Inflammatory diseases of the gastrointestinal tract are the most common reason for visiting a gastroenterologist. Such pathologies significantly reduce the quality of life and force a person to limit their diet. In addition, diseases of the digestive system always progress into more serious disorders.
To prevent gastritis from becoming chronic, it is necessary to begin therapy from the appearance of the first symptoms. This article will be useful for those who want to learn about inflammatory diseases of the stomach and how to cure chronic gastritis.
What is chronic gastritis?
Chronic gastritis can occur against the background of autoimmune pathology.
The term "gastritis" was first used in 1730 by the German physician Georg Ernst Stahl to describe inflammation of the stomach lining.
In the last century, many considered gastritis to be a curious histological finding, but not a disease. Everything changed with the discovery of an infectious agent, the bacterium Helicobacter pylori.
The organism was found in inflamed stomach tissue by Robin Warren and Barry Marshall in 1983, leading to a precise definition of the disease and the introduction of designations for the different types of gastritis.
Chronic gastritis is classified based on the cause of its occurrence (Helicobacter, bile reflux from the duodenum, the use of non-steroidal anti-inflammatory drugs, autoimmune pathology, allergies) and the histological picture, indicating the probable clinical mechanism of the development of the pathology. Other classifications of gastritis are based on the endoscopic picture of the gastric mucosa.
It is important to distinguish between gastritis and other gastric diseases in which processes of cell damage and regeneration are observed against the background of minimal inflammation. In order to distinguish between these pathologies, gastroenterologists use differential diagnostic methods.
Chemical or reactive gastritis occurs when the gastric mucosa is damaged as a result of reflux of bile and pancreatic juice into the stomach, although sometimes the pathology is associated with taking medications such as painkillers, acetylsalicylic acid and chemotherapy.
Gastritis or functional dyspepsia?
The term “gastritis” is usually used to refer to various inflammatory and degenerative changes in the gastric mucosa. But in fact, the disease itself is quite rare and can only be diagnosed using a biopsy during a gastroscopy procedure.
Often what is called gastritis is functional dyspepsia (a set of disorders of the digestive system). The term “gastritis” is also mistakenly used to mean gastroesophageal reflux disease (GERD) or irritable bowel syndrome (IBS).
Currently, the diagnosis of “gastritis” is usually made in the presence of morphological signs discovered after undergoing a series of medical examinations, in particular, after laboratory identification of the main causative agent of the disease - the bacterium Helicobacter pylori (H. Pilory), histological studies and FGDS.
What is the mechanism of disease development?
Helicobacter pylori infection is the main cause of chronic gastritis.
Helicobacter pylori infection is the main cause of chronic gastritis, gastric ulcer, adenocarcinoma and primary gastric lymphoma.
Helicobacter is a spiral gram-negative bacterium that has the ability to colonize and infect gastric tissue.
Bacteria of this type survive in the mucous membrane of the organ, despite the aggressive environment of gastric juice. The result is widespread inflammation of cells and tissues.
The presence of H-pylori is associated with tissue damage and histological features of acute and chronic gastritis. The human body releases lymphocytes in response to bacterial invasion. Lymphocytes are densely distributed in the mucous membrane, which makes it possible to accurately identify the disease during laboratory testing.
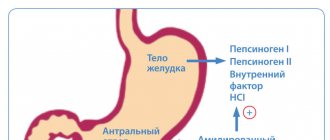
The inflammatory process leads to functional changes in the stomach. When the damage reaches the main part of the organ, the functioning of the parietal cells is disrupted, which leads to a decrease in the secretion of gastric juice. The progression of gastritis leads to the loss of parietal cells, and the decrease in acidity becomes permanent.
Inflammation of the initial part of the stomach alters the interaction of important regulatory factors, gastrin and somatostatin. Patients with such diseases have abnormal secretions of gastrin, a hormone responsible for stimulating digestion. Helicobacter chronic gastritis progresses in accordance with the following two forms of pathology:
- Antral gastritis. It is characterized by inflammation mainly of the initial part of the organ. Typically, this picture is observed in patients with peptic ulcer disease.
- Multifactorial atrophic gastritis. It is characterized by widespread inflammation and is also observed in individuals with gastric ulcers.
- Although the role of Helicobacter in the development of peptic ulcer disease is well proven, the effect of infection in non-ulcer cases is very controversial.
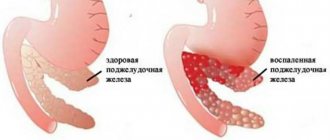
Treatment of atrophic gastritis
There is no single approach to the treatment of atrophic gastritis due to the diversity of its microstructural manifestations, as well as the meager clinical symptoms. Degenerated cells cannot be turned back into glandular cells.
Chronic atrophic gastritis can be cured by stopping the development of pathological processes. Treatment should be based on careful investigation, as different cases require different therapeutic approaches.
The traditional scheme includes:
- Helicobacter eradication. These methods are constantly being improved. The objectives of eradication are: suppressing bacteria, preventing them from developing resistance to antibiotics; using PPIs to improve well-being; reducing the number of medications. Preference is given to a three- or four-component eradication scheme.
- The effect on autoimmune processes in atrophic gastritis has not yet been fully studied.
