One of the dangerous and insidious diseases in young children is rotavirus infection. According to WHO, the mortality rate from it is 30%. The symptoms are similar to those of many other diseases: food poisoning, intestinal upset, cholera and others. Therefore, if parents try to make a diagnosis on their own, in most cases they are mistaken. Failure to see a doctor in a timely manner or treating “diarrhea” with home remedies can result in tragedy. What is the disease for which vaccination is included in the national calendar of the USA and some European countries?
What are rotaviruses
Rotaviruses are a group of viral particles that are similar in morphological and antigenic characteristics. These are RNA viruses with a 3-layer shell of protein molecules. The particles got their name because of their similar appearance to a wheel (in Latin the word “wheel” is translated as “rota”).
How is rotavirus disease transmitted?
The main source of infection is a sick person. The virus is transmitted through the “hand-to-mouth” route. Through the patient's unwashed hands, children's toys, dishes, food and household items contaminated with viruses, the infectious agent enters the body.
Next comes the incubation period of rotavirus infection: the “wheel” virus enters the small intestine and begins to multiply in the cells of the mucous membrane. At the first sign of illness, billions of viruses begin to be excreted in the feces. On the 7th-10th day of the disease, virus release ends. The favorite time of year for this viral infection is autumn and winter. The virus is highly contagious, so it spreads quickly in children's institutions.
What's interesting...
Scientists, based on many years of observations, claim that rotavirus activity increases shortly before influenza outbreaks.
Routes of transmission
Rotavirus infection is transmitted from a sick person in several ways:
- fecal-oral;
- contact and household;
- airborne.
At the onset of the disease, the feces of an infected person contain up to 1011 particles of rotavirus. After about a week, their number decreases, but the person remains a source of infection for almost a month.
What factors influence the transmission of the virus? These are: water, food, household items. When the pathogen enters the aquatic environment, especially into water supply systems, epidemic situations may occur. Among food products, the most dangerous are dairy and meat products, raw vegetables and fruits. The hygienic condition of kitchen equipment, household items, and cleanliness of hands are of great importance.
How can a child become infected?
There are certain conditions under which a child may get this infection. The occurrence of the disease will be facilitated by:
- Irregular and inadequate nutrition of the child;
- Poor hygienic and sanitary conditions in which the child and his family live;
- The child eating low-quality or stale foods;
- Presence of stomach and intestinal diseases;
- The presence of immunodeficiency conditions (the child often suffers from colds or is often treated with antibiotics)
The source of infection for rotavirus disease is a person who already has this disease. It is dangerous to others from the appearance of the first symptoms until the end of the disease (5-7 days).
This infection is transmitted through the digestive system. A child can become infected while swimming in a pond where there is rotavirus in the water. Infection can occur through dirty hands, dishes, towels, napkins, toys and other items if they were used by a sick person. The disease can also occur in a baby when consuming foods that contain rotavirus - most often these are various dairy products.
Rotavirus infection most often occurs in autumn or spring. A person can get this disease several times during his life.
From the moment of infection to the appearance of vomiting, abdominal pain or diarrhea in the child, it takes from several hours to several days.
Interpretation of child tests by pediatricians online
cost of service: 500 rubles
Order
The pediatrician will interpret the tests during an online call using the Zoom or WhatsApp application.
- detailed explanation from the pediatrician.
- an alternative opinion from a competent specialist in interpreting the analyses.
- the opportunity to ask questions to the doctor regarding test results.
Who's at risk
The main risk group is children aged six months to five years. During this period, they manage to get sick with rotavirus up to five times. 90% of older children have antibodies to the infection in their blood, which indicates a previous illness.
Rotavirus infection easily penetrates the body - if a person does not have immunity to it, the probability of getting sick is almost 70%. Re-infection is also possible, but how long the immune response to rotavirus lasts and when secondary infection can occur has not been established.
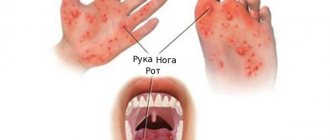
Distinctive features of rotavirus and dysentery (gastroenteritis)
Since the virus affects the epithelium of the small intestine, the disease is characterized by the same symptoms as many infectious diseases. But pediatricians and infectious disease specialists are able to recognize and distinguish the main signs.
When collecting information, symptoms such as nausea, heartburn, loss of appetite are not taken into account; they are relevant for any infection.
