What is echogenicity
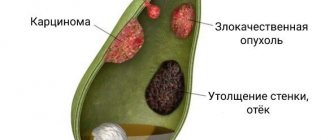
Often, when conducting ultrasound diagnostics, specialists are faced with hyperechoic formations in the gallbladder, which are not a disease, but only indicate the presence of pathologies in this organ. These are mainly tissues with a calcified structure or fatty deposits. To make an accurate diagnosis, additional examination is required.
On the monitor of ultrasound equipment, echogenicity appears as a white or light spot, which leads to a conclusion regarding the presence of compactions in this area. Structures can be point or linear, and also quite voluminous.
Why does echogenicity appear?
There are many reasons for the occurrence of hyperechoic formations in the gallbladder. They depend mainly on the general condition of the body, the size and area of localization of the formations. Most often, ultrasound reveals calcified structures, which can be single or multiple or have an acoustic shadow.
If microscopic calcifications are found, these are usually malignant tumors. Such pathologies occur with nephritis occurring in the chronic stage, injury and many other diseases. There is no liquid inside such seals, but their acoustic density is very high, so sound is poorly transmitted. Sometimes such structures can act as frame elements in organ tissues.
Causes of polyps
- Heredity and predisposition more often than other reasons lead to the formation of polyps. This may be due to the structure of the bladder mucosa - most often this is the so-called “launching pad” for the appearance of polyposis.
- Irregular and irrational nutrition, abuse of food containing cholesterol is also one of the unfavorable factors.
- Chronic cholecystitis, in which the flow of bile into the duodenum is impaired.
Despite the fact that adenoma and papilloma are benign formations, there is a possibility of their degeneration into malignant tumors. In addition, tumor particles entering outside the gallbladder can lead to the spread of polyps to other organs.
Who is at risk
The formation of atypical tissues in an organ, which is detected during ultrasound, is considered an echo-positive structure. The risk group for the occurrence of such seals includes patients with conditions such as:
- acute infections in the body;
- prolonged chemical or thermal effects on the organ;
- inflammation of the gallbladder;
- chronic diseases in the acute stage;
- poor diet and bad habits;
- insufficient physical activity;
- mechanical injury.
All these factors lead to the occurrence of pathology, so there is a need to carry out comprehensive diagnostics, treatment and preventive procedures.
There are several types of polyps in the gallbladder:
- Inflammatory polyps appear as a result of an acute reaction of the organ mucosa to the proliferation of granulation tissue.
- Cholesterol - the mucous membrane of the bladder changes due to cholesterol deposits and accumulations; This type is the most common. Despite the fact that the presence of such plaques does not pose a danger, the need for urgent surgical treatment causes debate among doctors.
- Papilloma is a benign tumor, which is characterized by the presence of papillae on the mucosa.
- Gallbladder adenoma is a benign formation that appears as a result of the growth of glandular tissue.
Gallbladder polyp.
Main symptoms
In the presence of a hyperechoic formation, symptoms largely depend on the degree of damage to the mucous membranes. Among the main signs of pathology, the following should be highlighted:
- fever, weakness, headache;
- weight loss, sleep problems;
- dizziness and severe irritability.
In addition, pain on the right side under the ribs, swelling, nausea and vomiting may appear. If such symptoms are present, diagnosis and treatment are required.
Treatment
Removing a stone from the bile duct cannot be done with medication or other non-invasive methods. The optimal method for diagnosing and treating choledocholithiasis is ERCP (Endoscopic retrograde pancreatic cholangiography). Using an X-ray contrast agent introduced through an endoscope, the condition of the biliary system can be assessed using a series of images. If the diagnosis is confirmed, the endoscopist surgeon immediately makes a decision on treatment. Large stones are crushed. When the area of the papilla of Vater narrows, it is dissected. The advantages of the technique are that there is no need to move the patient between examination and treatment procedures - everything takes place in one operating room, on one equipment, by one doctor.
If ERCP is impossible or ineffective, laparoscopic surgery is performed. Stones in the bile ducts are removed mechanically, after dissecting the wall of the duct. The gallbladder is also removed. In difficult cases, they resort to classical abdominal surgery.
Features of formation in the gallbladder
Detection of an area with increased density may indicate that it is:
- stone;
- cholesterol polyp;
- bile sludge
The stone is located in the lumen of the organ and provides an acoustic shadow. He is often agile when turning and taking deep breaths. However, it may be a hyperechoic nondisplaceable mass in the gallbladder.
A cholesterol polyp grows from the wall of the organ. It has increased density. This is a parietal hyperechoic formation in the gallbladder, which has a small diameter and even outline.
Bile sludge is the accumulation of thick bile sediment at the bottom of the organ. In this case, you need to conduct an additional ultrasound after taking choleretic drugs.
