New surgical techniques make it possible to perform operations that were previously considered difficult and risky faster and safer. Labor-intensive methods of treatment fade into the background and open the way to cost-effective surgical techniques.
These techniques include laparoscopy, which is used in modern hospitals to perform a wide range of surgical interventions. Laparoscopy is also used for appendicitis.
What is laparoscopy?
Laparoscopy is a method of surgical and diagnostic intervention.
Laparoscopy is a method of minimally invasive surgical and diagnostic intervention. To perform such operations, surgeons use special equipment:
- A laparoscope is a tube with a set of lenses.
- Optical cable with light source.
- A video camera with a chip connected to the laparoscope.
- Monitor.
- Trocar.
For laparoscopic operations, surgeons make a small incision (no more than 2 cm), into which a laparoscope with a camera and other equipment is inserted.
The image from the camera is transmitted to the monitor, so the surgeon can control his manipulations in real time and observe small anatomical structures in high resolution.
Historical reference
Laparoscopy is most often used for diagnostic examination of the abdominal cavity.
Laparoscopy has been developed over many decades, so it is difficult to single out one person as the pioneer of the approach.
In 1902, German veterinarian Georg Kelling from Dresden performed the first laparoscopic surgery on a dog, and already in 1910, Swedish surgeon Hans Christian used this technique on humans.
Over the next few decades, the procedure was refined and spread throughout the medical community. The introduction of a camera with a computer chip was a key event in the development of laparoscopy, since the procedure in a new format could be used for diagnostic examination of the abdominal organs.
Laparoscopy and appendicitis
When removing the appendix, the laparoscopic method can be used.
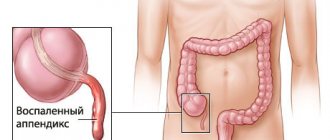
The laparoscopic method is also used for appendicitis, an inflammatory disease of the vermiform appendix of the cecum (appendix).
This allows treatment to be carried out less traumatically for the body and significantly reduce rehabilitation time.
The appendix is a narrow, small, rod-shaped part of the large intestine located in the lower right side of the abdomen.
If the appendix becomes infected or inflammatory, it must be surgically removed immediately (emergency appendectomy). If timely treatment is not carried out, a hole may form in the wall of the appendix - this will lead to an infectious lesion of the abdominal cavity, peritonitis.
The cause of appendicitis in each individual case is usually unknown. The disease can occur after a viral infection in the digestive tract or when the opening connecting the colon to the appendix is blocked by stool. Symptoms of appendicitis:
- Abdominal pain. It may first occur in the upper mid-abdomen and then become sharp and localized.
- Increased abdominal pain when walking or coughing.
- Fever that occurs within a few hours after the first attacks of pain.
- Loss of appetite.
- Nausea.
- Vomit.
- Constipation.
- Chills and trembling.
Laparoscopy for appendicitis - a method of removing appendicitis can be performed as an emergency or planned operation. As a rule, this method is suitable for appendicitis uncomplicated by peritonitis, since in the case of diffuse inflammation of the abdominal cavity, the surgeon needs a larger access.
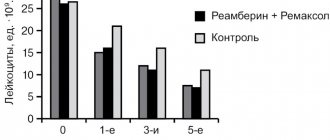
Material and methods
In the department of surgery of the city multidisciplinary emergency hospital (Veliky Novgorod), from the beginning of 2007 to June 2017, 2096 patients with acute appendicitis were operated on: 1334 (63.6%) patients - laparoscopically and 762 (36.4%) - open access. The following clinical and morphological forms were observed in those operated by the laparoscopic method: simple appendicitis - in 12 (0.9%) patients, phlegmonous - in 844 (63.3%), gangrenous - in 376 (28.2%) and perforated - in 102 (7.6%). In 363 patients, complications of acute appendicitis were noted: local peritonitis - in 162 (12.1%) patients, widespread peritonitis - in 66 (4.9%), periappendicular infiltrate - in 86 (6.4%) and periappendiceal abscess - in 49 (3.7%) patients.
The diagnosis of peritonitis was established on the basis of clinical data, ultrasound results, laparoscopic examination of the abdominal cavity, bacteriological and histological studies.
