Duodenitis is an inflammation of the mucous membrane of the duodenum. It digests food evacuated from the stomach with the help of pancreatic juice and bile. In addition, the duodenum produces hormones that regulate the activity of the digestive tract.
There is an acute and chronic form of the disease. In 90% of cases it is the second option that occurs. The disease is dangerous because it can be complicated by intestinal bleeding, pancreatitis and other diseases.
At CELT you can get advice from a gastroenterologist.
- Initial consultation – 4,200
- Repeated consultation – 3,000
Make an appointment
Causes of the disease
There are many factors leading to duodenitis. The most common are the following:
- poor nutrition (abuse of spicy, sour, smoked, fried foods);
- bad habits (drinking alcohol, smoking);
- Helicobacter Pylori infection;
- uncontrolled use of certain medications (in particular anti-inflammatory drugs);
- gastritis and peptic ulcer;
- disruption of the blood supply to the organ;
- chronic liver diseases (cirrhosis, hepatitis, etc.);
- anatomical features leading to obstruction of patency;
- Crohn's disease;
- helminthiasis and others.
Symptoms of acute and chronic duodenitis
The acute course of duodenitis lasts 7-10 days, all symptoms are quickly relieved with medications. Chronic duodenitis lasts a long time, can recur several times a year, clinical signs are not so pronounced.
Symptoms of acute duodenitis:
- Pain in the epigastric region (night pain, after eating, when feeling hungry).
- Feeling of bloating, flatulence.
- Belching with a bitter taste and heartburn.
- Decreased appetite.
- Diarrhea, vomiting.
- Abdominal muscle tension.
In the absence of timely and adequate assistance, the disease can become chronic. Characteristic signs of the disease in the chronic stage:
- Disruption of the digestive process.
- Painful sensations in the epigastrium of an aching nature.
- Pain in the right hypochondrium, radiating to the back.
- Feeling of fullness in the stomach.
- Belching and bitter taste in the mouth.
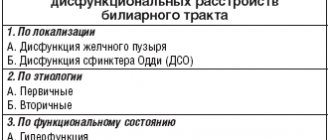
Complex treatment of dysfunctions of the major duodenal papilla
Dysfunction of the major duodenal papilla (MDP) is a functional disease manifested by a violation of the mechanisms of relaxation and contraction of the sphincter of Oddi with a predominance of increased tone and spasm (hypermotor, hyperkinetic) or relaxation and atony (hypomotor, hypokinetic), without organic and inflammatory changes, causing disruption of bile flow and pancreatic juice into the duodenum.
Dyskinesia of the bile ducts usually occurs as a result of a violation of the neurohumoral regulation of the mechanisms of relaxation and contraction of the sphincters of Oddi, Martynov-Lutkens and Mirizzi. In some cases, atony of the common bile duct and spasm of the sphincter of Oddi predominate due to an increase in the tone of the sympathetic part of the autonomic nervous system, in others - hypertension and hyperkinesia of the common bile duct during relaxation of the above-mentioned sphincter, which is associated with excitation of the vagus nerve. In clinical practice, hypermotor dyskinesia is more common. The reason is psychogenic effects (emotional stress, stress), neuroendocrine disorders, inflammatory diseases of the gallbladder, pancreas, duodenum. BDS dysfunctions are often combined with hypermotor and hypomotor dyskinesias of the gallbladder.
Classification:
1. Dysfunction of the hypertensive type:
- with hypermotor, hyperkinetic dyskinesia of the gallbladder;
- with hypomotor, hypokinetic dyskinesia of the gallbladder.
2. Hypotonic type dysfunction (sphincter of Oddi insufficiency):
- with hypermotor, hyperkinetic dyskinesia of the gallbladder;
- with hypomotor, hypokinetic dyskinesia of the gallbladder.
