Types of proctalgia
Proctalgia can be of a volatile nature, when the pain appears suddenly and disappears abruptly. It can last for several hours and not go away even after taking strong painkillers. The pain is stabbing and spastic in nature.
If we talk about the pathogenetic cause of proctalgia, it is often a neurogenic spasm of the levator muscles of the rectum or coccygeal muscle. The cause may be stress or any other experience, as well as physical strain.
The secondary type of proctalgia is considered a consequence of one of the proctological diseases (hemorrhoids, fissures or tumors of the anal canal, paraproctitis, perianal lesions in the case of Crohn's disease). In addition, proctalgia is also a manifestation of idiopathic anococcygeal pain syndrome. With endometriosis, pain can radiate to the rectal area.
General information
The acromioclavicular joint (shoulder) in shape and structure belongs to simple, spherical joints. It is the most mobile due to the spacious articular cavity, thin, mobile capsule, rounded and different-sized articular surfaces, as well as ligaments, tendons, and powerful muscles that surround it.
The joint cavity is located inside the shoulder capsule, which prevents external influences (ruptures, mechanical damage). It contains dense fibers, giving it high strength, and consists of two layers:
- outdoor
– denser and thicker, compared to the internal one, containing fibrous connective tissue;
- internal
– a synovial membrane that produces a special fluid necessary for nutrition, hydration of joints, and elimination of friction between surfaces.
When there is inflammation in the shoulder capsule (in the inner and outer layers), capsulitis is diagnosed. Pathological processes develop predominantly in adulthood, in patients over 50 years of age, and are observed with equal frequency in both the dominant and non-dominant limbs. In approximately 8-10% of patients, the disease affects both hands with a difference of several months or years.
According to the International Classification of Diseases (ICD-10), adhesive capsulitis of the shoulder is assigned code M75.10. It is classified as a disease of the muscular system and connective tissue and is recognized as a shoulder lesion.
Clinical picture
The transient type of proctalgia is spontaneously occurring and quickly passing pain, characterized by its sharpness in the rectal area. In some cases, such pain can be felt as painful spasms of a convulsive nature. The pain may radiate to the tailbone or anus. Some patients complain of pain in the perineum or even in the hip joints.
The pain may not be associated with the act of defecation. It happens that painful attacks occur with great frequency and progress further, increasingly worsening a person’s quality of life. Often the disease occurs with a feeling of discomfort in the perineal area, giving the patient a reason to think about pathologies of the genitourinary system.
Proctalgia is a long-term disease, occurring in waves, alternating with exacerbations and lulls. Often exacerbations become very severe. What exact factors provoke them is not completely known, but it is assumed that these factors are psycho-neurogenic in nature.
Symptoms of adhesive capsulitis
One of the main symptoms of capsulitis is causeless pain in the damaged joint, sometimes it appears after physical exertion or minor traumatic injury. During the first 2-3 weeks they increase. Aching pain occurs in the evening and at night; it is impossible to lie down on the affected shoulder and roll over from side to side without waking up.
The second important symptom of capsulitis is limitation of motor activity of the affected shoulder. It becomes difficult to turn the arm outward, move it to the side, and over time, problems appear in performing rotational movements with the shoulder. In the future, basic everyday activities become impossible: eating, washing, dressing, undressing, combing.
In some cases, the disease leads to:
- increase in body temperature to a low-grade level;
- feeling of general malaise, body aches;
- redness of the skin and severe swelling of the tissue over the damaged joint;
- pronounced pain.
In addition to debilitating pain, ability to work is impaired. This forces you to consult a rheumatologist. The disease does not have characteristic symptoms, which makes timely diagnosis difficult.
Diagnosis of proctalgia
Usually, when examining for proctalgia, a patient’s history reveals previous diseases of the urinary and genital organs. Proctological abnormalities may also be detected. If we talk about primary proctalgia, then it precedes all these pathologies. Patients, as a rule, say that they have had pain in the rectum before. Primary proctalgia is often a condition for patients to visit a gynecologist (urologist).
In order to make a correct diagnosis, the doctor should conduct a full examination to identify diseases that may be causing pain in the rectum.
