This site was made by experts: toxicologists, narcologists, hepatologists. Strictly scientific. Tested experimentally.
Author of this article, expert: gastroenterologist Daniela Sergeevna Purgina
In short: The idea of crushing gallstones without surgery is certainly a good one. However, in practice, this method is not yet justified: it does not affect the metabolism in any way, and over time the stones grow again. Almost all patients who undergo lithotripsy still have their entire gallbladder removed.
- What is lithotripsy
- Is it effective to crush gallstones?
- In what cases is stone crushing carried out?
- When the procedure is prohibited
- What complications are there?
- How is lithotripsy performed?
- Laser crushing
- Shock wave crushing
- Contact chemical cholelitholysis
- What are the advantages of lithotripsy
- Cons of the procedure
- Alternatives to lithotripsy
This article was edited by gastroenterologist Daniela Sergeevna Purgina.
In this article, we will talk about a method of treating cholelithiasis, such as lithotripsy, that is, crushing stones.
What is lithotripsy
Extracorporeal shock wave lithotripsy - destruction of stones using shock waves induced by a generator. This technique was first used in 1985. It is practiced strictly according to indications as independent therapy or in combination with oral administration of litholytic (dissolving) drugs, which gives the best result.
This type of treatment for gallstone disease is conceived as an alternative to cholecystectomy: in order to avoid removing the gallbladder. However, in practice, stone crushing is rarely used. This is explained by three reasons:
- High risk of serious complications (eg acute pancreatitis).
- Presence of contraindications.
- Limited indications.
Subscribe to our YouTube channel!
Is it effective to crush gallstones?
The effect is considered effective if there is no relapse within a year, and ultrasound 6 and 12 months after the procedure shows that the gallbladder is free of stones. If the patient, after crushing the stones, takes ursodeoxycholic acid, which has a litholytic effect, then the effectiveness can reach 80%, at least 45%. (For more information about such drugs and in what cases they work, read the article on how to dissolve gallstones.)
At its core, this method is symptomatic, and not etiotropic (eliminating the cause of the disease) treatment. Therefore, it does not prevent the reappearance of stones. Most often it is used to break up stones stuck in the duct after removal of the bladder. But only if for some reason it is impossible to perform endoscopic lithoextraction: for example, there are contraindications or other obstacles to the operation.
Complications
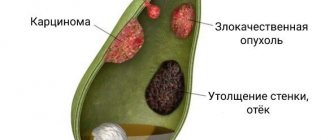
Complications of cholelithiasis are often observed due to blockage of any part of the biliary tract by a stone. Let's look at the most common of them.
Choledocholithiasis is the presence of stones in the bile ducts. This condition may be asymptomatic if the stones do not interfere with the patency of the bile ducts. If they obstruct (clog) the bile ducts, obstructive jaundice develops. Since bile does not flow from the liver into the duodenum, it enters the blood, turning the skin yellow.
Stones located in the bile ducts not only block them, but also, by injuring them, cause inflammation - cholangitis. Stagnation of bile also contributes to inflammation. A dangerous form of cholangitis is purulent cholangitis. With the progressive rapid course of purulent cholangitis, small ulcers form not only in the bile ducts, but also in the thickness of the liver itself, which leads to the formation of multiple liver abscesses. The prognosis in such cases is unfavorable.
Acute obstructive cholecystitis develops when the cystic duct, through which bile flows from the gallbladder, is blocked by a stone. The outcome of obstructive cholecystitis can be hydrocele of the gallbladder, if the body’s strength is high enough, and blockage of the cystic duct by a stone persists. If the strength of the bacteria present in the bile exceeds the strength of the body, either empyema of the gallbladder or gangrene of the gallbladder occurs. With empyema of the gallbladder, its lumen contains pus, which can break into the abdominal cavity with all the ensuing consequences. With gangrene of the gallbladder, the death of its wall occurs, which can provoke perforation (the formation of a hole), which, as in the case of empyema, leads to diffuse peritonitis.
Large gallbladder stones can form a bedsore in the gallbladder wall. And since the wall of the gallbladder often comes into contact with the wall of the duodenum, a bedsore can form in it. Once in the intestinal lumen, the stone usually blocks the intestinal lumen, and intestinal obstruction develops, requiring emergency surgical intervention.
If a stone blocks the pancreatic duct, pancreatitis develops, i.e. inflammation of the pancreas. Pancreatitis can progress to pancreatic necrosis - death of pancreatic tissue, which often leads to death.
We tried to characterize the main complications of gallstone disease so that you understand how important it is to see a doctor in a timely manner.
In what cases is stone crushing carried out?
