The indirect toxic effect of antibiotics on the liver and biliary system is known through toxic products of the transformation of antibiotics in the body (metabolites). Some metabolites bind to liver substances (glutathione, etc.) and reduce the toxicity of antibiotic breakdown products and improve their excretion from the liver with bile. In this case, the bile may become viscous, and stagnation of bile in the gallbladder may be observed with the formation of suspension and flakes (i.e., bile sludge), which are risk factors and early signs of stone formation in the gallbladder.
Patient K., 40 years old, consulted a gastroenterologist about periodic aching pain in the right hypochondrium, heaviness after eating, and rarely bitterness in the mouth. The patient has been suffering from these sensations for several years; these sensations are provoked by long breaks in eating. Heredity is not burdened.
Effect of antibiotics. Objectively
- satisfactory condition,
- sclera and visible mucous membranes of normal color,
- the abdomen participates in breathing, is painless on palpation in all parts, gall bladder symptoms are negative,
- liver at the edge of the costal arch.
The patient is suspected of having a violation of the contractile function of the gallbladder (dyskinesia). To clarify what dyskinesia is, an ultrasound examination of gallbladder function (cholecystokinetic test) with a test breakfast (sorbitol) was prescribed.
Fungal diseases
Antibiotics can lead to dysbiosis and contribute to the development of fungal infections. 3 It turns out that you can treat one disease, and in the “load” get another.
Fungi can affect the mucous membranes of the gastrointestinal tract, as well as the skin and genitourinary system. If the fungal disease is generalized, that is, has spread throughout the body, then there is a risk of damage to internal organs. 4
When a fungal disease develops, other infections are often associated, which can lead to a sharp decrease in immunity, ulcers, even baldness and other unpleasant and dangerous consequences. To avoid such complications, doctors sometimes prescribe antibiotics along with antifungal drugs, which increases the burden on the body.
Ultrasound results
Ultrasound of the gallbladder dated January 12, 2019: the shape is irregular due to the presence of kinks in the projection of the neck and body, dimensions 63*25*25 mm. The walls are not thickened, uniform in density, single-layer. The hepatic choledochus is 3.4 mm (the norm is 6 mm), it is not traceable throughout its entire length, it is passable, the contents are heterogeneous, the walls are moderately compacted. The contours are smooth and clear. The cavity is heterogeneous due to hypoechoic fine suspension. The initial volume of the gallbladder is 18.81 cubic cm. After giving a trial breakfast at 30 minutes, the gallbladder decreased by 51%.
According to ultrasound and clinical data, it was possible to conclude that the patient has a congenital deformation of the gallbladder in the neck and body with signs of bile stagnation - dyskinesia of the hypotonic type ("flaccid" gallbladder) with the presence of hypoechoic fine bile (sludge).
Diet food
Knowing why the stomach may hurt after a course of antibiotics, it is necessary to prevent the development of dysbiosis. Following the principles of dietary nutrition can help with this. The duration of the diet is at least three calendar months.
From the daily menu you will need to completely exclude foods that trigger fermentation processes. These include black bread, cabbage, granulated sugar, fresh milk, grapes. At night, you should definitely drink a fermented milk product that contains bifidobacteria, for example, kefir.
To relieve cramps felt in the lower abdomen and painful syndrome, chamomile decoction helps well. For this purpose, it is recommended to drink ½ glass up to 5 times a day. It is worth noting that the drink does not affect the absorption of antibiotics.
If the patient is bothered by diarrhea, then rice water will help stabilize the stool. It has enveloping properties and helps relieve irritation from the gastric mucosa.
During the treatment of dysbiosis, a person is recommended to adhere to a certain diet
To eliminate intestinal spasms, you can brew ginger tea. You should drink ½ glass 3 times a day. In addition, it is good for nausea.
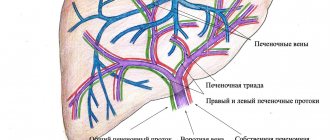
Force Majeure. The effect of antibiotics on the biliary system
The study was not carried out in April, because The patient had an attack of acute appendicitis, surgery, then a two-week course of antibiotics.
After 2 months, pain in the right hypochondrium, belching, bitterness in the mouth, and intestinal discomfort began again. And only in September the patient decided to do an ultrasound of the gallbladder and consult a gastroenterologist.
