Gallstone disease (GSD) is the formation of stones in the cavity of the gallbladder and ducts. The gallbladder is an organ that is a hollow “sac” with a volume of up to 60 ml, into which bile synthesized by the liver flows. In the bladder, bile is concentrated and becomes a participant in the digestive process. Through the ducts, through the duodenum, viscous black-green bile enters the food mass, where it emulsifies fats and participates in other biochemical processes. Stones in the bile duct (choledocholithiasis) can form independently or be thrown from the bladder.
How does the liver work?
The liver is the largest gland in humans. It is located in the upper floor of the abdominal cavity on the right. It consists of two main lobes - right and left, which in turn are divided into 8 segments.
In an adult, it weighs about 1/40 of the total body weight (approximately 1.6 kg in men and 1.2 kg in women). The liver has a dual blood supply: approximately 80% of the blood entering the liver comes from the portal vein (venous blood collected from all unpaired abdominal organs), the rest (oxygenated arterial blood) comes from the hepatic artery. Having entered the portal of the liver, both vessels give rise to multiple branching smaller vessels. At the exit from the liver, 3-4 hepatic veins are formed, which flow into the inferior vena cava.
The main structural unit of the liver is the hepatic lobule, which consists of liver cells - hepatocytes. This cell is one of the most important biochemical laboratories of the body. The hepatocyte takes part in the metabolism of proteins, carbohydrates, fats, bile acids, and vitamins. Neutralizes toxic substances coming from the intestines, followed by the release of associated products into the intestinal lumen. An important function of the hepatocyte is the synthesis of bile, which is involved in digestion.
Algorithm for managing patients with cholelithiasis
Gallstone disease (GSD) is one of the most common diseases of mankind. Among diseases of the digestive system, it occupies a leading place, and not only gastroenterologists and therapists, but also doctors of other specialties, including surgeons, participate in its treatment.
Epidemiological studies of the incidence of cholelithiasis indicate that the number of patients in the world at least doubles every decade. In general, in Europe and other regions of the world, cholelithiasis is detected in 10–40% of the population of various ages. In our country, the frequency of this disease ranges from 5% to 20%. In northwestern Russia, gallstones are detected on average in every fifth woman and every tenth man [2, 3, 6, 11]. The significant prevalence of this pathology is associated with the presence of a large number of risk factors that have become relevant recently. The most important of them include hereditary predisposition, developmental abnormalities of the biliary tract, inadequate nutrition, use of medications (oral contraceptives, drugs to normalize lipid metabolism, ceftriaxone, sandostatin derivatives, nicotinic acid), manifestations of metabolic syndrome (obesity, diabetes mellitus, dyslipoproteinemia) , pregnancy, inflammatory bowel diseases, chronic constipation, physical inactivity and others.
It should be noted that the pathogenesis of stone formation is still being studied, but it is known that disruption of the mechanisms of enterohepatic circulation (EHC) of cholesterol and bile acids is of key importance. The causes of EGC violation are:
- violation of bile rheology (supersaturation with cholesterol with increased nucleation and formation of crystals);
- violation of the outflow of bile associated with changes in the motility and patency of the gallbladder, small intestine, sphincter of Oddi, sphincters of the common pancreatic and bile ducts, combined with changes in peristalsis of the intestinal wall;
- disruption of intestinal microbiocenosis, since when the composition and decrease in the amount of bile in the intestinal lumen changes, the bactericidal capacity of the duodenal contents changes with excessive proliferation of bacteria in the ileum, followed by early deconjugation of bile acids and the formation of duodenal hypertension;
- disorder of digestion and absorption, since against the background of duodenal hypertension and increased intraluminal pressure in the ducts, damage to the pancreas occurs, with a decrease in the outflow of pancreatic lipase, which disrupts the mechanisms of fat emulsification and activation of the chain of pancreatic enzymes, creating the preconditions for biliary pancreatitis [3, 8, 11 , 15].
An important unfavorable prognostic factor for cholelithiasis is the development of serious complications that affect the course of the disease. These include acute cholecystitis, choledocholithiasis, obstructive jaundice, cholangitis and chronic pancreatitis (CP). In addition, inadequately chosen treatment tactics for a patient with cholelithiasis often leads to the development of postoperative complications, the so-called postcholecystectomy syndrome, which significantly worsens the quality of life of these patients. The main reason for these circumstances is the lack of compliance between therapists and surgeons, while the former do not have clear tactics for managing patients with cholelithiasis, and the latter are interested in broad surgical treatment of all patients of this profile.
Despite the long history of this disease, the only generally accepted classification tool remains a three-stage division of cholelithiasis into 1) physicochemical stage, 2) asymptomatic stone-bearing and 3) stage of clinical symptoms and complications.
This classification, developed with the direct participation of surgeons, however, does not answer the whole list of practical questions that arise for a therapist when treating patients of this profile, for example:
- Is it necessary to carry out medicinal treatment of cholelithiasis; if such a need exists, then with what drugs and in the conditions of the department of what profile;
- what are the criteria for the effectiveness and ineffectiveness of drug therapy;
- what are the indications for surgical treatment in a particular patient;
- should the patient be monitored after surgery, by which specialist, for how long and with what medications to carry out postoperative treatment.
That is, to date, generally accepted tactics for monitoring patients with cholelithiasis have not been developed.
As evidenced by the analysis of the literature, the only algorithm for the management of patients with this pathology is the international Euricterus recommendations for the selection of patients with cholelithiasis for surgical treatment, adopted at the congress of surgeons in 1997 (Table 1).
From those presented in table. 1 data shows that there are a large number of patients with cholelithiasis for whom surgical treatment is not indicated, but neither diagnostic nor therapeutic tactics have been determined for them. Therefore, it may be important for specialists to identify in detail clinical and diagnostic criteria that would allow dividing all patients with this pathology into groups.
For this purpose, the most important factors are those used in the Euricterus system to make a decision for surgical treatment. These include:
- the presence of clinical symptoms (right hypochondrium syndrome or biliary pain, biliary colic);
- presence of concomitant CP;
- reduced contractile function of the gallbladder;
- presence of complications.
Assessing the characteristics of clinical symptoms in patients with cholelithiasis requires differential diagnosis between right hypochondrium syndrome, due to functional biliary disorder (FBD), and biliary (hepatic) colic, which often causes difficulties even for qualified specialists. At the same time, a correct assessment of the clinical picture and, in particular, taking into account the number of colics in the history largely determine the tactics of managing a patient with cholelithiasis, followed by the choice of direction for conservative therapy, sphincteropapillotomy or cholecystectomy.
