Symptom complex
Symptoms of Barrett's esophagus correspond to severe manifestations of gastroesophageal reflux disease. Common patient complaints include:
- Unpleasant scratching sensations in the larynx, soreness. It usually occurs after eating.
- Heartburn is a burning sensation in the epigastric (epigastric) zone, spreading up the esophageal tube. It may bother you not only after drinking coffee, fried foods, or fatty foods, but also on an empty stomach.
- Belching is an intense accumulation of gases in the stomach and their release through the oral cavity. The symptom is accompanied by a bitter-sour taste in the mouth, particles of undigested food (regurgitation).
- Heaviness and pain in the epigastric region. The pain is localized in the cardia area (at the junction of the stomach and esophagus), and can radiate under the scapula.
- Dyspeptic syndrome - heaviness, a feeling of fullness, difficulty digesting food, accompanied by cutting pain, “rumbling” in the stomach.
- Odynophagia (painful swallowing of food) and dysphagia (sensation of a foreign object in the throat, “stuck” food).
- Lack of appetite is caused by unpleasant symptoms during and after eating. The result is weight loss.
- Decreased performance, muscle weakness, slowed brain activity. These signs are provoked by a malabsorption of food ingredients, as a result, a deficiency in the body of glucose, vitamins, and minerals.
Symptoms intensify with physical activity, in a horizontal position of the body after eating, and when bending the torso.
Important! The manifestation of disorders of the digestive processes is a reason to contact a gastroenterologist and undergo an examination. Ignoring the symptoms of GERD leads to deformation of the mucous membrane at the cellular level, further malignancy
Diagnosis of gastritis
Chronic gastritis can occur without any clinical manifestations. In such cases, the diagnosis is made based on the results of laboratory and instrumental examinations:
- General blood analysis.
- General urine analysis.
- General stool analysis.
- Fecal occult blood test.
- Blood chemistry.
- Detection of Helicobacter pylori infection.
- FGDS, or gastroscopy, is the main method of confirming the diagnosis, making it possible to clarify the variants of gastritis and the presence of Helicobacter pylori infection. Subjectively, patients perceive gastroscopy as an uncomfortable diagnostic method, therefore, for your convenience, GUTA CLINIC offers to undergo gastroscopy in your sleep - diagnostics of the condition of the gastric mucosa and analysis for Helicobacter pylori infection without pain and discomfort.
- We also recommend that you undergo an ultrasound of the liver, pancreas, and gallbladder - studies necessary to diagnose concomitant pathologies.
Features and risks
Intestinal metaplasia occurs:
- complete small intestine;
- incomplete colon.
The forms differ from each other in their tendency to malignancy. The first focal type is not precancer, since the altered cells retain their functions. The second type tends to become malignant due to impaired cellular differentiation, which is similar to dysplasia.
The danger of metaplasia lies in the difficulty of differentiating the disease due to the lack of specific signs. The clinical picture is fully consistent with the symptoms of focal pathology that caused cell atrophy. For example:
- In the chronic stage of gastritis with high acidity, “hunger” pains, increased heartburn, and “night hunger” appear.
- With an ulcer - clearly localized pain on an empty stomach. Symptoms will worsen in spring and autumn.
- With reflux syndrome with the reflux of intestinal contents into the stomach - a bitter taste in the mouth, widespread pain, vomiting.
- When a bolus of food is expelled from the stomach back into the esophagus, there is a strong burning sensation in the digestive tract, sour belching.
The only reliable method for diagnosing focal disease is fibroesogastroduodenoscopy, performed simultaneously with a biopsy. With its help, the stomach and intestines are carefully examined and the type of irritant, the localization of the tumor, the prevalence of the focal form are determined, and the malignancy of the process is confirmed or refuted.
Forms of gastritis
Depending on the localization of inflammation in a particular part of the stomach, there are:
- Antral gastritis.
- Gastritis of the body of the stomach (fundic).
- Pangastritis (diffuse gastritis).
Depending on the cause of the disease, chronic gastritis can take the following forms:
- Autoimmune gastritis (type A).
- Helicobacter (type B).
- Chemical or reflux gastritis (type C).
Special forms of gastritis include radiation, lymphocytic, granulomatous, eosinophilic gastritis. Recently, carditis has been additionally distinguished - inflammation in the cardiac part of the stomach, as well as atrophic gastritis.
Atrophic gastritis is a form of chronic gastritis with thinning of the mucous membrane, a decrease in the number of glands and secretory insufficiency. In 50% of cases, atrophic gastritis is combined with elements of structural restructuring of the mucous membrane (intestinal metaplasia).