On ultrasound, the cavity of the gallbladder is heterogeneous due to the presence of hypoechoic fine suspension and putty-like bile, occupying about 2/3 of the lumen of the gallbladder. The maximum contraction of the gallbladder was 25.1%.
The patient shows pronounced negative dynamics in the gallbladder, most likely associated with the course of antibiotics: the contractile function of the gallbladder has significantly worsened, the quality of bile has changed, and sludge has formed, occupying 2/3 of the lumen of the gallbladder.
Gastritis after eradication of Helicobacter pylori - simple traces or serious consequences?
The evolution of the relationship between Helicobacter pylori (HP) infection and humanity goes back more than one millennium [1]. During this period, mechanisms of interaction between the infection and the host were formed [2], allowing the bacterium to modulate the level of acid production, maintaining inflammation of the gastric mucosa. How important is it for the clinician to correctly interpret evidence of inflammation in the gastric mucosa associated with HP? On the one hand, the presence and severity of the inflammatory infiltrate does not determine whether the patient has clinical symptoms of dyspepsia that arise as a result of disorders of gastric secretion, gastroduodenal motility, visceral sensitivity, often caused by neuropsychic factors. It is no coincidence that none of the three modern classifications of chronic gastritis (Sydney, 1990; Houston, 1994; OLGA classification, 2008) contains a section regarding the assessment of clinical manifestations. Why then is the clinician’s attention focused on the data from the pathologist’s report? Why did the participation of clinicians become necessary in the process of creating a classification of chronic gastritis? The answer lies in the objectives of the classification system - to assess the condition of the mucous membrane, characterize the inflammatory process for prognosis, and, based on a standardized approach, enable the clinician to personalize the monitoring program for a patient with chronic gastritis [3].
Today we can say with confidence that HP, as one of the representatives of “slow” infections, is neither a new threat nor an old friend, and eradication of the bacterium is considered as a part of the treatment protocol for patients with HP-associated pathology [4, 5]. However, specific chronic inflammation of the gastric mucosa does not disappear with the elimination of the pathogen [6].
The persistence of the inflammatory infiltrate during the elimination of the infection is not just a biological phenomenon. Preservation of inflammation also means continued risk of damage to the gastric mucosa, which is of practical importance. Thus, infiltration of the mucous membrane by neutrophilic leukocytes is accompanied by the production of reactive oxygen species (“oxidative stress”), which leads to direct and cytokine-mediated damage to the mucosal epithelium and serves as a risk factor for the formation of ulcers and erosions. On the other hand, long-term exposure to reactive oxygen species leads to irreversible DNA damage that accumulates over time and creates a “launching pad” for the development of stomach cancer. Normally, neutrophil infiltration disappears only 1 month after successful eradication of Helicobacter pylori infection. Somewhat later, by activating apoptosis, the number of lymphocytes and plasma cells decreases. The last to undergo reduction are the lymphoid follicles of the lamina propria: the glands, pushed apart by the inflammatory infiltrate, take their original place, and the phenomenon of “indefinite atrophy” disappears. These processes, developing asynchronously, also differ in the different rates of inflammation reduction.
In a prospective cohort study that included 181 patients with HP-associated gastritis and dyspepsia syndrome, the observation period with clinical and biopsy control over time was 1 year [7]. Already a month after eradication of HP, a decrease was noted, primarily in the activity of gastritis, with a more restrained rate of reduction of mononuclear inflammatory infiltration. It was revealed that the severity of signs of chronic inflammation in the gastric mucosa decreased more slowly in patients with atrophic gastritis, which is consistent with the data of other researchers. Subsequently, along with regression of the inflammatory infiltrate, there was a significant decrease in the proliferation index and apoptosis index in the epithelial cells of the gastric mucosa. From a clinical point of view, eliminating the infection, helping to normalize the rate of cellular renewal, helps stop the progression of precancerous changes in the gastric mucosa, and is a measure for the prevention of stomach cancer.
Characteristic of the one-year post-eradication period was the “disappearance” of the phenomenon of vague atrophy, which was associated with a decrease in the density of inflammatory infiltration and the departure of patients into the category with or without true atrophy. Probably, the results of a number of studies, in which some patients showed the disappearance of atrophy of the gastric mucosa within 1–2 years after eradication of the infection, are due precisely to the fact that patients with the phenomenon of uncertain atrophy were not excluded from observation. At the same time, there are also data from studies with a longer observation period (more than 7–10 years), which are encouraging regarding some regression of the degree of atrophy of the gastric mucosa with the elimination of HP.
