What can cause ulcerative colitis?
It was previously believed that ulcerative colitis was caused by poor diet and frequent stress. However, further research has shown that these factors may increase the severity of the symptoms of the disease, but are not its cause.
Currently, there is no single concept regarding the pathogenesis of ulcerative colitis. Probably, a significant contribution to the development of this disease is made by disruption of the immune response mechanisms in the body.
Hereditary causes can also play a role - most often, if there are relatives in the family who suffer from this pathology, the rest of the family members are also at increased risk. This is especially clearly seen in the example of closed communities, for example, Ashkenazi Jews.
In addition, there is a theory according to which ulcerative colitis can be triggered by a high number of sulfate-reducing bacteria, the waste products of which trigger the development of this pathology.
Optimization of therapy for ulcerative colitis. Kaleidoscope of clinical observations
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
– I give the floor to Oksana Borisovna Shchukina. We are again in St. Petersburg. Oksana Borisovna, “Optimization of therapy for ulcerative colitis. Kaleidoscope of clinical observations."
Oksana Borisovna Shchukina , assistant professor, candidate of medical sciences:
– Dear colleagues, good afternoon! First of all, I would like to say that when we touch upon the treatment of ulcerative colitis, we necessarily emphasize the differences regarding the standard approaches for stopping a severe, fulminant attack of ulcerative colitis and inducing remission of mild and moderate ulcerative colitis. In addition, when prescribing therapy, we must take into account the localization of the lesion - it is proctitis, left-sided ulcerative colitis or total, widespread ulcerative colitis. And finally, our treatment tactics will differ depending on the stage of the disease - we are dealing with an exacerbation of ulcerative colitis, and then we are talking about the induction of remission, clinical-endoscopic remission with the withdrawal of steroids, or we are talking about the already achieved remission of ulcerative colitis, and it is about steroid-free maintenance with endoscopic assessment.
It should be emphasized that ulcerative colitis is currently an incurable disease, and therefore therapy for patients is lifelong. Unlike Crohn's disease, the lesion affects only the colon, so surgical cure is possible by performing a colproctectomy. As for the treatment of mild to moderate ulcerative colitis with 5-aminosalicylic acid drugs, these drugs are quite effective in 80% of patients. The consensus is that all mesalazine preparations are equally effective, in some cases increasing the dose of mesalazine more than 3-4 g leads to a faster response. It is recommended to prescribe mesalazine, taking into account not only effectiveness, but also taking into account the method of release of the active substance, the frequency of administration, which affects adherence to treatment, and various delivery systems for mesalazine, because the drug works specifically in the segment of the colon where it is delivered. Therefore, speaking in general about the identical effectiveness of mesalazines, for each specific patient the effectiveness may be individual, depending on these properties.
I will focus on three clinical cases - this will be a fulminant attack of ulcerative colitis, a severe attack and moderate ulcerative colitis - and using clinical examples I will try to highlight the features of optimizing therapy for inducing remission and maintaining remission in these patients. So, the patient, born in 1972, quits smoking at the age of thirty-four. Subsequently, about a year after birth, a fulminant attack of ulcerative colitis - up to 12 stools, high fever, with a decrease in hemoglobin to 96, with an accelerated ESR to 62, C-reactive protein at a norm of 5 to 136, and an endoscopic severity index of 8 points , that is, the maximum. The patient was transferred from the infectious diseases hospital, where intestinal infection was excluded, to our specialized hospital. This is a severe attack according to the Trulove-Witts index, so therapy with intravenous steroids was prescribed, but there was no response to therapy within two weeks.
The patient did not deteriorate, therefore, whenever surgical treatment was discussed with coloproctologists, the issue of surgery was postponed, and it was decided to achieve induction of remission with anti-cytokine therapy, that is, the patient was prescribed Remicade due to the lack of response to intravenous steroids. Therapy with the immunosuppressive drug azathioprine was also included. The patient responded to the induction course and received combination therapy with Remicade and azathioprine for almost 8 months. 6 infusions were performed. She received Remicade, azathioprine, 5-aminosalicylic acid preparations, and continued clinical remission in September, but the drug disappeared from the pharmacy network, and the seventh infusion was not administered in November. But the patient remained in remission, continued to receive azathioprine, 5-aminosalicylic acid preparations, and when Remicade appeared 3 months later, in February 2010, the question arose whether anticytokine therapy should be continued for the patient in remission. According to the examination, calprotectin was normal, he felt normal, and it was decided to refrain from continuing infusions and continue them if his health worsened.
The patient comes back a year later, in January 2012. She has normal calprotectin, she has a normal endoscopic picture, a study is carried out for friability, vulnerability (...)(05:11), the test is negative, which indicates good, deep healing of the mucous membrane, histological remission is also confirmed, and the patient asks to stop immunosuppressants in Due to the fact that she does not like the side effects, she is wary of the side effects of immunosuppressants listed there. Therapy with 5-aminosalicylic acid continues, and she has been receiving Mezavant for a year. At first there was 1 tablet, but after stopping the immunosuppressants we switched to 2 Mezavant tablets, and after a year clinical remission was assessed using calprotectin, and today the patient is in a state of clinical and laboratory remission.
Why were we able to get away from azathioprine in this case? Azathioprine is indicated in the following situations, says the latest Consensus on Ulcerative Colitis: relapses occurring during maintenance therapy with adequate doses of 5-aminosalicylic acid, or intolerance to these drugs. The patient did not receive treatment with us; it was a fulminant attack of ulcerative colitis, so in this case, despite the fact that induction of remission was achieved with Remicade, we allowed ourselves to move away from azathioprine and remain on adequate doses of 5-aminosalicylic acid. Thus, the peculiarity of this clinical observation is that this is a fulminant onset of ulcerative colitis. The patient was resistant to intravenous steroids, which led to the need for rescue therapy as an alternative to colectomy with Remicade (infliximab).