But the nature and course of vomiting and diarrhea are significantly different.
Vomit
With rotavirus infection, vomiting in a child always occurs once, at the beginning of the disease, when the body temperature rises to 37.5°. With gastroenteritis, vomiting is usually repeated, bringing short-term relief, and occurs every hour. With bacterial damage to the mucous membrane, the gag reflex is activated even after drinking water, drinks, or when trying to eat.
With rotavirus, vomit in the form of remnants of stomach contents. With enteritis, they contain mucus, gastric juice, bile, which is thrown from the duodenum into the stomach. Sometimes streaks of blood may be found in the vomit.
Diarrhea
With rotavirus infection, diarrhea does not occur immediately. It is preceded by a deterioration in general condition, single vomiting, and a rise in temperature. And only after the manifestation of all these signs does loose, watery stool occur. In infants, yellow water-like stool may be seen. The frequency of stool depends on the degree of epithelial damage and the protective functions of the child’s body. The average duration of diarrhea is 3-4 days.
With a viral infection, there is never any admixture of blood in the stool. If a child has blood in his stool, even hidden blood, which was discovered during a laboratory test, this indicates a bacterial infection of the mucous membrane.
This is how rotavirus differs from an intestinal infection.
With gastroenteritis, diarrhea appears first or simultaneously with vomiting. The frequency of stool can reach once a day, and in severe cases even more often.
A lot of mucus, pus, blood, and undigested food remains are found in the stool.
Other distinctive features
The difference between an intestinal infection and rotavirus also lies in the degree of dehydration of the body.
With a viral infection, it develops gradually. To eliminate it, it is enough to give the child fluids in a timely manner and in full. If you follow a drinking regime, complications (convulsions, pneumonia, kidney failure) associated with fluid loss develop extremely rarely.
Acute gastroenteritis leads to severe dehydration of both adults and children, which rapidly develops from the first day of the disease. This condition requires emergency care and parenteral (intravenous) administration of rehydration solutions to replenish salts and water.
It should also be said about the general condition of the children:
- Rotavirus begins with a mild illness that increases gradually. The child is capricious, eats poorly, lethargic, inactive, and drowsy during the day.
- The bacterial infection begins acutely. The baby is completely exhausted, is in bed, lies with his eyes closed, it is difficult for him to speak, and there is increased sensitivity to light and sound stimuli. At high temperatures there may be a semi-fainting state.
The duration of rotavirus infection, which occurs in a mild form, is no more than 2-3 days; children are sick for a maximum of 5-6 days. Acute infectious diseases last at least 8-10 days with timely treatment, and in severe cases 2-3 weeks.
Treatment of rotavirus in most cases does not require hospitalization or specific treatment and goes away on its own.
In case of bacterial infections, children are taken to the infectious diseases department for examination, observation, and correct and timely therapy.
Rotavirus infection and poisoning have similar symptoms.
The patient complains of pain, discomfort in the stomach, he is tormented by vomiting and upset stool. These are the so-called local symptoms.
There are also general symptoms: weakness, fever, headaches. At the same time, the nature of the diseases is different, therefore the courses of treatment differ significantly from each other.
That is why, for correct diagnosis and prescribing competent therapy, it is important to know how to distinguish rotavirus from poisoning.
With the beginning of autumn and the onset of spring, many people are susceptible to attack by bacteria and viruses that cause colds, although outbreaks of rotavirus infection occur year-round. Symptoms of poisoning are somewhat reminiscent of rotavirus, or, as it is popularly called, “intestinal flu.” Both diseases are extremely dangerous due to dehydration, especially for a child. That is why it is important for any doctor to determine on the very first day that he is dealing with poisoning or rotavirus, and immediately begin treatment.
Causes of poisoning and rotavirus infection
Since the symptoms of the two diseases are similar, it is important to understand how to distinguish poisoning from rotavirus, which cannot be done without understanding the etiology of the disease.
One of the most important differences is that rotavirus usually enters the body through a carrier, that is, infection occurs with the virus. Bacteria also enter the body due to dirty hands or poor water containing pathogenic microorganisms.
In case of poisoning, it all begins with the entry of a toxin or bacteria into the gastrointestinal tract (shigella dysentery, salmonella and others). Insufficient heat treatment of foods and eating dirty vegetables and fruits can play a role. Poisoning is often caused by mushrooms, adulterated alcohol, chemicals and other toxic substances.