Laparoscopic appendectomy was performed under endotracheal anesthesia using muscle relaxants. For prophylactic purposes, during laparoscopic surgery, cephalosporin antibiotics were administered intravenously in a dose of at least 1 g.
In most cases, three trocars were used, one of which (10 mm) was inserted at the upper paraumbilical point for the laparoscope, the second (5 mm) - in the right mesogastric region along the midclavicular line, and the third (5 mm) - in the left iliac region along the midclavicular line. In young women, the introduction of working trocars was used in both iliac regions. In case of anatomical features or technical difficulties, a 4th trocar was introduced, and the place of its insertion was selected in each case individually, depending on the surgical findings.
During the laparoscopic examination, the nature of the effusion was assessed, its distribution throughout the abdominal cavity, the severity of paresis of the small and large intestines, and the presence of adhesions were determined. After creating the desired exposure and assessing the nature of inflammatory changes in the ileocecal area, the adhesions were separated and pus or inflammatory exudate was aspirated. In the presence of purulent peritonitis, an important point in the operation is the primary sanitation of the abdominal cavity, aimed at preventing purulent exudate from entering the unaffected parts of the abdominal cavity.
In the case of inflammatory-infiltrative changes in the right iliac fossa, the separation of loose adhesions and isolation of the appendix was carried out using the tip of an aspirator-irrigator, which made it possible to quickly evacuate the purulent contents as a result of opening the periappendiceal abscess.
Antegrade mobilization of the appendix was performed in 854 (65.9%) patients. The mesentery of the appendix was in most cases transected using monopolar coagulation in small portions in the immediate vicinity of the appendix. For thickened, inflamed, infiltrated mesentery and the risk of intraoperative bleeding, the LigaSure device and an ultrasonic scalpel were used. Retrograde mobilization of the appendix was performed in 367 (28.3%) patients when it was impossible to visualize the entire appendix. In 75 (5.8%) patients, mobilization of the appendix was carried out using a combined approach, from the base to the apex and vice versa, most often in the case of gross infiltrative-inflammatory changes caused by destructive complicated appendicitis.
Treatment of the stump of the appendix was a critical stage of endovideosurgical intervention. It was performed using a ligature method using an intracorporeal knot at the base of the appendix in 842 (65.0%) patients, and a Roeder loop in 332 (25.6%). In 118 (9.1%) patients, combined ligation of the base of the process was performed by applying an intracorporeal node and a Raeder loop. This technique was used in the case of inflammatory-infiltrative changes in the proximal part of the appendix and the cecum. Regardless of the treatment method, mandatory demucosation of the stump was carried out by coagulating the mucous membrane with a spherical electrode. In 4 (0.3%) patients with self-amputation of the appendix and the inability to visualize and process the stump, the operation was limited to only removing the appendix and installing drainage.
After mobilization and cutting off the appendix in the left iliac region, a 5 mm trocar was removed and either a 10 mm trocar or a 20 mm evacuator was inserted, through which the drug was removed.
During laparoscopic operations for acute appendicitis, complicated by diffuse and diffuse peritonitis, up to 6-8 liters of antiseptic solution were used to sanitize the abdominal cavity. Methodical lavage of the small pelvis, the right and left lateral canal, both subdiaphragmatic and inter-loop spaces was carried out, periodically changing the position of the operating table in order to maximize aspiration of the rinsing fluid. Using the suction tip, we tried to remove loose fibrinous deposits on the parietal and visceral peritoneum. All patients with widespread peritonitis received a transnasal gastric tube to decompress the upper gastrointestinal tract.
Indications for drainage of the abdominal cavity were doubts about the reliability of sealing the stump of the appendix, especially in destructive forms of appendicitis, opening the lumen of the appendix during dissection or removing it in parts, the presence of a periappendiceal abscess, local or widespread peritonitis. Drains were installed in the right lateral canal, and, if necessary, in the small pelvis and subdiaphragmatic space.
Advantages and disadvantages of laparoscopy for appendicitis
Laparoscopy allows operations to be performed much faster.