Remission was achieved with a combination regimen - Remicade, azathioprine, 5-aminosalicylic acid. Maintenance therapy was provided with azathioprine and 5-aminosalicylic acid. We discontinued Remicade because she had not previously received azathioprine, this is consistent with the Consensus data, and a very important factor is that the patient was fully adherent to treatment. Finally, discontinuation of azathioprine became possible, provided, again, adherence to maintenance therapy with adequate doses of 5-aminosalicylic acid, the patient had not previously received fulminant attacks. Well, abandoning local forms of 5-aminosalicylic acid and switching to the multi-matrix form of mesalazine (Mezavant) allowed us to achieve very good adherence. Clinical case – patient born in 1987. He also quit smoking, and after about 7 months, a twenty-one-year-old young man developed a fever, more frequent stools, laboratory activity in the form of accelerated ESR, an increase in C-reactive protein, and also a fairly severe endoscopic index of severity of ulcerative colitis. This is a common ulcerative colitis, also a severe course, high activity, and intravenous steroids are prescribed to induce remission, followed by a transition to oral steroids.
Azathioprine is also prescribed, why, because induction is carried out with the prescription of intravenous prednisolone, so we make sure to immediately add azathioprine, and he receives mesalazine orally and rectally, a combined regimen. He has been on steroids for a very long time, gradual withdrawal - 6 months gradually reducing the dose, continues to receive azathioprine, mesalazine, and after stopping steroids, leukopenia develops on azathioprine, and therefore we are forced to abandon this drug. He remains on 5-aminosalicylic acid, in general, the full dose is 3 g orally and the Salofalk suppository 0.5 g rectally. Remission control. He feels well, remission is controlled by the level of fecal calprotectin, and without azathioprine he maintains remission on mesalazine and combination medications. Naturally, the young man does not really like the local treatment, and therefore at the beginning of 2011 he switched to prescribing multi-matrix mesalazine (Mezavant) at a dose of 2 tablets. He comes for a follow-up visit in March 2012, a year later - normal fecal calprotectin, completely healed mucous membrane with an endoscopic severity index of 0, and a test for friability and bleeding - it is also negative, deep histological remission without basal plasmacytosis.
The patient continues to take Mezavant 2 tablets once in the morning, a very convenient regimen. He is fully committed to therapy, this suits him well, and today he is in remission. Features of this clinical observation: severe attack, intravenous prednisolone is prescribed to induce remission; Steroid dependence develops and is overcome by prescribing azathioprine. Maintenance therapy with azathioprine and 5-aminosalicylic acid preparations, unfortunately, is impossible due to the development of leukopenia, that is, myelotoxicity against the background of azathioprine, and the possibility of discontinuing azathioprine while the patient is fully committed to therapy with 5-aminosalicylic acid. And let us immediately emphasize that before the onset of the disease, before the first symptoms appeared, he was an untreated patient with 5-aminosalicylic acid, so we can safely move away from azathioprine. Well, abandoning local forms of 5-aminosalicylic acid and prescribing multimatrix mesalazine only orally, and once a day, this is very convenient, allowed us to achieve excellent adherence.
And finally, the third case is a twenty-nine-year-old patient with moderate severity of ulcerative colitis. A weaker stool appeared mixed with blood, the endoscopic severity index was 5 points. Standard therapy was prescribed - mesalazine orally and in enemas, with a rapid achievement of remission - in fact, within 2 months the patient already felt great and stopped taking these drugs, that is, she stopped taking them. Against this background, an exacerbation develops, with acceleration of ESR, with endoscopic activity, and the patient is still recommended to take an induction course of mesalazine 3 g and a rectal suppository of mesalazine 2 times a day to induce remission. She achieves remission quite quickly, but then she starts again, either taking or not taking mesalazine, then she puts a suppository, when blood appears, then she stops taking it. And when she came for her next appointment - it was January 2011 - she had a tough conversation about the need to maintain remission, that the appearance of blood in the stool is just the tip of the iceberg, that persistent inflammation in the mucous membrane leads to completely unnecessary, dangerous consequences . A standard induction dose was prescribed again - 3 g orally and 0.5 g rectally, remission was achieved very quickly, and she felt so good that she again began to doubt the therapy. Literally 3 months later I asked if something could be done about rectal forms, she didn’t like suppositories. Remission-maintaining therapy was prescribed with multimatrix mesalazine (“Mezavant”), only one tablet, although the instructions for the drug indicate that maintenance of remission should be ensured by 2 tablets, 2.4 g per day.
But considering that the patient did not have any severe symptoms of proctitis, and she responded very well to therapy with 5-aminosalicylic acid, one maintenance dose of 1.2 g was quite sufficient for her. She came back after almost a year - normal calprotectin, fully committed to therapy, and the next year, in January 2013, she came to us asking what she should do, she was going to get pregnant. She generally doubts whether she has ulcerative colitis, that she feels great, maybe she should stop taking this pill. We send the patient for examination. Clinical remission is confirmed by endoscopic remission, there is no looseness, no vulnerability when performing a pressure test on the mucous membrane, the morphologist proves to us that there is no basal plasmacytosis, that is, complete deep histological remission, and the patient was asked to continue mesalazine one tablet continuously, to plan pregnancy.
