Human helminth infections
G
Helminthiasis is a group of diseases caused by parasitic worms - helminths.
Parasitism of over 250 species of helminths has been registered in humans, which belong mainly to two types of worms: roundworms - Nemathelminthes
(class
Nematoda
) and flatworms -
Plathelminthes
(class of tapeworms -
Cestoidea
and flukes -
Trematoda
). Depending on the characteristics of biology and the ways of their spread, 3 groups of helminths are distinguished: geohelminths, biohelminths and contact helminths.
The most common nematodes are geohelminthiases. According to official WHO data, about 1.2 billion people in the world are affected annually by ascariasis, hookworm disease - more than 900 million, trichuriasis - up to 700 million. V.P. Sergiev (1998) believes that the current prevalence of helminthiases among residents of various continents of the Earth is not much different from the assessment of the situation given by Le Riche back in the 60s: for every resident of Africa there are on average more than 2 types of helminths, in Asia and Latin America - more than 1 species, in Europe every third inhabitant is affected. In our country, at the end of the 20s, a scientifically based fight against helminthiases began, which led to a significant reduction in the incidence of the population. In recent years, there has again been a tendency towards an increase in the incidence of certain helminthiases, primarily nematodes (enterobiasis and ascariasis), and the number of patients with toxocariasis and trichinosis is growing; The epidemic situation in the foci of the spread of biohelminthiases - opisthorchiasis, diphyllobothriasis, taeniasis, echinococcosis - is not improving.
| In Europe, every third resident is affected by helminthiases. |
Helminthiasis is characterized by a relatively slow development of the disease, a chronic course, often with long-term compensation. More pronounced pathological changes are caused by the larval and developing stages of helminths. Depending on the location of the pathogen, helminthiasis is distinguished between luminal and tissue
. The latter include diseases such as schistosomiasis, filariasis, echinococcosis, paragonimiasis, cysticercosis and a number of others. In some intestinal helminthiases, the tissue phase corresponds to the initial migration period of the disease (ascariasis, hookworm disease).
Phases of the disease
In the pathogenesis and clinical picture of helminth infections, there are 2 main phases: acute - the first 2-3 weeks after invasion (in severe cases - up to 2 months or more) and chronic, lasting from several months to many years.
In the acute phase
Pathological changes predominate due to a general allergic reaction to antigens of migrating larvae, the early stages of developing parasites. During this period, the leading syndromes are characterized by stereotypicality, regardless of the type of pathogen, its localization and the routes of migration of larvae. Fever, edema, skin rashes, myalgia, arthralgia, lymphadenopathy, pulmonary, abdominal syndromes, hepatosplenomegaly, eosinophilia in the blood, dysproteinemia are observed.
The leading and prognostically serious organ and systemic lesions of the acute phase are: allergic myocarditis, pneumonia, meningoencephalitis, hepatitis, disorders in the hemostatic system.
In the chronic phase
the nature of developing disorders and associated clinical manifestations is largely determined by the localization of the pathogen, its number, and nutritional characteristics. The pathogenic effect of many types of helminths is due to a mechanical traumatic effect on tissues and organs in places of parasitism, compression of vital organs (hydatid cyst in the liver; cysticercus in the brain, eyes, etc.).
Changes in metabolic processes in the body occur due to the absorption of metabolically valuable nutrients by helminths, disruption of neurohumoral regulation and the processes of food absorption in the intestines. In a number of helminthiases, there is a pronounced causal relationship with anemia and vitamin deficiency (hookworm disease, diphyllobothriasis, trichocephalosis, schistosomiasis).
And in this phase, the factor of the pathogen’s influence on the host’s immune system continues to play a significant role. One of the important causes of organ and systemic damage, especially in tissue helminthiases, is the formation of immune complexes. Along with stimulating the immune response, helminths have an immunosuppressive effect. This negatively affects a person’s resistance to bacterial, viral and other infections and reduces the effectiveness of preventive vaccinations.