Clinic:
- dull or sharp, severe, persistent pain in the epigastric region or right hypochondrium with irradiation to the right scapula, left hypochondrium, may be of a girdling nature with irradiation to the back;
- not accompanied by fever, chills, enlarged liver or spleen;
- pain is associated with eating, but may appear at night;
- may be accompanied by nausea and vomiting;
- the presence of idiopathic recurrent pancreatitis;
- exclusion of organic pathology of the organs of the hepatopancreatic region;
- clinical criterion: recurrent attacks of severe or moderate pain lasting more than 20 minutes, alternating with pain-free intervals, repeated for at least 3 months, disrupting work activity.
Clinical types of BDS dysfunction:
1. Biliary (more common): characterized by pain in the epigastrium and right hypochondrium, radiating to the back, right scapula:
- option 1 - pain syndrome in combination with the following laboratory and instrumental signs: an increase in aspartate aminotransferase (AST) and/or alkaline phosphatase (ALP) by 2 or more times in a 2-fold study;
- delayed removal of contrast agent from the bile ducts during endoscopic retrograde cholangiopancreatography (ERCP) for more than 45 minutes;
- dilation of the common bile duct more than 12 mm;
2. Pancreatic - pain in the left hypochondrium, radiates to the back, decreases when bending forward, does not differ from pain in acute pancreatitis, may be accompanied by an increase in the activity of pancreatic enzymes in the absence of reasons (alcohol, cholelithiasis):
- option 1 - pain syndrome in combination with the following laboratory and instrumental signs: increased activity of serum amylase and/or lipase 1.5–2 times higher than normal;
- dilation of the pancreatic duct during ERCP in the head of the pancreas is over 6 mm, in the body - 5 mm;
- the time taken for the contrast agent to be removed from the ductal system in the supine position is exceeded by 9 minutes compared to the norm;
3. Mixed - pain in the epigastrium or girdles, can be combined with signs of both biliary and pancreatic types of dysfunction.
The diagnosis of “hypertension of the sphincter of Oddi” is made in cases where the closed sphincter phase lasts longer than 6 minutes, and the secretion of bile from the common bile duct is slow, intermittent, and sometimes accompanied by severe colicky pain in the right hypochondrium.
Insufficiency of BDS is most often secondary, in patients with cholelithiasis, chronic calculous cholecystitis, due to the passage of stones, inflammation of the pancreas, duodenal mucosa, and duodenal obstruction. With duodenal intubation, the closed phase of the sphincter of Oddi is reduced to less than 1 minute or the absence of the sphincter closing phase is noted, the absence of a shadow of the gallbladder and ducts during cholecystocholangiography, the reflux of a contrast agent into the bile ducts during fluoroscopy of the stomach, the presence of gas in the bile ducts, a decrease in residual pressure during cholangiomanometry, reducing the time of radiopharmaceutical entry into the intestine to less than 15–20 minutes with hepatobilis scintigraphy.
Diagnostics
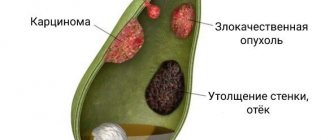
1. Transabdominal ultrasonography. The ultrasound screening method of examination occupies a leading place in the diagnosis of dyskinesias (Table) and makes it possible to identify with high accuracy:
- features of structural changes in the gallbladder and bile ducts, as well as the liver, pancreas (shape, location, size of the gallbladder, thickness, structure and density of the walls, deformations, presence of constrictions);
- the nature of the homogeneity of the gallbladder cavity;
- the nature of the intraluminal contents, the presence of intracavitary inclusions;
- changes in the echogenicity of the liver parenchyma surrounding the gallbladder;
- contractility of the gallbladder.
Ultrasound signs of dyskinesia:
- increase or decrease in volume;
- heterogeneity of the cavity (hyperechoic suspension);
- decreased contractile function;
- with deformation of the gallbladder (kinks, constrictions, septa), which may be a consequence of inflammation, dyskinesias are much more common;
- other signs indicate an inflammatory process, past inflammation, cholelithiasis, and serve for differential diagnosis.
2. Ultrasound cholecystography. Makes it possible to study the motor-evacuation function of the gallbladder within 1.5–2 hours from the moment of taking a choleretic breakfast until the initial volume is achieved. Normally, 30–40 minutes after stimulation, the gallbladder should contract by 1/3–1/2 of its volume. An extension of the latent phase to more than 6 minutes indicates an increase in the tone of the sphincter of Oddi.