This is a completely acceptable drug, and even you need to take it, be sure to protect the mucous membrane during pregnancy, childbirth and feeding. Monitor fecal calprotectin - she does this, the data in 2013, as of January 2014 are quite satisfactory to us, and it is recommended to monitor fecal calprotectin every 4-6 months. Continue taking one tablet of Mezavant, and if there is an increase in the level of fecal calprotectin, add suppositories with 5-aminosalicylic acid. In this case, the localization of ulcerative colitis was left-sided, but the cecum was involved, so we could not limit ourselves to topical mesalazine; we definitely had to prescribe therapy with oral 5-aminosalicylic acid. And the main factor in the lack of stable remission was lack of adherence to treatment. The patient did not like the large number of tablets, did not like the rectal forms, and giving up the rectal forms, switching to actually one tablet a day in the morning, which did not burden her life, so to speak, led to good adherence.
And the last two slides. We often encounter in our center that patients are prescribed steroids very inadequately and not always on time. What does the Consensus say about this? When to prescribe steroids to patients? How should the response to 5-aminosalicylic acid therapy be correctly assessed? We prescribe steroids if deterioration occurs on an adequate dose of mesalazine. That is, when more than 2 g per day is prescribed, and the patient worsens, then we turn on steroids. The next situation is when there is no improvement within 10-14 days of mesalazine therapy, that is, blood remains in the stool, we discuss the issue of prescribing steroids. And finally, if by 4-6 weeks there is also no complete clinical response, that is, blood remains in the stool. An interesting study was conducted on Mezavant, on multi-matrix mesalazine. Patients who did not respond to Mezavant by week 8 achieved clinical remission in 60% of cases in the subsequent 8 weeks. That is, if they took the maximum dose of the drug for the next 8 weeks - this is 4 tablets, 4.8 g - 60% of those who did not respond by the 8th week responded over the next 8 weeks. This is very important information for clinicians. That is, if the patient does not deteriorate, then slowly and surely you need to try to wait for these another 8 weeks, because everyone heals at a different pace, everyone has a slightly different response from the mucous membrane to therapy.
Finally, we say that left-sided ulcerative colitis can generally be treated topically with enemas or foam, but the Consensus in this case says that in cases of mild ulcerative colitis, moderate ulcerative colitis can be attempted with multi-matrix mesalazine, which covers not only the ascending, transverse colon, descending colon, and in the rectum, in general, there is enough 5-aminosalicylic acid. Therefore, you can start with tablet forms, and only if symptoms persist and the rectum does not heal, add topical forms. Thank you for your attention.
Typology of ulcerative colitis
Based on the location of the affected area in the gastrointestinal tract, the following types of ulcerative colitis are distinguished:
- Proctitis – the rectum is susceptible to inflammation.
- Proctsigmoiditis - affects the rectum and sigmoid colon.
- Distal colitis - pathological changes occur in the rectum, sigmoid and descending colon.
- Left-sided colitis - the part of the large intestine located on the left side of the abdominal cavity (distal intestine plus transverse colon) becomes inflamed.
- Pancolitis - inflammation of the large intestine along its entire length.
Symptoms of Ulcerative Colitis
The most common symptoms of ulcerative colitis, depending on its location, are diarrhea with blood or pus, abdominal pain and cramping. In addition, fatigue, fever, nausea, sudden weight loss, anemia, joint pain and skin rashes are possible.
Symptoms of the disease may be stronger or weaker in different people, all at once or separately. Spontaneous disappearance of symptoms (remission) is also possible, which can last for years.
Page 5 of 12
Diet therapy for deficiency of macro- and microelements in patients with inflammatory bowel diseases
Calcium deficiency is often observed in patients with inflammatory bowel disease. Calcium has anti-inflammatory, antidiarrheal, antiallergic effects, accelerates the restoration of the intestinal mucosa. The cause of deficiency may be impaired absorption, increased losses and/or insufficient intake of calcium from food. Products containing calcium - dairy products (the source of more than half of the amount of calcium consumed), cheeses, eggs, soy isolates, buckwheat and oatmeal, fish and fish caviar.
Patients with IBD often have micronutrient deficiencies, such as zinc. In the human body, zinc performs a number of functions in relation to immune defense and the fight against inflammation, it has an antidiarrheal effect, and accelerates the restoration of the intestinal mucosa. Zinc deficiency is more common in Crohn's disease than in ulcerative colitis, and zinc excretion in feces is higher than normal. Untreatable diarrhea is often due to zinc deficiency because it is lost in feces. In case of zinc deficiency, you should take vitamin and mineral complexes containing zinc (for example, Gerimax, Tri-vi-plus, Zinkit, etc.). In this case, the frequency of stool quickly decreases. However, not all zinc preparations are well absorbed in the intestine. It is difficult to achieve a high zinc content in the diet because... Only a few foods are high in this micronutrient. These include: yeast, eggs, cereals (buckwheat, oatmeal), corn products, legumes, mushrooms, hard cheeses, meat, entrails (which, however, should be avoided in the acute phase of diseases due to the possible high content of toxins in them) and oysters. Plant foods usually contain small amounts of zinc and in many cases may even impair the absorption of zinc in the intestines.
The cause of iron deficiency and the development of iron deficiency anemia in Crohn's disease is primarily a decrease in the absorption of this microelement in the small intestine due to the inflammatory process. In ulcerative colitis, such a deficiency occurs mainly due to increased loss of iron in the blood during bowel movements. Healthy people absorb approximately 5-10% of the iron contained in food, and in conditions of iron deficiency - 10-20%. The absorption of iron from the intestines depends on the type of food, it is best absorbed from mammalian meat - 22%, from liver - 12-16%, from fish - 9-11%, from eggs and beans - 2-3%, from fruits - 3 -4%, from rice and spinach – 1%. Oxalic acid (spinach, sorrel, legumes), tannins (blueberries, quince), phosphates and phytins (cereals, legumes), strong tea and excess dietary fiber worsen the absorption of iron. Egg and soy proteins also reduce the absorption of iron from the gut. Organic acids (malic, citric, ascorbic) improve iron absorption. The optimal combination in one dose is of products containing heme iron with high bioavailability (animal meat, poultry, liver, kidneys) and products rich in organic acids (rosehip decoction, blackcurrant, clarified juices, lemons, etc.)
