a clinical picture of the disease. Thus, in the work of E.V. Nikishina identified intragastric and intraduodenal hypertension in 78% of patients with erosive gastritis, and also noted the predominance of the hyperkinetic type of gastric motor disorders.
5. In some cases, an increase in the blood levels of cortisol, gastrin, thyroid-stimulating hormone and insulin in patients with erosions is shown. Using correlation analysis, the authors established a direct relationship between the level of intragastric and intraduodenal pressure and the content of gastrin, insulin and thyroid-stimulating hormone.
6. Recently, more and more works have appeared indicating the importance of immunity disorders in the development of chronic gastric erosions. In this disease, disturbances are detected in the system of nonspecific defense factors in the form of a decrease in the phagocytic activity of leukocytes, levels of components of the complement system and lysozyme, as well as in the systems of cellular and humoral immunity. An adequate immune response is detected in only 13.5% of patients with chronic gastric erosions. In the epithelium lining the edges of the erosion, the synthesis of secretory IgA is disrupted, while the number of IgG-producing cells increases. With overproduction of IgG, T-suppressor receptors capable of regulating the local humoral immune response are blocked by immune complexes. At the same time, the fixation of immune complexes disrupts tissue metabolism, which leads to aggravation of degenerative processes in the gastric mucosa and inhibition of regeneration processes.
7. The significance of the acid-peptic factor in the development of chronic gastric erosions has not been clearly defined. I.V. Maev et al. (1998) report that chronic erosions are more common against the background of high rates of gastric secretion. According to their data, 24-hour monitoring of gastric pH did not reveal anacid conditions, hyperacidity was recorded in 47.7%, normoacidity in 25.2%, hypoacidity in 27.4% of patients with chronic gastric erosions. These data are contradicted by the results of other researchers, in which, in chronic gastric erosions, there was no pronounced hyperacidity and normo- and hypoacidity predominated. According to Ya.S. Zimmerman, V.E. Vedernikova (2001), in patients with chronic erosions, as a rule, no pronounced hyperacidity is observed - more often the pH is increased or remains within the normal range. However, never in the presence of chronic erosion was an anacid state recorded, which may indicate that the presence of hydrochloric acid in the stomach is a necessary condition for the appearance of chronic erosions.
8. With erosive damage to the gastroduodenal zone, regardless of the presence or absence of HP, the protective ability of the mucous gel is reduced, its quantity is reduced, and at the submicroscopic level the prevalence of destructive processes with damage to cellular structures - mitochondria and the Golgi apparatus is shown. In patients with erosions against the background of Hp infection, the protective ability of the gastric mucous gel is reduced due to the predominance of the synthesis of immature mucus components, and in uninfected patients - as a result of increased catabolism of mucus components. Studies by some authors suggest that, along with the production of hydrochloric acid, the presence of bile acids and a decrease in the activity of lysozyme, disturbances in the quantitative and qualitative composition of gastric mucus are a pathogenetic factor in the chronicity of the erosive process in the mucous membrane.
9. In recent years, much attention has been paid to disorders of prostaglandin (PG) metabolism in the development of erosive gastritis. According to some researchers, PGEs increase mucus secretion, activate regenerative processes in the gastric mucosa, and enhance its barrier function due to reverse diffusion of H+ ions. In addition, PGE1 presumably increases the production of gastric mucus glycoproteins, in particular N-acetylneuraminic acid and bicarbonates, thereby restoring the protective properties of the gastric mucosa and improving microcirculation in its wall. In patients with erosive gastritis, the content of PGE and PGE2a in the edge of the mucosal defect and the near-erosive zone is reduced.
10. Nonsteroidal anti-inflammatory drugs occupy a special place among the causes of the development of gastroduodenal erosions. Gastroduodenal ulcers occur in 20–25% of patients taking these drugs for a long time, and erosions of the mucous membrane of the stomach and duodenum occur in more than 50% of patients, and the risk of developing such lesions persists for several months after stopping treatment. Fundamental research by J. Vane showed that, as a result of inhibition of the enzyme cyclooxygenase (COX), NSAIDs block the synthesis of PG in the gastric mucosa. This enzyme has two isomers - COX-1 and COX-2. Activation of the COX-1 isomer leads to the formation of prostacyclin, which has a cytoprotective function in relation to the gastric mucosa. The release of the COX-2 isomer is induced by inflammatory mediators. The anti-inflammatory effect of NSAIDs is associated with the suppression of the COX-2 isomer, while side effects depend on the degree of suppression of this isomer.