It should be noted that these clinical phenomena have fundamentally different mechanisms, for example, with FBS, pain is a consequence of a violation of the contractile function (spasm or stretching) of the sphincter of Oddi or the gallbladder muscles, which prevents the normal outflow of bile and pancreatic secretions into the duodenum. Whereas with biliary colic, it occurs due to mechanical irritation of the gallbladder wall by a stone, obstruction of the gallbladder, wedging into the neck of the gallbladder, into the common bile, hepatic or cystic duct. It should be emphasized, however, that part of the pain associated with colic is due to FBR. To carry out differential diagnosis, the authors proposed taking into account the main clinical signs presented in
Having thus assessed the clinical picture of patients with cholelithiasis, it is possible to subsequently subdivide them into groups.
Group 1 of patients with cholelithiasis should include patients without active complaints and obvious clinical symptoms. The diagnostic criteria will be the absence of biliary pain and the presence of biliary sludge (clots) detected by ultrasound.
Group 2 includes patients with biliary pain (in the epigastric region and/or in the right hypochondrium, characteristic of a functional biliary disorder, and dyspeptic manifestations. Diagnostic criteria in this case are the presence of biliary/pancreatic pain, the absence of biliary colic, the presence of biliary sludge or stones on ultrasound. Rarely, a transient increase in transaminase and amylase activity associated with an attack is also possible.
Patients with cholelithiasis and symptoms of chronic pancreatitis deserve special attention, who, due to clinical, prognostic and, most importantly, therapeutic features, constitute the 3rd group. Diagnostic criteria for this category of patients include: the presence of pancreatic pain, the absence of biliary colic, the presence of signs of pancreatitis, stones and/or biliary sludge with radiation methods (ultrasound, CT, MRI), possibly increased activity of lipase, amylase, decreased elastase-1 and the presence of steatorrhea.
Patients with cholelithiasis with symptoms of one or more attacks of biliary colic, belonging to group 4, are already patients with surgical pathology. Diagnostic criteria in this case are: the presence of one or more biliary colic, stones in the gallbladder, possible transient jaundice, increased activity of ALT, AST, GGTP, bilirubin level associated with hepatic colic. It should be emphasized the need for a detailed identification of biliary colic in the anamnesis, after the manifestation of which months and even years can pass.
After determining the clinical groups, the directions of therapy for patients with cholelithiasis are both general and individual, group-specific. General directions include approaches that help improve EGC processes and suppress the mechanism of stone formation in the gallbladder. These approaches include:
- impact on risk factors and factors for relapse of the disease;
- improvement of the rheological properties of bile;
- normalization of motility of the gallbladder, small intestine and restoration of the patency of the sphincter of Oddi, as well as the sphincters of the common pancreatic and bile ducts;
- restoration of the normal composition of intestinal microflora;
- normalization of digestion and absorption processes with restoration of the functioning of the pancreas.
Impact on risk factors and factors for recurrence of the disease
A set of measures aimed at eliminating factors contributing to stone formation includes the abolition or dose adjustment of lithogenic drugs (estrogens, third-generation cephalosporins, drugs affecting the lipid spectrum, somatostatin, etc.), prevention of congestive gastrointestinal tract, including in pregnant women, treatment of biliary sludge, correction of hormonal levels [1, 11, 13, 14].
The diet of patients with cholelithiasis should be balanced in the content of proteins (meat, fish, cottage cheese) and fats, mainly vegetable. Thus, rational intake of protein and fat increases the cholate-cholesterol ratio and reduces the lithogenicity of bile. The polyunsaturated fatty acids contained in vegetable oils help normalize cholesterol metabolism, restore cell membranes, participate in the synthesis of prostaglandins and normalize the contractile function of the gallbladder. Prevention of excessive pH shifts to the acidic side by limiting flour and cereal products and prescribing dairy products (if tolerated) also reduces the risk of stone formation. High-calorie and cholesterol-rich foods are excluded. Following a diet helps reduce the likelihood of spastic contraction of the gallbladder muscles and sphincter of Oddi, which can cause migration of stones, including small ones (sand).
If there is a severe exacerbation of CP, in the first three days the patient is prescribed complete fasting with water consumption. Subsequently, meals should be frequent, fractional, with the exception of fatty, fried, sour, spicy foods and help normalize the patient’s body weight [3, 4, 7, 9].
Improving the rheological properties of bile
To date, the only pharmacological agent with a proven effect on bile rheology is ursodeoxycholic acid. Our own experience in treating patients with cholelithiasis is associated with the drug Ursosan. With regard to determining the indications for the use of ursodeoxycholic acid drugs in cholelithiasis, it is important to take into account the achievement of remission of pancreatitis and the absence of extrahepatic cholestasis. Therapy with this drug is carried out until the physicochemical and rheological properties of bile are normalized, the amount of microlites in the bile is reduced, further stone formation is prevented and the possible dissolution of stones is achieved. Its additional immunomodulatory and hepatoprotective effects are also taken into account. Ursosan is prescribed in a dose of up to 15 mg/kg body weight, the entire dose is taken once in the evening, an hour after dinner or at night. The duration of use depends on the clinical situation, being approximately 6–12 months [12, 13]. In the presence of abdominal pain and dyspeptic syndromes, the dose should be titrated, starting from a minimum of 250 mg, one hour after dinner, for approximately 7-14 days, with a further increase by 250 mg at similar time intervals to the maximum effectiveness. In this case, cover therapy is advisable, including the parallel use of a selective antispasmodic - Duspatalin (mebeverine).
Normalization of motility of the gallbladder, small intestine and restoration of the patency of the sphincter of Oddi, as well as the sphincters of the common pancreatic and bile ducts
The treatment includes measures to correct the outflow from the ductal system of the pancreas and biliary tract using endoscopy (in the presence of organic changes - cicatricial stenosis of the sphincter of Oddi, calcifications and stones in the ducts) and/or using medications. The means of conservative therapy are drugs that have antispasmodic and eukinetic effects.
Frequently used non-selective antispasmodics (No-shpa, Papaverine) are drugs that do not have a dose-dependent effect, with low affinity for the biliary system and pancreatic ducts. The mechanism of action of these drugs generally comes down to inhibition of phosphodiesterase or activation of adenylate cyclase, blockade of adenosine receptors. Their disadvantages are significant differences in individual effectiveness; in addition, there is no selective effect on the sphincter of Oddi; there are undesirable effects caused by the effect on the smooth muscles of blood vessels, the urinary system, and the gastrointestinal tract [1, 3, 12].