The main advantages of laparoscopic appendectomy are that such a procedure can be performed much faster with a shorter rehabilitation period in the hospital. This is a really short operation, usually taking between 30 minutes and an hour.
The patient can be transferred to outpatient treatment within a couple of days after surgery. In addition, shorter hospital stays reduce the risk of hospital-acquired infections.
Patients appreciate laparoscopy for much less cosmetic harm. Indeed, with such an operation the incision does not exceed two centimeters, whereas with an open appendectomy the wound reaches ten centimeters in length.
The disadvantages include the complexity of the method. To perform such an operation, the hands of an experienced surgeon specializing in endoscopic techniques are required. The surgical field is small, the surgeon's movements are limited, and there are no tactile sensations.
If bleeding or other serious complications occur, it may be necessary to switch to an open type of surgery.
Appendectomy (removal of appendicitis) in a child
An appendectomy is a surgical procedure to remove the appendix. The appendix is a small appendage that extends from the large intestine. Sometimes the appendix becomes clogged, becomes infected, and becomes swollen. Symptoms of an infected appendix include pain in the lower right side of the abdomen, fever, poor appetite, nausea and vomiting. If your appendix ruptures, you may feel very unwell.
There are two ways to perform this surgery: • Open appendectomy - a single incision is made in the abdomen. Through this large incision, the doctor removes the appendix. • Laparoscopic appendectomy – 3 or 4 small incisions are made in the abdomen. Using a camera and instruments, the doctor removes the appendix through these small incisions. With this type of surgery, your child will recover faster, the surgery will be less painful, the scars will be smaller, there will be fewer healing problems, and there will often be a shorter hospital stay.
To prepare • Tell the doctor what medications your child takes, including prescription drugs, over-the-counter drugs, vitamins, and herbs. • If your child has any allergic reactions to medications, foods, or anything else, tell the health care team. • The child should not drink anything until the operation is completed.
During surgery • Your child will be dressed in a hospital gown. • An IV will be inserted into a vein in your child's arm or leg to give medications and fluids. • Your child will then be transported on a gurney to the operating room. For safety reasons, your child's legs may be secured with a seat belt. • Your child will be given medication to help him sleep during the operation. The medicine will be given intravenously or through a mask. • To ensure that the area of the body being operated on is clean, your child's abdomen will be disinfected and covered with sheets. • An incision will be made in your baby's abdomen. In laparoscopic surgery, 3 or 4 incisions will be made. • The appendix will then be removed. • The incision(s) are closed with sutures, staples, or special tapes called sterile strips. • If sutures or staples are used, they are covered with a bandage.
After operation
In the hospital • Your child will be moved to the recovery room where he or she will be closely monitored until he or she wakes up and feels well.
• Your baby's breathing, blood pressure and pulse will be checked regularly. • Your doctor will tell you about your child's surgery. • Most babies are ready for discharge within 24 hours. • Medicines given during surgery will make the child drowsy. The child should be closely monitored for 24 hours after returning home. At home • Your child should get plenty of rest.
• Give him medications as prescribed by the doctor. • Call your child's doctor and make an appointment after surgery. • Your child can shower. Do not allow your child to take baths for a week after surgery. Remove the bandage(s) from your child's incision(s) while showering or at least once a day. Wash your incisions thoroughly with soap and water, then gently pat them dry. Apply a new patch to each cut. Change the patch as soon as it gets wet or dirty. • If your child has a cut covered with sterile strips, do not touch them. Over time, they will disappear on their own. • Your child may have problems with bowel movements after surgery. Walking and eating high fiber grains, beans, vegetables and whole grain bread will help in this situation. Drinking plenty of fluids may also help. • Your child may need to do deep breathing or coughing exercises to avoid chest infections. Encourage your child to breathe deeply and clear his throat every hour while he is awake and whenever he wakes up during the night. • Your child should not lift anything heavier than 4.5 kg (10 lbs) for three days. • Talk to your child's doctor or nurse about other activity restrictions. If laparoscopic surgery was performed, your child will be able to return to normal activities in about a week. If open surgery was performed, recovery may take longer. Call your doctor right away if your child has: • Abdominal or shoulder pain that doesn't go away or gets worse. • Increased redness, bruising or swelling • Temperature greater than 38° • Chills, cough or feeling weak and muscle pain • Vomiting • Itchy feeling, swelling or rash on the skin. • Difficulty bowel movements or frequent diarrhea
Call 103 immediately if: • The stitches come apart. • New bleeding from the incisions has begun. • Your child has sudden trouble breathing. • Your child has chest pain.