The main cause of atrophic gastritis is considered to be contamination with the bacteria Helicobacter pylori. Atrophic gastritis can be localized in different parts of the stomach; it is this form that most often leads to the development of stomach cancer.
Possible complications
Improper treatment or its complete absence can lead to the development of serious complications, including the development of neoplasia and dysplasia of the patient’s stomach, dysfunction of the epithelium and atrophy of the glands. When microorganisms settle, a necrotic focus of inflammation develops, which is chronic in nature. It leads to the gradual degeneration of tissues, which are eventually replaced by diseased cells.
Stomach cancer is an oncological process that affects the mucous membrane and deeper layers of this organ
The presence of other pathogenic microorganisms that can synthesize carcinogenic substances can also provoke an acceleration of the development of neoplasms. To avoid serious complications of the pathology, it is necessary to carry out timely diagnosis and, accordingly, treatment.
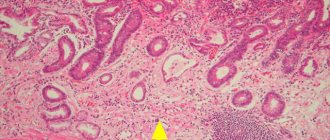
Pictured is stomach cancer
Intestinal metaplasia - treatment
To properly begin treatment, the doctor must get a complete picture of how widespread intestinal metaplasia is in the digestive system. To do this, endoscopy is performed. Once the diagnosis is confirmed, the doctor will recommend various treatments to reduce the progression of intestinal metaplasia.
If an H. pylori infection is suspected, your doctor will prescribe a course of antibiotics, including:
- amoxicillin;
- metronidazole;
- clarithromycin;
- tetracycline.
Antibiotic treatment usually lasts about 2 weeks.
The doctor may also recommend medications that reduce acidity.
Certain dietary changes can prevent intestinal metaplasia. These usually involve eating a diet rich in natural foods such as vegetables, fruits, nuts and whole grains. These foods contain nutrients and antioxidants.
People who have gastrointestinal disorders such as GERD should avoid fried, fatty or spicy foods. Salty foods may also be a culprit in intestinal metaplasia. Reducing salt intake helps prevent intestinal metaplasia.
Main symptoms
One of the main threats of this disease is its practically asymptomatic course.
In the early stages, when treatment is particularly successful, the disease manifests itself as minor discomfort, which usually no one pays attention to.
The situation is worsened by the fact that metaplasia usually develops against the background of chronic gastritis or ulcers, so patients mistake the signs for symptoms of existing diseases.
The main signs of gastric metaplasia:
- Nausea or vomiting.
- Burning feeling in the stomach.
- Feelings of hunger appear in the evening and at night.
- Heartburn and bitterness in the mouth.
- Periodic pain in the side.
- Loss of appetite.
- Weight loss.
In most patients, symptoms appeared irregularly and without great intensity. This significantly complicates the diagnostic task and also leads to significant progress of the disease.
Development mechanism
Metaplasia of the esophagus develops as a result of long-term systematic reflux of food and hydrochloric acid from the stomach into the esophagus. The aggressive effect of acid deprives the squamous cell epithelium of the ability to regenerate, and it is replaced by columnar cell epithelium, characteristic of the intestinal mucosa.
The formation of Barrett's esophagus can be caused by other forms of pathological changes in the epithelium:
- dysplasia - mutation and uncontrolled division of epithelial cells;
- erosions – superficial defects of the mucous membrane.
The key reason for the transformation of epithelial cells is gastroesophageal reflux disease (GERD) with severe dysfunction of the cardiac sphincter - the sphincter (valve) that closes the stomach to prevent the reflux of its contents in the opposite direction. There are three stages of pulp failure:
- Stage I – the valve closes 2/3 (relative to healthy function);
- Stage II - the sphincter closes by 50%, prolapse forms - the mucous membrane shrinks into folds that partially extend into the lumen of the esophagus;
- Stage III - the sphincter does not close, the stomach loses its ability to hold food.
Due to the prolonged relaxed state of the cardiac valve, hydrochloric acid constantly enters the esophagus, destroying the squamous epithelium. As a result, a precancerous condition develops - metaplasia of the esophageal mucosa, which in 3 cases out of 100 turns into adenocarcinoma.
The root causes of Barrett's syndrome are factors that provoke the development of GERD:
- eating habits - excessive passion for coffee, citrus fruits, excess fatty foods, hot seasonings and spices in the diet;
- alcohol and nicotine addiction;
- incorrect self-medication with NSAIDs (non-steroidal anti-inflammatory drugs);
- obesity.
Reflux is common in pregnant women and people with chronic constipation. Barrett's esophagus develops as a complication of duodenal ulcer, gastric ulcer, gastrinoma (a hormonally active gastrin-producing tumor of the pancreas).
Recent research from Columbia University Medical Center refutes the formation of Barrett's esophagus due to genetic predisposition.