Anticholinergics (Buscopan, Platyfillin, Metacin) also have an antispasmodic effect. Anticholinergic drugs that block muscarinic receptors on the postsynaptic membranes of target organs realize their effect by blocking calcium channels, stopping the penetration of calcium ions into the cytoplasm of smooth muscle cells and, as a result, relieving muscle spasm. However, their effectiveness is relatively low, and a wide range of side effects (dry mouth, urinary retention, tachycardia, impaired accommodation, etc.) limit their use in this category of patients [1, 5, 9].
Separately in this series is an antispasmodic with a normalizing effect on the tone of the sphincter of Oddi - Duspatalin (mebeverine). The drug has a dual, eukinetic mechanism of action: reducing the permeability of smooth muscle cells to Na+, causing an antispastic effect, and preventing the development of hypotension by reducing the outflow of K+ from the cell. At the same time, Duspatalin has affinity for the smooth muscles of the pancreatic and intestinal ducts. It eliminates functional duodenostasis and hyperperistalsis without causing hypotension and without affecting the cholinergic system [1, 4]. The drug is usually prescribed 2 times a day 20 minutes before meals, at a dose of 400 mg/day, for a course of up to 8 weeks.
Restoring the normal composition of intestinal microflora
Antibacterial therapy is an important part of the treatment of cholelithiasis. A completely adequate requirement is the prescription of antibiotics in cases of exacerbation of cholecystitis, as well as in concomitant disorders of the intestinal microbiocenosis. Empirically used derivatives of 8-hydroxyquinoline (ciprofloxacin), creating a secondary concentration in the biliary tract, imipenem, cefuroxime, cefotaxime, Ampiox, Sumamed, fluoroquinolones in combination with metronidazole. A limitation for the use of ceftriaxone is the formation of biliary sludge when taking it. At the same time, a number of antibacterial drugs (tetracycline, rifampicin, isoniazid, amphotericin B) have a toxic effect on pancreatic acinar cells.
As a rule, all patients with cholelithiasis combined with CP exhibit varying degrees of severity of intestinal microbiocenosis disturbances, which significantly affect the course of the disease and the rate of regression of abdominal pain and dyspeptic syndromes. To correct it, the antibiotic rifaximin (Alfa-normix), which is not absorbed in the intestine, is used, which is prescribed 3 times a day, at a dose of 1200 mg/day, for a course of 7 days.
It is mandatory to combine the stage of intestinal sanitation with the use of probiotics (live cultures of symbiont microorganisms) and prebiotics (drugs that do not contain live microorganisms that stimulate the growth and activity of symbiont intestinal flora). Lactulose (Duphalac) has a proven prebiotic effect. Duphalac is a drug with the highest lactulose content and the least amount of impurities. It belongs to synthetic disaccharides, the main mechanism of action of which is associated with their metabolism by colon bacteria to short-chain fatty acids, which perform important physiological functions - both local, in the colon, and systemic, at the level of the whole organism. Clinical studies have proven that Duphalac has pronounced prebiotic properties, realized due to bacterial fermentation of disaccharides and increased growth of bifidobacteria and lactobacilli, as well as a physiological laxative effect.
Normalization of digestion and absorption processes
For this purpose, buffer antacids and multienzyme preparations are used. The indication for prescribing buffer antacids (Maalox, Phospholugel) in patients with cholelithiasis is their ability to:
- bind organic acids;
- increase intraduodenal pH levels;
- bind deconjugated bile acids, which reduces secretory diarrhea and their damaging effect on the mucosa;
- reduce the absorption of antibacterial drugs, which increases their concentration in the intestinal lumen, enhances the antibacterial effect and reduces side effects.
Indications for multienzyme drugs are:
- damage to the pancreas due to duodenal hypertension, increased intraluminal pressure in the ducts;
- violation of fat emulsification;
- impaired activation of the chain of pancreatic proteolytic enzymes;
- violation of the time of contact of food with the intestinal wall against the background of changes in peristalsis.
To correct these changes, it is advisable to use enzyme preparations with a high content of lipase, resistant to the action of hydrochloric acid, pepsin, with an optimum action at pH 5–7, in the form of minimicrospheres with a maximum contact surface with Creon type chyme of 10,000–25,000 units.
Taking into account the stated approaches to the treatment of cholelithiasis in practice in specific groups, it is assumed that they will be individualized. These schemes are presented in the form of stepwise therapy, which can be carried out either simultaneously or sequentially, depending on the clinical situation.
Group 1 - patients with cholelithiasis without clinical symptoms
1st stage. Normalization of bile rheology and prevention of stone formation: ursodeoxycholic acid (Ursosan) 8–15 mg/kg once in the evening until sludge resolution (3–6 months).
2nd stage. Correction of intestinal dysbiosis: Duphalac 2.5–5 ml per day, 200–500 ml per course, for prebiotic purposes.
Prevention. 1-2 times a year for 1-3 months, maintenance therapy with Ursosan at a dose of 4-6 mg/mg body weight per day in combination with Duspatalin 400 mg/day orally in 2 doses 20 minutes before breakfast and dinner - 4 weeks.
Group 2 - patients with cholelithiasis with symptoms of functional biliary/pancreatic disorder or gallbladder disorder
1st stage. Correction of motor-evacuation function and intraduodenal pH:
- Duspatalin 400 mg/day in 2 doses 20 minutes before meals - 4 weeks.
- Creon 10,000–25,000 units, 1 capsule 3 times a day at the beginning of meals - 4 weeks.
- Antacid drug, 40 minutes after meals and at night, up to 4 weeks.
2nd stage. Correction of intestinal dysbiosis:
- Alpha Normix 400 mg 3 times a day for 7 days.
- Duphalac 2.5–5 ml per day, 200–500 ml per course with a probiotic.
3rd stage. Normalization of bile rheology and prevention of stone formation: Ursosan - intake from 250 mg/day (4-6 mg/kg), then weekly increase in dose by 250 mg, up to 15 mg/kg. The drug is taken once in the evening until the sludge resolves (3-6 months).
Group 3 - patients with cholelithiasis with symptoms of CP
Diet 1–3 days of fasting, then table No. 5P.