Types of polyps
Polypous formations of the gallbladder are as follows:
- Cholesterol polyps, benign in nature.
- Cholesterosis of the gallbladder, polypous form.
- True polyps of the gallbladder (adenomas).
- Malignant polyps.
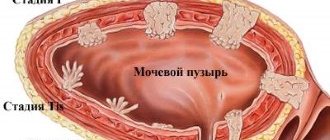
Cholesterol polyps
According to research results, from 45 to 70% of all gallbladder polyps are cholesterol in nature and do not require surgical intervention. According to various researchers, among patients who underwent removal of the gallbladder (cholecystectomy), from 39 to 63% had cholesterol polyps. Detected polyps 4 - 10 mm in diameter are benign cholesterol polyps, immobile, with an even contour, on a broad base, do not give an echo-shadow during ultrasound examination, most often single or multiple, without a blood supply.
Gallbladder cholesterosis
This is the most common morphological form of polypoid formations of the gallbladder and is observed in 42-99% of cases. Previously, cholesterosis was rarely observed, but with the advent of ultrasound examination, this pathology of the gallbladder began to be detected very often.
Cholesterosis is a benign, non-inflammatory disease in which multiple polypoid formations are observed in the wall of the gallbladder. Polypoid cholesterosis is characterized by small size (less than 10-15 mm) and slow growth.
Cholesterol polyps of the gallbladder, cholesterosis - accumulation of pure cholesterol and its esters and bile acids in the submucosal layer of the gallbladder wall in the form of outgrowths (polyps).
The causes of such polyps can be:
- general lipid metabolism disorders,
- violation of the contractile function of the gallbladder - stagnation of concentrated bile in it,
- changes in the composition of bile (dyscholia) produced by the liver,
- impaired lymph circulation in the walls of the gallbladder when it is inflamed.
Cholesterol polyps and gallbladder cholesterosis are not precancerous diseases. Cases of transition to malignant degeneration of polypoid cholesterosis have not been described.
The frequency of gallbladder polyps in men and women is almost the same, but polypoid cholesterosis is more common in men, and cholesterol polyps and adenomas are more common in women.
Gallbladder polyps are often asymptomatic (according to research results, up to 66%).
True polyps of the gallbladder
They are often combined with gallstones or inflammation. Only 9% of those examined had a healthy gallbladder (research data). These polyps belong to precancerous diseases of the gallbladder.
To clarify the nature of the polyp - cholesterol or true polyp, an ultrasound Doppler examination of the polyp is performed, determining the presence of blood supply in the leg of the polyp: with a cholesterol polyp it is absent, with a true polyp the blood supply is present. If a true gallbladder polyp is detected, an annual ultrasound examination is indicated.
Malignant polyps of the gallbladder
According to cholecystectomy data, they were found in persons over 60 years of age.
Gallbladder cancer is a rare disease, occurring in 1-2 cases per 100,000 people.
Polyps measuring more than 1.5-2 cm in the lumen of the gallbladder and their rapid growth of more than 2 mm per year are at risk and require dynamic monitoring. More often, malignant polyps of the gallbladder are diagnosed in an inoperable form.
Formations with acoustic shadow
During diagnostics, various foreign inclusions may be detected. Quite often, after an ultrasound examination, the report states “hyperechoic formation with an acoustic shadow.” It is formed from stones, dense and connective tumors.
Many people are interested in what a hyperechoic formation means. This is a fairly dense structure that reflects ultrasonic waves. In addition, when conducting a study, the specialist must find out whether there is an acoustic shadow behind the formation. Its presence indicates that the object under study is so dense that it does not transmit ultrasonic waves at all.
If the doctor detects a solid mass followed by an acoustic shadow, the first thing he thinks about is a gallstone. It is dense enough that ultrasonic waves do not pass through.
A shadow forms at the border of tissues that reflect ultrasound well. During exploration and passage through such very dense structures, the ultrasonic beam is almost completely interrupted and a reflection is formed. That is, such fabrics have high acoustic density.
Heterogeneous formation
This may indicate the presence of malignant or inflammatory processes in the body. A heterogeneous hyperechoic formation generally indicates that cysts are forming inside the organ. Tumors can change the structure of the gallbladder at any stage. To determine what a hyperechoic formation with a heterogeneous structure means, a comprehensive diagnosis is required.
It may also indicate inflammation. In a healthy person, the echostructure of the gallbladder is homogeneous and even. When performing an ultrasound examination, it is possible to determine the peculiarities of the functioning of this organ.
Symptoms of the disease
Often the disease is asymptomatic. Half of the patients experience only a feeling of discomfort in the right hypochondrium. Some patients experience heartburn and belching, and sometimes pain may occur. Soreness is a common symptom in cases where the polyp is localized in the narrowest place of the gallbladder - in the neck. If large in size, it can lead to blockage of the duct, which will cause stagnation of bile. As a result, the digestion process is disrupted, leading to belching, pain in the right hypochondrium, constipation, etc.