Chronic pelvic pain in women
“Pelvic” refers to pain localized in the lower abdomen below the navel, in the lower back and sacrum, as well as in the perineum, in the area of the external genitalia, vagina, and rectum. Irradiation along the anterior inner surface of the thighs and the lower edge of the buttocks is often observed. Typically, patients cannot indicate the exact localization of pain; it is rather diffuse in nature, and it is not always easy to separate the epicenter of pain from the zone of irradiation. The temporal characteristics of pelvic pain - acute or chronic - are of fundamental importance for recognizing the causes and choosing treatment tactics. Acute pelvic pain is usually sudden, severe, and lasts up to several hours or days. Its causes are acute inflammatory diseases of the uterus and appendages, appendicitis, diverticulitis, acute colitis, acute urological diseases or conditions accompanied by ischemia of the pelvic organs or intraperitoneal bleeding - torsion or rupture of an ovarian cyst, ectopic pregnancy, complications of proctosigmoiditis. Acute pain is often accompanied by fever, reflex nausea, vomiting, signs of intestinal paresis, symptoms of general intoxication or internal bleeding. Patients with acute pelvic pain need immediate medical attention. Chronic pelvic pain is recurrent or constant pain that bothers the patient for at least 6 months. The nature of the painful sensations can be different: burning, stinging, stabbing, aching pain, a feeling of pressure or heaviness. The intensity of pain in the same patient can vary significantly [5]. This article will focus on chronic pelvic pain in women due to the particular relevance of this problem. The prevalence of chronic pelvic pain among women, according to the US National Institutes of Health, reaches 15%. Other epidemiological studies are currently being conducted [7]. The studied causes of chronic pelvic pain in women combine various gynecological, urological diseases, as well as diseases of the intestines and musculoskeletal system (Table 1) [17,33]. It is paradoxical that not all women suffering from these diseases develop chronic pelvic pain. The question of the mechanism of pain chronization is urgent. In conditions of persistence of the pathological process, and sometimes in the absence of obvious organic pathology, chronic pain can be the result of a decrease in the threshold of perception, when the pain sensation occurs under the influence of non-damaging stimuli. In such cases, pathophysiologists use the following terms: • hyperalgesia - the occurrence of pain when exposed to soft threshold stimuli; • allodynia – pain when exposed to physiological stimuli that normally do not have an irritating effect; • spontaneous painful spasms - pain that occurs generally in the absence of any influence on the sensory nerve endings. The modern theory of pain explains the formation of chronic pain by dysfunction of the nerve pathways and centers that control the flow of pain impulses. In some cases, the main role is played by a decrease in the activity of the antinociceptive system, in others - the phenomenon of neuronal sensitization, in others - the development of neurogenic inflammation supported by constant nerve impulses and the production of substance P, the peptide encoded by the calcitonin gene related peptide (CGRP), growth factor nerves and neurokinins in the affected organ [2,3,15,25,28]. Surgical interventions on the pelvic organs and rheumatic diseases predispose to the formation of chronic pain [19]. In maintaining painful sensations, great importance is attached to the phenomenon of hyperesthesia/hyperalgesia of soft tissues, manifested, in particular, by the formation of trigger points in the muscles and fascia of the pelvic floor. This phenomenon was first described by the English neurologist H. Head and the outstanding Russian clinician G.A. Zakharyin. Zakharyin-Ged zones, as a rule, correspond to certain dermatomes, at the level of which sensitive innervation of the affected organ and the corresponding area of soft tissue is provided. Pelvic muscle soreness often accompanies urological diseases, and physical therapy for myofascial pain often cures chronic pelvic pain [13]. Chronic pelvic pain is characterized by irradiation, which manifests itself as a feeling of pain, burning or itching in more distant areas simultaneously with the appearance of pain impulses from the affected organ. This phenomenon is, in fact, close to the phenomenon of hyperalgesia of the corresponding dermatome. A number of researchers also point to the existence of visceral hyperalgesia - mutual strengthening of pain impulses due to partial intersection of the innervation paths of two affected organs. It has been shown, for example, that women with inflammatory diseases of the genitals are more likely to suffer from attacks of renal colic; in the same group of patients, pain in the back muscles is often observed at the ThX–LI level. [2,3,15,22]. The threshold for pain perception may be reduced under the influence of negative affective and social factors. Women suffering from chronic pelvic pain (usually in the form of dysmenorrhea, dysparenuria and vulvodynia) are more likely to have a history of physical or sexual abuse and show signs of post-traumatic stress disorder. Such patients are more prone to depression [26]. Due to the variety of causes of chronic pelvic pain, a multidisciplinary research group has been created in the United States based on large medical centers that register and thoroughly analyze the causes of each case [9]. Assessing associated symptoms can be a significant aid in recognizing the cause. Chronic pelvic pain rarely exists as an isolated symptom and is often combined with other complaints; it may be associated with defecation, urination, the menstrual cycle, and sexual intercourse. The most important diagnostic value is the identification of obvious signs indicating, for example, damage to the excretory system (hematuria, dysuria, etc.), genital organs (pathological discharge, menstrual irregularities, infertility, herpetiform rash, papillomatosis, etc.) or intestines (diarrhea, constipation, pathological impurities in feces, etc.). But in many cases, the symptoms are nonspecific, which makes diagnosis difficult. For women suffering from pelvic pain, the following complaints are quite “universal”: pain localized in the abdomen or lower back, very painful menstruation, dysparenuria (pain during sexual intercourse, as well as immediately before or after it), vulvodynia (burning or stabbing pain). pain in the perineum and vaginal opening). In men, the