Although both illnesses can be severe, there are common and distinctive signs of the diseases, and it is important to distinguish between them as quickly as possible.
Doctors also call rotavirus infection rotavirus gastroenteritis, and it is one of the forms of acute intestinal infection. A person becomes infected either through a carrier of the infection, or becomes ill through the fecal-oral route, that is, through dirty water in which microscopic particles of feces from a patient with rotavirus are dissolved.
What other symptoms help us understand: is it rotavirus or poisoning?
Differences between rotavirus infection
The incubation period for rotavirus infection can last 5 days: suddenly a person feels pain in the stomach, which begins to shrink, spasm, vomiting, and stools become yellowish in color.
Popular signs are:
- Increased body temperature.
- General weakness.
- Body aches.
- Runny nose.
- Cough.
- Conjunctivitis.
Intestinal flu is especially painful in children: against the background of malaise, children become capricious, they refuse to drink and eat, cry incessantly and demand attention. Upon examination, the doctor may detect symptoms similar to a cold: redness in the throat and swelling of the mucous tissues. But with both poisoning and rotavirus, children are especially at risk of dehydration.
How long does the virus live
The pathogen has a fairly high viability - on various surfaces, depending on environmental conditions, it can retain its properties for up to a month, and in feces for up to six months. The virus is resistant to factors such as:
- high temperature (up to 60-70˚С);
- low temperature (withstands even freezing);
- ultrasonic influence;
- UV irradiation;
- antibacterial agents;
- fat solvents;
- chloroform and ether.
Rotavirus can be killed by boiling, treating with strong alkaline solutions or acids. The pathogen has increased sensitivity to ethanol (96˚), formaldehyde, and hydrogen peroxide.
Prognosis and prevention
The disease is dangerous if severe dehydration is allowed to develop. To protect young children from rotavirus gastroenteritis, specific prevention of rotavirus infection has been developed. This is a vaccine in the form of drops. The medicine is dripped into the child’s mouth and the procedure is repeated three times at intervals of a month. You can start vaccinating infants at 1.5 months, before that they have maternal antibodies against rotavirus in their blood.
Nonspecific prevention also plays a significant role:
- You need to wash your hands after transport, walking, using the toilet, and before eating.
- Boil water.
- If a carrier or sick person who can become a source of spread of infection is identified in the team, he must be isolated until he recovers.
- Proper nutrition of the mother and breastfeeding strengthens the child’s immune strength. It’s no wonder that formula-fed children are more likely to get rotavirus disease.
- In a family, a sick person should have separate dishes, a towel, and a bed. Cleaning should be done with the addition of disinfectants, and things should be washed at high temperatures.
How does infection occur?
Penetrating into the body through the oral cavity, rotavirus penetrates into the mucous membrane of the small intestine within half an hour. After just 1-3 days, changes begin in it: cells die and exfoliate from the surface of the intestine, food digestion processes are disrupted, absorption of substances and the functioning of enzymes deteriorate. At the same time, intestinal motor activity increases. Undigested residues accumulate in it, acids and other metabolic products are formed, and difficulties arise with the absorption of water. As a result, diarrhea and dehydration develop.
What can parents do before the doctor arrives?
Even before the doctor arrives, parents should start giving their sick child something to drink. You can try to do this in various ways. Some children drink well during illness using a spoon. Someone will have to slowly pour liquid into their mouth from a syringe. The main thing is not to rush and do it evenly and regularly - 5-20 ml every few minutes. If the baby continues to have nausea or vomiting, you need to make the intervals between drinks a little longer, but do not stop offering the patient something to drink. In addition to saline solutions, it is useful to drink dried fruit compote and chamomile decoction.
To reduce the symptoms of the disease, sorbents and preparations containing probiotics are used. Sorbents ensure binding and removal of the pathogen from the body. For this purpose, carbon, fibrous, mineral or synthetic sorbents can be used, which effectively sorb and remove from the body food decomposition products formed during enzymatic deficiency, help accelerate epithelial regeneration, reduce flatulence and pain, and also do not affect the composition of normal intestinal flora .
In some situations, enzymes may be used in treatment if the child has difficulty digesting food due to severe damage to the intestines and pancreas.
In addition to medications, it is important to pay attention to diet during illness. To prevent nausea, food should be given to the child in small quantities and more often. For about a month, you should exclude dairy products, fresh vegetables, fruits, pasta, baked goods, pastries, sweets, and fried foods from your diet.