There are indications of the possibility of transphase and transovarian transmission of enteroviruses, Shigella, cholera vibrios and other infectious agents by helminths. Some helminthiases, characterized by pronounced proliferative processes in the affected organs (schistosomiasis, opisthorchiasis, clonorchiasis), increase the risk of carcinogenesis.
In addition to immunosuppression, the phenomenon of immunological tolerance also occurs during helminthiasis. In the clinical aspect, this is reflected by the absence of an acute phase, subclinical or mild course of the chronic disease. The intensity of the immune response changes at different stages of invasion: it is more pronounced during the presence of larvae in the body. After spontaneous recovery or deworming, specific antibodies disappear within 6–12 months. Among helminthiases common in our country, stable immunity is characteristic only of trichinosis, due to the presence of encapsulated larvae of the pathogen in the muscles.
Clinical picture
Acute phase
In clinically pronounced forms of various helminthiasis, the first signs appear at different times after infection: with ascariasis, manifestations of the acute phase are observed already on the 2-3rd day, with most other helminthiases - after 2-3 weeks, with filariasis the incubation period lasts 6-18 months . Characteristic manifestations of general allergic reactions are: fever, recurrent itchy skin rashes, swelling (from local to generalized), enlarged lymph nodes, myalgia, arthralgia, in the peripheral blood - leukocytosis with hypereosinophilia. Against this background, pulmonary syndrome (from minor catarrhal phenomena to asthmatic conditions, pneumonia and pleurisy) and abdominal syndrome (abdominal pain and dyspeptic disorders) often develop. The liver and spleen increase in size, and symptoms of the central nervous system (CNS) of varying severity are possible.
| In the acute phase, different helminthiases have similar clinical manifestations: fever, rashes, lymphadenopathy, myalgia, pulmonary and abdominal syndromes. |
Due to the common pathogenesis, different helminthiasis in the acute phase have similar clinical manifestations, but there are also specific signs.
With trichinosis, in typical cases, from the first days of the disease, fever, muscle pain, swelling of the eyelids and face are observed; with liver trematodes (opisthorchiasis, fascioliasis), jaundice, enlarged liver and spleen are more often expressed, with ascariasis - pulmonary and abdominal syndromes. Chronic phase
In the chronic phase of helminth infections, the nature of clinical manifestations, the severity of the course and outcomes depend on the intensity of invasion and the habitat of the parasite, and sometimes on its size. With most intestinal helminthiasis, parasitism of individual individuals is usually asymptomatic, and only in the presence of large-sized helminths (wide tapeworm, taeniaids, etc.) are any symptoms observed. For each type of helminth, there is a certain level of parasite abundance at which clinical manifestations occur.
In the chronic phase, symptoms and syndromes predominate, reflecting dysfunction of the organ or system in which the pathogen parasitizes, or which are under the influence of its pathogenic factors.
For intestinal helminthiasis
Dyspeptic, pain and often asthenoneurotic syndromes predominate, more pronounced in children.
With enterobiasis
, the leading one is perianal itching in the evening and at night;
trichocephalosis
in cases of intense invasion can be accompanied by hemorrhagic colitis, and in children sometimes rectal prolapse occurs.
Ascariasis
when parasitized by a large number of helminths can be complicated by intestinal obstruction, obstructive jaundice, and pancreatitis.
In patients with hookworm disease
even with moderate intensity of invasion, iron deficiency anemia naturally develops, associated with hematophagy of the pathogen and blood loss from the damaged intestinal mucosa.
Strongyloidiasis
is characterized by great polymorphism : along with a variety of allergic and dyspeptic symptoms, dysfunction of the biliary tract is often observed.
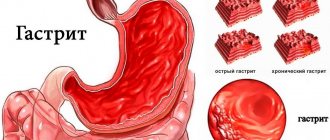
With liver trematodes
(opisthorchiasis, clonorchiasis, fascioliasis),
chronic cholecystocholangitis, hepatitis, pancreatitis naturally develop, damage to various parts of the gastrointestinal tract is possible, and neurological disorders are also observed.