Formation with anechogenic inclusions
The echogenicity of tissues depends on the ability to absorb and reflect ultrasound passing through them. This is directly related to the characteristics of the organs. The less liquid is contained inside the object under study, the higher the degree of echogenicity. The absence of fluid indicates the lowest density, that is, anechogenicity.
A hyperechoic formation with inclusions generally indicates malignant processes in the body. Additional research may be required to more accurately indicate the type of echostructure and its danger.
Carrying out diagnostics
The main method for detecting a hyperechoic formation is ultrasound diagnostics. If such a compaction is detected, the cause of its occurrence must be determined. It is important to take into account the general condition of the body, as well as existing symptoms. To make an accurate diagnosis, additional studies may be required, which are prescribed by the doctor.
After the diagnosis, the doctor draws up a treatment plan. Treatment may be medication or surgery. If a small parietal hyperechoic formation is detected, which is not accompanied by pathological symptoms, constant monitoring of its condition through regular ultrasound is indicated.
Diagnostics involves the use of laboratory research techniques. To identify tissues with increased acoustic density, the following is prescribed:
- general blood analysis;
- Analysis of urine;
- biochemical research.
Based on the results of all these studies, a plan for subsequent diagnostic procedures is drawn up. In addition, an instrumental study may be required, which mainly includes:
- radiography;
- puncture biopsy;
- Ultrasound diagnostics;
- CT;
- MRI.
Typically, a hyperechoic formation is detected on ultrasound, where its structure is clearly visible. This is a safe, non-invasive, reliable method that helps detect stones, tumors and bile accumulation.
Radiography helps to accurately determine the location of the formation and its structure. Often used together with a contrast agent. Computed tomography is a reliable method of radiation diagnostics, based on obtaining a layer-by-layer image of a tissue or organ. MRI helps visualize deep-seated lumps. Often used to study inclusions in the brain. If all these methods confirm the presence of stones or lipoma, then a puncture biopsy is prescribed. The resulting tissues are sent for histology and cytology.
Features of treatment
Treatment of hyperechoic formation in the gallbladder is selected depending on the results of the study. If calcifications are detected, the doctor prescribes medications that help remove them. In particularly complex and advanced cases, surgery is indicated.
In the presence of compactions caused by various diseases, inflammatory and infectious processes, antibiotics are required. Benign and malignant tumors are treated with surgery and may also require chemotherapy. For multiple hyperechoic avascular formations, medical supervision is indicated.
Treatment of polyposis
First of all, nutritional correction is necessary. As a result of the disease, the amount of incoming bile is insufficient for digestion. But with the help of diet you can ease the work of the gastrointestinal tract. Fractional balanced nutrition in small portions, easily digestible foods will help prevent the occurrence of digestive system dysfunction.
As a rule, the most effective way to get rid of polyps is surgery. However, the question of the advisability of surgical treatment is decided only individually. Therapeutic tactics are based on observation of the patient, taking into account the structure and number of polyps, the presence of a pedicle, etc. If there is a formation with a pedicle, it is recommended to conduct an ultrasound every six months; in the absence of a pedicle, control studies should be done more often.
Drug therapy
Treatment largely depends on the underlying cause that provoked the appearance of a hyperechoic formation in the gallbladder. Medicines should be selected only by a doctor, taking into account the patient’s condition. If inflammation is observed in the body, then anti-inflammatory drugs are required, in particular, such as Ibuprofen or Ketorol.
Ibuprofen is an anti-inflammatory drug with an analgesic effect. Used for inflammation. The dosage and duration of administration depends on the severity of the pathology. It is worth remembering that the medicine has contraindications and can cause side effects.
"Ketorol" is an anti-inflammatory drug with analgesic and anti-inflammatory effects. It is used for fairly intense pain and inflammation in the body.
Additionally, you may need to take vitamin complexes that help strengthen the immune system and help fight various diseases.
Physiotherapeutic techniques
For hyperechoic round formations, physiotherapeutic techniques may be prescribed for treatment. They imply an effect on the body through:
- electric current;
- heat or cold;
- laser, infrared, ultraviolet radiation;
- ultrasound;
- magnetic field.
It is also possible to use hirudotherapy and massage. The main advantage of such methods is that they are effective and safe. This will help reduce the period of therapy for various pathologies and activate biochemical processes. As a result, recovery is accelerated.
Cryotherapy is based on the effect of fairly low temperatures on the body. It relieves pain, stimulates the immune system, eliminates inflammation and swelling.