Food is served to the patient boiled, stewed or baked without crust. The child should have such food for about a month, and then the diet can be gradually expanded.
If you rush and do not follow a diet, recovery will slow down. Complications may arise and chronic diseases of the liver, stomach, intestines or pancreas may develop.
An unpleasant surprise - rotavirus during trips and travels
Many stories have been told on the Internet about how rotavirus ruined a vacation while traveling abroad. This usually happens with small children, but cases are not excluded when the whole family spends several days, what is popularly called, “embracing the toilet.” One of these cases, although it ended happily, was not pleasant enough. Thailand. Vacation. Heat. A family with a 9-month-old child is admitted to the hospital. Diagnosis: rotavirus infection. It was not possible to combat dehydration with improvised means; it is difficult to explain to a child at this age that he needs to drink a lot. Therefore, for 3 days of vacation, instead of swimming in the sea and riding elephants, there were IVs and other treatment. It’s good that insurance was taken out that covered this “entertainment”, because the bill that was presented to the insurance company was about 100 thousand rubles.
Diagnostics
When making a diagnosis, take into account:
- Clinical picture: the infection begins 12 hours to several days after contact with the patient. The main symptoms are acute gastroenteritis (inflammation of the stomach and small intestine), fever, intoxication, and dehydration in severe forms.
- Epidemiological data - infection with rotavirus occurs in several people from the same team. When washing off surfaces, examining food debris, and feces, virus particles are detected using the PCR method.
- Laboratory data - blood test, urine test, stool microscopy. Stool culture and microbiological examination help to exclude other gastrointestinal infections - cholera, salmonellosis, dysentery, escherichiosis, enterovirus infection. From the fifth day of illness, specific antibodies to rotavirus are detected in the blood.
After examining the child, the doctor will be able to rule out acute poisoning, exacerbation of chronic pathology of the liver, stomach, pancreas, intestines, and other bacterial and viral infections.
Symptoms of rotavirus infection
Symptoms appear approximately 3-5 days after infection. As a rule, this happens very brightly and suddenly. Among them are:
- heat;
- chills;
- vomit;
- diarrhea;
- pain in the abdomen (especially in the navel area);
- dizziness;
- loss of appetite.
In some cases, the disease begins with sensations reminiscent of a cold: sore throat, nasal congestion, and a slight cough. After this, rotavirus infection manifests itself with intestinal symptoms and fever.
ON A NOTE! In most cases, rotavirus manifests itself as a monodisease. However, recently its combination with other infections has become increasingly common. This may be a viral-viral form of the disease, for example, with an enterovirus, or a viral-bacterial one (for example, with salmonella).
Possible complications8
Rotavirus infection poses the greatest danger to young children from the first days of life to 3-5 years and pregnant women:
- At an early age, intestinal flu is a deadly disease - severe dehydration of the body can lead to death.
- Dehydration caused by rotavirus gastroenteritis during pregnancy leads to the risk of miscarriage.
Possible complications of rotavirus infection:
- Pancreatitis, gastritis, enlarged pancreas.
- Intestinal inflammation.
- Hemorrhagic gastroenteritis.
- Acute renal failure.
- Circulatory disorders.
- Gasser syndrome.
- Necrotizing enterocolitis.
To minimize the risk of the disease and prevent the development of complications, it is important to promptly diagnose rotavirus infection and begin adequate treatment.
Treatment methods
In its normal course, rotavirus infection can be treated on an outpatient basis, at home, under the supervision of a pediatrician. Hospitalization is required if very severe intoxication is observed, which threatens rapid dehydration of the child’s body.
For treatment use:
- enterosorbents;
- antiviral drugs;
- symptomatic drugs, for example, antipyretics;
- probiotics;
- antibacterial drugs (if necessary);
- special solutions that replenish the loss of microelements.
The main goal of therapy is to stop fluid loss, remove toxins, and normalize intestinal functions.
The prognosis for mild to moderate disease is most often favorable.
Treatment12
Drug treatment for rotavirus infection is prescribed by a doctor. In most cases the following are used:
- To remove toxins: activated carbon, Smecta, Enterosgel.
- To restore the functions of the gastrointestinal tract: digestive enzymes (Festal, Somilase, Solizim).
- To reduce the temperature (in cases where it rises above 38 ºС): antipyretic drugs (Ibuprofen, Paracetamol).