1st stage. Correction of pancreatic function:
- Omeprazole (Rabeprazole) 20–40 mg/day in the morning on an empty stomach and at 8 pm, 4–8 weeks.
- Duspatalin 400 mg/day in 2 doses 20 minutes before meals - 8 weeks.
- Creon 25,000–40,000 units, 1 capsule 3 times a day at the beginning of meals - 8 weeks.
2nd stage. Correction of intestinal dysbiosis:
- Alpha Normix 400 mg 3 times a day, 7 days.
- Duphalac 2.5–5 ml per day, 200–500 ml per course, with a probiotic.
3rd stage. Normalization of bile rheology and prevention of stone formation: Ursosan - from 250 mg/day (4–6 mg/kg), followed by a 7–14-day dose increase to 10–15 mg/kg body weight, lasting up to 6–12 months. Subsequently, 2 times a year for 3 months or continuous maintenance therapy at a dose of 4–6 mg/kg/day in combination with Duspatalin 400 mg/day orally in 2 divided doses 20 minutes before breakfast and dinner for the first 4 weeks.
Group 4 - patients with cholelithiasis with symptoms of one or more attacks of biliary colic
- Diet - hunger, then individually.
- Hospitalization in a surgical hospital, where conservative treatment is carried out jointly with a gastroenterologist. When relieving colic, patients are treated as group 3. If ineffective, laparoscopic cholecystectomy is performed. The choice of an adequate type of treatment for cholelithiasis is largely determined by the mutually agreed upon tactics of the therapist (gastroenterologist), surgeon and patient.
Indications for surgical treatment in various groups are:
- in group 4: ineffectiveness of conservative therapy, for urgent indications;
- in the 3rd group: after carrying out three stages of therapy as planned, and, as a rule, surgical treatment is indicated even with a mild clinical picture of CP, both in patients with large (more than 3 cm) stones, which pose a risk of bedsores, and small ones ( less than 5 mm) stones, due to the possibility of their migration. It should be borne in mind that removal of the gallbladder with stones does not completely eliminate the factors that contributed to the development and progression of pancreatitis. Thus, against the background of disorders of bile secretion, leading to impaired digestion and absorption of food (malassimilation), due, first of all, to a deficiency of pancreatic enzymes (primary, associated with insufficient production, and secondary, due to their inactivation), subsequently in patients who have undergone cholecystectomy, severe digestive disorders may occur [2, 5, 10];
- in group 2: if conservative cholelitic therapy is ineffective, as planned, possibly after sphincteropapillotomy.
An important goal of treatment is the therapeutic preparation of cholelithiasis patients for planned surgery, as well as their drug rehabilitation in the postoperative period. Due to the presence of mechanisms that disrupt normal bile secretion and digestion before and after surgery for cholelithiasis, therapy should be carried out with modern minimicrosphere polyenzyme drugs and antispasmodics with a eukinetic effect. In addition, the use of pancreatins and Duspatalin in the preoperative period is due to the need to achieve full clinical remission of FBI and CP. For the same purposes, additional prescription of drugs that correct the state of intestinal microbiocenosis and ursodeoxycholic acid preparations is indicated. Therefore, patients who are planning to undergo cholecystectomy need preparatory (before surgery) and further (after surgery) drug correction. In fact, the preoperative preparation option includes the same principles and drugs that are used in planned therapy:
I stage
- Diet.
- Multienzyme drug (Creon 10,000–25,000 units) 4–8 weeks.
- Secretolics, antacids, 4–8 weeks.
- Correction of motor-evacuation disorders (Duspatalin 400 mg/day) 4 weeks.
II stage
- Bacterial decontamination, course 5–14 days (ciprofloxacin, Alpha-normix).
- Prebiotic therapy (Duphalac 200–500 ml per course).
- Probiotic therapy.
III stage
- Impact on bile rheology (Ursosan 15 mg/kg 1 time per day), if the clinical situation allows, for a course of up to 6 months.
In the postoperative period, from the moment fluid intake is allowed, the following are prescribed in parallel:
- Duspatalin 400 mg/day orally in 2 doses 20 minutes before meals, 4 weeks.
- Creon 25,000–40,000 units, 3 times a day with meals for 8 weeks, then 1 capsule with a maximum meal 1 time a day and on demand - 4 weeks.
- Secretolytic according to indications.
Maintenance therapy includes:
- Ursosan 4–10 mg/kg/day, courses 2 times a year for 1–3 months.
- Duspatalin 400 mg/day – 4 weeks.
- Duphalac 2.5–5 ml per day, 200–500 ml per course.
Dispensary observation of patients who have undergone cholecystectomy is carried out for at least 12 months and is aimed at the prevention and timely diagnosis of relapses of cholelithiasis and concomitant diseases of the pancreatic-hepatoduodenal system. Dispensary observation should include regular examinations by a therapist and at least 4 times a year examination by a gastroenterologist with semi-annual monitoring of laboratory parameters (ALT, AST, bilirubin, alkaline phosphatase, GGTP, amylase, lipase), ultrasound of the abdominal organs. According to indications, it is possible to perform fibrogastrodudenoscopy (FGDS), MRI, etc.
Unfortunately, today there is no continuity in the management of patients with cholelithiasis. As a rule, these patients are admitted to surgical hospitals without prior examination and drug preparation, which significantly increases the risk of both surgical and postoperative complications. The first on this list is the formation of the so-called postcholecystectomy syndrome, which is a variant of FBS and an exacerbation of CP. This is especially true for patients who have clinical symptoms before surgical treatment.
Our experience in observing patients who underwent special outpatient and/or inpatient preparation for surgery, including step-by-step therapy, allowed us to conclude that in the case when a patient with cholelithiasis did not undergo preoperative therapy, clinical symptoms after surgery tended to intensify. The deterioration of the condition lengthened the postoperative period and required repeated visits for medical help in the immediate future after the patient was discharged from the surgical department. In those situations where such preparation was carried out, the postoperative course was smooth, with a minimum number of complications.
Thus, the development of approaches to the treatment of cholelithiasis continues to remain promising, while the proposed algorithm on page 56) makes it possible not only to correctly distribute patients into clinical groups, but, taking into account the early and balanced use of modern pharmacotherapeutic agents, to achieve effective prevention and treatment of the disease , including full rehabilitation after cholecystectomy.
Literature
- Diseases of the liver and biliary tract: A guide for doctors / Ed. V. T. Ivashkina. M.: M-Vesti Publishing House LLC, 2002. 416 p.