Laser therapy is a biostimulation method based on the effect of laser on living tissues. It activates the most basic biochemical processes occurring in the body, promotes the regeneration of cells and tissues. Laser therapy improves blood microcirculation, accelerates the healing process of various lesions and eliminates inflammation.
Magnetotherapy is a modern method of influencing the body using a magnetic field. It promotes overall health, normalizes blood circulation and oxygen saturation. In addition, this technique improves the functioning of internal organs.
If a person has echogenic inclusions in the form of stones, then electrophoresis with antibiotics is often used to treat them. During the procedure, medications quickly penetrate the affected tissues, normalize blood circulation and promote the resorption of tumors.
Surgical methods for treating gallbladder polyps
Watch a video of operations performed by Professor K.V. Puchkov. You can visit the website “Video of operations of the best surgeons in the world.”
Today there are two main methods of surgical treatment of polyposis:
Puchkov K.V., Khubezov D.A., Puchkov D.K., Rodimov S.V. Minimally invasive laparoscopic methods for treating gallbladder diseases: a textbook for surgeons // Ryazan State Medical University of the Ministry of Health of Russia. - Ryazan: RIO RyazGMU, 2015. - 115 p.
Puchkov K.V., Puchkov D.K. SURGERY FOR GALLSTONES: laparoscopy, minilaparoscopy, single port, transanal access, simultaneous operations. - M.: ID "MEPRACTIKA-M", 2022, 312 p.
Patent. A method for temporary fixation of abdominal and pelvic organs during laparoscopic operations.
Laparoscopic gallbladder removal - single-port cholecystectomy
- Laparoscopic cholecystectomy - with this method, the intervention is performed using laparoscopic equipment through small incisions on the anterior wall of the peritoneum, through a puncture in the umbilical area or transvaginally. Today, laparoscopy is recognized as the “gold” standard in abdominal surgery. Among the advantages of this method, it is worth noting the excellent cosmetic result: only small incisions remain on the skin. The rehabilitation period is much shorter than with traditional surgical treatment. The patient begins to walk on the first day, and on the second day he is allowed to take liquid food. The operated patient usually leaves the clinic on the 2nd or 3rd day after the operation. A person can usually start work within 10-14 days.
- traditional cholecystectomy
is an open operation, performed manually, with a 15-20 cm long incision made on the anterior abdominal wall. Currently, surgical intervention by this method is performed only for complications of gallbladder polyps - degeneration into cancer with metastases to regional lymph nodes.
These operations are performed under general anesthesia, and the gallbladder is removed along with the polyps. Unfortunately, there are currently no methods for removing polyps from the gallbladder.
Folk remedies
They are used to reduce the size of echostructures and prevent their growth, help relieve inflammation and help accelerate metabolic processes.
Take 20 g of rosehip rhizome, pour boiling water and leave for 5-7 minutes. Drink 50-70 ml before meals. Positive results are observed with regular use of the product for 6 months.
Take 10-15 g of birch bark and pour 200 ml of boiling water. After 30 minutes, filter, add water and 10 ml of lemon juice. Drink the infusion 3 times a day before eating. If a stone has been discovered, then to treat it you need to mix dandelion roots, larkspur, St. John's wort, knotweed and violet in equal proportions. Take 5 tbsp. l. mixture, pour 1 liter of boiling water and leave until completely cool. Drink 250 ml 2-3 times a day.
Carrying out the operation
A radical method of getting rid of echo-positive formations is to perform surgery. It is indicated for large calcifications that are localized in various tissues and organs. The operation can be open or using laparoscopy.
Surgery is required if there are many small stones with sharp edges. Such compactions are considered very dangerous, since there is a risk of injury to tissues and organs due to the movement of these inclusions. It is also possible to remove malignant tumors. The operation is combined with drug therapy and various physiotherapeutic techniques.
TUMORS OF THE BALL TRACT
04.11.18
Benign tumors of the gallbladder and extrahepatic bile ducts. They are very rare. Pathological anatomy and diagnosis. The most common benign tumors of the gallbladder are adenomas. These tumors do not have pronounced specific clinical symptoms. They are usually detected during cholecystectomy and autopsies and are often in combination with cholelithiasis. They are often localized in the area of the bottom of the gallbladder. Hole histograms reveal round-shaped filling defects. When localized in the cervical area, the gallbladder can interfere with the outflow of bile from it, which contributes to the development of XX. Benign tumors often include papillomas (papillomatosis), fibromas, fibroids, and in some cases also neuromas, leiomyomas and hamartomas. Severe cellular atypia and a tendency to relapse give grounds to consider these tumors of epithelial origin as precancerous diseases. The clinical interest of such tumors is that they cause obstruction of the biliary tract and lead to breast cancer. Polypoid tumors of the terminal part of the common bile duct can block the external opening of the pancreatic duct, which usually leads to the development of CP. Before surgery, these tumors can only be diagnosed using cholecystography and ultrasound. With cholecystography, unlike gallbladder stones, the position of the filling defect does not change with changes in the patient’s body position. Treatment. If benign tumors of the gallbladder are detected, cholecystectomy is indicated, as well as removal of the tumor within healthy tissue. For tumors of the terminal part of the common bile duct, pancreaticoduodenal resection is sometimes necessary. This intervention poses a high risk and must be performed according to strict indications (bleeding, malignant tumor degeneration, etc.). In all other cases, they are limited to papillectomy or excision of the tumor. If it is impossible to perform the latter, they resort to curettage or electrocoagulation of the tumor. The use of these methods does not prevent tumor recurrence.
