Panniculitis is a heterogeneous group of diseases characterized by damage to subcutaneous fatty tissue (SAT) and often involving the musculoskeletal system and internal organs. Diagnosis of panniculitis is a rather difficult task, especially in rheumatological patients, since until now there are no clear clinical, morphological and laboratory data to determine this condition. The morphological picture is of fundamental importance. The disease is characterized by alternating periods of remission and exacerbations. The polymorphism of the clinical picture of panniculitis creates certain difficulties in diagnosing the disease. The lack of clear examination algorithms often leads to untimely recognition of the disease, which entails inadequate treatment tactics for patients.
In 1892, V. Pfeiffer [1] described spontaneous panniculitis as a syndrome of focal atrophy of the pancreas in the mammary glands, cheeks and lower extremities. In 1925, F. Weber [2] called this disease “non-suppurating nodular panniculitis”, and 3 years later H. Christian [3] noted the presence of fever. And only in 1938 I. Brill called this disease Pfeiffer-Weber-Christian disease [4]. The first description in the USSR was made by Yu.V. Postnov and L.P. Nikolaev [5].
Of particular interest in the practice of a rheumatologist is idiopathic lobular panniculitis (ILP) (syn.: Weber-Christian disease, Weber-Christian panniculitis, etc.), which, in accordance with the International Classification of Diseases, 10th revision (ICD-10), refers to systemic lesions of connective tissue (M 35.6). ILP is considered a chronic disease with multiple organ damage and is regarded as a clinical and morphological variant of lobular panniculitis with certain clinical symptoms. The disease is characterized by the rapid development of limited subcutaneous, usually multiple, nodes located in the tissue at different depths with predominant localization on the lower and upper extremities, less often on the chest and abdomen. Usually, within a few weeks the nodes resolve, leaving “saucer-shaped” recesses of the skin due to the development of atrophy of the pancreas. Sometimes calcium salts are deposited [1, 6]. Along with this, the clinical stages of development of the node in patients are distinguished depending on the color of the skin in the area of the induration: 0 - no rash, I - pale pink or pink color, II - red or purplish-red and III - bluish color and / or subcutaneous induration [6].
Today, the “gold standard” for diagnosing this disease is pathological examination, which occupies one of the central places in the algorithm for examining patients. The pathologist's conclusion on the localization and involvement of vessels in the pathological process, as well as the nature of the cellular composition of the infiltrate, helps clinicians clarify the diagnosis in accordance with the existing classification of panniculitis (Table 1) [7,
Table 1. Classification of panniculitis 8].
Features of ILP are the development of inflammation in the lobules of the pancreas, liponecrosis and the formation of granulomas. The changes go through 3 morphological stages: acute inflammatory, lipophagic and fibrotic [9]. Unfortunately, most often a biopsy is performed at the stage of fibrosis. Consequently, the pathologist is not able to reflect in his conclusion those morphological features that could contribute to a correct diagnosis. There is no data in the literature on the complementarity of the morphological and clinical stages of the disease.
The purpose of the study was to study the morphological features of ILP in accordance with the nature of the course and clinical forms of the disease.
Causes of panniculitis
- immunological panniculitis develops due to systemic vasculitis;
- enzymatic panniculitis occurs due to the action of enzymes produced by the pancreas and appears during the disease with pancreatitis;
- proliferative - cellular panniculitis appears in patients with leukemia or lymphoma;
- lupus or lupus - a panniculitis form that occurs when lupus is diseased; their symptoms are almost the same;
- The cold form develops with hypothermia and is characterized by the appearance of dense nodules. Often found in children and adolescents, it occurs within a few days after hypothermia. The lesions are localized on the cheeks and chin. Women who ride horses also suffer from this disease, and areas of the hips and pelvis are affected. This form of panniculitis does not require special treatment, but it is recommended to use protective equipment against hypothermia;
- the crystalline form develops with renal failure or gout. Characterized by deposits of urates and calcifications in the subcutaneous tissue;
- artificial fat granuloma occurs at the injection site when various drugs and liquids are administered. This form is observed in people with mental disorders who inject various substances under their skin. Measures are taken based on the fluid that was injected into the subcutaneous tissue;
- the steroid form occurs in children as a reaction to steroid drugs. No special treatment is carried out, recovery occurs immediately after stopping the drugs;
- the hereditary form develops due to a deficiency of a substance called antipripsin.