- Burkov S.G. On the consequences of cholecystectomy or postcholecystectomy syndrome // Consilium medicum, gastroenterology. 2004. T. 6, No. 2, p. 24–27.
- Burkov S. G., Grebenev A. L. Gallstone disease (epidemiology, pathogenesis, clinic) // Guide to gastroenterology. In three volumes. Under the general editorship of F. I. Komarov and A. L. Grebenev. T. 2. Diseases of the liver and biliary system. M.: Medicine, 1995, p. 417–441.
- Grigoriev P. Ya., Yakovenko A. V. Clinical gastroenterology. M.: Medical Information Agency, 2001. 693 p.
- Grigoriev P. Ya., Soluyanova I. P., Yakovenko A. V. Gallstone disease and consequences of cholecystectomy: diagnosis, treatment and prevention // Attending Physician. 2002, No. 6, p. 26–32.
- Lazebnik L. B., Kopaneva M. I., Ezhova T. B. The need for medical care after surgical interventions on the stomach and gall bladder (literature review and own data) // Ter. archive. 2004, No. 2, p. 83–87.
- Leuschner U. Practical guide to diseases of the biliary tract. M.: GEOTAR-MED, 2001. 234 p.
- McNally P.R. Secrets of gastroenterology: Trans. from English M.–SPb.: ZAO “BINOM Publishing House”, “Nevsky Dialect”, 1998. 1023 p.
- Petukhov V. A. Gallstone disease and indigestion syndrome. M.: Vedi, 2003. 128 p.
- Sokolov V.I., Tsybyrne K.A. Cholepancreatitis. Chisinau: Shtiintsa, 1978. 234 p.
- Sherlock S., Dooley J. Diseases of the liver and biliary tract: Pract. hand: Per. from English edited by Z. G. Aprosina, N. A. Mukhina. M.: Geotar Medicine, 1999. 864 p.
- Yakovenko E. P., Grigoriev P. Ya. Chronic diseases of the extrahepatic biliary tract. Diagnosis and treatment. Methodological manual for doctors. M.: Medpraktika-M, 2001. 31 p.
- Yakovenko E. P. Intrahepatic cholestasis - from pathogenesis to treatment // Practitioner. 1998. No. 2 (13), p. 20–24.
- Kuntz E., Kuntz HD. Hepatology, Principles and practice: history, morphology, biochemistry, diagnostics, clinic, therapy. Berlin Heidelberg New York Springer Verlag, 2000. 825 p.
- Rose S. (ed). Gastrointestinal and Hepatobiliary pathophysiology. Fence Greek Publishing, LLC, Madison, Connecticut, 1998. 475 p.
S. N. Mehdiev *, Doctor of Medical Sciences, Professor O. A. Mehtieva **, Candidate of Medical Sciences, Associate Professor R. N. Bogdanov *** * St. Petersburg State Medical University named after. I. P. Pavlova, ** St. Petersburg State Medical Academy named after. I. I. Mechnikova, *** Hospital of the Holy Martyr Elizabeth , St. Petersburg
Contact information for authors for correspondence
What is bile and why is it needed?
Bile is a secretion produced by hepatocytes. The color of bile ranges from light yellow to dark green. Bile contains bile pigments - bilirubin and biliverdin, cholesterol, fatty acids, lecithin, mucin.
Bile is the main participant in digestion. It neutralizes hydrochloric acid that enters the duodenum from the stomach, thereby creating favorable conditions for the action of pancreatic juice and parietal digestion in the jejunum.
Bile acids emulsify fats, allowing them to be absorbed in the intestines.
Bile has a bactericidal effect that prevents the proliferation of pathogenic microflora.
How are the bile ducts arranged and how do they work?
The bile ducts are a system of ducts that originate from hepatocytes and gradually gather into interlobular, segmental and right and left lobar ducts, which unite into the common hepatic duct.
One of the stages of bile removal is its accumulation in the reservoir - the gallbladder. The main function of the gallbladder is to concentrate bile and release it into the lumen of the duodenum during digestion. The volume of this organ is about 80 ml.
The gallbladder is located on the lower surface of the liver. It is a hollow muscular organ, externally covered with a serous membrane and internally lined with mucous membrane. The structure of the gallbladder is divided into the bottom, body and neck of the bladder, which passes into the cystic duct.
Crushing stones using ultrasound
Ultrasound crushing of stones is used if the patient has no more than four stones.
This method is used if the patient has no more than four stones, up to 3 cm in size, that do not contain calcareous impurities.
The principle of operation is to expose the stones to high pressure and vibrations of a regenerated shock wave, in order to crush the resulting stones to a size not exceeding 3 mm.
Next, small stones are excreted through the bile ducts into the duodenum. Disadvantages of ultrasonic crushing:
- there is a possibility of blockage of the bile ducts due to vibration waves;
- sharp stones can damage the walls of the gallbladder.
Contraindications:
- poor blood clotting;
- pregnancy period;
- inflammatory processes and chronic diseases of the gastrointestinal tract: pancreatitis, peptic ulcers, cholecystitis.
Why do gallstones form?
The exact cause of cholelithiasis has not yet been fully elucidated. Only a few factors are known that increase the likelihood of its occurrence.
- Genetic: family predisposition increases the risk of cholelithiasis by 4-5 times;
- Congenital anomalies of the biliary tract;
- Gender - the risk of developing gallstones in women is approximately 2-3 times higher, which is associated with the influence of estrogens on the ability to form gallstones;
- Age - the maximum frequency of clinical manifestations of cholelithiasis is recorded at the age of 40-69 years;
- Dietary (high-calorie diet, poor in plant fiber, as well as with an excess of simple carbohydrates, animal proteins, foods containing cholesterol);
- Use of medications (oral contraceptives, fibrates, ceftriaxone, somatostatin, nicotinic acid);
- Concomitant diseases and conditions (obesity - a tendency to form gallstones in persons with a body mass index of more than 30 is 3 times higher, type 2 diabetes mellitus, hypothyroidism, cirrhosis of the liver, etc.);
- Pregnancy - the risk of developing cholelithiasis increases during pregnancy, especially with repeated pregnancies (the likelihood of stone formation increases by 10-11 times). During pregnancy, bile heterogeneity, or the so-called biliary sludge, develops in 20-30% of patients, stones - in 5-12% of cases.