Malignant tumors
Malignant tumors. GB cancer . Accounts for 3-6% of all cancer lesions. In recent years, in parallel with the increase in the incidence of gallstone disease, there has been an increase in the number of patients with gallstone cancer, especially among the population of developed countries. Among malignant tumors of the gastrointestinal tract, gastrointestinal cancer ranks 5-6th. Mortality is 2.5-5.5% of all cancer patients with an overall mortality of 0.1-0.5%. Among malignant tumors of the hepato-pancreatobiliary zone, gallbladder cancer accounts for 10%. Women aged 60-70 years are more likely to get sick. Pathological anatomy. GB cancer often (85-90% of cases) develops against the background of long-term chronic cancer. From this point of view, a number of authors consider CCC to be a precancerous disease. GB cancer quickly spreads through the lymphatic system to the perihepatic tissues, which often causes the development of breast cancer. Of the individual types of cancer, the most common (85% of cases) are adenocarcinoma and scirrhus, rarely mucous, solid and poorly differentiated cancer. In the early stage of development of gallbladder carcinoma, the process occurs without any clinical symptoms or with the characteristic symptoms of chronic cancer, which is caused by a combination of gallbladder cancer and cholelithiasis. The cancerous tumor is more often localized in the anterosuperior part of the body of the gallbladder. Relatively rarely, it is localized in the neck of the gallbladder or on its lower surface. GB cancer exhibits an extremely malignant course and already at an early stage of development gives metastases to the lymph nodes and into the thickness of the liver parenchyma. Primary tumors located in the area of the bottom of the gallbladder spread more quickly to the liver. They give metastases primarily to the lymph nodes located in the area of the hepatic hilum. Starting from the area of the cervix of the gallbladder, cancer quickly spreads to the hepaticocholedochus, as a result of which the outflow of bile through the CBD is blocked and breast cancer, hydrocele of the gallbladder, etc. occurs. Clinical picture and diagnosis. GB cancer has no specific symptoms. In a later period, it is also not possible to identify the symptoms characteristic of this disease, and only when the tumor spreads are both general and local signs noted. At different stages of development of gallbladder cancer, only symptoms of cholecystitis are expressed. It should be noted that about 1% of operations performed for cholelithiasis are diagnosed as cancer during revision of the biliary tract or GI of a remote gallbladder. GB cancer is characterized by the presence of a dense, bumpy and, as a rule, painless infiltrate in the right hypochondrium. When the tumor is localized in the area of the cervix of the gallbladder, hydrops occurs. Often this is accompanied by the clinical picture of obstructive cholecystitis, destruction of the wall of the gallbladder develops, and sometimes its perforation into the free abdominal cavity or into the lumen of neighboring organs (duodenum, OK), which becomes the cause of peritonitis or the occurrence of internal bile duct. In such cases, the patient’s body temperature rises and is hectic in nature. A tumor from the cervical area of the gallbladder quickly spreads to the CBD and leads to the development of a rapidly progressing breast cancer. Common signs of gallbladder cancer often include general weakness, loss of appetite and weight loss. Patients often die from NP. When, during prolonged chronic cancer in an elderly patient, pain in the right hypochondrium becomes constant, low-grade fever, anorexia, constant weight loss and dyspeptic symptoms appear, then gastric cancer should be assumed. In such cases, leukocytosis is detected in the blood, and the ESR increases. When the CBD is compressed by a tumor or affected lymph nodes, the level of bilirubin, cholesterol, and alkaline phosphatase in the blood increases, and bile pigments appear in the urine, i.e. all the signs of breast cancer are present. In the early stage of the disease, cholecystograms show a filling defect. Of the existing methods of instrumental research, laparoscopy is considered more reliable, in which it is possible to examine the gallbladder with the bumpy surface of the tumor on it, growing into the liver, as well as metastases in it. The scanogram reveals a “silent zone” in the right lobe. Treatment. Possible treatment for gallbladder cancer is only surgical, despite the fact that it is not always possible to perform radical intervention. From the point of view of the patient's recovery, the chance is very small. If possible, both radical and palliative operations are performed. Often the gallbladder is removed due to chronic cancer, and the diagnosis of cancer is clarified after hysterectomy. In the vast majority of cases, the outcome of surgical intervention is unfavorable. About 10% of patients live up to 5 years after surgery. If the diagnosis of cancer is confirmed during surgery, extended cholecystectomy is indicated. In this case, a wedge-shaped resection of the liver and removal of the lymph nodes located in the hepatoduodenal ligament are performed. If the tumor grows into the bladder neck and hepaticocholedochus, in some cases it will be possible to remove the gallbladder and perform resection of the hepaticocholedochus along with the lymph nodes located in the hepatoduodenal ligament. If the tumor grows into the liver, segmental liver resection or right hemihepatectomy is performed. For advanced pancreatic tumors, long-term results of radical operations are unfavorable. The average life expectancy after surgery is one year. When high sections of the bile ducts are affected, even palliative surgery often fails. In some cases, it is possible to apply only external drainage of the lobar duct of the liver according to Prader or Smith (figure) or to recanalize the tumor using transhepatic drainage. In some cases, it is possible to perform a palliative operation, the purpose of which is to drain the disintegrated tumor cavity, and in case of obstruction of the common bile duct, to drain the intrahepatic ducts (figure).