Analysis of the results of histological examination of gastrobiopsy specimens 1 year after eradication of the infection made it possible to identify three groups of patients:
- restoration of the structure of the gastric mucosa (complete reduction of inflammatory changes in the gastric mucosa, the content of interepithelial lymphocytes (1–5 per 100 epithelial cells) corresponds to the norm) was noted in 24 (13.2%) treated patients;
- partial regression of inflammatory changes during histological examination of gastrobiopsy specimens was detected in 106 (58.6%) patients;
- preservation of the severity of inflammatory changes in the gastric mucosa even 1 year after elimination of the pathogen was recorded in 51 (28.2%) patients.
In the absence of HP, the main factor determining the rate of cellular renewal in the gastric mucosa becomes the mononuclear inflammatory infiltrate of the lamina propria of the mucous membrane (Fig. 1), which implements the apoptosis program through the FasL-FasR system of interepithelial CD8 lymphocytes and mucocytes [8]. When analyzing immunohistochemical indicators of cellular renewal of epithelial cells of the gastric mucosa in patients with various options for the course of the post-eradication period (restoration of the structure of the mucous membrane, reduction in the severity of inflammation, persistence of the inflammatory infiltrate), it was found that the indicators of patients of the first and third groups have statistically significant differences, which is consistent with the obtained data on the existence of a direct correlation between the apoptosis index, the epithelial cell proliferation index and the severity of mononuclear infiltration of the lamina propria of the gastric mucosa.
| Rice. 1. Persistence of mononuclear inflammatory infiltrate in the post-eradication period is a factor that determines the rate of cellular renewal of epithelial cells of the gastric mucosa |
It should be recognized that the course of the post-eradication period of chronic gastritis is heterogeneous and is determined by the peculiarities of intercellular interactions of the inflammatory infiltrate and the epithelium of the gastric mucosa, which developed at the stage of formation of the “infector-host” system.
Successfully carried out anti-Helicobacter therapy leads to the pathomorphism of chronic HP-associated gastritis, which requires indicating the fact of eradication of the pathogen when formulating the diagnosis. This strategy does not conflict with the generally accepted ICD-10, but allows us to expand our understanding of HP-associated chronic gastritis.
Of course, eradication carries the potential to normalize cellular renewal, which, in fact, is a measure of cancer prevention. At the same time, inflammatory infiltration of the gastric mucosa that persists for a certain time is associated with the possibility of cell damage [9], including due to the increased activity of lipid peroxidation enzymes - cyclooxygenase-2 (COX-2) and inducible nitric oxide synthase (INOS) - proteins involved in carcinogenesis within a year after eradication has taken place [10].
Thus, for patients with ex-Helicobacter gastritis, it is necessary to include in the supervision program courses of muco/cytoprotective therapy to protect the cells of the gastric mucosa from the damaging effects of inflammatory products in order to prevent the progression of gastritis [11].
The group of muco/cytoprotectors today includes several drugs (table), among which the therapeutic capabilities of bismuth tripotassium dicitrate (De-Nol) should be highlighted. Numerous studies have shown that bismuth tripotassium dicitrate forms a protective layer on the affected areas of the mucous membrane, protecting it from the effects of aggressive factors, stimulates the secretion of mucus and bicarbonate, inhibits the activity of pepsin, protects epithelial growth factors from decay, promoting the regeneration of epithelial cells, improves microcirculation, stimulates the secretion of gastroprotective prostaglandins.
The experience accumulated over decades of eradication therapy and follow-up of patients with various stages of gastritis in the post-eradication period has made it possible to identify another problem. In conditions of already formed atrophy of the gastric mucosa, elimination of the infection does not solve the problem of contamination of the gastric mucosa with non-NR microorganisms [12], including Helicobacter spp. [13], Proteus mirabilis, Citrobacter freundii, Klebsiella pneumoniae, Enterobacter cloacae, Staphylococcus aureus, with an additional stimulus for the persistence of the inflammatory infiltrate, activation of lipid peroxidation processes and the production of nitrosamines by bacteria, which have pro-carcinogenic potential [14]. A similar picture can form during the natural course of gastritis, known to the clinician as the “P. Correa cascade” (Fig. 2).