There is a so-called 5F rule that describes patients at greatest risk of developing stones:
1. Female (female);
2. Fat (overweight/obesity);
3. Forty (age 40 years or more);
4. Fertile (fertile women - that is, pregnant and giving birth);
5. Fair (light-skinned blondes).
Sources
- Nambapana MN., Wickramasuriya SS., Macelline SP., Samarasinghe K., Vidanarachchi JK. Algae-based antioxidant containing selenium yeast (Economase®) enhanced the growth performance, oxidative stability, and meat quality of broiler chickens. // Anim Biosci - 2021 - Vol - NNULL - p.; PMID:33902180
- Wu H., Sun H., Ma C., Lian L., Lu L., Xu L., Xu L. Effects of maternal dietary energy restriction on breast muscle fiber development in the offspring of broiler breeders. // Anim Biosci - 2021 - Vol - NNULL - p.; PMID:33902177
- Taniguchi S., Zhu Z., Matsuzaki M., Tsudzuki M., Maeda T. 5-aminolevulinic acid improves chicken sperm motility. // Anim Biosci - 2022 - Vol - NNULL - p.; PMID:33902172
- Li W., Geng Z., Zhou XH. Causal mediation analysis with sure outcomes of random events model. // Stat Med - 2022 - Vol - NNULL - p.; PMID:33902164
- Junqueira FMD., Nadal JAH., Brandão MB., Nogueira RJN., de Souza TH. High-frequency oscillatory ventilation in children: A systematic review and meta-analysis. // Pediatr Pulmonol - 2022 - Vol - NNULL - p.; PMID:33902159
- Webb C., Chang YH., Pockaj BA., Gray RJ., Stucky CC., Wasif N. Lymph node positivity and association with long-term survival for different histologies of appendiceal cancer. // J Surg Oncol - 2021 - Vol - NNULL - p.; PMID:33902156
- Fontao M., Schorer L., Ross T. . // Fortschr Neurol Psychiatr - 2021 - Vol - NNULL - p.; PMID:33902150
- Eddicks M., Eddicks L., Stadler J., Hermanns W., Ritzmann M. // Tierarztl Prax Ausg G Grosstiere Nutztiere - 2022 - Vol49 - N2 - p.120-132; PMID:33902142
How are gallstones formed?
The process of stone formation is quite well studied. The key links are:
- An increase in the lithogenicity of bile (the ability to form stones) means an increase in the content of cholesterol and bilirubin in it.
- Impaired contractile function of the gallbladder.
- Increased pressure in the bile duct system.
Mucin is a natural gel, constantly secreted by the wall of the gallbladder; when lithogenicity increases, it begins to “absorb” cholesterol crystals, thereby forming a “fossilization nucleus.” The formed suspension, with impaired contractile function, continues to attach salt crystals encrusted with calcium salts. Thus, gallstones can grow up to 5-7 mm per year.
Clinical picture and symptoms of the disease
Most often, the first sign that forces the patient to see a doctor is pain in the right hypochondrium, of varying intensity. Cutting or stabbing in nature, the pain is most often constant, often radiating to the right shoulder blade, lower back, and forearm. In some cases (with cholecystocoronary Botkin's symptom), it can radiate beyond the sternum, resembling an attack of angina. It should be borne in mind that the intensity of pain is in no way an indicator of the severity of the process. For example, in some cases, severe pain may disappear, but mild pain does not mean a mild form of the disease.
Often the patient’s condition worsens after eating spicy or fatty foods; their consumption increases the need for bile to process food, which leads to contraction of the gallbladder. In any form of the disease, there is an increase in body temperature. In the form of short rises, the temperature rises to 37-38°C, and the patient often experiences pain. However, during an acute attack accompanied by chills, the temperature can rise to 38-40°C.
How does gallstone disease occur?
The main factors influencing the course of the disease are the nature of nutrition and the size of the stones. Gallstone disease can occur both in the form of chronic stone carriage and in acute, and sometimes in complicated, form.
Where does pain come from with gallstone disease?
By themselves, gallstones do not cause any pain and can be an accidental finding during medical examination. When food enters the duodenum, the mechanoreceptors are irritated and cause contraction of the gallbladder. The stones wedge into the cervix, causing a prolonged spasm, which manifests itself as pain. When taking antispasmodic drugs, the calculus can “move” back from the cervix and the attack of hepatic colic is stopped. If the stone remains in the cervix, then inflammation begins to develop against the background of obstruction.
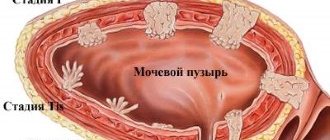
Chronic calculous cholecystitis is an asymptomatic stone carrier. The size of the stones can vary from 2 – 3 mm to 5 cm. This stage is characterized by an almost complete absence of clinical manifestations of the disease. Stones can remain in the lumen of the gallbladder for years without causing any symptoms. However, if there is an error, discomfort may occur in the right hypochondrium, which can be relieved independently or while taking antispasmodic drugs.
Hydrocele of the gallbladder - occurs against the background of obstruction of the neck of the gallbladder by a calculus, cutting off the latter from the entry of bile. The bladder is filled with mucus secreted by the mucous membrane and is not involved in digestion.
Acute calculous cholecystitis - occurs with prolonged obstruction of the neck of the gallbladder by a calculus. The pain syndrome persists against the background of ineffective conservative treatment. The patient is bothered by vomiting, which does not bring relief; pain can be felt behind the sternum - cholecystocardial syndrome, in the right shoulder blade. Body temperature rises and chills appear. Inflammatory changes begin to develop in the wall of the gallbladder, which progress from catarrhal, phlegmonous and gangrenous forms. Against the background of the latter, perforation of the gallbladder or abscess may develop.
Choledocholithiasis and acute biliary pancreatitis. Choledocholithiasis develops as a result of migration of biliary sludge or small stones from the gallbladder into the common bile duct. Once in the common bile duct, small stones freely descend to the sphincter of Oddi, which is a release mechanism - a circular muscle cuff. Sludge and stones “wedge” into the sphincter, causing its long-term spasm, causing a violation of the outflow of bile - obstructive jaundice. The patient's skin and sclera become a rich yellow color. This condition requires emergency decompression of the bile ducts - restoration of bile outflow.
An increase in pressure in the common bile duct promotes the reflux of bile into the main pancreatic duct and intraductal activation of pancreatic juice enzymes - a trigger for the development of acute biliary pancreatitis.