- To relieve stomach pain: antispasmodics (No-Shpa, Enterofuril).
- To suppress bacterial infections that often accompany rotavirus gastroenteritis: antibiotics.
- To restore electrolyte balance: probiotics.
General recommendations:
- Drink small amounts of fluid frequently to prevent dehydration. You should drink clean boiled water, dried fruit compotes, berry fruit drinks, and unsweetened tea.
- The patient's menu should include light, quick-to-digest, protein-rich foods - dairy-free cereals, steamed poultry and fish cutlets, fruit and vegetable purees. From the patient’s diet it is necessary to exclude everything fried, smoked and salted, sweets, foods high in fats and carbohydrates, flour products (including pasta), millet and pearl barley porridges, milk and fermented milk products, spices, coffee, legumes (and other products , which can cause flatulence).
How dangerous is the infection?
Rotavirus infection primarily poses a danger to the child’s body, since the child has not yet developed resistance to dehydration, and it occurs faster than in an adult. In addition, according to experts, rotavirus, transmitted even in a mild form (especially repeated infections) can subsequently cause:
- gallbladder problems;
- secondary lactase deficiency;
- food allergies;
- functional disorders of the gastrointestinal tract.
In adults, the infection can cause complications from the endocrine and cardiovascular systems if they have chronic diseases, for example, diabetes mellitus, a tendency to blood clots. A healthy adult can contract rotavirus without consequences.
How to distinguish rotavirus from poisoning
Poisoning, unlike rotavirus infection, develops suddenly and very quickly. In this case, similar symptoms usually appear simultaneously in all people who ate the same foods. Rotavirus, which is a seasonal disease, in addition to digestive upset, is accompanied by fever and respiratory symptoms. The characteristic differences of this disease are grayish-yellow feces with a characteristic clayey consistency and very dark urine, sometimes mixed with blood.
Up to contents
Preventive measures
Prevention of rotavirus consists of strengthening the immune system and observing hygiene rules. Regarding infants, this also includes breastfeeding. In addition, there is a vaccination against rotavirus infection.
How does vaccination help?
Vaccination against rotavirus is already included in the National Vaccination Calendar of the USA, Germany, France and some other countries. In Russia this is just being planned, so for now it can be done on a paid basis; Only the wishes of the parents are enough. And here it is important not to miss deadlines - now we will explain why.
There are 2 vaccines against rotavirus: Rotarix (monovalent) and RotaTek (pentavalent). The RotaTek vaccine is available in our country (Manufacturer: Merck Sharp and Dome B.V., the Netherlands). It helps fight rotaviruses of serotypes G1, G2, G3, G4 and serotypes G containing P1A[8] (for example, G9). The vaccine is a drinking solution (not an injection).
According to the instructions, the vaccination course consists of three doses with an interval between doses of 4 to 10 weeks. And now, as promised, we pay attention to the deadlines. The first vaccination is given no later than 12 weeks from birth! That is, active immunization of children is carried out between the ages of 6 and 32 weeks.
Why can't you vaccinate after 32 weeks?
As mentioned above, the instructions stipulate that the course of vaccination should be completed at 32 weeks, and the child should receive the first dose no later than 12 weeks of age. The effect of the vaccine at later stages of the course of vaccinations has not been studied, and in the absence of data on effectiveness and safety, the drug cannot be used.
Another common question is why a vaccine is not developed to vaccinate older children or adults. Perhaps such a vaccine will also appear someday, but for now it is only possible to vaccinate children. Yes, it is understandable that the vaccine was primarily developed for those who suffer this infection the hardest: children in the first years of life. A child's weak immune and digestive system cannot cope with intoxication, which leads to a severe course of the disease and complications. 3 doses of the vaccine are the conditional 3 first “meetings” with the virus. If the virus is real, i.e. wild - the consequences of such contacts are unpredictable, but if it is vaccine - it is transferred almost unnoticed. As a result of the vaccine, the child acquires immunity. It is valid for up to 5 years, that is, precisely the period when rotavirus is especially dangerous for humans.
About rotavirus infection, as well as about other vaccinations that are not included in the National Calendar of the Russian Federation, see our video (narrated by allergist-immunologist Natalya Nikolaevna Nagornaya):
For all questions related to rotavirus and vaccination, you can contact the specialists of our center. Sign up for vaccination now.