Since iron absorption cannot exceed certain values, dietary correction of this microelement deficiency may not be enough. In these cases, it is necessary to use drugs containing iron, for oral or intramuscular and intravenous administration.
How do you know which foods you tolerate well and which you don’t?
A great help in answering this question is keeping a food diary, which daily reflects all the foods and dishes that were consumed during the day, and also notes changes in well-being. The frequency and nature of stool, the intensity of abdominal pain, and the presence of nausea must be indicated. Foods that may be poorly tolerated by patients with intestinal diseases: vegetables, herbs, legumes, fruits, berries in their natural form, mushrooms, nuts, citrus fruits, whole milk, sauces, spices, snacks, sweets, confectionery, honey, jam, carbonated drinks , cold dishes.
One food that is often poorly tolerated by patients with IBD is whole milk. This occurs due to a deficiency of the lactase enzyme, which is produced in the small intestine and breaks down milk sugar - lactose. Lactase deficiency is often observed during exacerbation of both Crohn's disease and ulcerative colitis. As a result, a large amount of undigested milk sugar accumulates in the intestinal lumen, which causes diarrhea, bloating, nausea, heaviness and pain in the upper abdomen. If milk intolerance is observed during the period of exacerbation of the disease, this does not mean at all that the symptoms of intolerance will persist during the period of remission.
Dairy products that are generally well tolerated in lactose intolerant patients include yogurt and cheese. It is advisable to maintain dairy products in the diet of those patients who tolerate them well.
In IBD, so-called hidden food intolerance often occurs, which is based on the processes of inadequate response of the patient’s immune system to certain foods. Without clear symptoms, the components of a number of food products cause disruption of the digestive and absorption functions of the intestine, destabilization of its microflora, leading to intoxication of the body, and even an additional factor of intestinal damage in patients with ulcerative colitis and Crohn's disease. Identification of the fact of hidden (immune-dependent) food intolerance is carried out using special immunological tests, which determine antibodies (associated with G4 immunoglobulins) to food products. To do this, all patients with inflammatory bowel diseases should undergo the so-called York Test, developed at the British Scientific Laboratory of Clinical Nutrition in York (in some Russian laboratories and clinics it is called the “hidden food intolerance test”). This blood test reveals the degree of intolerance (mild, moderate or severe) to specific nutrients from over 100 foods tested.
Some patients with inflammatory bowel disease have celiac disease , a disease of the small intestine characterized by intolerance to gluten (a protein found in wheat, rye, and barley). As a result, the absorption of nutrients in the intestine is impaired to one degree or another, which manifests itself in the form of a deficiency of proteins, vitamins, and microelements. Celiac disease can often be combined with Crohn's disease and even imitate its exacerbation.
The main method of treating celiac disease is a lifelong diet, the main principle of which should be the exclusion of all products containing gluten, these are barley, millet, wheat, rye, oats and products containing them (white and black bread, pasta, dumplings, pancakes, cakes, cakes, cookies, gingerbread, ice cream, puddings, etc.).
Cereals intolerable to those with celiac disease are found in some alcoholic drinks (beer, whiskey), instant soups, and instant coffee drinks. Flour can be added to yoghurts, glazed cheese curds, sausages, sausages and sausages, cheeses, canned food, ketchups, mayonnaise, and sauces.
Dietary restrictions must be strictly followed by the patient, since taking even 100 mg of gluten-containing foods (a few crumbs of bread) can worsen the course of the disease. Products with food colorings and preservatives are prohibited.
Products made from gluten-free grains and vegetables (rice, corn, legumes) are allowed. When preparing various dishes (for example, baked goods, sauces), rice and corn flour are used as substitutes for wheat flour. Buckwheat porridge is shown in limited quantities.
Table 5. Products allowed and prohibited for celiac disease
| Allowed | Forbidden | |
| Soups | Decoctions, vegetable and meat soups without thickener | Noodle soup, canned soups, bouillon cubes, dry soup mixes |
| Dairy | Milk and dairy products, cheese | Some commercial dairy drinks (milk sauces, ice cream, yoghurts, some cheeses (including processed cheeses), yoghurts, glazed cheese curds |
| Fats | All types of fats | Margarines with gluten-containing stabilizers |
| Meat products, eggs | All types of meat, eggs | Breaded products, products in sauces, some types of sausages, ready-made cutlets, canned meat |
| Fish, seafood | All types of fish and seafood, canned fish in oil and own juice | Breaded products, products in sauces, imitation seafood, some canned fish |
| Cereals and pasta | Rice, corn | Wheat, rye, barley, oats (cereals - wheat, semolina, oatmeal, pearl barley, “Hercules”, oatmeal, pearl barley, barley, “Artek”, “Poltavskaya”, “7 grains”, “4 grains”, etc. ), bran, “Muesli” and other breakfast cereals, baby cereals, pasta, corn flakes when using barley molasses |
| Flour and starch | From rice, buckwheat, corn, potatoes, tapioca, cassava, sweet potato, beans, peas, soybeans, various nuts | Wheat, rye, oat flour and starch |
| Legumes | All types of legumes | Canned legumes |
| Vegetables and fruits | All types of vegetables and fruits in various preparations | Commercially prepared salads, vegetables in sauces, breaded, many canned vegetables and fruits, incl. tomato pastes, ketchups |
| Bakery products | Special types of bread (corn flour, soy flour, etc.) | Bakery products from wheat, rye, barley, ready-made confectionery products |
| Beverages | Coffee, tea, juices, cocoa | Dry mixes for preparing drinks, coffee substitutes |
| Sauces, spices | Yeast, vinegar, MSG, chili | Mustard, chewing gum; some types of vinegars and salad sauces, ketchups, mayonnaises; multi-component dry seasonings and spices (“Vegeta”, etc.) |