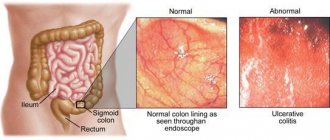
Schistosomiasis
within Russia they are found only in the form of imported cases of chronic forms. A characteristic symptom of genitourinary schistosomiasis is “terminal hematuria” - the appearance of a drop of blood at the end of urination and dysuric disorders. The clinical picture of intestinal schistosomiasis is dominated by symptoms of colitis, and during periods of exacerbation of the process - hemocolitis; over time, hepatosplenomegaly and signs of portal hypertension develop.
In patients with filariasis
, also registered in our country as an imported pathology, allergic syndrome and lymphadenopathy are expressed to varying degrees; characteristic of lymphatic filariasis (wuchereriosis and brugiosis), lymphangitis and lymphostasis are rarely observed in endemic regions, as are serious eye lesions in patients with imported onchocerciasis.
Intestinal cestodiasis (diphyllobothriasis, teniarinhoz, taeniasis, hymenolepiasis)
in many cases they are asymptomatic, manifesting themselves only by the passage of mature helminth segments on their own (with teniahrynchiasis) or during defecation. Some infected people experience dyspeptic disorders and pain; Patients with diphyllobothriasis develop anemia caused by vitamin B12 deficiency.
Among helminthiases, a special place is occupied by larval cestodiases: echinococcosis, alveococcosis, cysticercosis
.
They can be asymptomatic for a long time, even in the presence of fairly large cysts. At the same time, rupture or suppuration of even a small echinococcal bladder leads to serious consequences: the development of anaphylactic shock, purulent peritonitis, pleurisy, etc. As a result of compression of the portal and inferior vena cava by a growing bladder or alveococcus, portal hypertension develops. Cysticercosis
of the central nervous system occurs in the form of cerebral and spinal lesions with various symptoms; localization of the helminth in the ventricles of the brain is accompanied by signs of intracranial hypertension.
Toxocariasis
is expressed by abdominal and pulmonary syndromes, neurological disorders, eye damage, and blood eosinophilia.
Laboratory diagnostics
Biological material for research on the presence of helminths, their fragments, larvae and eggs are feces, urine, duodenal contents, bile, sputum, rectal and perianal mucus, blood, and muscle tissue. The most common object of study is feces. Macroscopic methods
used to detect isolated helminths or their fragments; the purpose of microscopic examination is to detect eggs and larvae.
For widespread use, including in field conditions, the Kato method is recommended, based on the detection of helminth eggs in a thick smear of feces cleared with glycerin and tinted with malachite green. The diagnosis of enterobiasis is established on the basis of examination of material obtained from the perianal folds using a swab, spatula, or imprint using adhesive tape. Enrichment methods
are based on the difference in relative density of the solutions used and helminth eggs. In our country, the flotation methods of Kalantaryan and Fulleborn are used. The Ritchie sedimentation method is more effective for detecting schistosome eggs in feces. Helminth larvae (strongylids, hookworms) are detected using special methods. The Berman and Brumpt methods are used to diagnose strongyloidiasis, the Harada-Mori method and its modifications are used to detect hookworm and necator larvae.
Eggs and larvae of helminths that parasitize the liver, biliary tract, pancreas and duodenum are found in bile and duodenal contents. If paragonimiasis is suspected, sputum should be examined, and urine should be examined for genitourinary schistosomiasis.
| With most intestinal helminthiases, parasitism of single individuals is usually asymptomatic. |
To diagnose filariasis, blood (lymphatic filariasis, loiasis) and skin sections (onchocerciasis) are examined.