If you have any questions or concerns, ask your doctor or nurse.
Read other articles on this topic
How is a laparoscopic appendectomy performed?
Laparoscopic appendectomy is performed under general anesthesia.
The operation is performed under general anesthesia. Immediately before surgical procedures, the abdominal cavity is filled with carbon dioxide to improve vision. Stages of the operation:
- Step one. The surgeon makes a small incision in the navel area and inserts laparoscopic instruments.
- Step two. The surgeon finds a vermiform appendix in the abdominal cavity. There is often a lot of inflamed fatty tissue around the appendix.
- Step three. The surgeon orients the appendix so that it can be opened safely.
- Step four. The appendix is opened at the junction with the cecum. A ligature is applied. The surgeon also separates the mesoappendix from the adjacent blood vessels.
- Step five. The surgeon removes a portion of the appendix that is separated by a ligature from the loop of large intestine.
- Step six. The vermiform appendix is removed from the abdominal cavity, and the surgeon sutures the tissue and skin.
Appendectomy
Appendectomy can be performed in two ways:
- traditional open surgery through an incision in the abdominal wall;
— laparoscopic appendectomy.
Both operations are performed under general anesthesia and take from 30 minutes to an hour and a half, depending on the presence of complications and the method used.
Traditional open appendectomy
Classic open surgery to remove the appendix is performed for complicated appendicitis, for example, if the appendix has ruptured and the infection has spread beyond the appendix in the abdominal cavity (peritonitis), retroperitoneal space in the form of phlegmon, or an abscess has formed. In such cases, traditional surgery allows the surgeon to thoroughly cleanse the abdominal cavity of infection (sanitise and drain).
In addition, open appendectomy may be required for patients: with severe obesity; with a pronounced adhesive process that makes access to the appendix difficult; with an atypical location of the process; with a long-term inflammatory process in the appendix, when there is a high probability of complications in the form of spread of inflammation to the cecum or rupture of the appendix.
Another reason for traditional open surgery may be concomitant diseases that prevent the application of pneumoperitoneum (injection of carbon dioxide into the abdominal cavity), which is required for laparoscopic surgery.
Laparoscopic appendectomy
Laparoscopic appendectomy is performed most often and is a fairly simple operation that rarely entails complications. The operation is performed under general anesthesia, the average duration of the operation is about 40 minutes. In most cases, the patient can go home 1-2 days after the operation.
Main stages of laparoscopic appendectomy
Preparatory stage. After the onset of anesthesia, the surgeon will pump carbon dioxide into the abdominal cavity through a special thin needle. The purpose of pumping carbon dioxide is to lift the abdominal wall and at the same time tighten the internal organs, figuratively speaking, “inflate the stomach.” Carbon dioxide is absolutely harmless to the body and its injection allows you to create space in the abdominal cavity for the surgeon to work. After this, two punctures are made in the abdominal wall (one in the navel area and one in the bikini area), through which a laparoscope equipped with a video camera is inserted to examine the abdominal and pelvic organs, as well as to visually monitor the further progress of the operation. The image from the laparoscope video camera is transmitted to the monitor in the operating room and allows surgeons to control their actions.
Diagnostic laparoscopy. At this stage, the surgeon, examining the abdominal cavity and appendix using a laparoscope, confirms or removes the diagnosis of acute appendicitis. Evaluates the anatomical location of the appendix and the possibility of accessing it using surgical instruments for laparoscopy. Reveals, if any, the presence of contraindications for continuing laparoscopic appendectomy: spread of inflammation to the dome of the cecum; ruptured appendix (peritonitis); phlegmon of the retroperitoneum; formed abscess; inaccessibility of removing the appendix using the laparoscopic method. In such cases, a transition to a traditional open appendectomy is required.