Damages associated with NSAIDs may also be due to the participation of free radicals, increased production of tumor necrosis factor a (TNF-α), and increased chemotaxis of neutrophils into the gastric mucosa.
Thus, the etiology and pathogenesis of chronic gastric erosions are multifactorial. Many questions, despite significant achievements in recent years, remain open. Domestic and foreign literary publications are often quite contradictory, which greatly complicates the implementation of etiotropic and pathogenetic therapy.
Clinical course
Acute erosions have a clearly defined clinical symptom complex; clinical signs of underlying diseases come to the fore. In 30–90% of young people with unchanged mucous membrane, acute erosions can be asymptomatic or the clinical manifestations are quite scanty and nonspecific. More often, heartburn and sour belching occur; extremely rarely, low-intensity fasting and “hungry” pain in the epigastrium occurs. Acute gastric erosions are characterized by relatively frequent (up to 4.5%) development of hemorrhagic complications.
For chronic erosions, the manifestations of dyspeptic and abdominal pain syndromes are quite pronounced and specific. Belching and heartburn are observed in 75% of patients with chronic erosions, often combined with a feeling of heaviness in the right hypochondrium and flatulence. Periodic fasting and “hungry” pain in the epigastrium, observed in most patients with chronic erosions, often radiates to the spine. Moreover, if in young patients aching and dull pain predominate, then in the older age group the pain against the background of an increasing feeling of heaviness in the epigastrium is predominantly cramping in nature with the development at their height of nausea, unstable stool with a predominance of constipation. Thus, the clinical picture of chronic erosions reveals a certain similarity with the symptoms of duodenal localization of an ulcerative defect. Quite frequent formation of pronounced symptoms of underlying diseases was also noted. These include diseases of the cardiovascular system (arterial hypertension, coronary heart disease) and liver (chronic hepatitis and cirrhosis).
At the same time, there are studies indicating the nonspecificity of the clinical picture, which consists of pain and dyspeptic syndromes of varying severity. I'M WITH. Zimmerman et al. They also believe that it is impossible to use clinical manifestations for diagnostic purposes in relation to erosive gastritis.
Diagnosis of two types of erosions is carried out using fibrogastroduodenoscopic examination. However, a full judgment about the nature of erosions can be made only on the basis of a histological examination.
The development of acute erosions is usually preceded by subepithelial hemorrhages of the petechial type, but without compromising the integrity of the gastric mucosa, and therefore they are often described as hemorrhagic erosions. On histological examination, the defect in the mucous membrane of the stomach or duodenum is usually shallow, but occupies several ridges. The period of epithelization of acute erosions does not exceed 2–7 days.
Chronic erosions are located in the antrum of the stomach in the form of chains going towards the pylorus, in numbers from 1 to 15. The depth of the mucosal defect in chronic erosions is almost the same as in acute erosion; their bottom is usually formed by glands, less often by a muscular plate mucous membrane. Morphologically, chronic erosions are characterized by the presence of coagulative necrosis, which resembles fibrinoid necrosis in acute erosion, but without the typical fibrosis of the edges. Hyperplasia of the pyloric glands in the zone of chronic erosion is the cause of the formation of those elevations that serve as an endoscopic criterion. In the area of the bottom of complete erosions, granulation tissue is detected, and in the marginal sections - dystrophic and atrophic changes in the epithelium of the glands.
Chronic erosions exist for a long time - from 4 weeks to several years. According to a number of authors, this type of erosion can be divided into “immature” and “mature” based on the nature of histological changes. In the first case, erosion goes through all stages of development and epithelializes, then swelling of the mucous membrane at the site of its bulging remains permanently as a result of developing tissue fibrosis and pronounced productive inflammation.
Treatment
One of the most important and difficult problems is the treatment of chronic gastric erosions. Considering the versatility of the pathogenesis, most authors recommend complex treatment of erosions with an impact on various parts of their pathogenesis.