The frequency of appearance of microfilariae in peripheral blood (night or day) should be taken into account; During the initial examination, it is preferable to take blood for analysis from the patient both during the day and at night. In the diagnosis of the acute phase of helminth infections and diseases caused by tissue helminths or larval stages (echinococcosis, cysticercosis, trichinosis, toxocariasis), serological methods
: RNGA, RSK, RAL, RIF, IFA, etc.
For topical diagnostics, ultrasound examination of organs, computed tomography, and endoscopy with endobiopsy are used.
Treatment
In the acute period, the basis of treatment is desensitization and detoxification. Glucocorticoids are used according to indications only for severe cases of certain helminthiasis (trichinosis, schistosomiasis, liver trematodes) or to prevent allergic complications of chemotherapy (onchocerciasis, loiasis). It should be taken into account that if they are used incorrectly, generalization of invasion (strongyloidiasis) or a transition from the acute phase to a long-term subacute phase (opisthorchiasis, trichinosis, etc.) may occur.
Specific treatment is the basis for combating most human helminthiases. In the last two decades, highly active and low-toxic anthelmintic drugs such as levamisole, thiabendazole, mebendazole, albendazole, medamin, pyrantel
.
Chemotherapy for schistosomiasis and liver trematodes was successfully developed, for the treatment of which praziquantel
.
This drug has also proven to be highly effective for the treatment of intestinal cestodias. Extensive clinical trials of ivermectin
in the treatment of patients with filariasis are being successfully completed.
Widely used in the past to treat nematodes
In recent years, levamisole has been prescribed only for ascariasis at a dose of 2.5 mg per 1 kg of body weight in 1 dose.
Gradually it was replaced by more effective drugs. Mebendazole
for adults is taken 100 mg 2 times a day for 1–2 days for ascariasis and enterobiasis, 3 days for hookworm disease and trichuriasis;
children - at the rate of 2.5–5.0 mg per 1 kg of body weight. Medamin
for the same helminthiasis is prescribed in a daily dose of 10 mg per 1 kg in 3 divided doses 30 minutes after meals.
Pyrantel pamoate
is used for ascariasis and enterobiasis at a dose of 10 mg per 1 kg (no more than 1 g) once, and for patients with hookworm disease - at the same dose for 2-3 days.
Albendazole
has the widest spectrum of action , which is prescribed 200 mg 2 times or 400 mg once for the treatment of patients with hookworm disease and trichuriasis; for ascariasis and enterobiasis, with low intensity of invasion, 200 mg is sufficient.
An indispensable condition for successful deworming of patients with enterobiasis is the simultaneous treatment of all family members (team) and strict adherence to a hygienic regime to exclude reinvasion; in addition, re-treatment is usually carried out at intervals of 10 days.
Medamine
or
albendazole
are used to treat patients with strongyloidiasis .
Specific therapy for patients with trichinosis
is carried out
with mebendazole
100 mg 3 times a day for 7–10 days;
albendazole
.
For the treatment of patients with lymphatic filariasis and loiasis,
diethylcarbamazine
(6 mg per 1 kg per day in 3 doses for 14–21 days) is quite effective
For trematodes and cestodes
Praziquantel
is widely used . For patients with opisthorchiasis, clonorchiasis, and paragonimiasis, it is prescribed in a daily dose of 75 mg per 1 kg (in 3 doses) for 1 day, for schistosomiasis, depending on the form, in doses from 40 mg per 1 kg once to 60 mg per 1 kg in 2 doses; for fascioliasis, the effectiveness of the drug is low; triclabendazole is recommended for these purposes abroad.
For intestinal cestodias
(diphyllobothriasis and taeniasis) deworming is achieved with a single dose
of praziquantel
at a dose of 20 mg per 1 kg, for hymenolepiasis the same dose is prescribed 2 times with an interval of 10 days, for cerebral cysticercosis abroad the same drug is used in a daily dose of 50 mg per 1 kg in 3 reception for 14 days or more. Specific treatment for other larval cestodiases – echinococcosis and alveococcosis – has not yet been practically developed.