nature of the complaints is somewhat different: the localization of pain in the lower back, difficult or painful urination, pain or discomfort at the base of the penis, around the anus, in the scrotum, pain during ejaculation, and blood in the seminal fluid are more typical. Often these symptoms are unreasonably interpreted as manifestations of infectious prostatitis [5,23]. There is often an “overlap” of symptoms, when the same complaints are noted in different pathological conditions. This is especially true for dysparenuria and vulvodynia. For the purpose of differential diagnosis of chronic pelvic pain, it is important to establish whether it is cyclic (periodic) in nature. A connection with the menstrual cycle most likely indicates a gynecological pathology, in particular endometriosis or venous congestion in the pelvic cavity. “Algodysmenorrhea (syn. dysmenorrhea)” is pelvic pain during menstruation. “Ovulatory pain” is observed in the middle of the menstrual cycle, is associated with ovulation and occurs quite regularly in some women; pain may persist for up to 2–3 days and is relieved by the use of heat or analgesics. And yet, the cyclical nature of pain does not allow us to completely exclude the pathology of neighboring organs that are not related to the reproductive system, since the existence of viscero-visceral reflexes is possible. From the point of view of some specialists, true chronic pelvic pain should mean only cases of non-cyclical pain of unknown origin, when all known organic causes have been excluded. This rigorous approach helps to identify a group of patients with functional pain, often associated with mental disorders, similar to the functional abdominal pain described in the Rome III criteria [26,34]. It must be noted that the diagnosis of “functional pelvic pain” has not yet been reflected in the Rome criteria. Some symptom complexes observed in certain pathological conditions are described below. Chronic pelvic pain due to pathology of the urinary system is most typical for disorders such as interstitial cystitis, bladder stones and tumors, and obstructive uropathy. Symptoms can be very different: • pain (discomfort, feeling of pressure) in the suprapubic region, intensifying as the bladder fills or after it is emptied. • pain in the suprapubic region, urethra during urination; • vaguely localized pain in the pelvic area, with possible irradiation; • imperative calls to urinate and/or frequent urination; • presence of pathological impurities in urine; • dysparenuria. Of particular interest is a disease such as interstitial cystitis (“irritated or painful bladder”). This is a fairly common disease, the causes of which are not well understood. Approximately 90% of patients suffering from this disease are women; worsening symptoms are observed during menstruation or after sexual intercourse. Pelvic pain in interstitial cystitis is often combined with fibromyalgia, chronic fatigue syndrome, and irritable bowel syndrome, which indicates the common pathogenetic mechanisms of pain formation [9]. Chronic pelvic pain in gynecological pathology is characterized by a particularly frequent combination with dysparenuria, vulvodynia, and sometimes with dysuria and is often cyclical in nature. About 15% of visits to a gynecologist are due to chronic pelvic pain. Among the most common causes of pain are endometriosis, inflammation and venous congestion in the pelvis [11,29,32]. Chronic pelvic pain due to inflammation of the pubic symphysis (osteitis pubis) is localized in the pubic area and intensifies during physical activity, when squeezing the hips, climbing stairs or squatting. Chronic pelvic pain with damage to the sensory nerves of the lower abdominal wall and pelvic area – n. Pudendus, n. ilio-inguinale, n. ilio-hypogastrum, n. genito-femoral. Damage to these nerves can occur during childbirth, surgery, or systemic neuropathy. It is possible that in some cases neuropathy is caused by herpetiform viruses. The following symptoms may occur alone or in combination: • dysparenuria; • pain when urinating or defecating; • pain when sitting; • pain in the lower abdomen or back - constant or associated with changes in body position; • pain in the genitals (vulvodynia) radiating along the posterior inner surface of the thighs and buttocks. Chronic pelvic pain in diseases of the rectum. Chronic proctalgia is one of the most common types of pelvic pain. Its causes can be injuries, cracks in the mucous membrane of the rectum and skin around the anus, stercoral ulcers, hemorrhoids, rectal prolapse, recurrent herpetic and cytomegalovirus infections, human papillomavirus infection, tumor, chronic pararectal abscess. Proctalgia is a striking symptom of functional anorectal disorders: musculus levator ani syndrome or nonspecific functional anorectal pain, proctalgia fugax [4,10]. Proctalgia can be observed as part of ischemic colitis, stercoral, ulcerative colitis, irritable bowel syndrome. Pain may be associated with sexual intercourse, bowel movements and passing gas; You should pay attention to pathological impurities in the stool, changes in the perianal area. Chronic pelvic pain against the background of inflammatory bowel diseases is characterized by a combination with tenesmus, diarrhea mixed with blood, mucus and pus, general weakness, and weight loss. Similar symptoms can be observed with ischemic colitis, which is also characterized by persistent flatulence, abdominal pain, and unstable stool. Irritable bowel syndrome (IBS) is one of the most common causes of chronic pelvic pain in patients of both sexes [9]. In typical cases, the pain is localized in the lower abdomen, mainly on the left, is spastic in nature and is combined with diarrhea, constipation, and bloating. The pain intensifies after eating and relieves after defecation. According to the Rome criteria for functional disorders in IBS, periods of pain must necessarily be combined with changes in stool frequency and stool consistency [10]. IBS is also characterized by a feeling of “obstruction” in the rectum when straining during bowel movements, a feeling of incomplete emptying of the rectum, and the release of mucus with feces. When IBS is combined with proctalgia, there is severe stabbing pain in the rectum during bowel movements and the passage of gas. Exacerbation of symptoms is observed against the background of stress, anxiety or depression. Simultaneously with pelvic pain in IBS, a whole range of other symptoms can be observed: dysparenuria, algodismenorrhea, dysuric disorders. It is also very typical to have signs of autonomic dysfunction accompanying migraine and