| Sweet dishes | Marmalade, marshmallows, some types of ice cream and sweets. Jams, preserves, caramels, etc. homemade | caramel, soy and chocolate candies with filling, oriental sweets, industrial jam |
| Beverages | Juices, coffee beans | Kvass, instant coffee and cocoa drinks, some alcoholic drinks (vodka, beer, whiskey) |
| Nutritional supplements | Annatto dye E160b, caramel colors E150a-E150d, oat gum E411, maltol E636, ethyl maltol 637, isomaltol E953, malitol and maltitol syrup E965, mono- and diglycerides of fatty acids E471) | |
| Non-food products containing gluten | Glue on postage stamps and envelopes, some types of cosmetics, incl. lipstick, some types of toothpaste | |
| Medications | Most medications | Certain medications (mostly film-coated tablets) |
- Back
- Forward
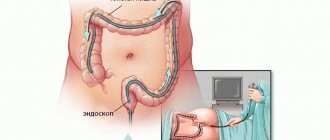
Diagnosis of ulcerative colitis
The leading diagnostic method today is endoscopy. Also, to make a diagnosis of ulcerative colitis, a histological analysis is performed to exclude Crohn's disease from the diagnosis. To assess the severity of the disease, laboratory tests are used (complete blood count, blood test for specific antibodies (pANCA) and inflammatory markers (C-reactive protein, CRP), stool analysis). Ultrasound scanning and computed tomography can be used to assess the degree of swelling of the large intestine and monitor its possible perforation.
Treatment of ulcerative colitis
Treatment of ulcerative colitis, depending on the severity of the disease, includes drug therapy, diet changes and, in extreme cases, surgery. The course of therapy is aimed primarily at eliminating the symptoms of the disease and can be adjusted if unwanted side effects occur.
Clinical guidelines for the treatment of ulcerative colitis include the following types of drugs:
- Anti-inflammatory – to eliminate pathological inflammation;
- Antibiotics – to treat concomitant infections;
- Corticosteroids - to short-term reduce the immune response and relieve inflammation;
- Immunosuppressants - to reduce the intensity of the immune response in the long term;
- Iron supplements – to prevent anemia and restore hemoglobin levels;
- Specialized probiotics - to change the composition of the microflora of the gastrointestinal tract.
Everything you need to know about ulcerative colitis and Crohn's disease
What are inflammatory bowel diseases?
Inflammatory bowel diseases (IBD) are a group of diseases characterized by the development of swelling and inflammation in the wall of the gastrointestinal tract. There are two types of IBD: ulcerative colitis (UC) and Crohn's disease (CD) . These conditions are different in their course, but their symptoms are similar. In ulcerative colitis, the inner (mucous) lining of the colon is inflamed, which can lead to the development of ulcers and erosions (superficial defects in the lining of the colon). In Crohn's disease, inflammation affects the deeper layers of the wall of the gastrointestinal tract. In addition, with this pathology, any part of the digestive tract, from the oral cavity to the rectum, can be involved in the inflammatory process. Inflammatory bowel diseases are often accompanied by the development of damage to other organs and systems, for example: eyes, skin, joints, liver, kidneys, etc. Inflammation in IBD persists for a long time and, as a rule, periods of remission (inactive phase) are followed by periods of exacerbation. The disease can occur in people of different nationalities and at any age, but young people are more often affected.
What are the causes of IBD?
The causes of IBD are not fully understood. It is believed that the disease can be caused by pathogenic microorganisms (viruses or bacteria) that live in the intestines with increased activity of the immune system. At the initial stage of the process, inflammation develops in the small or large intestine, which often depends on the genetic predisposition of the patient. This leads to the formation of antibodies that permanently damage the intestines. It is possible that patients have a violation of the defense mechanisms against bacteria that normally live in the gastrointestinal tract. It is possible that the reaction of the immune system to certain types of bacteria or viruses plays an important role. Inflammatory bowel disease cannot be transmitted to other family members of the patient.
What are the symptoms and course of IBD?
UC and CD can vary in course and are related to the severity of the disease, ranging from mild to severe, depending on the extent of the lesion and other factors. In the inactive stage of UC and CD, patients experience virtually no symptoms, that is, the disease is in remission. Periodically, throughout the year, the disease may worsen (pass into the active phase).
The main symptoms of exacerbation are: - frequent urge to have bowel movements with the release of mucus and blood; - diarrhea (frequent, loose stools); - abdominal pain before bowel movement; - general weakness, weight loss; - elevated temperature.
If only the rectum is involved in the inflammatory process (proctitis), then the disease is manifested only by the appearance of mucus and blood in the stool without diarrhea. The severity of symptoms varies from exacerbation to exacerbation: they can be less pronounced, more severe, or remain at the same level. In severe cases of Crohn's disease, inflammation can lead to the formation of perforation of the intestinal wall (perforation), the formation of fistulas, which requires immediate surgical intervention. If any of the above symptoms appear, as well as weight loss, vomiting, fever, weakness, joint pain or eye inflammation, the patient should immediately consult a doctor. This means that the previous treatment does not give the desired result.
Ulcerative colitis, as a chronic disease, increases the risk of colon cancer, so even if the patient feels better or has no symptoms at all, he should visit his doctor regularly. Endoscopic examination should be carried out at least once a year , and more often if the condition worsens or changes in the clinical course. It is necessary for the patient to be employed—free from work associated with business trips, night shifts, irregular meals, and emotional overload. Spa treatment for patients with ulcerative colitis and Crohn's disease is not indicated!