A set of therapeutic measures must be carried out in accordance with the characteristics of the pathological effect of a particular pathogen and the characteristics of the course of helminthiasis in the infected person.
Prevention
Prevention of helminthiasis includes a set of measures to identify patients, treat them, ensure living conditions, everyday life and production that exclude the spread of these diseases, protect and improve the environment from pathogens. Requirements for the prevention of certain groups of parasitic diseases are different and are regulated by relevant regulatory documents.
The volume and nature of the measures taken to reduce the incidence of the most common geohelminthic infections among the population of the Russian Federation (ascariasis and trichuriasis) are determined by the level of infection, climatic conditions, the characteristics of everyday life and economic activities of the population and the results of sanitary and helminthological monitoring, since geohelminthic infections are primarily a sanitary problem .
The basis for the prevention of trichinosis, teniarynchosis, taeniosis is to ensure the safety of meat products for human health, and the prevention of opisthorchiasis, clonorchiasis, metagonimiasis, nanophyetosis, paragonimiasis, diphyllobothriasis, anisakiasis, heterophyosis, sparganosis and other helminthiases transmitted through fish, crustaceans, mollusks and reptiles, is to ensure guaranteed safety of fish and other related products. Prevention and control of echinococcosis and alveococcosis is carried out through measures aimed at preventing infection of humans, farm animals, dogs, health education, and regular medical examinations of risk groups (reindeer herders, fur breeders, hunters). In the prevention of helminthiases transmitted by contact (enterobiasis, hymenolepiasis, as well as strongyloidiasis), the main importance is measures aimed at breaking the transmission mechanism of their pathogens, it should be taken into account that the first two helminthiases predominantly affect children in organized groups, and strongyloidiasis is registered in in the form of outbreaks in specialized institutions (psychiatric institutions, etc.) and poses a danger to patients with reduced immunity. Literature:
1. Vasiliev V.S., Komar V.I., Tsykunov V.M. Infectious disease practice, Minsk, Higher School, 1994; 494.
2. Geller I.Yu. Echinococcosis. M., Medicine, 1989; 208.
3. Human helminth infections, edited by Prof. V.I. Luchshev, MD. V.V. Lebedeva; manual for doctors. Krasnodar. “Soviet Kuban”, 1998; 124.
4. Human helminth infections. Ed. F.F.Soprunova, M., Medicine, 1985; 368.
5. Ozeretskovskaya N.N., Zalnova N.S., Tumolskaya N.I. Clinic and treatment of helminthiases. L., Medicine, 1985.
6. Prevention of parasitic diseases on the territory of the Russian Federation; Sanitary rules and regulations. M., Information and Publishing Center of the Ministry of Health of Russia, 1997; 168.
7. Guide to infectious diseases Ed. Yu.V. Lobzina, A.P. Kazantseva, St. Petersburg, TIT Cometa, 1996; 720.
8. Sergiev V.P., Drynov I.D., Malyshev N.A. Problems of health care reforms. Approaches and prospects. M., 1998; 120.
9. Sergiev V.P., Lebedeva M.N., Frolova A.A., Romanenko N.A. Epidemiology and infectious diseases. 1996; 2:8–11.
10. Tokmalaev A.K. Clinical characteristics and treatment of the most important imported helminthiases. Dissertation of Doctor of Medical Sciences. M., 1990; 364.
11. Yushchuk N.D., Vengerov Yu.Ya. Lectures on infectious diseases. In two volumes, 2nd ed., revised. and additional M., VUNMTs, 1999; 433.
12. Yarovoy P.I., Zubchuk M.P., Tokmalaev A.K. Handbook of medical helminthology, ed. K.M.Lobana. Kishinev; Kartya Moldovenaske, 1984; 288.
13. Yarotsky L.S. Schistosomiasis, M., Medicine, 1982; 280.
14. Anderson RM and May RM Infectious Diseases of Humans. Oxford, Oxford University Press, 1991.
15.Cioli D/ Chemotherapy of schistosomiasis: An update. Parasitology Today, 1998, 14; 418–22.