| Rice. 2. P. Correa cascade (cited from [15]) |
What should a clinician do in this situation? Choose only observational tactics? Conduct repeated courses of antibacterial therapy? Probably, conducting large prospective multicenter studies will make it possible in the future to find an answer to this question, to determine the feasibility, components and timing of such therapy, but what are our capabilities now? We believe that in such a situation, the clinician should consider including the patient in the patient supervision program, along with clinical and biopsy control, and conducting courses of therapy with bismuth preparations. Firstly, not being an antibiotic, bismuth tripotassium dicitrate suppresses the activity of bacterial flora without the risk of developing resistance, which has been successfully used for many years in standard eradication therapy. Secondly, in conditions of persistent inflammation, the properties of De-Nol that affect the activity of the inflammatory process become necessary, namely a decrease in the content of pro-inflammatory cytokines and the presence of an antioxidant effect. It should be noted that these properties of the drug are successfully used in the treatment of other diseases, including intestines. Thirdly, patients with atrophic gastritis especially need mucocytoprotective therapy with increased production of mucus, prostaglandins, and improved microcirculation in the gastric mucosa.
Thus, the analysis of literature data and the results of our own research allow us to speak about the persistence of the inflammatory infiltrate after the elimination of HP, while the course of gastritis in the post-eradication period is determined primarily by the formed inflammation even at the stage of infection of the host by HP. The persistence of the inflammatory infiltrate requires active supervision of the patient to reduce changes in the gastric mucosa as completely and quickly as possible and prevent the progression of gastritis. For effective and safe treatment of patients in the post-eradication period, bismuth preparations (De-Nol) should be considered as the drugs of choice, especially with atrophy of the gastric mucosa and a high degree of gastritis.
Literature
- Amieva MR Host-bacterial interactions in Helicobacter pylori infection/MR Amieva, EM El-Omar // Gastroenterology. 2008. Vol. 134, No. 1. P. 306–323.
- Ricci V., Romano M., Boquet P. Molecular cross-talk between Helicobacter pylori and human gastric mucosa. World J Gastroenterol 2011; 17 (11): 1383–1399.
- Dai YC, Tang ZP, Zhang YL How to assess the severity of atrophic gastritis. World J Gastroenterol 2011; 17 (13): 1690–1693.
- Malfertheiner P. Guidelines for the Management of Helicobacter pylori Infection Summary of the Maastricht-3 2005 Consensus Report / P. Malfertheiner, F. Megraud, C. O'Morain // Business briefing: European gastroenterology review. 2005. R. 59–60.
- Osipenko, M. F. Program for local therapists “effective eradication” / M. F. Osipenko et al. // Gastroenterology of St. Petersburg. 2008. No. 2–3. S. M91.
- Kononov A.V. Inflammation as the basis of Helicobacter pylori-associated diseases: from gastritis to stomach cancer / A.V. Kononov // Proceedings of the II Congress of the Russian Society of Pathologists. M., 2006. pp. 229–231.
- Livzan M. A. The course of chronic gastritis associated with Helicobacter pylori in the post-eradication period / M. A. Livzan, A. V. Kononov, S. I. Mozgovoy // Experimental and clinical pharmacology. 2007. No. 5. pp. 116–123.
- Expression of HLA-DR, costimulatory molecules B7–1, B7–2, intercellular adhesion molecule-1 (ICAM-1) and Fas ligand (FasL) on gastric epithelial cells in Helicobacter pylori gastritis; influence of H. pylori eradication / A. Archimandritis [et al.] // Clin. Exp. Immunol. 2000. Vol. 119. P. 464–471.
- Yoshimura T., Shimoyama T., Tanaka M., Sasaki Y., Fukuda S., Munakata A. Gastric mucosal inflammation and epithelial cell turnover are associated with gastric cancer in patients with Helicobacter pylori infection. J Clin Pathol 2000; 53:532–536.
- Sung Soo Kim, Young Jick Sung, Min Kyoung Park et al. The Change of Cyclooxygenase-2 and Inducible Nitric Oxide Synthase in the Gastric Mucosa One Year after Eradication of Helicobacter pylori Korean J Gastroenterol 2008; 52:286–292.
- Tulassay Z., Herszenyi L. Gastric mucosal defense and cytoprotection. Best Pract Res Clin Gastroenterol. 2010 Apr; 24 (2): 99–108.
- Takako Osaki, Katsuhiro Mabe, Tomoko Hanawa and Shigeru Kamiya. Urease-positive bacteria in the stomach induce a false-positive reaction in a urea breath test for diagnosis of Helicobacter pylori infection Journal of Medical Microbiology (2008), 57, 814–819.