Removal of the appendix. If the diagnosis is confirmed and no contraindications are identified, the surgeon makes one additional incision (1 cm) to insert the instruments - manipulators necessary to remove the appendix. Then they begin to isolate the appendix, intersect its mesentery, remove the appendix and remove it from the abdominal cavity (through one of the punctures).
The final stage. At the end of the operation, carbon dioxide is removed from the abdominal cavity, stitches and a sterile dressing are applied. After full awakening, the patient is transferred to the postoperative department.
Benefits of laparoscopic appendectomy
1. No incisions in the anterior abdominal wall and, as a result, less pain, less chance of infection, short recovery period;
2. Already 2-3 hours after laparoscopy, the patient can get up. Usually, by the evening or morning of the next day, the condition already allows you to return to normal physical activity, and after a few days to return to work. Marks on the skin from punctures heal quite quickly; after a few months they can hardly be detected;
3. Great information content. The technology of laparoscopy, in which an image from the abdominal cavity is displayed on a monitor screen, makes it possible to detect the smallest pathology that is not visible during classical surgery. This is possible due to the fact that the monitor can magnify the image of organs up to 10 times.
4. Gentle surgical effect. Muscles and vessels are not cut, minimal trauma to the intestines, as a result - rapid restoration of peristalsis and intestinal function.
Complications of the operation
Frequent complications of such surgery include infection. The appendix contains pathogenic flora, so if removed carelessly, bacteria can enter the abdominal cavity. There are also less common complications:
- If carbon dioxide is administered incorrectly, subcutaneous emphysema may occur.
- During the operation, the surgeon may damage the abdominal wall and abdominal vessels.
- Carbon dioxide can enter a damaged vessel and cause a gas embolism.
As mentioned above, serious complications may require additional open surgery, which will significantly increase the length of hospital stay.
The following video will tell you about laparoscopy:
The purpose of the work is to analyze 11 years of experience in introducing the technique of laparoscopic appendectomy (LAE) into the daily practice of the pediatric surgery clinic of the Moscow State Medical University on the basis of the Izmailovo Children's City Clinical Hospital in Moscow.
Material and methods
Between 2000 and 2010, 2299 laparoscopic operations were performed for destructive appendicitis (Fig. 1)
Figure 1. The absolute number of appendectomies performed in the clinic for destructive forms of acute appendicitis by year - from 1999 to 2010 (total 2299 operations).
— uncomplicated forms (1771 patients) and appendiceal peritonitis (528 patients) (Fig. 2).
Figure 2. The ratio of patients with uncomplicated forms of destructive appendicitis and patients with appendiceal peritonitis in absolute numbers by year.
Children of various ages were operated on - from 2 months to 17 years.
A gradual and steady increase in the share of laparoscopic operations in the total number of interventions for acute appendicitis (OA) was observed - from their complete absence in 1999 to more than 99% in 2010.
Currently, LAE is performed by all duty teams - on average, about 250 operations per year.
results
Over the 11-year period of development and implementation of the methodology, the following indicators were analyzed:
— the ratio of LAE and “open” appendectomies (OAE) has been steadily changing in favor of the laparoscopic technique, which in recent years has become absolutely predominant (96-99%) (Fig. 3, 4);
Figure 3. Correlation between LAE and UAE in absolute numbers by year.
Figure 4. Correlation between LAE and OAE in percentage by year.
— duration of LAE. The average duration of laparoscopic surgery gradually decreased from 63 minutes (2000) to 32-35 minutes (2007-2010) (Fig. 5);
Figure 5. Average duration of laparoscopic surgery by year.
— number of “conversions”. A justified transition to open intervention, which was common at the first stage of the introduction of the technique (39 out of 90 operations in 2000), has become extremely rare in recent years (1-2 cases per year) (Fig. 6).
Figure 6. Number of conversions in absolute numbers by year. It should be noted that in no case was conversion associated with serious intraoperative complications;
- complications. The total number of postoperative complications remained small throughout the study period of LAE implementation (from 2 to 7 cases per year - mainly complications of an inflammatory nature) (Fig. 7).