16.Control of Foodborne Trematode Infections (WHO, Techn. Rep. Ser. 849), Geneva, 1995.
17. Control of Schistosomiasis (WHO, Techn. Rep. Ser. є830), Geneva, 1993.
18. Report of the WHO Informal Consultation on monitoring of drug efficacy in the control of schistosomiasis and intestinal nematodes, Geneva, 1998.
19. De Silva N., Guyatt H., Bundy DAP Anthelmintics: a comparative review of their clinical pharmacology. Drugs, 1997; 53 (5): 769–88.
20. Warren KS et al. Helminth infection. In: Jamison DT et al. eds. Disease control priorities in developing countries, Oxford, University Press, 1993.
21. WHO. Basic Laboratory Methods in Medical Parasitology, Geneva, 1991.
22. WHO. Report of the WHO Informal Consultation on Hookworm Infection and Anaemia in Girls and Women, Geneva, 1996.
Mebendazole–
Vero-mebendazole (trade name)
(Veropharm)
(trade name)
Classification
There is no unified classification of helminthiases. The disease is divided into types according to localization, type of pathogen and stage.
| Classification sign | Form | Explanation |
| Type of pathogen | Roundworms (nematodes) | Roundworms are a common type of worms, more often diagnosed in children (enterobiasis, ascariasis, toxocariasis, etc.) |
| Tapeworms (cestodes) | Tapeworms are the largest parasites; they cause serious harm to health (echinococcosis, alveococcosis, taeniasis, etc.) | |
| Flukes (trematodes) | Flukes are flat helminths that lead a completely parasitic lifestyle (opisthorchiasis, heterophyosis, fascioliasis, etc.) | |
| Localization | Intestinal | Intestinal diseases include ascariasis, strongyloidiasis, trichuriasis, teniarinchiasis. |
| Pulmonary | The pulmonary form is caused by tominxosis and paragonimiasis. | |
| Fabric | Schistosomiasis, trichinosis, toxocariasis and filariasis develop in tissues. | |
| Hepatobiliary (gall bladder, bile ducts and liver) | The hepatobiliary system is affected by opisthorchiasis, fascioliasis and clonorchiasis. | |
| Stage | Acute | The acute stage appears several weeks after infection. Symptoms of the disease appear within one to two months, then the disease becomes chronic. |
| Chronic | Clinical manifestations of chronic helminthiasis depend on the type of parasite. An allergic reaction may occur. |
Diagnostics
Helminthiasis can be suspected as a result of a general clinical blood test. In the case of a parasitic infection, eosinophils (white blood cells produced when a foreign protein structure penetrates) are increased and pronounced leukocytosis is observed (an increase in the number of protective blood cells - leukocytes).
If indicated, a set of tests should be done. Methods for laboratory diagnosis of helminths:
- coproovoscopy (examination of stool for worm eggs);
- microscopic examination (helps to detect eggs, larval forms);
- macroscopic examination (detects whole helminths: roundworms, pinworms);
- scraping from the anal folds (reveals enterobiasis);
- study of bile content;
- immunological blood test;
- examination of duodenal contents (detects parasites in the duodenum using probing);
- biopsy of muscle tissue (if trichinosis is suspected);
- blood test for the presence of antibodies to helminth infections;
- ultrasound and x-ray (allow you to clarify the location of helminths).
It is not always possible to identify worms the first time. To increase the likelihood of detecting helminths in feces, it is necessary to be tested three times every 3-4 days. Each test must be interpreted correctly. Only a doctor can do this. He needs an in-person examination of the patient to identify signs of helminthiasis.