Literature:
- Acute diarrhea in adults and children: a global perspective. Global practical recommendations of the World Gastroenterological Organization, 2012. 27 p. URL: https://www.worldgastroenterology.org/UserFiles/file/guidelines/acute-diarrhea-russian-2012.pdf (date of access: 10/08/2021, access mode - free).
- Tkhakushinova N.Kh. Rotavirus infection in children. Epidemiology and infectious diseases. 2012; 2: 56-59.
- Rotavirus gastroenteritis in children. Clinical recommendations of the International public organization “Euro-Asian Society for Infectious Diseases”, Interregional public organization “Association of Infectious Disease Doctors of St. Petersburg and Leningrad Region”, 2022.
- Rotavirus infection. URL: https://cgon.rospotrebnadzor.ru/content/63/531 (access date: 10/08/2021, access mode: free).
- Rychkova O.A., Grakhova M.A., Sagitova A.S. Rotavirus infection: possibilities of modern vaccine prevention. Medical advice. 2018; 17: 115-219.
- Mikhailova E.V., Shuldyakov A.A., Koshkin A.P., Levin D.Yu. Rotavirus infection in children: Textbook. Saratov: Saratov Medical University Publishing House, 2006; 80s.
- Khlynina Yu.O. Rotavirus infection in children. Medicinal bulletin. 2020; 2(78): 47-52.
- State Register of Medicines: Instructions for medical use of the drug Anaferon for children (lozenges). URL: https://grls.rosminzdrav.ru/Grls_View_v2.aspx?routingGuid=2ba954e0-47b6-4d93-a96e-d03cc7695d2c&t= (date of access: 10/08/2021, access mode - free).
- Nikolaeva I.V. Experience with the use of Anaferon for children in the treatment of acute respiratory viral infections with gastrointestinal syndrome and viral diarrhea in children. Literature review. Effective pharmacotherapy. Pediatrics. 2013; 1:8-12.
- Gorelov A.V. Acute intestinal infections in children: a pocket guide. M.: GEOTAR - Media, 2022, 144 p.
- Baranov A.A., Namazova-Baranova L.S., Tatochenko V.K., Vishneva E.A., Fedoseenko M.V., Selimzyanova L.R. et al. Rotavirus infection in children is an unresolved problem. Review of recommendations for vaccination. Pediatric pharmacology. 2017; 14(4): 248–257.
[January 26, 2022].
Chronic enteritis in adults - clinical symptoms, treatment
Enteritis is an inflammation (acute or chronic) of the small intestinal mucosa, characterized by dystrophic changes in the lining and dysfunction of the organ.
Signs of acute enteritis in children: loose stools, attacks of nausea, rumbling in the stomach, fever, dry skin, headache. The causes of this condition may be viruses, bacteria, toxic substances, allergic reactions to foods or medications. Causes of chronic enteritis in adults:
- autoimmune diseases;
- giardiasis;
- intoxication with chemical, toxic substances;
- overeating fatty foods;
- heredity;
- chronic gastrointestinal diseases;
- long-term use of medications;
- intestinal operations.
Predisposing factors include a sedentary lifestyle, abdominal trauma, poor circulation, and adhesions.
Forms of the disease
Doctors divided the disease into 3 forms according to severity:
- light;
- moderate severity;
- heavy.
The mild form is characterized by a slight deterioration in general condition, diarrhea up to 5 times a day. On the fourth or fifth day of the disease, the person recovers.
Next comes a moderate rotavirus infection. How many days does the body fight viruses? Over the course of a week, frequent bowel movements (up to 16 times a day), vomiting, weakness, fever, decreased blood pressure, and low pulse have been a concern.
A severe form of the disease occurs with severe intoxication, the patient suffers from repeated vomiting, defecation up to 20 times a day, with a large number of watery stools. Due to dehydration, kidney and heart failure develop. How long does rotavirus infection last with this variant of the disease? Due to the addition of bacterial flora, the disease has to be treated a little longer - up to 10 days.
If therapy is started in a timely manner, the prognosis is favorable. The body’s defenses actively fight against rotavirus infection, and in most cases this fight ends in the defeat of the “strangers”.
Recovery of the body after rotavirus infection is accompanied by weakness, indigestion, fatigue and takes 1-2 weeks.
Be vigilant - past rotavirus infection does not exclude the possibility of re-infection. Only partial immunity to the virus remains!
This is interesting
Sick animals do not pose a danger to humans, but the “king of nature” may well cause illness in his pet.