Lithotripsy is in principle only possible under the following conditions:
- cholelithiasis with an uncomplicated course;
- the ability of the gallbladder to contract is preserved by 60% or more;
- cholesterol stones or partially (only at the edges) calcified, i.e. transparent to x-rays;
- number of inclusions from 1 to 3, no more;
- the size of the stones is no more than 3 cm and no less than 1 cm;
- stones occupy no more than half the volume of the gallbladder.
The most important condition: the gallbladder must have sufficient motility, and the ducts must have normal lumen for the evacuation of fragments.
Crushing gallstones without surgery is possible, but it is usually not worth it.
Gallstone disease (GSD)
Gallstones are a common disease that develops in people over the age of 40. This disease is especially common among the urban population of industrialized countries. According to most researchers, about 10% of men and up to 25% of women in European countries suffer from cholelithiasis.
With cholelithiasis, calculi (stones) form in the gallbladder and bile ducts. These stones consist of the usual components of bile - bilirubin, cholesterol, calcium salts. Most often, mixed stones are found, containing in greater or lesser proportions the indicated components. If a stone consists of 90% cholesterol, then such a stone is called “cholesterol”, if it is made of bilirubin - “pigment”, and if it is made of calcium salts - “lime”. The size and shape of stones in gallstone disease can vary. Dimensions generally vary from 1–2 mm to 3–5 cm; the shape can be round, oval, polyhedron, etc.
Causes of gallstone disease
The main site of gallstone formation is the gallbladder, and in very rare cases, the bile ducts. Currently, in clinical medicine there are three main reasons for their formation: stagnation of bile in the bladder, metabolic disorders, inflammatory changes in the wall of the gallbladder . Metabolic disorders cause a change in the ratio of the concentrations of cholesterol, phospholipids (lecithin) and bile acids in bile. The concentration of cholesterol increases and phospholipids decreases. Such bile is considered to be lithogenic. Under such conditions, bile cholesterol easily falls out in the form of crystals; these crystals are grouped and combined with each other, which leads to the formation of stones. It is known that gallstone disease often develops in patients with metabolic diseases such as diabetes, obesity, and hemolytic anemia. When bile stagnates for a long time in the bladder, it becomes infected. The infection leads to damage to the wall of the gallbladder and desquamation of its epithelium. All this contributes to faster deposition of cholesterol crystals and the formation of gallstones. In the damaged wall of the gallbladder, the absorption process of some bile components is disrupted, their physicochemical ratio changes, which also contributes to stone formation. In addition, with cholestasis in the bile located in the gallbladder, the concentration of cholesterol, bilirubin, and calcium may increase, which increases the lithogenicity of the bile. This is facilitated by eating foods rich in cholesterol, obesity, and taking oral contraceptives.
Clinical manifestations of cholelithiasis
Gallstone disease can be asymptomatic (the so-called latent form of cholelithiasis). In this case, gallstones are discovered as an incidental finding when examining patients for another disease.
Patients with gallstones may be bothered by dyspeptic disorders : an unpleasant metallic taste, bitterness in the mouth, nausea, bloating, a feeling of heaviness in the right hypochondrium, especially after eating fatty foods. Such phenomena are caused by impaired motility of the biliary tract and gastrointestinal tract with the reflux of bile into the stomach and esophagus. This form of cholelithiasis is called dyspeptic.
The classic clinical manifestation of cholelithiasis is hepatic (biliary) colic, which is characterized by intense cutting, stabbing, tearing, and less often paroxysmal pain in the right hypochondrium and epigastric region. These pains often radiate to the lumbar region, right shoulder blade, and right forearm. The pain can also spread to the heart area and be mistakenly perceived as an angina attack. Pain occurs most often after an error in diet (eating fatty, spicy foods), during physical activity, psycho-emotional stress, or bumpy driving. The occurrence of pain is associated with the movement of stones in the biliary tract and their infringement in the neck of the gallbladder or cystic duct, increased pressure in the gallbladder or ducts as a result of impaired outflow of bile. Often an attack of hepatic colic is accompanied by nausea and repeated vomiting mixed with bile, which does not bring relief to the patient. Colic can last from a few minutes to several hours. Patients are restless and often change position, trying to find a comfortable position that reduces the intensity of pain. This form of cholelithiasis is called painful paroxysmal.