3. Dynamic hepatobiliscintigraphy. It is based on recording time indicators of the passage of short-lived radionuclides along the biliary tract. Allows you to evaluate the absorption-excretory function of the liver, the storage-evacuation function of the gallbladder (hypermotor, hypomotor), the patency of the terminal part of the common bile duct, to identify obstruction of the bile ducts, insufficiency, hypertonicity, spasm of the sphincter of Oddi, stenosis of the BDS, to differentiate organic and functional disorders using tests with Nitroglycerin or Cerucal. With hypertonicity of the sphincter of Oddi, there is a slowdown in the flow of the drug into the duodenum after a choleretic breakfast. This method most accurately allows you to determine the type of dyskinesia and the degree of functional impairment.
4. Fractional chromatic duodenal sounding. Gives information about:
- tone and motility of the gallbladder;
- tone of the sphincter of Oddi and Lutkens;
- colloidal stability of cystic and hepatic bile fractions;
- bacteriological composition of bile;
- secretory function of the liver.
5. Gastroduodenoscopy. Allows you to exclude organic lesions of the upper gastrointestinal tract, assess the condition of the obstructive system, and the flow of bile.
6. Endoscopic ultrasonography. Allows you to more clearly visualize the terminal section of the common bile duct, BDS, head of the pancreas, the confluence of the Wirsung duct for the purpose of diagnosing stones, differential diagnosis of organic lesions of the BDS and hypertonicity.
7. Endoscopic retrograde cholangiopancreatography. The method of direct contrasting of the biliary tract allows us to identify the presence of stones, stenosis of the biliary tract, dilatation of the biliary tract, perform direct manometry of the sphincter of Oddi, and is of great importance in the differential diagnosis of organic and functional diseases.
8. Computed tomography. Allows you to identify organic damage to the liver and pancreas.
9. Laboratory diagnostics. In case of primary dysfunctions, laboratory tests do not have any deviations from the norm, which is important for differential diagnosis. A transient increase in the level of transaminases and pancreatic enzymes can be observed after an attack with dysfunction of the sphincter of Oddi.
Treatment
The main goal is to restore the normal outflow of bile and pancreatic juice into the duodenum.
Basic principles of treatment:
1) normalization of the processes of neurohumoral regulation of bile secretion mechanisms - treatment of neuroses, psychotherapy, elimination of hormonal disorders, conflict situations, rest, proper diet; 2) treatment of diseases of the abdominal organs, which are the source of pathological reflexes to the muscles of the gallbladder and bile ducts; 3) treatment of dyskinesia, which is determined by its form; 4) elimination of dyspeptic manifestations.
Treatment for hypertensive dyskinesia
1. Elimination of neurotic disorders, correction of autonomic disorders:
- sedatives: herbal infusions of valerian and motherwort, Corvalol, Novo-passit - have a sedative effect, normalize sleep, relax smooth muscles;
- tranquilizers: Rudotel (medazepam) - 5 mg in the morning and afternoon, 5-10 mg in the evening; Grandaxin - 50 mg 1-3 times a day;
- psychotherapy.
2. Diet therapy:
- diet with frequent (5–6 times a day), split meals;
- exclude alcoholic and carbonated drinks, smoked, fried, fatty, spicy, sour foods, seasonings, animal fats, oils, concentrated broths (diet No. 5);
- exclude or limit the consumption of egg yolks, baked goods, creams, nuts, strong coffee, tea;
- buckwheat porridge, millet, wheat bran, cabbage are shown.
3. Antispasmodics:
- No-spa (drotaverine) - 40 mg 3 times a day for 7-10 days to 1 month, to relieve a painful attack - 40-80 mg, or 2-4 ml of a 2% solution intramuscularly, intravenously drip in physiological sodium chloride solution ;
- Papaverine - 2 ml of 2% solution intramuscularly, intravenously; in tablets 50 mg 3 times a day;
- Duspatalin (mebeverine) - 200 mg 2 times a day 20 minutes before meals.