Sources
- Panniculitis in the practice of a rheumatologist (lecture)/ Belov B.S., Egorova O.N., Radenska-Lopovok S.G. // Scientific and practical rheumatology - 2013 - No. 4.
- Panniculitis in the practice of an internist and dermatologist (lecture)/ Egorova O.N., Belov B.S.// Consilium medicum - 2022 - No. 7.
- Spontaneous panniculitis: modern approaches to treatment / Egorova O.N., Belov B.S., Karpova Yu.A. // Scientific and practical rheumatology - 2012 - No. 5.
- Dermatovenerology / Butov Yu.S., Potekaev N.N. – 2022.
Symptoms of panniculitis
Panniculitis manifests itself as nodular formations. Localized mainly on the legs, arms or stomach. After the panniculitis nodes are cured, skin depressions remain in their places.
In the case of the nodular form of panniculitis, separately located nodes with a red tint on the surface appear in the subcutaneous tissue.
The plaque form of panniculitis is characterized by the presence of nodes that, fused together, form a tuberous area. The skin color of such formations varies from pink to purple-blue. Such areas sometimes occupy the entire area of the lower leg or shoulder, compressing blood vessels and nerve bundles, thus causing pain and swelling.
The infiltrative form occurs with the disintegration of nodes, then in the area of the blue node, a fluctuation appears. When such nodes are opened, a thick yellow liquid resembling a purulent substance is released, but it is not pus.
It is also possible to transition from the nodular form of panniculitis to the plaque form and then to the infiltrative form.
With spontaneous infection with panniculitis, changes are observed in the subcutaneous fatty tissue, which may not be accompanied by disruptions in the general condition of the body. But most often, at the initial stage of the disease, symptoms appear, for example, weakness or headache, and an increase in body temperature is also observed.
Panniculitis can have an acute, subacute or recurrent form of development. Development time ranges from two or three weeks to two years.
The acute form of panniculitis is manifested by high fever and pain in the joints and muscles, impaired functioning of the kidneys and liver. During treatment, the patient's condition continues to deteriorate and ends in death within a year.
The patient's subacute condition is more benign, but liver dysfunction is observed and is accompanied by fever.
The most benign state of panniculitis is recurrent or chronic. Relapses of the disease are severe, the general condition of the patient does not change, but this period is replaced by a long period of remission.
Treatment
Photo: astrakhanfm.ru
For single nodes, treatment is often carried out on an outpatient basis; the indication for hospitalization is the ineffectiveness of therapy for 10 days. Patients with subacute and chronic course are hospitalized if parenteral hormonal therapy is necessary. In addition, patients with infiltrative panniculitis and systemic manifestations (visceral symptoms, fever) are subject to observation in a specialized department.
The treatment plan is drawn up taking into account the characteristics of the causative disease (if any), the form and course of panniculitis, and the effectiveness of previously used methods. In case of a nodular form and the presence of a bacterial infection, antibiotics are used; in case of a viral load, antiviral agents are used. In addition, drug therapy includes anti-inflammatory drugs, antioxidants, and angioprotectors. Single nodes are injected with glucocorticosteroids. Laser therapy, ozokerite, and magnetic therapy are prescribed.
With infiltrative and plaque panniculitis, cytostatics and glucocorticosteroids for systemic use come to the fore. Liver tests, platelet count and creatinine tests are performed regularly throughout the course of treatment to detect side effects in a timely manner. Hepatoprotectors are used to improve liver function. Surgical interventions for all variants of the disease are ineffective, moreover, they can contribute to the progression of the pathological process and deterioration of the patient’s condition.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Diagnosis of panniculitis
Panniculitis is diagnosed at an appointment with a dermatologist; a rheumatologist and nephrologist, as well as a gastroenterologist, also help him in making the diagnosis. A biochemical analysis of urine and blood is prescribed. Using ultrasound, the abdominal cavity, kidneys and liver, and pancreas are examined to identify nodes of visceral panniculitis. A blood test for sterility helps to exclude the septic nature of the disease. Bacteriological examination of the yellow contents, which are released when the node is opened, helps to distinguish the infiltrative version of panniculitis from an abscess.