anxiety and depressive disorders. The literature indicates a close relationship between the two most common types of pain in women – pelvic pain and migraine. According to a study by the US National Institutes of Health, chronic pelvic pain occurs in 15-24% of women of reproductive age, and migraines in about 20%. There is an “overlap” of these conditions: no less than 67% of women with chronic pelvic pain have migraine. One possible explanation for this is the peculiarities of prostaglandin or serotonin metabolism and the regulation of smooth muscle cell tone, another is the peculiarities of pain perception in such patients [8]. Myofascial pelvic pain syndrome is a disorder that causes painful trigger points in the pelvic floor muscles. The pain is aching or burning in nature, its localization is varied. On palpation, the muscles of the pelvic floor and pelvic girdle appear tense, and points of sharp pain are identified in them. This is often accompanied by increased sensitivity or itching of the skin, making it difficult to wear clothes. Compression of sensory nerves by muscles also leads to itching and burning. Concomitant dysuric disorders, urgency, constipation, pain during defecation, and dysparenuria are often observed. Probably, myofascial syndrome is formed secondary to traumatic physical activity, joint diseases, frequent straining during bowel movements, repeated genitourinary infections as a consequence of injuries and childbirth - and makes a significant contribution to the persistence of pain. An analysis of medical records showed that patients with diagnoses of “vulvodynia”, “interstitial cystitis”, “chronic pelvic pain”, “non-bacterial prostatitis”, “neuralgia”, “IBS” often have signs of myofascial pelvic syndrome [31]. Dangerous symptoms indicating the likelihood of dangerous complications in patients with pelvic pain: intense or increasing pain, fever (>38.5 ° C) with chills, vomiting with blood, bleeding from the vagina or rectum, signs of blood loss, difficult or painful urination, increasing increase in abdominal size. Diagnostic search. Because chronic pelvic pain and its associated symptoms can occur in different combinations and severity, diagnosis is often difficult. Sometimes the cause of pain remains unrecognized. Analysis of complaints and anamnesis implies a thorough assessment of the nature and localization of pain (lumbosacral region, coccyx region, sacroiliac joint, pelvic floor, groin area, abdominal wall), duration and frequency, and the influence of provoking factors. It is necessary to clarify complaints from all organs and systems, and analyze in detail the gynecological and drug history. Particular attention should be paid to the description of the first episode of pain, which can serve as a key to identifying the “generator” of pain [14]. Rectal and vaginal examination are mandatory components of the examination of a patient with chronic pelvic pain. It allows you to identify diseases of the genital organs, rectum, changes in perirectal tissue and “trigger” points of the pelvic floor [21]. According to experts, a medical examination complemented by an ultrasound examination of the pelvic organs, in most cases, allows you to recognize gynecological pathology that serves as a cause of pain. Experience shows that in order to establish pathology by the intestines or urinary tract, it is often necessary to perform endoscopy with biopsy, irrigoscopy, urography, computed or magnetic resonance imaging [18]. In difficult cases, the question of diagnostic laparoscopy is raised. Only with the help of this study can one reliably confirm the diagnosis of ceremonial endometriosis, adhesive disease and at the same time conduct surgical treatment [16]. Effective treatment, of course, depends on the correctly established basic diagnosis. Due to a wide variety of causes of pelvic pain, the author is not able to examine in detail the treatment of each disease. With cyclic pain, as a rule, associated with premenstrual syndrome, menstruation or ovulation, the use of combined hormonal contraceptives or progesterone preparations is effective. With dysmenorrhea, symptomatic agents are prescribed - analgesics and antispasmodics. Corresponding treatment of genital infections is carried out. For example, the use of acyclovir or valaciclovir in herpetic infection, the prevention of relapses of candidiasis makes it possible to lengthen the periods of remission and facilitate manifestations of vulwa and dysparenuria. In some cases, physiotherapeutic treatment, physiotherapy exercises, acupuncture are effective, especially when the causes of pain are associated with damage to the nerves, generic injuries, impaired pelvic bottom muscle tone. In an open pilot study, the characteristics of a special device were evaluated to identify and neutralize internal myofascial “trigger” points in patients suffering from urological diseases. The device provides a dosed compression in place of pain based on the indicators of the built -in algometer [13]. With confirmed myofascial syndrome, muscle relaxants, blockade of “trigger” points can be used. The use of tricyclic antidepressants and selective serotonin reversal inhibitors not only eliminates depressive disorders, but also effectively support the function of the antinociceptive system. Antidepressants are used in an individual dose, starting with a small one. Surgical methods of treatment. In case of detection of foci of endometriosis on the peritoneum during diagnostic laparoscopy, their ablation is carried out [16]. Laparoscopic ablation of the uterine -cross -nerves and presetacral neurectomy can be used to treat pelvic pain and dyspresion of unclear origin, but technically these interventions are complex and are of increased risk of bleeding [16,20]. American researchers have analyzed the experience of hysterectomy to patients suffering from endometriosis or chronic pelvic pain of indecent origin, refractory to other methods of treatment. In a large proportion of cases after surgery, the quality of life of women improves, manifestations of dyspareuria are reduced. But in 21–40% of women after a hysterectomy, pelvic pain remains, and in 5% it occurs for the first time. The chances of getting rid of pain below in the presence of initial depression [24]. Spasmolytics have an anesthetic effect in situations where the pain is caused by spasm or stretching of a hollow organ (in particular, intestines) or an inflammatory process, accompanied by reactive spasm of smooth muscles and blood flow disorders. Therefore, drugs of this class are very often used in the treatment of chronic pelvic pain. Spasmolytic