4. Prokinetics: Cerucal (metoclopramide) - 10 mg 3 times a day 1 hour before meals.
5. Odeston (hymecromone) - has an antispasmodic effect, relaxes the sphincter of the gallbladder, bile ducts and sphincter of Oddi, without affecting the motility of the gallbladder - 200-400 mg 3 times a day for 2-3 weeks.
Treatment for hypotonic dyskinesia
1. Diet therapy:
- fractional meals - 5-6 times a day;
- the diet includes products that have a choleretic effect: vegetable oil, sour cream, cream, eggs;
- The menu should include a sufficient amount of fiber, dietary fiber in the form of fruits, vegetables, rye bread, since regular bowel movements have a tonic effect on the bile ducts.
2. Choleretics - stimulate the bile-forming function of the liver:
- Festal - 1-2 tablets 3 times a day after meals;
- Kholosas, Kholagol - 5-10 drops 3 times a day 30 minutes before meals, decoction of choleretic herbs - 3 times a day - 10-15 days.
3. Having antispasmodic and choleretic effects:
- Odeston - 200-400 mg 3 times a day - 2-3 weeks. Effective in cases of simultaneous presence of hypomotor dysfunction of the gallbladder and hypermotor dysfunction of the sphincter of Oddi;
- Essentiale Forte N - 2 capsules 3 times a day.
4. Cholekinetics - increase the tone of the gallbladder, reduce the tone of the bile ducts:
- 10–25% solution of magnesium sulfate, 1–2 tablespoons 3 times a day;
- 10% sorbitol solution, 50–100 ml 2–3 times a day, 30 minutes before meals;
- herbal products.
5. Prokinetics:
- Cerucal (metoclopramide) - 10 mg 3 times a day 1 hour before meals;
- Motilium (domperidone) - 10 mg 3 times a day 30 minutes before meals.
6. “Blind tubage” - duodenal intubation and duodenal lavage with warm mineral water, administration of a 20% sorbitol solution, which reduces or eliminates sphincter spasm, increases the outflow of bile - 2 times a week.
Odeston is effective in cases of simultaneous presence of hypomotor dysfunction of the gallbladder and hypermotor dysfunction of the sphincter of Oddi. With a combination of hyperkinetic, normokinetic dysfunction of the gallbladder and hyperkinetic dysfunction of the sphincter of Oddi, the effectiveness of No-shpa therapy reaches 70–100%. When hypokinetic dysfunction of the gallbladder and hyperkinetic sphincter of Oddi are combined, the appointment of Cerucal or Motilium is indicated, possibly in combination with No-shpa. When hypermotor dysfunction of the gallbladder and hypomotor sphincter of Oddi are combined, the administration of artichoke extract 300 mg 3 times a day is effective.
Antispasmodics are the main medication for the treatment of hypertensive, hyperkinetic dysfunctions of the gallbladder and sphincter of Oddi during acute pain attacks and pain during the interictal period. Myotropic antispasmodics have a targeted effect on the smooth muscles of the entire biliary system. The results of numerous studies have shown that drotaverine (No-shpa) is the drug of choice from the group of myotropic antispasmodics, it allows to relieve pain, restore the patency of the cystic duct and the normal outflow of bile into the duodenum, and eliminate dyspeptic disorders. The mechanism of action is inhibition of phosphodiesterase, blocking Ca2+ channels and calmodulin, blocking Na+ channels, resulting in a decrease in the tone of the smooth muscles of the gallbladder and bile ducts. Dosage forms: for parenteral use - ampoules of 2 ml (40 mg) of drotaverine, for oral administration - 1 tablet of the drug No-Shpa (40 mg of drotaverine), 1 tablet of the drug No-Shpa forte (80 mg of drotaverine).
Advantages of the drug No-Shpa:
- Rapid absorption: the peak concentration of the drug in plasma occurs after 45–60 minutes, 50% absorption is achieved in 12 minutes, which characterizes drotaverine as a rapidly absorbed drug.