Therapy of both acute and chronic erosive lesions of the stomach involves, first of all, eliminating the influence of unfavorable factors of an exogenous and endogenous nature, that is, eliminating stressful influences, normalizing the diet and quality of nutrition, quitting smoking and drinking alcohol, and taking drugs with ulcerogenic properties.
Antisecretory drugs are intended for the treatment of gastroduodenal erosions, especially those occurring with ulcer-like manifestations and severe hyperacidity. Proton pump inhibitors (PPIs) are used - omeprazole 40 mg per day. It is possible to use H2 receptor blockers (famotidine 40 mg per day for 4–6 weeks with gradual withdrawal).
Considering the frequent detection of HP in the erosion zone, it is recommended to treat with anti-Helicobacter drugs as part of triple or quadruple therapy using mainly de-nol, which not only promotes the elimination of HP, but also has an anti-inflammatory and cytoprotective effect.
The II Maastricht Consensus recommendations for first-line treatment included the following triple treatment regimens: PPI at a standard dose 2 times a day (or ranitidine bismuth citrate) + clarithromycin 500 mg 2 times a day + amoxicillin 1000 mg (or metronidazole 500 mg) 2 times a day for 7 days.
Quadruple therapy was used as second-line therapy: PPI in a standard dose 2 times a day + bismuth subcitrate 120 mg 4 times a day + tetracycline 500 mg 4 times a day + metronidazole 500 mg 3 times a day.
The III Maastricht Consensus made the following changes to the treatment of Helicobacter pylori infection:
— first-line therapy: PPI + clarithromycin + amoxicillin (metronidazole can be used if primary resistance to clarithromycin in a given region is over 15–20%);
- PPI + amoxicillin + metronidazole regimen (can be used if resistance to metronidazole in the region is less than 40%);
— a 14-day prescription of eradication therapy increases the frequency of HP eradication by 9–12% compared to a 7-day course;
— quadruple therapy with colloidal bismuth can be used as an alternative to first-line therapy;
— as a second-line eradication scheme, bismuth-based quadruple therapy has retained its importance as the most optimal.
In case of ineffectiveness of first- and second-line eradication regimens, the III Maastricht Consensus offers the practitioner several acceptable options for further therapy. It is possible to prescribe high doses of amoxicillin (0.75 g 4 times a day for 14 days) in combination with high (4-fold) doses of PPIs. Another option may be to replace metronidazole in the quadruple therapy regimen with furazolidone (100–200 mg 2 times a day). An alternative is the use of a combination of PPIs with amoxicillin and rifabutin (300 mg per day) or levofloxacin (500 mg per day). The optimal way to overcome Hp resistance remains the selection of antibiotics, taking into account the individual sensitivity of a given Hp strain.
With NSAID gastropathy, according to the III Maastricht consensus, the risk of developing erosions and ulcers of the stomach and duodenum in Hp-positive patients is higher than in Hp-negative patients. Carrying out eradication therapy reduces the risk of developing ulcers and erosions in patients, and therefore, before starting to take these drugs, it is necessary to conduct a study of Hp infection and, if confirmed, prescribe eradication therapy. However, eradication therapy alone is not enough to prevent the development of NSAID gastropathy.
Regulators of motor function of the gastrointestinal tract. As already noted, with erosions, according to various authors, the frequency of duodenogastric reflux reaches 22.9–85%. According to Ya.M. Vakhrushev and E.V. Nikitina, during a comprehensive examination, duodenogastric reflux is detected in 75% of patients with erosive lesions of the gastroduodenal zone.
With erosive lesions of the gastroduodenal zone, the motor-evacuation function of the stomach and duodenum is disrupted, characterized by increased intracavitary pressure and significant dysfunction of the pylorus. As a result of duodenogastric reflux, the intragastric concentration of bile acids increases, which, by destroying gastric mucus, contribute to the colonization of HP in the gastric mucosa. Therefore, pathogenetically justified in the treatment of patients with erosions is the use of regulators of gastrointestinal motor function (domperidone, metoclopramide) and antacids (Maalox®). Regulators of the motor function of the gastrointestinal tract increase the tone of the stomach, lower esophageal and pyloric sphincters, strengthen and normalize their motility, and stimulate the evacuation of stomach contents.