Drawing. Transhepatic drainage of the hepaticocholedochus: a - according to Prader. b—according to Smith
Drawing. Hepaticojejunostomy (scheme)
Extrahepatic bile duct cancer. It is rare, but more common than gallbladder cancer. Accounts for 2.5-4.5% of all cancer sites. The proportion of this type of cancer among malignant tumors of the biliopancreatic zone is 15%. In men, bile duct cancer occurs 2-3 times more often than in women. The cancerous process of the bile ducts is often preceded by cholelithiasis, cicatricial changes in the wall of the duct and its benign tumors. The tumor can be localized in any part of the CBD - from the porta hepatis to its terminal part. There are exophytic and endophytic cancers. In the exophytic form, the tumor grows into the lumen of the duct and quite quickly obstructs it. With endophytic cancer, the duct narrows evenly over a long distance. Pathological anatomy. In 30% of cases, bile duct cancer occurs in combination with cholecystitis. All parts of the bile ducts are affected by the tumor with almost the same frequency. The lobar ducts of the liver are relatively less affected by primary cancer. The tumor often develops at the confluence of the lobar ducts, in the area of the papilla of Vater, etc. According to statistics, in 14% of cases the tumor is localized at the confluence of the lobar ducts, in 24% of cases at the confluence of the cystic and hepatic ducts, in 36% of cases in the gallbladder and in 10% in the area of the papilla of Vater. In other areas the tumor is rarely localized. With exophytic growth, the tumor appears in the form of a dense node upon palpation. With an infiltrating tumor, it occurs in the form of a dense cord or an obstructed tube. These tumors grow into the thickness of the submucosal layer and significantly narrow the lumen of the ducts. In some cases, the tumor occurs in the form of a massive conglomerate, which, in addition to the ducts, also involves surrounding tissues. Bile duct cancer spreads quite quickly. In 50-75% of operated patients, tumor growth into adjacent tissues and metastases in other organs are detected. If the tumor affects the lymph nodes located at the gates of the liver, in the paraortic region, it is often impossible to perform radical surgery even for small tumors. The liver is most often affected by metastases. The vast majority of bile duct tumors are adenocarcinomas. Papillary scirrhus is relatively less common, and differentiated or squamous cell carcinoma is relatively less common. Clinic and diagnostics. In a relatively early period of the disease, cancer of the bile ducts leads to the development of breast cancer, which is caused by obstruction of the lumen of the bile ducts or their narrowing and impaired outflow of bile into the duodenum. Unlike jaundice that develops with cholelithiasis, when the CBD is obstructed by a tumor, the appearance of jaundice may not be preceded by a painful attack. When the process of narrowing of the bile ducts is slow, patients are often bothered by skin itching, only after which jaundice appears. In a number of patients, jaundice increases quickly and is often intermittent in nature, due to the breakdown of tumor tissue and temporary restoration of the patency of the cancer process (weakness, apathy, lack of appetite, weight loss, anemia, etc.). Cholangitis often develops, which significantly worsens the patient’s condition. When a cancerous tumor is localized in the right or left hepatic duct and the CBD remains patent, jaundice does not occur, which complicates diagnosis. With a tumor of the common hepatic duct, an enlarged, painless gallbladder is palpated (Courvoisier's sign). The gallbladder can also be palpated when there is dropsy, which is also caused by the blocking of the CBD by the tumor. The location and level of obstruction are determined by the condition of the gallbladder using laparoscopy. Identification of an empty gallbladder indicates obstruction of the upper part of the hepatic duct. With a low location of the CBD obstruction, the GB is filled and tense. To determine the state of the PP and the level of obstruction of the ducts, laparoscopic cholecystocholangiography and percutaneous hepatocholangiography are performed. To identify a common bile duct tumor and differentiate it from BDS cancer, fibroduodenoscopy and ascending cholangiography are performed. The latter helps to determine the extent of the tumor, and in case of incomplete obturation, to identify the boundaries of its prevalence, assess the condition of the upper bile ducts and the possibility of surgical treatment. To diagnose biliary tract cancer, ultrasound, percutaneous transhepatic cholangiography, RPCG, laparoscopic puncture of the gallbladder, and cholangiography are used. Clarification of the morphological diagnosis is possible only during surgery: after choledochotomy, choledochoscopy and GI of the tumor. Differential diagnosis is primarily carried out between the cholestatic form of hepatitis, cholelithiasis, pancreatic cancer, liver cancer and