An accurate analysis of panniculitis is determined by a biopsy of the node. Histological examination determines inflammatory infiltration, replacement of fat cells with connective tissue. Immunological testing diagnoses lupus panniculitis.
Diagnostics
Photo: peachbetter.com
Diagnostic measures are carried out by a dermatologist. When preliminary determining the nature of the pathology, attention is paid to the occurrence of typical formations in soft tissues against the background of general infectious symptoms. During the physical examination, painful nodes with unclear or clear boundaries (depending on the stage of the disease), conglomerates, areas of fluctuation, and ulceration are detected. In the chronic course, limited zones of soft tissue retraction are identified in the place of already disappeared nodes.
Panniculitis is confirmed by biopsy. Morphological examination of the tissue sample confirms signs of granulomatous inflammation, multiple giant multinucleated cells, and lymphohistiocytic infiltration. To exclude systemic damage involving internal organs and timely detection of complications, the following procedures are prescribed:
- Ultrasound, CT or MRI of the abdominal organs;
- plain radiography of the chest organs;
- X-ray examination of joints (if there are complaints of pain, external changes).
A general blood test reveals an increase in ESR, leukocytosis with an increase in the number of neutrophils, thrombocytosis, and normochromic anemia. A general urinalysis reveals hematuria and proteinuria. According to a biochemical blood test, a violation of the results of functional liver tests is confirmed.
If visceral panniculitis is suspected, an examination by a surgeon is required. Consultations with other specialists (infectious disease specialist, oncologist, phthisiatrician) are prescribed according to indications, depending on the identified symptoms and the need for differentiation from other diseases.
symptoms
The most common symptom of mesenteric panniculitis is abdominal pain. This occurs when inflammation in the mesentery becomes so bad that the swelling puts pressure on the organs around the mesentery and intestines.
Other symptoms of mesenteric panniculitis include abdominal and digestive complications such as:
- there is very little feeling of fullness after eating
- nausea
- vomit
- swelling
- diarrhea
- constipation
- fatigue
- fever
- loss of appetite
- weight loss
The symptoms of mesenteric panniculitis can vary from person to person. Some people with the disorder may not notice any symptoms, or they may only notice minor symptoms. Others may experience severe symptoms requiring hospitalization.
Some people may also feel like there is a lump in their stomach. Symptoms of mesenteric panniculitis may last for weeks or months before departure.
What is mesenteric panniculitis?
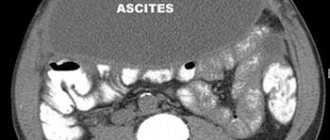
Mesenteric panniculitis is a chronic disorder that affects fat cells in the mesentery. The mesentery is a fold of tissue in the abdomen that attaches the intestine to the abdominal wall to hold it in place.
Mesenteric panniculitis causes persistent inflammation that can damage or destroy fat cells in the mesentery. This can lead to scar tissue and other symptoms.
There are three stages of mesenteric panniculitis. These:
- Mesenteric lipodystrophy is when fat cells begin to be replaced by cells from the immune system.
- Mesenteric panniculitis is when more immune system cells enter the mesentery and cause inflammation.
- Retractive mesenteritis is when inflammation worsens and scar tissue begins to form in the mesentery.
While mesenteric panniculitis is usually not life-threatening, symptoms can make daily life difficult. It may also be a sign of an underlying condition that may be more serious.
forecast
Mesenteric panniculitis is a long-term condition, but it is not life-threatening. The disorder usually improves without treatment, but some symptoms may interfere with daily life. Managing these symptoms is critical to maintaining a person's quality of life.