Antacids, especially Maalox®, are effective means of combating duodenogastric reflux. Of course, in classic gastroesophageal reflux disease, the anti-acid activity of antacids cannot be compared with that of PPIs. But in the presence of biliary reflux, the purpose of their use is not only the neutralization of hydrochloric acid, but also the adsorption of bile acids and lysolecithin, as well as increasing the resistance of the mucous membrane to the action of aggressive factors (cytoprotection). These requirements are met, in particular, by the drug Maalox®, which contains aluminum hydroxide and magnesium hydroxide in a ratio of 1: 1 (tablets) and 1.1: 1 (suspension). Maalox® adsorbs lysolecithin and bile acids by 59–96%. It has a long-lasting (up to 4-6 hours) effect, adsorbs not only hydrochloric acid, forming buffer compounds with it, but also pepsin, bile acids and lysolecithin. It is known that in the damaging effect on the mucous membrane of the stomach and esophagus, hydrochloric acid and bile components compete for the right to be considered a more aggressive agent.
Cytoprotectors. It is known that the mucous protective barrier of the stomach has two lines of defense. The first line includes mucus, gastric and duodenal secretion of bicarbonates, the hydrophobic surface of the mucous membrane of the stomach and duodenum. The second line of defense is formed by the epithelial barrier. The apical surface of the gastric epithelium and intercellular junctions are extremely resistant to reverse diffusion of H+ ions due to the presence on their basolateral surfaces of two transport systems that remove H+ ions from the gastric mucosa. The integrity of this barrier is regulated by gastric growth factors, one of which is transforming growth factor α. This barrier includes tissue substances containing sulfhydryl groups (glutathione- and thiol-containing proteins), which are powerful natural antioxidants, as well as traps for free radicals of hydrogen and oxygen. The third line of defense includes normal blood flow, which promotes the elimination of H+ ions, provides energy for metabolic processes, supports the first and second lines of defense, and also regulates reparative processes in the gastric mucosa.
To restore the protective properties of the gastric mucosa, cytoprotectors are used. Maalox® also has cytoprotective activity, which is important in the treatment of erosive lesions of the gastroduodenal zone, both due to the formation of a protective layer of the drug on the surface of the epithelium, and as a result of increasing the production of endogenous prostaglandins in the gastric mucosa. Magnesium hydroxide increases the resistance of the gastric mucosa and enhances mucus formation, and aluminum hydroxide creates a protective film and enhances the production of prostaglandins. The combination of aluminum and magnesium in Maalox® supplements the range of positive properties of each antacid component separately and neutralizes the negative aspects of aluminum and magnesium hydroxide.
A significant clinical effect was obtained in the treatment of gastroduodenal erosions when prescribing 800 mg per day for 2–4 weeks of synthetic PGs enprostil and misoprostol, which improve regional blood flow and microcirculation, stimulate the formation of a mucous-bicarbonate barrier. In addition to prostaglandins, bismuth preparations (mainly bismuth tripotassium dicitrate - de-nol), sucralfate, and pentoxifylline also have a cytoprotective effect.
Drugs that improve microcirculation. Trental is most effective, improving microcirculation, rheological properties of blood and oxygen supply to tissues. In isolated works one can find recommendations for the inclusion of immunocorrectors in the treatment regimens of patients with chronic gastric erosions - T-activin 100 mg per day for 5-10 days, B-leukin (human recombinant interleukin), Galavit 200 mg per day for 5–10 days. There are reports of the effectiveness of the use of opioid peptides - dalargin and solcoseryl - for chronic gastric erosions, especially in combination with antisecretory drugs.
Thus, chronic gastric erosions are characterized by a recurrent course and, despite the large number of medications and regimens for their use, are often resistant to therapy. Often, the effectiveness of treatment for patients with chronic erosions remains low; in 24–25% of cases, clinical and endoscopic remission cannot be achieved, which can lead to the development of serious complications.
All this indicates the need to conduct more in-depth studies of the etiology and pathogenesis of chronic gastric erosions in compliance with the principle of complexity. This will allow you to choose the optimal treatment regimen for patients and significantly reduce the time for epithelization of chronic gastric erosions. Further dynamic observation makes it possible to reduce the frequency of recurrence of chronic erosions and improve the quality of life of patients.