gallbladder. When palpating a dense, elastic, fairly mobile and painless formation (Courvoisier’s symptom), it becomes clear that we are dealing with saturation of the terminal part of the CBD. In such cases, almost no additional research is required. In cases where these symptoms are absent, it is difficult to diagnose a tumor without the use of special research methods. Treatment. Treatment of extrahepatic bile duct cancer is only surgical. Radical surgery can be performed only in 10-15% of patients. The earlier the patient undergoes surgery, the greater the likelihood of radical surgery. In the late stage, as a result of breast cancer, irreversible changes can develop in the body. In the presence of gall bladder cancer, when the tumor is localized in the distal part, it is possible to perform pancreatoduodenal resection, since radical surgery is rarely possible for bile duct cancer. More often, forced intervention is performed to eliminate jaundice and decompress the biliary tract. For this purpose, BDA is applied. In some cases (prolonged jaundice), pancreatic-duodenal resection is considered advisable to be performed in two stages. The first stage of the operation is laparoscopic cholecystostomy. If the cancerous tumor is localized in the middle part of the hepaticocholedochus, the entire mass is removed along with the lymph nodes of the peri-vesical region and the hepatoduodenal ligament. The hole is anastomosed with the duodenum or intestinal loop. In the presence of tumors in the terminal part of the common bile duct, CDA or cslecystogastroenteroanastomosis is applied. For low (below PP) tumor localization, hepaticojejunostomy (see Figure 20) or hepaticoduodenoanastomosis is performed. When the tumor is localized in the proximal part, the tumor is recanalized and this part is drained. When the tumor is localized in the more proximal part of the hepatic duct, internal drainage of the intrahepatic ducts is performed (hepatojejuno- or hepatogastroanastomosis). If the tumor is localized in the area of the hepatic hilum, it is impossible to use extrahepatic bile ducts for drainage. Only in some cases is it possible to recanalize the bile duct and drain the affected section with rigid drainage. The latter is excreted or introduced into the intestinal lumen. With such a localization of the tumor, the intrahepatic bile ducts are usually drained or an anastomosis of the intrahepatic bile ducts with the stomach (Dolioti operation) or TC (Longmeyer operation) is performed (Figure 21).
Drawing. Cholangiojejunostomoses: a - according to Longmeier; b—modification of Longmeyer’s method
Cancer of the papilla of Vater. Among malignant tumors of the pancreaticoduodenal zone, it occurs in 40% of cases. There are: 1) primary carcinoma of the ampullary part of the common bile duct; 2) primary carcinoma of the terminal part of the Wirsung duct; 3) primary cancer of the terminal part of the common bile duct; 4) primary cancer of the papilla of Vater itself; 5) carcinoma of all anatomical elements of the papilla of Vater. Adenocarcinoma and scirrhus are more common. Often, cancer of the papilla of Vater is mistaken for cicatricial degeneration of the papilla. Cancer of the papilla of Vater, spreading to the duodenum, causes its ulceration, which often causes duodenal bleeding. Cancer of the papilla of Vater exhibits a relatively “benign” course. It grows slowly, metastases are rare and at a late stage. Clinic and diagnostics. Cancer of the extrahepatic bile ducts in the initial stage occurs without pronounced symptoms until obstruction and jaundice develop. In some cases, patients report dull pain in the epigastric and right hypochondrium areas. In the initial period, jaundice is inconsistent. This is due to the elimination of perifocal inflammation and spastic contractions. With complete obstruction of the bile duct, jaundice becomes permanent and progresses rapidly. The skin takes on a yellow-green tint. Depending on the location, jaundice progresses at different rates. During the icteric period of the disease, most patients have no pain or they are mild. General phenomena are rapidly increasing: intoxication, exhaustion, caused by disruption of the process of bile and PS entering the duodenum. When the tumor is localized in the terminal parts of the common bile duct, the gallbladder performs a certain compensatory function. In this regard, it expands significantly, increases in size, becomes palpable, mobile and painless (Courvoisier's symptom). In such cases, jaundice increases slowly. In the initial stage, thick bile accumulates in the gallbladder, then, as a result of the absorption of bile pigments, the bile becomes discolored (“white bile”). Some authors explain this by profound impairment of liver function. When the tumor is localized in the upper parts of the bile duct, jaundice develops faster. Here, bile does not pass into the gallbladder, as a result of which it is empty and Courvoisier’s symptom is not observed. When the tumor is localized in the distal part of the RA, the