is perhaps an integral component of the treatment of patients with SRK, regardless of the severity of its course. Given the laws of pain chronic, the prescription of antispasmodics should be resorted to already at the earliest stages of the disease in order to prevent a prolonged existence of a stream of pain impulse from the affected organ. From this point of view, it is necessary to choose the most safe and effective antispasmodics as possible, which has high selectivity and the power of action on the smooth muscle cells of the pelvic cavity - intestinal, urinary tract, genitals. Drotaverine hydrochloride (NO -Shpa® production of Sanofi - Aventis) is a selective inhibitor of phosphodesterase (FDE) type, which controls the contractile activity of the smooth muscle cells of the gastrointestinal tract and the genitourinary system. Inhibiting the IV type FDE is accompanied by an increase in the intracellular concentration of the TsAMF and a violation of the interaction of Aktin and myosin. Drotaverin also prevents the intake of calcium into the smooth muscle cage and reduces the activity of calcululo - muscle contraction catalyst. Since the type IV FDE is actively involved in the development of inflammation, its inhibition is accompanied by an anti -reducing and anti -inflammatory effect [12]. High, compared to papaverine, the selectivity of the drotaverine, reduces to a minimum the probability of affecting blood vessels and myocardium. There are no anticholinergic effects in drotaverin, which allows you to prescribe this drug for both elderly patients and children without significant fears. The efficiency of taking drotaverine hydrochloride (NO -SHPI®) at a dose of 80 mg 3 times/day. Within 4-8 weeks. In the treatment of pain in the IBS and its safety, it is proved in randomized double blind placebo -controlled studies, including 132 patients [27,30]. A pronounced antispasmodic, analgesic effect of drotaverine in urolithiasis and gynecological pathology (painful menstruation, ovulatory pain, inflammatory diseases) is well known and confirmed in a number of studies. In China, a multicenter open prospective study of the safety and effectiveness of the pills of drotaverin hydrochloride (NO -ShPA®) in the treatment of irritated colon syndrome was carried out. The study was attended by 217 patients aged 18–70 years, 52% - women. Patients are divided into four subgroups: SRK with a predominance of diarrhea, constipation, mixed course or non -specific type. A group of Patients of IBS with a predominance of diarrhea turned out to be the largest and included 45.6% of the participants. All patients were prescribed NO -Shpa® 80 mg 2 times/day. within 2 weeks. As the primary endpoint, the severity of abdominal pain was evaluated (on a 3 -point scale, where 0 points corresponded to the lack of pain), as secondary ones - a change in the frequency, form of stool, accompanying symptoms. After two weeks of treatment, the severity of pain has significantly decreased in all subgroups of patients; The average indicator in the general group is from 1.42 ± 0.42 to 0.66 ± 0.59 points (p <0.0001). The result of the action in relation to pain relief in the late 2nd week. The treatment was evaluated as excellent - from 28 to 36%, as good - from 26 to 36% of patients in different subgroups. The absence of the effect was reported from 15 to 31% of patients. Compared to the end of the 1st week. By the end of the 2nd week. Treatment of the number of patients who noted significant relief (“clinical cure”) has doubled. Drotaverine hydrochloride had a positive effect on the frequency and consistency of the stool. With a CRC with a predominance of diarrhea, the average frequency of defecation per day decreased from 2.8 ± 1.2 to 1.6 ± 0.8 (p <0.0001); In case of CRC with constipation - increased from 0.6 ± 0.4 to 0.8 ± 0.3 (p = 0.0004). The latter can be explained by a decrease in the spastic activity of the colon. The number of patients who experienced a sense of difficulty defecation, incomplete emptying of the rectum, and imperative urges decreased significantly. Serious undesirable phenomena during treatment were not recorded [6]. Pharmacoeconomic analysis of the use of antispasmodics for the relief of pain at the IPC, published by Afonin A.V., Depkina O.M., Kolbin A.S., Pchelintsev MV, Ivashkin V.T., showed that “Drotaverin has a faster dynamics To reduce the signs of spasm and the associated abdominal pain in comparison with the furniturerin and hyoscin with butyl bromide. But - shpa has distinct clinical and economic advantages in the pharmacoeconomic parameters “cost - efficiency” and “minimization of value” [1]. In recent years, much attention has been devoted to the problem of magnesium deficiency in the pathogenesis of diseases of the reproductive sphere in women, as well as emotional disorders and increased neuromuscular excitability. The effects that magnesium has in the body are closely associated with the action of pyridoxine (vitamin B6). These substances, acting synergistically, regulate the functions of many enzymes, prevent the accumulation of homocysteine and prevent thrombophilia. Magnesium is involved in maintaining a transmembrane potential, and also reduces thromboxan products, showing anti -inflammatory and anti -aggregate effects. In the modern food diet of Russians, the magnesium content often does not meet physiological needs. The causes of a poisonous deficiency of magnesium can be the purpose of diuretics, cyclosporine, cardiac glycosides, antibiotics (especially aminoglycosides), adrenectators, caffeine ,ogromin, theophillin, anti -tuberculosis, estrogen -containing contraceptives. Loss of magnesium occurs with diarrhea. In conditions of vitamin B6 deficiency and magnesium, pain sensitivity increases, probably partly due to a violation of the synthesis of neurotransmitters that regulate the nocication - GABA, serotonin, dopamine. With a deficiency of magnesium, pregnant women have pelvic pains associated with impaired blood flow and tone of the uterus, as well as increased muscle excitability. Organic magnesium salts (lactate, orotate, asparaginate, citrate, fag) are significantly better than inorganic, are absorbed during the oral administration. A combination with pyridoxin improves magnesium absorption. Magnesium lactate 470 mg with vitamin B6 5 mg in a tablet (Magnev6® drug) and citrate citrate 618.34 mg with vitamin B6 10 mg in a tablet (Magnev6 of Forte® production of Sanofi - Aventis) can be used in the complectional treatment of patients with chronic pelvic pelvic Pain against the background of states accompanied by a deficiency of magnesium.