- Cinthia G. Goldman and Hazel M. Mitchell. Helicobacter spp. other than Helicobacter pylori 2010 Blackwell Publishing Ltd, Helicobacter 15(Suppl. 1): 69–75.
- Correa P. A human model of gastric carcinogenesis. Cancer Res 1988; 48:3554–3560.
- Correa P. Chronic gastritis as a cancer precursor. Scand J Gastroenterol Suppl. 1984; 104:131–6.
M. A. Livzan, Doctor of Medical Sciences S. I. Mozgovoy, Doctor of Medical Sciences A. V. Kononov, Doctor of Medical Sciences, Professor
State Educational Institution of Higher Professional Education "Omsk State Medical Academy of the Ministry of Health and Social Development of Russia", Omsk
Contact information for authors for correspondence
Correction of treatment
Treatment was prescribed for a longer period of 3-4 months, humane tubes, ursodeoxycholic acid preparations, choleretic drugs, a diet, and therapeutic nutrition were prescribed.
Patients who already have gallbladder dyskinesia and bile sludge should protect the liver and biliary tract during antibiotic treatment and continue individual treatment based on the duration of treatment and the set of drugs after the end of the course.
The drugs Heptral, Ursosan and its analogues, Hofitol and other choleretic drugs have proven themselves well. If, after taking antibiotics, complaints of pain in the right hypochondrium or bitterness in the mouth appear, it is necessary to conduct an examination of the biliary system and carry out the required amount of treatment.
How to minimize the risk of developing dysbiosis
If it is not possible to avoid long-term use of antibiotics, then efforts must be made to minimize the negative impact of drugs on the intestinal microflora. To avoid the development of pain, you must adhere to the following rules:
Pain in the abdomen and stomach
- It is highly undesirable to take the drug on an empty stomach. You need to eat something about 20 minutes beforehand.
- During the entire period of taking antibiotics, it is necessary to review the diet. The menu should contain products that have enveloping properties. These are slimy porridges, pureed purees, jelly, and pureed soups. It is necessary to completely eliminate spicy foods, marinades, coffee and strong tea, and alcohol. These products, in combination with antibiotics, can cause significant harm to the gastric mucosa.
- If you have a choice, it is advisable to replace the tablet format with injections. In this case, the medicine will enter directly into the bloodstream, bypassing the stomach.
- To take the medicine, you should use only clean water. The minimum volume is ½ cup.
- Simultaneously with the start of a course of antibiotics (especially for a child), it is necessary to start taking probiotics - agents that restore the normal balance of intestinal microflora. “I take antibiotics and definitely take probiotics.”
If the body gives too strong a negative reaction to treatment with drugs from the antibiotic category, then it is advisable to replace the prescribed medication. The selection of an analogue should be carried out by the attending doctor.
Allergy
Of course, one of the most common side effects of antibiotics is allergies. 5 In this case, an itchy rash and swelling may appear on the skin. In severe forms, the eyelids, lips and tongue become swollen, there is difficulty swallowing and speaking, severe weakness appears, heaviness is felt behind the sternum and shortness of breath even at rest. This is how anaphylactic shock manifests itself - an acute pathological condition that is life-threatening. In case of rapid development of allergy symptoms, emergency medical care and resuscitation measures are necessary.
It is also necessary to take into account the fact that antibiotics can enter our body along with some food products - for example, meat may contain penicillins. This means that almost every person has a risk of developing allergies when taking antibacterial drugs. 6 This once again indicates the need for medical supervision when taking antibiotics.
What do you need to remember?
It is necessary to be very careful when choosing medications and, if possible, choose those that have the greatest therapeutic and least toxic effects. Therefore, you should not take antibiotics if there is no indication for this and these drugs are not recommended to you by your doctor.
For ARVI and sore throat, in most cases it is advisable to choose symptomatic therapy, which helps to get rid of unpleasant symptoms, regardless of the cause of their occurrence. The drug Strepsils® Intensive, lozenges [honey-lemon] has a local analgesic and anti-inflammatory effect on the mucous membrane of the mouth and throat: reduces swelling, difficulty swallowing, pain and irritation in the throat.9
The drug helps eliminate sore throat, regardless of the cause of its occurrence (be it viruses, bacteria or fungi).