presence of Courvoisier's sign does not always indicate its obstruction. With cancer of the papilla of Vater, jaundice is often wavy, which can cause diagnostic errors. In addition to jaundice, patients suffer from skin itching, weakness, loss of appetite, and weight loss. With such localizations of cancer, occult blood is often detected in the stool (positive Gregersen reaction), which indicates the disintegration of the tumor. Patients often develop cholangitis, body temperature rises, and sometimes chills and profuse sweating are noted. In this case, for the diagnosis of cancer of the papilla of Vater, duodenoscopy and duodenography in a state of hypotension of the duodenum are of great importance. Laparoscopy is also used, which makes it possible to see dilated subcapsular bile ducts and an enlarged gallbladder. Radionuclide testing, percutaneous, transhepatic hedecystocholangiography are used. The latter makes it possible not only to identify the cause of jaundice, but also to clarify the location and nature of the obstruction to the outflow of bile. Treatment. Treatment for cancer of the papilla of Vater is only surgical. Radical surgery is often possible. In the early stage of the disease, when the tumor is 2-2.5 cm in size, not all the duodenum is involved in the tumor process, the head of the pancreas is not infiltrated, and there are no immediate or distant metastases. At this stage, a palillectomy is performed, after which the CBD and pancreatic duct are sutured into the duodenum (from the back). When the tumor reaches a significant size and the patient’s condition is relatively favorable, pancreaticoduodenectomy is performed. However, often the patient’s condition does not allow such an extensive and traumatic operation to be performed. In such cases, it is considered possible to remove the tumor along with the papilla of Vater (transduodenal papillectomy). In advanced cases, when the patient’s condition is serious, palliative surgery, EDA, cholecystojejunostomy, and choledochotomy are performed. With radical operations, the average life expectancy in 5-8% of cases is about 5 years.
Forecast
Identification of hyperechoic areas during ultrasound diagnostics is not a diagnosis. However, in any case, you need to undergo repeated diagnostics or resort to auxiliary instrumental techniques. The prognosis directly depends on the results of the examination.
If the compacted areas are small and do not affect other organs and tissues, then you can simply monitor them and visit a doctor periodically. If stones, calcifications, or tumors are detected, then it is imperative to carry out the therapy prescribed by the doctor. Treatment can be conservative and surgical.
When to suspect cancer
Usually it all depends on the size of the polyp.
Polyps larger than 2 cm are almost always cancerous.
If the polyp is 1 - 2 cm in size, then it is very likely that it is growing cancer.
People over 50 have a much higher risk of cancer than younger people.
Most polyps are benign, but distinguishing them from malignant ones is very difficult. In addition, advanced gallbladder cancer is difficult to treat. It is best when the gallbladder is removed in the early stages.
If there are polyps in the gallbladder at the same time as stones, the bladder is removed regardless of the size of the polyps or symptoms. This must be done because stones, together with polyps, are considered a risk factor for cancer.
People who don't have any symptoms usually don't want to just have their gallbladder removed. A special algorithm has been developed for them:
Polyps larger than 20 mm
Very similar to cancer. The gallbladder is removed.
Polyps ranging in size from 10 to 20 mm
Could be cancer. The gallbladder is removed. You will be very lucky if the surgeon undertakes to remove such a gallbladder laparoscopically.
Polyps ranging in size from 5 to 10 mm
They will be monitored and have ultrasound scans every 6 months. If the polyps grow, the gallbladder will be removed.
Prevention
There are many reasons for the appearance of echostructures in tissues and internal organs. Their prevention consists in preventing provoking factors, that is, possible diseases. Prevention measures include:
- timely treatment of chronic diseases;
- proper nutrition and sufficient physical activity;
- consumption of vitamins.
Particular attention should be paid to the treatment of infectious and inflammatory processes, which often provoke pathological changes. Proper nutrition and sufficient physical activity are very important to maintain beauty and health. Diet therapy and drinking regimen are required. They help keep the body in good shape and give a boost of vivacity and energy.
It is important to regularly consume foods and vitamin supplements containing vitamins A and E. They improve immunity and protect the body from bacteria and infections.
In addition, it is imperative to undergo periodic preventive examinations with a doctor. If pathological symptoms occur, you should not self-medicate, but immediately seek medical help.