Literature 1. Afonin A.V., Drapkina O.M., Kolbin A.S., Pchelintsev M.V., Ivashkin V.T. Clinical and economic analysis of antispasmodics for the relief of abdominal pain caused by intestinal spasm. //Russian Medical Journal - Vol. 18, No. 13, 2010. - With. 845–9. 2. Baranskaya E. K. Abdominal pain: clinical approach to the patient and treatment algorithm. The place of antispasmodic therapy in the treatment of abdominal pain // Farmateka. – 2005. – No. 14. 3. Ivashkin V.T., Shulpekova Yu.O. Nervous mechanisms of pain sensitivity // Russian Journal of Gastroenterology, Hepatology, Coloproctology. – 2002. – No. 4. – P. 16–21. 4. Website https://www.aids.about.com/od/otherconditions/a/rectal_pain_2.htm – June 20, 2011 5. Website https://www.bettermedicine.com/article/pelvic–pain – June 20, 2011 6. Website https://www.cjge–manuscriptcentral.com/Web/ViewAbstract.aspx?GaoHao=wcbx 10000241 – July 12, 2011 7. Website http//www. clinicaltrials.gov – July 1, 2011 8. Internet site https://www.medikforum.ru/news/medicine_news/5148–tazovaya–bol–oznachaet–migren.html – June 20, 2011 9. Website https://painconsortium.nih.gov/MAPPResearch.html - July 2, 2011 10. Website https://www.romecriteria.org – July 1, 2011 11. Website https://www.sirweb.org/patients/chronic–pelvic–pain – June 20, 2011 12. Pchelintsev M.V. Antispasmodics: from clinical pharmacology to pharmacotherapy // Attending physician - No. 7, 2008. - With. 3–6. 13. Anderson R, Wise D, Sawyer T, Nathanson BH. Safety and Effectiveness of an Internal Pelvic Myofascial Trigger Point Wand for Urologic Chronic Pelvic Pain Syndrome. Clin J Pain. 2011 May 25. 14. Apte G, Nelson P, Brismee JM et al. Chronic Female Pelvic Pain–Part 1: Clinical Pathoanatomy and Examination of the Pelvic Region. Pain Pract. 2011 May 26. doi: 10.1111/j.1533–2500.2011.00465.x. 15. Chang L. Brain responses to visceral and somatic stimuli in irritable bowel syndrome: a central nervous system disorder? // Gastroenterol Clin North Am. – 2005, June; 34(2):271–279. 16. Check JH. Chronic pelvic pain syndromes––traditional and novel therapies: part I surgical therapy. Clin Exp Obstet Gynecol. 2011;38(1):10–3. 17. Chronic pelvic pain. ACOG American Congress of Obstetricians and Gynecologists. Website https://www.acog.org/publications/patient_education/bp099.cfm. Accessed May 18, 2011 – June 20, 2011 18. Cicchiello LA, Hamper UM, Scoutt LM. Ultrasound evaluation of gynecologic causes of pelvic pain. Obstet Gynecol Clin North Am. 2011 Mar;38(1):85–114. 19. Driul L, Bertozzi S, Londero AP et al. Risk factors for chronic pelvic pain in a cohort of primipara and secondipara at one year after delivery: association of chronic pelvic pain with autoimmune pathologies. Minerva Ginecol. 2011 Apr;63(2):181–7. 20. El–Din Shawki H. The efficacy of laparoscopic uterosacral nerve ablation (LUNA) in the treatment of unexplained chronic pelvic pain: a randomized controlled trial. Gynecol Surg. 2011 Feb;8(1):31–39. 21. Fitzgerald CM, Neville CE, Mallinson T et al. Pelvic floor muscle examination in female chronic pelvic pain. J Reprod Med. 2011 Mar–Apr;56(3–4):117–22. 22. Glasgow R., Mulvihil S. Abdominal pain, including the acute abdomen. Sleisenger&Fordtrans's Gastroentestinal and Liver Disease. Philadelphia – London – Toronto – Montreal – Sydney – Tokyo, 2003; 1: 80–90. 23. Jacques E. Common Chronic Pelvic Pain Symptoms by Diagnosis Internet site https://www.pain.about.com/od/typesofchronicpain/a/CPP symptoms.htm. 24. Lamvu G. Role of hysterectomy in the treatment of chronic pelvic pain. Obstet Gynecol. 2011 May;117(5):1175–8. 25. Mayer E., Berman S., Suyenobu B. et al. Differences in brain responses to visceral pain between patients with irritable bowel syndrome and ulcerative colitis // Pain. – 2005, June; 115(3):398–409. 26. Meltzer–Brody S, Leserman J. Psychiatric Comorbidity in Women with Chronic Pelvic Pain. CNS Spectr. 2011 Feb 1. pii: Meltzer–Brody. 27. Misra SC, Pandey RM. Efficacy of drotaverine in irritable bowel syndrome: a double–blind, randomized, placebo–controlled clinical trial. Am J Gastroenterology 2000; 95: 2544 (Abs 455). 28. Musial F., Huser W., Langhorst J. et al. Psychophysiology of visceral pain in IBS and health // J. Psychosom. Res. – 2008, Jun; 64(6):589–597. 29. Neslihan Zehra Gultasl, Aydn Kurt, Ali Ipek, Mehmet Gumus, Kemal Rdvan Yazcoglu, Gulcin Dilmen, Ismet Tas The relation between pelvic varicose veins, chronic pelvic pain and lower extremity venous insufficiency in women. Diagn Interv Radiol 2006; 12:34–38. 30. Pap A, Hamvas J, Filiczky I, Burai M. Beneficial effect of drotaverine in irritable bowel syndrome. Gastroenterology 1998; 114: G3359 (AGA Abs). 31. Prendergast S. Myofascial pelvic pain syndrome Website https://www.examiner.com/pelvic-health-in-national/myofascial-pelvic-pain-syndrome - June 20, 2011. 32. Soleymani H, Ismail L, Currie I. GPs should be vigilant for pelvic inflammatory disease. Practitioner. 2011 Mar;255(1738):15–8. 33. Vulvodynia. ACOG American Congress of Obstetricians and Gynecologists. Website https://www.acog.org/publications/patient_education/bp127.cfm. Accessed May 18, 2011 – June 20, 2011 34. Warren JW, Morozov V, Howard FM. Could chronic pelvic pain be a functional somatic syndrome? Am J Obstet Gynecol. 2011 Apr 14.
Examination and physical examination
The physical examination may be supplemented by examination of the anus, as well as digital examination of the anal canal. Such a digital examination is painless. Not common, but levator spasm may occur. Doctors may prescribe sphincteromanometry if a corresponding disease is detected. However, it should be remembered that such a procedure often does not reveal pathological changes in tone.
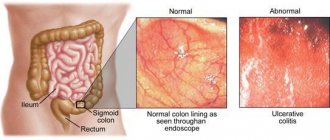
For the purpose of a detailed examination of the walls of the rectum, sigmoidoscopy can be performed. If necessary, the doctor will refer you to examine the upper parts of the colon, which is done through irrigoscopy or colonoscopy.
Treatment of adhesive capsulitis
Treatment of capsulitis does not require hospitalization and consists of medicinal and non-medicinal measures. The treatment regimen is drawn up individually, taking into account the characteristics of the patient’s body and the severity of the clinical picture.