Figure 7. Number of complications and reoperations in absolute numbers by year. Repeated surgery over 11 years was required in 5 cases, and in all these patients, primary laparoscopic surgery was performed for complicated forms of destructive appendicitis. In 4 children, relaparoscopy was performed in 2 cases for postoperative abscess infiltrate, in another 2 cases for early acute adhesive intestinal obstruction; in 1 case - with developed perforation of the ileum - laparotomy, sanitation of the abdominal cavity, ileostomy with subsequent closure of the ileostomy were required.
There were no deaths during the study period.
Discussion
Thanks to numerous works and studies carried out at the end of the last century [1-10], LAE in children has proven not only its feasibility, but also high efficiency in the treatment of large groups of children with both uncomplicated forms of OA and appendiceal peritonitis.
The advantages of LAE (low morbidity, the possibility of full inspection and sanitation of all parts of the abdominal cavity, unexpressed postoperative pain syndrome, reduction of postoperative complications, reduction of length of stay of patients in the hospital, good cosmetic effect, etc.), in our opinion, are indisputable. In this regard, the clinic was tasked with a gradual complete transition to this technique.
The following can be considered the main stages of implementation and dissemination of the LAE technique in the Izmailovo Children's City Clinical Hospital:
— 1999 — complete lack of methodology; the clinic had 1 specialist performing laparoscopic examinations, manipulations and some operations;
— 1999—2002 — training of surgeons (all those providing emergency care “on duty”) was conducted in the basics of laparoscopic surgery. At the same time, there was a gradual development and implementation of the LAE technique in clinical practice;
— 2003—2010 — stage of mandatory use of the technique for OA in children; At the same time, training and improvement of staff in pediatric laparoscopic surgery continued.
Currently, all surgeons on duty are proficient in the LAE technique; there are 4 equipped laparoscopic “racks”, two of which are used for emergency operations; more than 99% of operations for all forms of acute appendicitis are successfully performed laparoscopically; The average duration of surgery for uncomplicated OA is about 26 minutes, for peritonitis - 52 minutes.
A steady increase in the absolute number and percentage of LAE leads to a decrease in the conversion rate and is not accompanied by an increase in the number of postoperative complications (Fig. 8).
Figure 8. The ratio of the number of LAE, conversions and postoperative complications as a percentage by year.
In our opinion, several important factors contribute to the successful widespread implementation of the technique in everyday practice:
— optimized and standardized surgical technique;
— optimized anesthesia and postoperative intensive care (in children with peritonitis), rational antibiotic therapy;
— constant monitoring and improvement of the implementation of the LAE technique by individual surgeons.
1. Optimized and standardized surgical technique
The LAE technique for uncomplicated appendicitis includes several mandatory stages: “open” laparoscopy with the introduction of a blunt-tipped 5- or 10-mm trocar is the only used and safest method of primary entry into the abdominal cavity; always standard arrangement of 3 trocars (5-10 mm + 2x3-5 mm trocar); resection of the omentum - according to indications; bipolar coagulation of the mesentery; application of 2 ligatures (endoloops) to the base of the appendix; coagulation and cutting off the appendage; thorough sanitation of the stump; removal of the appendage (if necessary, in an endobag); sanitation of the abdominal cavity; accompanying operations - according to indications; cosmetic stitches on wounds.
For appendiceal peritonitis, the main stages of the operation are: the same standard arrangement of 3 trocars (10 mm + 2x3-5 mm trocar); primary sanitation of the abdominal cavity with removal of most of the purulent effusion; resection of the omentum - according to indications; isolation of the process from adhesions and adhesions; bipolar coagulation of the mesentery; applying 2 ligatures to the base; coagulation and cutting off the appendage; stump sanitation; removal of the appendix - almost always in the endobag; thorough complete sanitation of the abdominal cavity (dosed lavage and complete aspiration); pelvic drainage.
Intradermal sutures on wounds.