What is the treatment for ulcerative colitis and Crohn's disease?
For ulcerative colitis and Crohn's disease, various classes of drugs are used, primarily 5-aminosalicylic acid drugs - Salofalk , Pentasa, Mezavant, Asacol, systemic and topical glucocorticoids (prednisolone, budesonide), immunosuppressants (azathioprine) and biological drugs (Remicade, etc. .). Depending on the location and severity of the inflammatory process in the intestines, medications are used in the form of tablets, suppositories, enemas or foam. The choice of drug and dose depends on the severity of UC and CD, and should always be made by the attending physician. We must remember the need for long-term (years) maintenance therapy, that is, constantly taking small doses of 5-ASA drugs even in the absence of symptoms! Maintenance therapy reduces the frequency of exacerbations of the disease and improves its course, and also prevents the development of colon cancer.
IBD and pregnancy For women of childbearing age, these diseases are not a contraindication for pregnancy. In some patients, pregnancy can lead to an exacerbation of the disease, in others, on the contrary, it can improve its course. 5-ASA medications and hormones can be used before, during and after pregnancy.
Nutrition of patients with IBD - should special diets be followed? Nutrition for patients suffering from ulcerative colitis and Crohn's disease presents significant difficulties, both for the doctor and for the patient. There are no specific dietary recommendations for nutrition for these diseases. During remission, with good health and no diarrhea, the nature of the diet does not differ from the usually recommended healthy, nutritious diet. Some evidence suggests that during an exacerbation, milk and dairy products are poorly tolerated, which may require their exclusion from the diet. For diarrhea, to prevent its worsening, a diet low in dietary fiber is recommended.
General characteristics of the diet in the phase of severe exacerbation of the disease.
The content of fats and carbohydrates is limited; protein content is normal or slightly increased. A diet with a reduced content of table salt, with a sharp limitation of mechanical and chemical irritants of the mucous membrane of the gastrointestinal tract. Products and dishes that enhance the processes of fermentation and putrefaction in the intestines are excluded, in particular milk, coarse fiber, spices and all dishes that stimulate bile secretion, secretion of the stomach and pancreas. The diet is fractional - 5 - 6 times a day. Culinary processing. All dishes are pureed and cooked boiled or steamed. Recommended products and dishes: - bread and bakery products: crackers from white wheat bread, not toasted; - soups - in vegetarian, low-fat meat or fish broth with the addition of mucous infusions (rice, buckwheat, oatmeal, wheat flour), steamed or boiled meat or fish dumplings, meatballs, egg flakes, boiled and pureed meat, which is added together with mucous decoctions; - meat and fish dishes: lean and lean varieties (beef, veal, poultry) in the form of steam cutlets, quenelles, meatballs, boiled meat soufflé - minced meat is passed 3-4 times through a meat grinder with a fine grid. Only fresh (not frozen) and low-fat varieties of fish (pike perch, bream, carp, cod, navaga, etc.) are allowed. The technology for preparing fish dishes is the same as for meat dishes; - eggs and egg products: eggs (no more than 1 egg per day) are added to dishes; - milk and dairy products: fresh cottage cheese (preferably precipitated with calcium salts - calcined) in pureed form. Whole milk – according to tolerance; - cereals and pasta: pureed porridges made from rice, oatmeal, buckwheat, semolina and other cereals are prepared in water or in low-fat meat broth. - fats: fresh butter is added to dishes; - drinks and juices: weak tea, juices in the form of jelly, fruit and berry jelly, decoction of dried black currants, blueberries, bird cherry. Prohibited: fresh bread, vegetables, herbs, legumes, fruits, berries in their natural form, mushrooms, whole milk, sauces, spices, snacks, eggs in their natural form, sweets, confectionery, honey, jam, carbonated drinks, cold dishes.
| Approximate one-day diet menu for patients with inflammatory bowel diseases in the acute phase |
| 1st breakfast: boiled fish, mashed potatoes, pureed rice porridge with the addition of “DISO” Nutrinor mixture,” tea |
| 2nd breakfast: calcined cottage cheese (100 g) |
| Lunch: mild grated cheese (30 g), pearl barley soup in meat broth with grated carrots, meatloaf with grated buckwheat porridge, apple jelly |
| Afternoon snack: rosehip decoction (1/2 cup), white omelette |
| Dinner: boiled tongue with carrot puree, calcined cottage cheese |
| At night: kefir (1 glass) |
| For the whole day: white bread – 300 g, sugar – 50 g, butter – 10 g, fruits, berries – 300 g |
In the phase of subsiding exacerbation, they switch to a full diet with a normal content of proteins and fats, a decrease in carbohydrates with a moderate restriction of table salt. Avoid foods and dishes that enhance the processes of fermentation and putrefaction in the intestines, as well as active stimulants of gastric secretion. The diet is divided: 5-6 times a day. Culinary processing. Dishes are pureed, cooked boiled or steamed. Soups are pureed or with finely chopped vegetables and well-cooked cereals. Individual dishes can be baked, but without a rough crust.