- Pathogenetic therapy uses a whole group of drugs. This includes digestive aids (enzymes). If there is a deficiency of vitamin B12, vitamin preparations are used in the form of injections. In some cases, the use of mineral waters has high therapeutic activity. Preparations with plantain juice help reduce inflammation.
- To protect the mucous membrane in atrophic gastritis, aluminum and bismuth preparations (Vicalin, Kaolin, Rotor, Vikair) are recommended.
- Cisapride and Domperidone help regulate motor function.
All of the listed drugs are prescribed only in the active phase of inflammation with mucosal atrophy.
Diagnosis of chronic gastritis
Chronic gastritis causes discomfort in the stomach.
Physical examination of the patient makes a rather minor contribution to the diagnosis and treatment of chronic gastritis, however, there are also specific manifestations of the disease.
With uncomplicated atrophic gastritis associated with Helicobacter, clinical data say almost nothing.
Sometimes it is possible to detect tension in the epigastric region, signs of a gastric ulcer and occult blood in the patient's stool. Rarely, breathing problems and signs of flatulence associated with bacterial overgrowth occur.
How to cure chronic gastritis?
Treatment of chronic gastritis should be aimed at a specific etiological factor if the cause of the disease is known. For example, bacterial invasion requires antibiotics. If gastritis has developed into a systemic disease of the digestive system, then it is necessary to direct therapy to treat the primary disease.
Some forms of organ damage do not have precise therapeutic recommendations. For example, there are known cases of spontaneous healing of lymphocytic gastritis. However, any chronic pathologies must be treated.
Therapy of chronic gastritis in children
Pediatricians have not established an optimal treatment regimen for chronic gastritis in childhood. Some experts believe that the clear indication for treatment is the development of a stomach ulcer, and asymptomatic treatment does not require medication. The child’s body is more susceptible to the effects of antibiotics, so antimicrobial therapy should be approached with caution.
We examined the general issues of the manifestation of the disease and provided information on how to cure chronic gastritis. The sooner the patient consults a gastroenterologist, the higher the likelihood of complete remission.
Prevention of all types of gastritis
A proper diet will help keep the microflora in order.
So, paying attention to the prevention of chronic gastritis, it is important to note that a number of preventive measures for this disease completely coincide with similar measures, but with respect to the acute form of the disease. In general, all types of gastritis can be prevented in two ways:
- The first is public prevention. The essence of this procedure is that government agencies monitor how all food products are produced on the territory of the Russian Federation and whether their quality meets what is necessary for the normal functioning of the gastrointestinal tract of the residents of our country.
- The second is individual prevention. In the same event, each patient with gastritis must personally carry out some preventive measures that should minimize all risks of exacerbation of gastritis.
If the first type of prevention does not require the participation of the person suffering from the disease at all, but for the second, the responsibility lies entirely with him. In order to comply with basic preventive measures of an individual nature, it is necessary:
- Stick to some diet. No strict restrictions are required, but you will have to give up fast food, large amounts of fried, half-raw and fish foods. In addition, it is important to minimize the intake of spices as much as possible, because in any form this food product greatly irritates the gastrointestinal mucosa, and this can already aggravate any form of gastritis. The ideal nutritional option in the presence of chronic or acute gastritis is to alternate liquid and dry foods in the diet.
- Monitor the quality of products. Prevention in this regard is to try not to eat food of questionable production or origin. That is, it is better not to risk consuming possibly expired food or food made from low quality raw materials.
- Organize the most correct diet. There are no particular difficulties in this - it is enough to eat small meals, 4-7 times a day. This approach to nutrition stabilizes the level and secretion of gastric fluid, which minimizes the risk of re-inflammation of the gastrointestinal mucosa.
- Carefully monitor the amount of food you eat. It is, of course, possible to undereat, but overeating is, in principle, unacceptable. Try to eat proportionate portions and do not go hungry for long periods of time.
- Eat food following a certain technique. This means that you need to eat in a calm environment, chewing your food thoroughly and slowly. Otherwise, the risk of re-exacerbation of gastritis increases by 10-15%.
- Limit your consumption of alcoholic beverages. Everything is simple here - don’t abuse alcohol, and especially don’t drink low-quality surrogate. Such phenomena not only irritate the gastrointestinal mucosa, but can also cause chemical burns, which is very dangerous not only for gastritis.
- Quit smoking or “smoking” as correctly as possible. It's no secret that tobacco smoke is the worst enemy of any mucous membrane. Fortunately, it practically does not reach the stomach, but still there is some contact. In order to minimize it in the presence of gastritis of any form, it is advisable to completely quit smoking. Otherwise, you should stop “smoking” on an empty stomach, while eating or immediately after it, and also give up flavored cigarettes and reduce the amount you smoke.
- Avoid contact with chemical compounds in the form of smoke or vapors. The essence of the effect of such things on the gastrointestinal mucosa is completely similar to tobacco smoke. Considering this nuance, any person suffering from gastritis is simply obliged not to come into contact with chemicals and poisons in the form of vapors, as this is guaranteed to aggravate the inflammation of the mucous membrane of his stomach.
Note: if the disease in your particular case is accompanied by purulent formations or phlegmon in the stomach, it is important to supplement the prevention of gastritis with timely and adequate neutralization of their exacerbations.