Diagnosis of cholelithiasis
The diagnosis of cholelithiasis is made on the basis of: patient complaints, medical history, physical examination by a doctor and mainly according to instrumental examination data. At the same time, to make a diagnosis, it is often enough to conduct only one ultrasound examination of the abdominal organs, in which stones are detected in the lumen of the gallbladder or in the ducts. The patient examination can also be supplemented with X-ray examination. In this case, radiocontrast techniques are used, such as oral cholecystography or intravenous cholecystocholangiography. With the first method, the patient takes a special radiocontrast drug inside, several hours before taking an x-ray, which is captured by the liver cells and released into the bile. During cholecystocholangiography, a radiopaque contrast agent is administered intravenously; it is also captured by liver cells and released into the bile. After contrast, an x-ray is taken and if a defect in the filling of the lumen of the gallbladder or ducts is detected, this may indirectly indicate the presence of stones (stones) in them, although the same x-ray picture can be given by both polyps and a cancerous tumor of the gallbladder. Currently, the X-ray method for diagnosing cholelithiasis is practically not used due to its low information content, low cost-effectiveness, and lack of ease of use.
Treatment of cholelithiasis
Currently, surgical treatment is the only possible way to radically get rid of cholelithiasis.
There are still no effective drugs that can cause the dissolution of stones in the gallbladder and bile ducts. Some drugs can dissolve only certain types of stones, but with long-term use they cause serious side effects and complications.
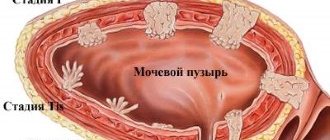
There is an alternative, less traumatic surgical method for treating gallstone disease, such as extracorporeal shock wave lithotripsy. The essence of the method is the destruction of gallstones by a shock wave generated by a special device. The shock wave is strictly focused on the gallbladder, under its influence the stones are crushed into small fragments and sand, which in some cases, along with bile, are released into the duodenum. Despite the simplicity of this treatment method and its low invasiveness, the effectiveness of treatment remains very low even today. This is due to the fact that not all stones can be crushed. In 10–30% of cases, fragments of destroyed stones are large and cannot exit through the natural opening of the common bile duct. In this case, they can become pinched in the neck of the gallbladder and lead to a severe attack of hepatic colic, or get stuck in the common bile duct and disrupt the flow of bile into the duodenum, which will lead to the development of obstructive jaundice. Both of these conditions require immediate hospitalization in a surgical hospital! The shock wave not only destroys stones, but in some cases causes serious damage to the liver and gallbladder walls. The use of extracorporeal lithotripsy in patients with gallstone disease should be carried out according to certain indications: single cholesterol (X-ray negative) stones with a diameter of no more than 3 cm, occupying no more than half of a well-functioning gallbladder. This bloodless method is especially indicated in the treatment of elderly and senile patients. Contraindications for lithotripsy are: x-ray positive stones (with the inclusion of calcium salts), stone diameter more than 3 cm, multiple stones occupying more than half of the gallbladder, disabled gallbladder, history of frequent renal colic, inflammatory diseases of the hepatoduodenal zone.
To date, many methods of surgical treatment of cholelithiasis have been developed. With any type of surgical treatment, stones are completely removed along with the gallbladder - the main pathogenetic substrate of the disease! This completely eliminates the return of the disease.
The absolute indications for surgical treatment of gallstone disease are:
- history of severe attacks of hepatic colic;
- the presence of large stones that can cause a pressure sore of the bladder wall;
- the risk of developing gallbladder cancer, which occurs in 5% of patients suffering from gallstone disease for a long time;
- small bladder stones that can block the cystic duct, penetrate the common bile duct and cause obstructive jaundice, cholangitis, biliary acute or chronic pancreatitis.
A relative indication for surgical treatment is the presence of latent and dyspeptic forms of cholelithiasis.
The main type of surgery for gallstone disease is traditional (open) cholecystectomy (removal of the gallbladder). In this case, various types of accesses (incisions) are performed through the anterior abdominal wall and penetrate into the abdominal cavity. After intraoperative inspection of the gallbladder, extrahepatic bile ducts, duodenum and pancreas, and assessment of the nature of pathological changes, its complete removal is performed. The classical approach provides wide access to the hepatobiliary zone and a good overview of all interested organs, however, it is associated with significant tissue trauma (especially the anterior abdominal wall), which leads to a rather long period of postoperative rehabilitation and a higher risk of complications in the operating room compared to minimally invasive techniques wounds.
Currently, the most popular are minimally invasive surgical interventions in the treatment of cholelithiasis, such as mini-access cholecystectomy and laparoscopic cholecystectomy.
Advantages of laparoscopic surgery
Pain in the postoperative period is minor and, as a rule, is observed only on the first day.
Immediately after recovery from anesthesia (several hours after the operation), the patient can walk and care for himself.
The length of hospital stay is much reduced (up to 1–4 days), as is the time required to restore working capacity.