Complications
Complications of helminthiasis depend on the type of parasite, the degree of infestation and the stage of the disease. Modern medicine makes it possible to detect invasion in time and take therapeutic measures. However, sometimes damage to organs by parasites leads to serious complications:
- intestinal obstruction (a ball of helminths interferes with the passage of feces);
- inflammation of the gallbladder due to the penetration of parasites into the biliary tract;
- pancreatitis (inflammation of the pancreas);
- purulent ulcers on the skin around the anus (develops with enterobiasis);
- anemia (decrease in the amount of hemoglobin – an iron-containing protein that delivers oxygen to the body’s tissues);
- acne;
- damage to the nervous system;
- perforation (occurrence of a through defect) of the intestinal walls;
- various liver diseases.
Note. The most serious complication is considered to be depression of respiratory function due to helminths entering the lungs. If medical assistance is not provided in time, death is possible.
Prevention
Prevention of helminthiasis in children and adults should be carried out regularly. A number of rules must be followed:
- wash your hands regularly with soap;
- use personal hygiene items;
- wash vegetables, berries, fruits thoroughly before eating;
- drink water only from proven sources;
- do not eat poorly cooked meat;
- do not eat raw, under-salted fish, undercooked crayfish, crabs;
- swim only in permitted bodies of water;
- carry out wet cleaning;
- Avoid traveling to unfavorable tropical countries.
An important preventive measure is periodic examination of the population, especially medical workers and catering establishments. To avoid the formation of a focus of infection, all family members of the patient diagnosed with helminthiasis are treated simultaneously.
Pathogenesis
All helminthiases are characterized by the presence of several stages of development, each of them has its own clinical manifestations. The most difficult stage for the body is considered to be the initial stage – the acute period. At this time, helminths migrate to the internal organs. Allergic reactions and sensitization (specific hypersensitivity) to parasite antigens are formed. During the chronic stage there is no longer such a pronounced reaction. During their life, parasites release toxins that cause toxic-allergic reactions. Mechanical damage to internal organs also causes the appearance of typical symptoms of the disease.
Causes and routes of infection by helminth infections
The occurrence of a certain form of helminthiasis occurs through various methods of infection. More than three hundred species of parasites are known that live in the human body. There are three ways of infection with helminths:
- biohelminthiasis (carriers of parasites – animals);
- contagious (carrier is a sick person);
- geohelminthiases (infection through the soil).
Common helminthiases in adults and children include enterobiasis (pinworms), ascariasis (roundworms), trichuriasis (whipworm), giardiasis (giardia). Roundworms and whipworms enter the human body by consuming unwashed vegetables and fruits. Infection with pinworms is possible by ingesting their eggs, at the same time the patient actively releases them into the external environment. Giardia reaches humans through food, water, and household items.
Helminths can be located on the fur of pets, and close contact with them leads to infection. For animals (especially if they live in the house) it is also necessary to carry out antiparasitic prevention once every three months.
Treatment
If you suspect a helminthic infestation, you should make an appointment with a general practitioner (pediatrician), infectious disease specialist or gastroenterologist. The main goal of treatment for helminthiasis is to expel parasites from the body and restore the functioning of its systems. Treatment can be prescribed only after a comprehensive examination and identification of the type of parasite.
Positive tests are a reason to prescribe specific anthelmintic drugs or their combinations. As a rule, it is necessary to use the remedy twice in order to destroy both the worms themselves and their eggs. The dosage is determined individually depending on the age and weight of the patient. In the acute phase, detoxification therapy is carried out:
- intravenous administration of water-salt solutions;
- vitamin therapy (vitamin B6, ascorbic acid);
- antihistamines.
In severe cases, the prescription of hormonal drugs is indicated. At the same time, symptomatic treatment is carried out to improve the patient’s condition. Complex therapy may include iron supplements (for established anemia), choleretic agents, enzymes, folk treatment methods with decoctions and herbal infusions (can only be used after consultation with a doctor).
Doctors cannot determine exact statistics on the number of cases, since many do not turn to them when they detect symptoms of the disease, but prefer to treat it themselves at home. This approach can lead to serious complications and unpleasant consequences. You should not self-medicate.