Recommended products and dishes: - bread and bakery products: day-old wheat bread, dry biscuit, dry “Maria” cookies (total bakery products no more than 200 g per day); - soups: prepared in water, weak low-fat meat or fish broth with well-cooked cereals, noodles, finely chopped vegetables (with the exception of white cabbage); - meat and fish dishes: from meat and lean fish (non-old and lean beef, veal, chicken, turkey, rabbit, pike perch, pike, navaga cod) minced cutlets, meatballs, dumplings, soufflés, boiled or steamed rolls are prepared form; — eggs and egg products: soft-boiled eggs (1 piece per day) or as additives to dishes; egg white omelettes, meringues, snowballs; - milk and dairy products: milk only in limited quantities in dishes, fermented milk drinks - kefir, acidophilus, acidophilus milk, fermented baked milk, yogurt, etc. Freshly prepared cottage cheese (preferably calcined), natural, in the form of curd mass, curd steam puddings; - vegetables and herbs: zucchini, pumpkin, carrots, green peas and a limited amount of potatoes are cooked boiled and pureed; a steamed vegetable soufflé from pureed vegetables is used. Ripe tomatoes in their natural form - no more than 100-150 g per day; — fruits, berries, sweets: sweet varieties of berries and fruits (except melons, watermelons, apricots and plums) in the form of mashed compotes, jelly, jellies, mousses and various juices; baked apples, pears, preserves and jams from sweet varieties of berries and fruits; if well tolerated, strawberries, sweet ripe apples and pears can be consumed raw in limited quantities (up to 150 g); — cereals and pasta: rice, buckwheat, oatmeal, rolled oats, semolina and other cereals in pureed form as side dishes, porridges, casseroles (without crust); vermicelli, noodles, small pasta - in soups, as side dishes and casseroles. It is advisable to add dry composite protein mixtures (for example, “DISO” Nutrinor”) to porridges in the amount of 2 tablespoons in order to increase the protein content in dishes; - fats: unsalted butter is added to prepared dishes and to the table, but not more than 10 g per meal; — snacks: mild cheese, Russian, Yaroslavl, etc.; doctor's sausage, pate sausage, veal sausage, soaked herring, jellied meat, jellied tongue; — sauces and spices: sauces based on meat, vegetable and fish weak broths with dill, parsley leaves, milk bechamel sauce with the addition of a small amount of sour cream, fruit sauces; cinnamon can be used; — drinks and juices: tea with milk, rosehip decoction, weak black coffee with milk; fruit and berry sweet juices, vegetable juices (not canned) half and half with water. Prohibited: black bread, baked goods and pastry products; white cabbage, cucumbers, peas, beans, lentils, canned meat, fish, vegetables; fatty meats and fish; fried foods; strong coffee, whole vegetable juices; carbonated and cold drinks; ice cream, whole milk, cream, sour cream in natural form; chocolate and chocolate candies.
| Approximate one-day diet menu for patients with inflammatory bowel diseases in remission |
| 1st breakfast: rice milk porridge with the addition of “DISO Nutrinor” mixture, steamed protein omelette (from 2 eggs), tea with milk |
| 2nd breakfast: calcined cottage cheese (150 g) |
| Lunch: meat broth soup with cauliflower, boiled meat with boiled rice, fresh apples |
| Afternoon snack: boiled meat, rosehip decoction (200 g) |
| Dinner: baked curd pudding, steamed meatloaf with stewed carrots and green peas, tea with milk, fresh fruits (or berries) |
| At night: kefir (1 glass) |
| For the whole day: white bread – 300 g, sugar – 40 g, butter – 10 g |
How do you know which foods you tolerate well and which you don’t? A great help in answering this question is keeping a food diary, which daily reflects all the foods and dishes that were consumed during the day, and also notes changes in well-being. The frequency and nature of stool, the intensity of abdominal pain, and the presence of nausea must be indicated. One food that is often poorly tolerated by patients with IBD is whole milk. This occurs due to a deficiency of the lactase enzyme, which is produced in the small intestine and breaks down milk sugar - lactose. Lactase deficiency is often observed during exacerbation of both Crohn's disease and ulcerative colitis.
Types of malnutrition in IBD Malnutrition often occurs both during exacerbation of UC and CD , and in the remission phase. Loss of body weight is observed in more than half of patients. The vast majority are deficient in protein, iron, folic acid, cyanocobalamin (vit. B12), calcium, magnesium, potassium, vitamin D, copper and zinc. Malnutrition significantly complicates the treatment of patients, especially young patients, who need energy and microelements not only for the functioning of the body, but also for growth and development. There is a wide range of enteral nutrition formulas available that can be used to provide nutritional support to patients with ulcerative colitis and Crohn's disease. The choice of a particular mixture can be determined both by the characteristics of its composition and by the economic capabilities and taste preferences of the patient himself. The most commonly used mixtures are “Clinutren”, “Nutrizon”, “Nutricomp standard”, “Nutrien standard”, “MD mil Klinipit”, “Modulen IBD” and others. “M A dry complete balanced mixture based on casein has been specially developed for patients with IBD; it contains proteins, fats and carbohydrates in an optimal ratio, as well as all the necessary vitamins, macro- and microelements.
Herbal medicine for inflammatory bowel diseases The use of medicinal herbs is possible as an adjuvant therapy for patients with ulcerative colitis and Crohn's disease. Correct use of herbal medicine is possible only with an established clinical diagnosis of the disease. Dose selection is the doctor’s task; it can vary at the beginning of treatment and over the course of the disease.