The number of postoperative hernias is reduced several times.
Laparoscopic surgery is a cosmetic operation; after a few months, scars after punctures become almost invisible in most patients.
Cholecystitis - inflammation of the gallbladder
Often develops with cholelithiasis (so-called stone cholecystitis, up to 80–90% of the total number of diseases [1]), after viral hepatitis and other infectious diseases, in the presence of chronic focal infection (for example, tonsillitis) or parasitic diseases (for example, opisthorchiasis). The development of cholecystitis is facilitated by stagnation and changes in the composition of bile, which may be associated with dietary habits. Often cholecystitis is combined with cholangitis.
There are calculous (presence of gallstones in the bladder) and acalculous, acute and chronic cholecystitis.
Diagnosis of cholecystitis
- Ultrasound of the abdominal organs with examination of the gallbladder, bile ducts, and pancreas.
- General and biochemical blood test.
- X-ray examination (if obstructive jaundice develops and the presence of stones in the bile ducts is suspected).
Acute cholecystitis
The main signs of acute cholecystitis: paroxysmal pain in the right half of the abdomen, radiating to the right shoulder and shoulder blade; nausea and vomiting; chills and increased body temperature; Jaundice and itching of the skin are possible. A dangerous complication of acute cholecystitis is peritonitis. Cholecystostomy (Greek chole bile + kystis bladder + stoma opening, passage) is indicated - external drainage of the gallbladder when other interventions are impossible.
The presence of stones in the gall bladder is an indication for surgery.
This is due to the fact that the presence of stones in the gallbladder can at any time lead to acute cholecystitis, its necrosis with the development of complications:
- empyema of the gallbladder - infection of the contents of the gallbladder;
- hydrocele of the gallbladder - a violation of the outflow of bile, but without its infection, while the elements of bile are absorbed, and the bladder remains filled with transparent contents;
- phlegmon of the gallbladder - purulent inflammation of the wall of the gallbladder;
- subhepatic abscess;
- biliary fistulas;
- peritonitis, sepsis are deadly complications that can develop with the progression of the complications described above.
If complications develop, the operation is performed on an emergency basis and is associated with a high risk of complications, and the rehabilitation period ranges from several weeks to several months!!!
Chronic cholecystitis
Chronic cholecystitis can be acalculous and calculous, from the Latin word “calculus”, which means “stone”. Calculous cholecystitis is one of the results of cholelithiasis. Chronic cholecystitis is manifested by nausea, dull pain in the right hypochondrium and other unpleasant sensations that occur after eating. In recognizing cholecystitis, laboratory data and cholecystocholangiography play an important role.
The most serious complication of calculous cholecystitis is hepatic colic. If a small stone (less than 1 cm) does not pass through the bile ducts, blocking the flow of bile, then bile pigments enter the blood and subhepatic jaundice develops.
The symptoms of colic are very similar to the onset of acute cholecystitis. However, colic hurts much more severely and usually begins at night or early in the morning.
After some time, the symptoms of jaundice appear: yellowing of the sclera and skin occurs - a peculiar lemon-yellow color appears, urine darkens and becomes like beer, and feces noticeably lighten, even white.
Patients in this condition are subject to emergency hospitalization.
Chronic cholecystitis can be a consequence of acute cholecystitis, but it can also occur independently. In Russian medical literature, it is customary to distinguish typical and atypical types of symptoms of gallbladder diseases (cholelithiasis-K 80.2 and chronic cholecystitis).
The presence of stones in the gall bladder significantly complicates the task of treatment and worsens the prognosis of the disease.
Share this page:
When the procedure is prohibited
We list the absolute contraindications to crushing stones:
- calculi are calcium in composition;
- too many inclusions: 3 or more;
- the stones are too large: their total diameter is 3 cm or more;
- blood clotting is impaired;
- there are cysts or vascular aneurysms in the path of the shock wave;
- cholecystitis;
- duodenal ulcer;
- pancreatitis;
- obstruction of the ducts;
- use of pacemakers;
- pregnancy.
How is lithotripsy performed?
Shock wave generators are:
- electrohydraulic;
- magnetically restrictive;
- piezoelectric.
Laser crushing
Cutting stones using a laser is also called percutaneous cholecystotomy, and this highly effective treatment is prescribed in cases where surgery cannot be performed.
This method prevents bacteria and viruses from entering the wound. The body recovers as quickly as possible after such exposure. During a 20-minute session, the stones are broken into fine sand and removed painlessly.
Laser crushing refers to laparoscopic operations. A laser tube is inserted into the stone through a small incision in the abdomen. Manipulations are carried out under ultrasound supervision. After the session, the hole is drained for a week.