Mirizzi syndrome . A fairly rare complication of gallstone disease. Develops as a result of prolonged stone bearing. First, a stricture forms, then a bedsore between the gallbladder and the common bile duct.
Mirizzi syndrome presents significant difficulties for surgical treatment. This is due to the fact that in the human body there is no plastic material to close the defect of the common bile duct. Surgical treatment of Mirizzi syndrome is often accompanied by the formation of an anastomosis between the small intestine and the common bile duct. When a stone migrates into the small intestine, acute intestinal obstruction may develop, requiring emergency surgical treatment.
In the photographs, in the lumen of the resected section of the small intestine there is a calculus that caused intestinal obstruction.
Main types of stones
Gallstones vary in size, shape, color and chemical composition.
Size
. There are no large single stones in the common bile duct (common bile duct), which is due to the diameter of the cystic duct. Smaller ones are lighter and leave the bladder with a flow of bile. Large ones remain at the bottom under their own weight.
Form.
If stones with “edges” are found in the ducts, it can be argued that they came from a bladder: this shape appears from the close adhesion of the stones to each other. Basically, the shape of bile formations is round, oval.
Color
depends on the chemical composition:
- cholesterol - predominantly yellow, greenish, golden in color;
- bilirubin (pigment) - soft and black in color;
- calcium (calcareous) formations are whitish, sometimes their surface is like an egg shell;
- with parasitic or bacterial infection - brown.
The classification is based on the predominance of one of the chemical elements. At the same time, the other two are also present. In addition to the main ones, dead cellular elements, protein parts and other components are mixed into the structure.
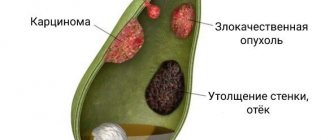
How to diagnose gallstone disease?
The gold standard for diagnosing gallstone disease is ultrasound examination of the abdominal cavity. This method allows you to identify stones in the gallbladder. Assess their size, shape and location. An important indicator is the thickness of the gallbladder wall. Normally, it does not exceed 2-3 mm. Thickening of the wall is an absolute sign of inflammatory changes - acute cholecystitis. An important criterion is the diameter of the common bile duct. If there are stones, its diameter increases from 3 – 6 to 20 mm.
Magnetic resonance imaging allows you to see the intra- and extrahepatic bile ducts, as well as the main pancreatic duct. This diagnostic method is used when there is a suspicion of the presence of stones in the common bile duct. This is necessary for treatment planning.
Multislice computed tomography is indicated for the development of acute biliary pancreatitis. This diagnostic method allows you to identify inflammatory changes in the pancreas and surrounding tissues.
Gastroduodenoscopy - this diagnostic method is especially valuable for complicated cholelithiasis, as it allows not only to evaluate the stomach, duodenum, but the flow of bile through the major duodenal papilla. If necessary, gastroduodenoscopy can easily be transformed from a diagnostic procedure into a therapeutic one. Using special instruments, you can “paint” the bile ducts and remove stones.
In the figure, the arrow indicates a stone in the common bile duct. Using a duodenoscope, a dissection of the sphincter of Oddi was performed in the duodenum. A radiopaque substance was introduced to allow visualization of the calculus. Using a special basket, the stone is captured and removed.
Consequences of choledocholithiasis
After treatment and following the doctor’s recommendations, the patient quickly returns to his normal life. However, if you do not seek medical help promptly, complications may arise.
- The presence of stones provokes inflammatory processes that are severe and painful.
- Since the bile and pancreatic ducts connect before entering the duodenum, if the mouth is blocked by a stone, the ducts become swollen and damage to the pancreas is possible. Acute pancreatitis can result in the death of the patient.
- Communicating with the liver, the inflamed biliary system disrupts the functional activity of this organ (and the liver participates in digestion, hematopoiesis, deposits necessary substances, utilizes and deactivates unnecessary ones, and so on). As a result, there is an imbalance in the functioning of almost all body systems.
Treatment of gallstone disease
Treatment of gallstone disease is only surgical. Conservative treatment, taking choleretic drugs promotes the migration of stones from the gallbladder into the common bile duct and can cause acute biliary pancreatitis and obstructive jaundice.
Depending on the access and equipment used, cholecystectomy can be performed openly, laparoscopically through punctures in the anterior abdominal wall, and robotically using the DaVinci apparatus. Each method has its own indications and limitations.
Open cholecystectomy, this type of surgical intervention is indicated if there are contraindications for laparoscopic cholecystectomy. Such as severe cardiovascular or respiratory failure, abdominal adhesive disease, the presence of internal biliodigestive fistulas, Mirizzi syndrome.
Laparoscopic cholecystectomy is the gold standard in the treatment of gallstone disease. This method is low-traumatic and provides excellent visualization and functionality. Modern high-tech equipment reduces the risk of intraoperative complications.
One of the options for laparoscopic surgery is robotic cholecystectomy using the DaVinci device. Allows you to isolate extrahepatic bile ducts with pinpoint accuracy, thereby protecting the patient from a dangerous complication - intersection of the common bile duct.
Special categories of patients
Elderly and senile patients require special attention. Many concomitant diseases can cause refusal of planned surgical treatment in favor of surgical treatment “for health reasons” in other clinics. Our clinic has accumulated extensive experience in providing care to patients of the older age group. After preoperative evaluation and preparation, older patients can expect to undergo surgical intervention.
Patients suffering from diabetes with a high body mass index require increased attention. Against the background of diabetes mellitus, the body's reparative capabilities are significantly reduced, which, along with severe pain and prolonged bed rest, can lead to a number of undesirable complications.
In both groups of patients, laparoscopic cholecystectomy is the operation of choice, because minimally invasive access can significantly reduce surgical trauma and significantly speed up the process of patient activation. As a rule, you can get out of bed 3-4 hours after surgery. Thanks to early activation, the risk of developing cardiovascular complications and abdominal adhesive disease is significantly reduced. The use of special extended instruments allows laparoscopic surgery to be performed on patients with a body mass index of more than 40 kg/m2.
How is laparoscopic cholecystectomy performed?
The photographs show in detail the stages of laparoscopic cholecystectomy.
The picture shows the stage of mobilization of the neck of the gallbladder, its isolation from the adhesions with the duodenum.
In this image, using a laparoscopic instrument, the peritoneum in the area of the neck of the gallbladder is opened and the cystic duct is mobilized.
In this image, the cystic duct is highlighted and a clip is applied to it.