The orthopedic regime involves eliminating loads on the damaged area. Immobilization must be dosed; prolonged immobilization of the joint is dangerous due to stiffness. For intense pain, a soft scarf bandage that is worn every day for 1-2 hours is perfect.
At the initial stages, therapeutic measures are aimed at eliminating pain with the help of nonsteroidal drugs (NSAIDs). The dosage and duration of therapy is determined by the attending physician. It is also recommended to carry out blockades with hormonal agents (glucocorticoids), which will not only alleviate the patient’s condition, but also reduce the pain phase. If necessary, the procedure is repeated after a 3-week break.
If a patient has diabetes mellitus, it is advisable to use intra-articular injections with preparations containing hyaluronic acid.
Important purpose:
- physical therapy and kinesiotherapy to restore motor activity of the joint and prevent the formation of contractures;
- massage and osteopathy sessions to increase the amount of synovium and restore its physiological properties;
- reflexology, restoring the natural structure of cartilage;
- laser treatment to eliminate fibrous and scar deformities in the joint;
- physiotherapy to provide a concomitant therapeutic effect.
If there are no results, there is a need for surgical intervention.
The benefits of chondroprotectors
Complete treatment of capsulitis is impossible without chondroprotectors - drugs based on chondroitin and glucosamine, which are involved in the formation of structural elements of the joint.
They are always included in the treatment regimen at any stage to restore the consistency and biochemical properties of the synovium. After completing a course of therapy with chondroprotectors, pain and swelling disappear, and motor activity is restored.
The most effective chondroprotectors include Artracam, which is available in powder form for the preparation of a solution for oral administration. The use of the drug is necessary in the following cases:
- Providing a rapid anti-inflammatory effect;
- Reducing pain;
- Getting rid of the feeling of stiffness;
- Activation of regenerative processes;
- Preventing the destruction of cartilage tissue.
With high efficiency, Artracam is considered a safe drug with virtually no contraindications or side effects.
Laboratory diagnostics
Laboratory blood tests will help determine signs of an ongoing inflammatory process. In order to finally exclude possible pathologies associated with the genitourinary system, a consultation with a gynecologist or urologist may be prescribed; an ultrasound of the bladder or an ultrasound of the pelvic organs may also be prescribed.
If there are no organic or functional abnormalities, but complaints of pain still remain, then the primary type of proctalgia is diagnosed. With the help of differential diagnosis, proctalgia can be distinguished from piriformis syndrome or coccydynia. Patients suffering from such pathologies may have previously undergone all kinds of treatment, so an analysis of the procedures that took place and the results obtained would be desirable.
Stages of shoulder capsulitis
There is a clinical classification of adhesive capsulitis depending on its stage. There are three of them. During development, the clinical picture changes gradually.
- Freezing stage (painful).
Its duration ranges from 3 months to one year. It is accompanied by severe inflammatory processes, leading to pain and further limitation of movements of the affected shoulder.
- Stiffness (rigidity).
Along with a decrease or complete disappearance of pain, there is an increase in stiffness of movement. It is impossible to carry out usual movements. The duration of this stage is from 4 months to a year.
- Resolution (defrost, defrost).
Over the next 12-42 months, the range of motion is restored and the pain syndrome completely disappears. 50% of patients recover completely. For the rest, motor activity remains limited to one degree or another, which does not prevent them from leading a full life.
Each phase and the disease as a whole does not have a precisely defined duration. This parameter is influenced by the individual characteristics of the body, concomitant pathologies, and the timeliness of diagnostic and therapeutic measures. It has been noticed that the longer the first stage lasts, the longer the next two. In the absence of therapy, recovery occurs in 1.5-4 years.
Basic principles of treatment of proctalgia
If proctalgia is diagnosed, the patient is prescribed the following treatment methods to relieve pain attacks:
- physiotherapy (infrared irradiation via intrarectal laser, mud therapy, diathermy, electrical stimulation);
- so-called novocaine blockades (usually perisacral, retrorectal and epidural-sacral);
- massage of the coccygeal muscle, massage of the elevators of the anus in case of pronounced spasm;
- microenemas using novocaine or sea buckthorn oil;
- sedatives (sleeping pills, sedatives and tranquilizers).
The course of treatment usually begins with sanitation of the rectum with antibacterial components, which are often used as a measure for the treatment of latent proctosigmoiditis. Since primary proctalgia is often associated with the psycho-emotional state of the patient, the main goal of therapy is to create a favorable psychological background and avoid stress and tension. Various psychotherapeutic relaxation methods are often used. It happens that a consultation with a psychologist is required.
In addition to strictly following all treatment instructions, you must adhere to the prescribed diet, which helps normalize the digestion process.
The secondary type of proctalgia goes away when the main disease causing this disease is cured.
Complications of capsulitis
Inflammatory processes in the joint capsule are accompanied by a pronounced clinical picture, which causes temporary disability. At the same time, the course of the disease is very favorable - in most cases there are no complications. In addition to accurate diagnostic measures and adequate treatment, it is important that the patient is confident in recovery and accurately fulfills all the doctor’s requirements.
In severe cases, with untimely treatment and excessively long immobilization, the functions of the joint are not fully restored, and contracture (stiffness) develops. The addition of plexitis, leading to damage to nerve fibers, and the onset of total muscular dystrophy cannot be ruled out. Subsequently, pathological processes begin to occur in the elbow and wrist joints, which is dangerous for disability. There is a need for surgical intervention and endoprosthetics.
Constant pain, the inability to perform basic actions and the prospect of fighting the disease for several years is a difficult, psychologically traumatic task for many.
Prognosis and prevention
With capsulitis, complete recovery and restoration of motor activity is possible only with timely diagnosis and treatment.
The only preventive method is a course of Artracam or other chondroprotectors. They strengthen joint structures and prevent the development of inflammatory processes.