Drugs used for the treatment and prevention of anemia in patients with ulcerative colitis and Crohn's disease at the rehabilitation stage:
Collection No. 1. Ingredients: St. John's wort herb 3 parts, nettle flowers 2 parts, blackberry leaves 2 parts. Method of preparation: chop everything, mix well, pour in 3 cups of boiling water, leave in a thermos for 3 hours, strain. Application: drink 1 glass 3 times a day hot. Collection No. 2. Ingredients: equal parts nettle leaves and birch leaves. Method of preparation: brew two tablespoons of the mixture with 1.5 cups of boiling water, leave for 1 hour, strain, add half a glass of beet juice. Application: drink 3-4 times a day, 20 minutes before meals. The course of treatment is 8 weeks. Collection No. 3. Ingredients: leaves of stinging nettle, flowering tops of buckwheat, leaves of angustifolia in equal parts. Method of preparation: brew three tablespoons of the mixture with two glasses of boiling water, leave for 3 hours, strain. Application: drink 3-4 times a day, 20 minutes before meals. The course of treatment is 6-8 weeks. Collection No. 4. Ingredients: nettle leaves, yarrow inflorescences, dandelion root in equal parts. Method of preparation: brew one tablespoon of the mixture with 1.5 cups of boiling water, leave for 3 hours, strain. Application: drink the infusion a day in 3-4 doses 20 minutes before meals. The course of treatment is 6-8 weeks. Collection No. 5. Ingredients: white chrysanthemum grass, tricolor violet grass, wild strawberry leaves (equal parts in total). Method of preparation: brew two tablespoons of the mixture with a glass of boiling water, boil for 10 minutes, leave for 3 hours, strain. Application: drink 2-3 times a day, 10 minutes before meals. The course of treatment is 4-6 weeks. Decoction of herb angustifolia. Method of preparation: pour 15 g of herb with a glass of water, boil for 15 minutes, leave for 1 hour. Application: drink 1 tablespoon 3-4 times a day before meals. A decoction of red clover inflorescences. Method of preparation: pour one teaspoon of inflorescences with 1 glass of hot water, boil for 5 minutes, strain. Application: drink 1 tablespoon 4-5 times a day. Infusion of wild strawberry leaves. Method of preparation: one tablespoon of dry chopped leaves (you can use a mixture of herbs and roots) and pour 1 glass of boiling water, leave for 1/2 hour, strain. Application: drink 1 glass 1-2 times a day for 1-2 months.
Medicines used for intestinal dysbiosis and flatulence in patients with ulcerative colitis and Crohn's disease at the rehabilitation stage:
Collection No. 1. Ingredients: St. John's wort herb, marshweed herb, yarrow herb in equal parts. Method of preparation: infuse three tablespoons of the mixture in 1 liter of boiling water for 2 hours, strain. Application: drink 1/2 glass 4-5 times a day. Collection No. 2. Ingredients: peppermint leaves, fennel fruits, cumin fruits, anise fruits equally. Method of preparation: brew two teaspoons of the mixture with a glass of boiling water, leave in a tightly sealed container for an hour, strain. Application: drink 1 glass of infusion in small sips in several doses throughout the day. Collection No. 3. Ingredients: peppermint leaves 20 g, chamomile flowers 30 g, calamus rhizome 15 g, fennel fruits 15 g. Method of preparation: infusion. Application: drink 1/2-3/4 cup as a warm infusion 3 times a day after meals. Collection No. 4. Ingredients: cinquefoil rhizome - 25 g, blueberry leaves - 20 g, blueberry fruits - 20 g, chamomile inflorescences - 55 g. Method of preparation: leave one tablespoon of the mixture for 6 hours in a glass of cold water, cook for 5-7 minutes, strain . Application: drink the entire infusion in small sips throughout the day. The course of treatment is at least 2 weeks.
Drugs used to improve vitamin and mineral metabolism in patients with ulcerative colitis and Crohn's disease
Collection No. 1. Ingredients: the whole lingonberry plant and the whole wild strawberry plant in equal parts. Method of preparation: pour one tablespoon of the mixture into 1 glass of water, bring to a boil, strain, add honey to taste. Application: drink a hot glass 3-4 times a day. Collection No. 2. Ingredients: rowan fruits 7 parts, nettle leaves 3 parts. Method of preparation: brew one tablespoon of the mixture with 2 cups of boiling water, boil for 10 minutes, leave for 4 hours in a tightly sealed container in a cool, dark place, strain. Application: drink 1/2 glass 3 times a day. Collection No. 3. Ingredients: rose hips, raspberry leaves, currant leaves, lingonberry leaves in equal parts. Method of preparation: brew two tablespoons of the mixture with a glass of boiling water, boil for 10 minutes, leave in a tightly sealed container until cool, strain, add sugar or honey to taste. Application: drink 1/2 cup 2 times a day. Collection No. 4. Ingredients: rose hips 3 parts, lingonberry fruits 2 parts, nettle leaves 3 parts. Method of preparation: mix the crushed raw materials well. Brew two tablespoons of the mixture with a glass of boiling water, leave for 3-4 hours, strain. Application: drink a glass 2-3 times a day.
Do you need help fighting ulcerative colitis and Crohn's disease? Are you a family member or loved one of a patient with ulcerative colitis or Crohn's disease?
Contact the Interregional public organization to support patients with ulcerative colitis and Crohn's disease "Trust".
"Trust" society in Stavropol: Igor Sergeevich Klushin, tel.: +7, email address: K [email protected] com.
All answers to the questions of patients and their attending physicians about new, modern and effective methods of treatment for ulcerative colitis and Crohn's disease, as well as for any other diseases of the digestive system, can be obtained at a consultation with Doctor of Medical Sciences, Professor Vladimir Vasilievich Pavlenko in Medical center "HEALTHY FAMILY" at the address: Stavropol, st. Tukhachevsky 19/3; tel.
Tags: Crohn's disease, ulcerative colitis
Traditional medicine in the treatment of ulcerative colitis
It is strictly not recommended to try to treat ulcerative colitis with “folk” remedies and alternative medicine. Considering the severity of the disease and the general danger it poses to the human body, all actions must be performed under the supervision and with the approval of a doctor.
Remember, even chronic diseases are not a death sentence, but a guide to action. Competent and timely diagnosis, professional consultation from highly qualified doctors and a personalized approach to therapy are the key to successful treatment and further fulfilling life.
You can make an appointment with a gastroenterologist at the Naedine Clinic by phone in Kirov: (8332) 32-7777 or through the form on our website.