After applying two clips to the remaining part of the cystic duct and one to the outgoing part, it can be crossed.
After crossing the cystic duct, the cystic artery is isolated and clipped.
Now that the cystic artery has been crossed, all that remains is to separate the gallbladder from the bed and remove it from the abdominal cavity.
This image shows the separation of the gallbladder from its bed in the cervical region. Seemingly simple to perform, it requires very careful work to avoid liver damage.
The final stage of the operation. The gallbladder is separated from the bed and removed from the abdominal cavity.
What do gallbladder stones look like?
The photographs show removed gallbladders with extracted stones. The appearance of stones is varied. They differ in shape, size, appearance and structure.
Diagnostics
The diagnosis is based on the results of instrumental studies and anamnesis data.
- Ultrasound examination (ultrasound) of the upper abdominal cavity is performed to diagnose cholelithiasis and calculous cholecystitis. During the study, in addition to stones in the gall bladder or ducts, the size of the gallbladder, the condition of its walls, and pathology of the liver or pancreas are determined.
- gastroduodenoscopy - allows you to determine diseases of the stomach, esophagus and duodenum.
- retrograde cholangiography (x-ray examination using a contrast agent) is performed in the presence of complications.
- transgastric ultrasound of the ducts is necessary when diagnosing choledocholithiasis.
Complications after laparoscopic cholecystectomy
The most common intraoperative complications are the intersection of the cystic artery and the common bile duct.
Bleeding from the transected cystic artery is stopped by clipping and does not cause technical difficulties for an experienced surgeon.
Damage to the common bile duct requires reconstructive intervention, which is associated with significant difficulties. In the long term, such a surgical injury can lead to a significant decrease in quality of life and disability.
Performing cholecystectomy using minimally invasive and high-tech equipment can significantly reduce the risks of intraoperative complications.
Symptoms of cholelithiasis
Heartburn can be a symptom of cholelithiasis.
Often, a person is not aware of the presence of cholelithiasis until the sudden onset of symptoms that require immediate action. List of common symptoms of this disease:
- acute pain in the right hypochondrium;
- a sharp attack of biliary colic;
- heartburn;
- nausea and vomiting;
- bloating;
- high temperature;
- yellowness of the skin.
Neglect of the disease can provoke the following complications:
- gallbladder infection;
- narrowing of the bile ducts;
- the formation of chronic inflammatory processes leading to diseases such as hepatitis, cholecystitis, duodenitis, pancreatitis.
Postoperative period
In case of an uncomplicated course of the postoperative period, early activation of the patient is practiced, 3-4 hours after the operation. Eating is allowed on the second day. Discharge from the hospital occurs within 3-4 days, and depends on the individual threshold of pain sensitivity. Removal of sutures is not required, as skin wounds are sutured with cosmetic sutures and absorbable sutures.
A return to normal lifestyle and physical activity is possible within 10–14 days, after complete healing of skin wounds.
Appearance after laparoscopic cholecystectomy:
Transvaginal laparoscopic cholecystectomy using the NOTES method
Rice. 6. Scheme of laparoscopic transvaginal cholecystectomy using NOTES technology
Rice. 7. View of the anterior abdominal wall during laparoscopic cholecystectomy using SILS technology.
Since 2007 in France, and since 2008 in the Russian Federation, a unique method of removing the gallbladder has been practiced - transvaginal cholecystectomy using NOTES technology. The operation is performed without any punctures of the abdominal wall, therefore, there are no postoperative scars. The essence of the surgical intervention is access to the affected organ through a small puncture (1 cm) of the posterior vaginal fornix. The intervention is performed using laparoscopic instruments and optics introduced into the peritoneal cavity through this access. After removing the gallbladder through the same access, one suture is placed on the puncture. The synthetic suture material used in this case dissolves within 3-4 weeks.
The advantages of this method are:
- in the absence of pain after surgery;
- the patient's motor activity is not impaired;
- short rehabilitation period, patient hospitalization lasts only one day;
- excellent cosmetic effect;
After 7-10 days after surgery, a person can begin to work, and they can play sports on the 14th day. Among the restrictions in the postoperative period should be the need to exclude intimate relationships for a month. At the same time, the genital organs (uterus, appendages, etc.) are not affected during transvaginal cholecystectomy, so their functionality remains unchanged.
What questions can you ask the doctor at your appointment?
- Do I need surgery?
- Is it possible to dissolve stones?
- Why is it better not to dissolve stones?
- Is it possible to simply remove the stones and leave the bubble?
- How will my life change after cholecystectomy?
- Will there be dietary restrictions?
- Will it hurt after the surgery?
- What kind of anesthesia will it be?
- When can I eat fatty heavy foods and alcohol?
- Are dressings necessary after discharge from the hospital?
You can contact the clinic of coloproctology and minimally invasive surgery for diagnosis and treatment of gallstone disease. Thanks to modern operating rooms and highly qualified staff, the clinic provides all types of treatment for gallstone disease, including robotic surgeries.
Treatment under the compulsory medical insurance policy is possible.
Sign up for a consultation and receive quality treatment as soon as possible.
Single-port laparoscopic cholecystectomy SILS
The use of the NOSE technique is technically impossible in cases where patients have undergone many surgical interventions on the pelvic organs in the past. Therefore, an equally effective method of minimally invasive cholecystectomy was developed, which has been used in America since 2008, and since 2009 such operations have been performed by domestic surgeons. We are talking about removing the gallbladder through a puncture in the navel area (SILS technology).
Single-port laparoscopic cholecystectomy
consists of performing an operation using a special device (port), which is a soft plastic apparatus that is inserted into the abdominal cavity through a puncture. Port diameter 23-24 mm. It is through this that laparoscopic instruments are inserted; the diameter of the laparoscope does not exceed 5 mm. Upon completion of the operation, a cosmetic suture is applied to the small wound. Surgical intervention using SILS technology (single-port surgery), in contrast to conventional laparoscopic access (multi-puncture), has a number of advantages:
- fewer punctures on the abdominal wall;
- less pain after surgery;
- shorter rehabilitation period;
- better cosmetic effect;
The advantages of this method of surgery are especially noticeable when there are multiple stones in the gallbladder - with the usual method, the surgeon must increase the puncture to remove stones and the diseased organ.
The choice of the appropriate surgical treatment method depends on the individual characteristics and health status of the patient. Visiting a clinic with qualified and experienced specialists guarantees the highest possible treatment results.