Adhesive capsulitis is characterized by the absence of specific symptoms. Therefore, any negative sensations in the shoulder joint are a reason for an immediate visit to the doctor.
Causes
The immediate cause of the pain that occurs during proctalgia is spasmodic contractions of the fibers of the muscular lining of the rectum, which causes excessive irritation of the nerve endings - a pain syndrome is formed.
Often these muscle spasms can:
- have a neurological nature;
- occur due to severe physical stress;
- become a consequence of psycho-emotional experiences.
Proctalgia of a neurological nature most often occurs against the background of:
- diseases of the lower gastrointestinal tract;
- pathologies of the pelvic organs.
Diseases of the digestive tract, in which proctalgia of a neurological nature can develop, are:
mesadenitis is an inflammatory process in the lymph nodes of the mesentery (a thin connective tissue film that attaches the intestine to the inner surface of the abdominal wall and in which there are lymph nodes, vessels feeding the intestine, as well as nerve branches responsible for its nervous support);- acute and chronic sigmoiditis - inflammatory damage to the mucous membrane of the sigmoid colon;
- acute and chronic proctosigmoiditis - combined inflammation of the sigmoid mucosa and the initial part of the rectum;
- acute and chronic paraproctitis - inflammatory damage to the tissues around the rectum;
- caudal teratoma - a tumor in the rectal tissue, which originated during the intrauterine formation of the fetus and which contains the rudiments of embryonic tissue;
- Crohn's disease - the formation of specific granulocyte tubercles in the intestine;
- nonspecific ulcerative colitis is an inflammatory lesion of the colon mucosa with the formation of ulcerations in it.
Pathologies of the pelvic organs, in which proctalgia of a neurological nature can develop, are often:
- endometriosis in women is a disease in which endometrial cells (the inner layer of the uterus) develop outside the uterus;
- prostate adenoma in men is a benign tumor of the prostate;
- Prostatitis in men is an inflammatory lesion of the prostate.
Proctalgia due to severe physical strain can occur with:
- even short-term lifting and carrying heavy objects;
- physical work for a long time without rest.
In fact, any person who is capable of succumbing to psycho-emotional influence is not immune from proctalgia, since it can arise against the background of stressful circumstances. They may be:
death of a loved one;- stressful work environment;
- professional responsibility associated with risks of one’s own (miners, test pilots, sappers) and those of other people (dispatchers of transport hubs, rescuers, doctors, and so on);
- conflict situations in the family;
- failures related to personal life (divorce, betrayal of a loved one, futile long-term attempts to arrange a personal life, and so on);
- social upheaval due to material factors (lack of means of subsistence, robbery, debts, outstanding loan);
- psycho-emotional stress associated with problems of loved ones (their stress at work, illness, major material losses);
- serious conflicts and problems in society (threats, blackmail, administrative and criminal liability)
and many others.
Proctalgia is most often preceded by psycho-emotional experiences with a negative connotation. But the influence of strong positive emotions cannot be ruled out, due to which excessive excitation of the brain centers develops, which causes a failure in the innervation (nervous supply) of the rectum. This:
- victory in high-ranking competitions;
- admission to a prestigious educational institution;
- significant promotion at work;
- major material acquisition;
- upcoming wedding.
and many others.
Only an experienced doctor who carefully ascertains the anamnesis (history) of the pathology can establish that proctalgia has developed against the background of excessive positive emotions - in a state of joyful euphoria, patients are not able to attach significance to it and may not mention it, guided by the stereotype that only negative stress situations can “undermine” health.
Proctalgia can also occur due to:
- constant irritation of the rectal wall from the inside;
- banal pressure from neighboring organs and tissues.
Regular irritation of the rectal wall from the inside with subsequent development of pain can be observed:
- after performing some medical procedures;
- due to specific sexual preferences.
Manipulations that irritate the wall of the rectum with the possible occurrence of proctalgia can be:
- diagnostic;
- medicinal.
Such diagnostic procedures include:
- digital examination of the rectum (especially often in men for the purpose of diagnosing diseases of the prostatic gland);
- rectoscopy - examination of the rectum using a rectal (rectal) mirror;
- sigmoidoscopy - examination of the rectum and terminal parts of the sigmoid colon using a sigmoidoscope (a type of endoscope - a medical device with a built-in optical system and illumination);
- colonoscopy - examination of all parts of the large intestine using a colonoscope (a type of endoscope);
- irrigoscopy is an X-ray examination of the large intestine with the preliminary introduction of a contrast agent into it through the rectum.
Therapeutic manipulations involving the rectum, which can lead to proctalgia, are:
- administration of cleansing or therapeutic microenemas;
- placing rectal suppositories (rectal suppositories) made at home, which is why their size may not correspond to the size of the rectal lumen;
- massage of the prostate gland in men through the rectum.
Due to specific sexual preferences, irritation of the rectal wall with the development of proctalgia can develop:
- in homosexuals, when there is a discrepancy between the size of the rectum of one sexual partner and the penis of the other;
- due to the rough impact on the rectum with devices for satisfaction and self-gratification (so-called sex toys) - especially random, inappropriate objects.
Pressure on the rectum from neighboring organs and tissues with the subsequent occurrence of pain can be observed with such pathologies as:
- any tumors of the uterus in women that can reach large sizes - fibroids (from muscle elements), fibroids (from connective tissue), fibroids and others;
- adhesive disease of the pelvis - the development of a large number of connective tissue cords that have formed as a result of any previous pathology (often inflammatory or purulent-inflammatory) or after surgery on the pelvic organs;
- a foreign body - for example, a shell fragment that entered soft tissue during combat operations, was encapsulated and remained in the rectal area for a long time, without provoking a purulent-inflammatory process, but putting pressure on the wall of the rectum
and so on.