For limited peritonitis (periappendiceal abscess or infiltrate), laparoscopic treatment methods are also always used:
— for periappendiceal abscess (120 patients): simultaneous treatment was carried out in 87 children — laparoscopic division of the abscess, appendectomy, sanitation and drainage; two-stage treatment was carried out in 33 children (laparoscopic opening, drainage of the abscess; conservative therapy; repeat laparoscopy and LAE - after 4-6 months);
— for periappendicular infiltrate without signs of abscess formation (28 patients), two-stage treatment was carried out: laparoscopic sanitation and drainage of the abdominal cavity; conservative therapy; repeat laparoscopy and LAE - after 4-6 months.
Features of the LAE technique that are important to ensure its safety, especially when widely used by specialists with different endosurgical training, are the following:
— standard arrangement of 3 trocars, providing the surgeon with convenient “bimanual” surgery;
— 30-degree optics are always used;
- changing the position of the patient and the table - up to the position of the patient on the left side - allows for maximum convenience in performing LAE for any variant of the appendix localization;
— this is also facilitated by the widespread use of retrograde appendectomy, which allows LAE to be conveniently performed in all cases without the introduction of additional trocars;
— almost complete exclusion of monopolar coagulation during LAE, especially in appendiceal peritonitis and in conditions of intestinal paresis;
— bipolar coagulation of the mesentery is always used;
— ligature appendectomy is always used;
— widespread use of endobags when removing the appendix, omentum, fecal stones, etc. through umbilical access.
2. Optimized anesthesia and postoperative intensive care (in children with peritonitis), rational antibiotic therapy:
— mandatory preoperative preparation — for complicated types of OA;
— antibiotic prophylaxis (with premedication) — in all cases;
— mandatory specific hematological preparation for children with bleeding disorders (hemophilia, thrombocytopenia, etc.);
— surgery under conditions of mechanical ventilation and muscle relaxation — always;
- widespread use of the laryngeal mask, including in “emergency” patients;
- widespread use of epidural anesthesia, including mandatory prolonged epidural anesthesia - in children with peritonitis;
- postoperative course of antibiotic therapy - from 3 to 14 days.
3. Constant monitoring and improvement of the implementation of the LAE technique by individual surgeons:
— mandatory video recording of all laparoscopic operations performed, including “on-duty” operations;
— constant viewing and analysis of video recordings of emergency operations (Deputy Chief Physician for Surgery, Head of the Department of Pediatric Surgery at Moscow State Medical University). At the same time, technical and tactical errors are analyzed. There is no doubt that it is technical errors and violations of treatment algorithms that underlie almost all postoperative complications.
Periodically - 2 times a year - hospital conferences are held to analyze errors and difficulties when performing emergency laparoscopic operations, and analyze “atypical” and rare variants of pathology.
conclusions
1. LAE in the described version is a simple, easily reproducible technique, ideal for widespread use in everyday clinical practice.
2. LAE in the described version is a “cheap” technique that does not require special material costs from the medical institution where laparoscopic surgery is practiced.
3. Maximum standardization of the treatment algorithm for children with OA at all stages - before surgery, intraoperatively (surgical technique), in the postoperative period - is a necessary condition for the widespread introduction of the LAE technique into the daily practice of a wide range of doctors - different in specialization, clinical experience and degree of preparedness in endoscopic surgery surgery.
4. The 100% introduction of the LAE technique into the practice of the Izmailovo Children's City Clinical Hospital was not accompanied by a noticeable increase in the number of intraoperative and postoperative complications; on the contrary, even at the initial stage of development and implementation of the technique, the number of complications after LAE was less compared to the standard “open” techniques that were simultaneously used at that time.
5. A reasonable and rational approach to conversion, in our opinion, is the basis for a minimum number of intra- and postoperative complications, especially at the stages of mastering the LAE method.
6. Widespread mastery of the LAE technique and its implementation in everyday practice can be the basis and incentive for the further development of new endosurgical techniques.
Postoperative care
Postoperative care in the first days includes bed rest, taking antibiotics and other medications, and using painkillers if necessary. After discharge from the hospital, you must carefully monitor the cleanliness of the suture and not expose yourself to serious physical stress for two to three months.
A strict diet is usually not necessary. Some doctors prescribe dietary table No. 0 for a week, recommended for nutrition after operations on the stomach and intestines. This diet excludes the consumption of solid food. Thus, laparoscopy for appendicitis is a good solution, requiring consultation with your doctor.