Due to the fact that the procedure does not affect the metabolism in any way, every second patient experiences a relapse - and the stones grow again.
Contraindications to laser crushing:
- inability to bring the laser tube to the stone;
- blood diseases;
- viral infection;
- pregnancy;
- the patient's weight is more than 120 kg;
- oncological diseases.
Shock wave crushing
The shock wave (or ultrasonic) method, unlike the laser method, does not require any incisions at all. The stones are destroyed by ultrasonic pulses that pass unhindered through the body tissues. The shock wave is generated under water, and is focally applied to the patient’s body through a bag of water, which is placed on the skin lubricated with gel.
After processing, the stones break down into smaller pieces and then come out. However, if they are hard, they may not break even after several sessions. The easiest to crush are urate and oxalate formations up to 25 millimeters in size.
Contraindications to ultrasonic crushing:
- the patient's weight is more than 120 kg;
- height more than 2 meters;
- diseases of the heart, blood, blood vessels;
- pregnancy;
- acute viral diseases.
Before the session, blood-thinning medications and antibiotic therapy are prescribed several days before the session in case of identified infections.
The duration of the session is no more than 1 hour, it is performed under general or local anesthesia. Pain can be observed both during the manipulation and over the next 2 weeks, when stone fragments come off. These pieces are quite large and have sharp edges. Therefore, they can injure the mucous membranes, cause severe colic or completely block the duct.
Contact chemical cholelitholysis
This technique has appeared recently, it is more experimental than practical. Necessary conditions for its implementation:
- cholesterol formations;
- the organ is fully functional and not inflamed;
- the ducts are completely passable.
The essence of the method: a catheter is inserted into the gallbladder through a peritoneal puncture, and through it a potent substance is supplied to the calculus, which dissolves the stone-forming substance. After some time, the “cocktail” is sucked out with a syringe and another portion of the solvent is supplied. The session lasts 4–16 hours.
For solidified cholesterol, methyl tert-boryl ether is used as a solvent. This substance does not irritate the mucous membrane, but is not able to completely dissolve the solid formation. New layers quickly grow on the remaining fragments. Therefore, the technique is not self-sufficient; it can only be used as an addition to traditional therapy.
Cons of the procedure
Gastroenterology clinics, where they were the first to practice lithotripsy, quickly became disillusioned with this method of treatment. Expensive equipment is practically idle. And there are two main reasons for this:
- Firstly, it turned out that after shock wave exposure, the wall of the gallbladder loses the ability to contract normally. In fact, it turns into a stone collection bag, which must be removed surgically. As practice has shown, most patients who have undergone lithotripsy sooner or later have their organ removed.
- Secondly, evacuation of fragments in half of the cases occurs with severe colic. The high risk of its occurrence lasts 2 weeks, and at this time the patient is already at home or at work. The patient's condition in this case requires emergency medical care. If the duct is completely blocked by a large fragment, then urgent surgical intervention is required within 3 hours after the onset of colic. Otherwise, death is possible due to rupture of the gallbladder or due to painful shock.
Sharp-edged fragments injure mucous membranes along the way. These microtraumas take time to heal. Also, scratches can become a gateway to infection and provoke various inflammatory processes in the digestive tract.
Therefore, most gastroenterologists have practically abandoned such therapy, preferring to solve the problem immediately radically: by removing the gallbladder on the operating table. Thus, cholelithiasis became a surgical pathology.
Causes of the disease
There are three main reasons for the formation of stones: metabolic disorders, bile stagnation and inflammatory changes in the wall of the gallbladder. Recently, there has been an increase in the prevalence of gallstone disease, which is associated with changes in the diet and lifestyle of the modern population. Abuse of fatty and fried foods leads to changes in the composition of bile, changes in the ratio of cholesterol and bile acids. Bile becomes lithogenic, i.e. prone to stone formation. The components of bile precipitate and form a substrate for further precipitation of cholesterol, bilirubin and calcium crystals on their surface. Lithogenic bile can be compared to sticky snow during the thaw period, when snow masses easily stick to a snowball. It is known that gallstone disease often develops in patients with metabolic diseases such as diabetes, obesity and hemolytic anemia.
Damage to the gallbladder wall is also important in the formation of stones. Most patients have bacteria in their bile that leads to the destruction of the inner layer (epithelium) of the gallbladder. The desquamated particles serve as the basis for the precipitation of bile components, which were previously in dissolved form, into a crystalline state - stones are formed.
Prolonged stagnation of bile leads to its thickening and also contributes to the precipitation of bilirubin, cholesterol and calcium into crystals.
The most common site for stone formation is the gallbladder.