Doctors will also check for any underlying conditions that may be causing mesenteric panniculitis. Working closely with your doctor to monitor the progress of this condition is the best way to avoid complications and relieve symptoms.
Complications and related conditions
Mesenteric panniculitis is usually benign, meaning the condition itself is not dangerous or cancerous. However, complications may arise.
Severe inflammation can cause slowing and blockage in the intestines. This can worsen other symptoms such as nausea and bloating. This may also be a factor in abdominal pain.
In some cases, the added pressure from a blockage in the intestines can make it difficult for the body to absorb nutrients from food.
Mesenteric panniculitis may also occur along with some types of cancer. Doctors will rule out cancers at the time of diagnosis.
Panniculitis: causes of development
In most cases, Beber-Christian panniculitis occurs in the idiopathic (spontaneous) form of the disease. It is more common among the female population aged 25-40 years. The rest of the cases, approximately 35%, are so-called cases of secondary panniculitis, which develops against the background of systemic and skin diseases, provoking environmental factors (cold, UV radiation, medication) and various immunological disorders.
The development of panniculitis is based on a violation of metabolic processes in the human body, namely fat peroxidation. Despite many years of research aimed at identifying the factors that cause panniculitis, there is no clear understanding of the mechanism of its development.
Panniculitis: classification
Weber-Christian panniculitis (see photo) is classified into primary (idiopathic form) and secondary.
The following types of secondary panniculitis include:
- immunological – occurs against the background of systemic vasculitis. In children, it may be a variant of erythema nodosum;
- mesenteric panniculitis is a rare pathological disease that affects the adipose tissue of the intestinal mesentery, omentum, pre- and retroperitoneal tissue;
- lupus – accompanies systemic lupus erythematosus and is characterized by the manifestation of symptoms of panniculitis with typical skin symptoms of lupus;
- enzymatic – associated with the action of pancreatic enzymes;
- proliferative cell – occurs with leukemia, lymphoma, histiocytosis;
- cold - a local form of panniculitis that forms in response to severe cold exposure;
- steroid – occurs in children within one to two weeks after discontinuation of glucocorticoid therapy, occurs independently;
- Panniculitis, which develops with gout and renal failure due to the deposition of uric acid calcifications in the subcutaneous fat;
- Panniculitis associated with L1-antitrypsin deficiency is a hereditary disease accompanied by systemic manifestations: vasculitis, hemorrhages, pancreatitis, hepatitis and nephritis.
Primary, or lobular panniculitis, belongs to rare diseases from the group of systemic connective tissue diseases. Verification of lobular panniculitis is based on the results of histology only, since a specific marker or study confirming the presence of this disease has not yet been found. Based on the shape of the nodes formed during panniculitis, they are distinguished:
- Nodal variant of the disease;
- Infiltrative option;
- Plaque option.
Panniculitis: treatment in Moscow
The approach to the treatment of panniculitis, both primary and secondary, is complex. For the treatment of nodular panniculitis, non-steroidal anti-inflammatory drugs and antioxidants (vitamin E, ascorbic acid) are prescribed. Sometimes single nodular formations are injected with glucocorticoid drugs. The following physiotherapy procedures have also proven their effectiveness:
- UHF;
- Magnetotherapy;
- Ozokerite;
- Ultrasound;
- Laser therapy.
For plaque and infiltrative forms, subacute panniculitis, glucocorticosteroids (hydrocortisone, prednisolone) and cytostatics (methotrexate, cyclophosphamide) are used. Treatment of secondary forms of panniculitis must necessarily include therapy for the underlying disease, for example, pancreatitis, SLE, vasculitis, gout.
The Yusupov Hospital provides each patient with a full cycle of medical services: high-quality diagnostics, timely treatment, and responsive medical staff. The clinic’s specialists strive to create the most comfortable conditions for the patient’s stay in the hospital. Convenient location, away from the bustle of the city, the presence of targeted programs for prevention and rehabilitation and the availability of a day hospital will ensure the fastest possible recovery for the patient. To make an appointment please call.