- High bioavailability: when taken orally it is 60%, after a single oral dose of 80 mg of drotaverine hydrochloride, the maximum concentration in plasma is achieved after 2 hours, penetrates well into the vascular wall, liver, wall of the gallbladder and bile ducts.
- The main route of metabolism is the oxidation of drotaverine to monophenolic compounds; the metabolites are quickly conjugated with glucuronic acid.
- Complete elimination: the half-life is 9–16 hours, about 60% of oral administration is excreted through the gastrointestinal tract and up to 25% in the urine.
- The presence of a dosage form of No-shpa for both oral and parenteral administration makes possible the widespread use of the drug in emergency situations.
- The drug No-shpa can be used during pregnancy (after carefully weighing the balance of benefits and risks).
- Quick onset of action, long-lasting effect: parenteral administration of drotaverine (No-Shpa) provides a quick (within 2-4 minutes) and pronounced antispasmodic effect, which is especially important for the relief of acute pain.
- The tablet form is also characterized by a rapid onset of action.
- High clinical effectiveness in small doses: 70%, 80% of patients experience relief of symptoms of spasm and pain within 30 minutes.
- There is no significant difference in the speed of achieving the antispasmodic effect between monotherapy with No-shpa and combination therapy.
- Time-tested safety, no serious side effects for a period of more than 50 years. The lack of anticholinergic activity affects the safety of drotaverine, expanding the range of people to whom it can be prescribed, in particular, in children, in elderly men with prostate pathology, with concomitant pathology and in combination with other drugs when taking two or more drugs simultaneously.
Thus, a review of the results of numerous clinical studies indicates that No-Spa is an effective drug for the rapid relief of spasms and pain in hypertensive, hyperkinetic forms of dyskinesia of the gallbladder and sphincter of Oddi.
Literature
- Dadvani S. A., Vetshev P. S., Shulutko A. M. et al. Gallstone disease. M.: Vidar-M, 2000. 139 p.
- Leuschner U. Practical guide to biliary tract disease. M.: GEOTAR-MED, 2001. 264 p.: ill.
- Galperin E.I., Vetshev P.S. Guide to biliary tract surgery. 2nd ed. M.: Vidar-M, 2009. 568 p.
- Ilchenko A. A. Diseases of the gallbladder and biliary tract: A guide for doctors. M.: Anacharsis. 2006. 448 p.: ill.
- Ilchenko A. A. Gallstone disease. M.: Anacharsis. 2004. 200 p.: ill.
- Ivanchenkova R. A. Chronic diseases of the biliary tract. M.: Publishing house "Atmosphere", 2006. 416 pp.: ill.
- Butov M. A., Shelukhina S. V., Ardatova V. B. On the issue of pharmacotherapy of biliary tract dysfunction / Abstracts of the V Congress of the Scientific Society of Gastroenterologists of Russia, February 3–6, 2005, Moscow. pp. 330–332.
- Mathur SK, Soonawalla ZF, Shah SR et al. Role of biliary scintiscan in predicting the need for cholangiography // Br. J. Surg. 2000. No. 87 (2). P. 181–185.
- Blasko G. Pharmacology, mechanism of action and clinical significance of a convenient antispasmodic agent: drotaverine // JAMA India - The physician's update, 1998, v. 1 (No. 6), p. 63–70.
- Functional diseases of the intestine and biliary tract: issues of classification and therapy // Gastroenterology. 2001, No. 5, p. 1–4.
- Rational pharmacotherapy of diseases of the digestive system / Ed. V. T. Ivashkina. M.: Litterra, 2003, 1046 p.
- Tomoskozi Z., Finance O., Aranyi P. Drotaverine interacts with L-type Ca2+ channel in pregnant rats uterine membranes // Eur. J. Pharmacol. 2002, v. 449, p. 55–60.
- Malyarchuk V.I., Pautkin Yu.F., Plavunov N.F. Diseases of the major duodenal papilla. Monograph. M.: Cameron Publishing House, 2004. 168 pp.: ill.
- Nazarenko P. M., Kanishchev Yu. V., Nazarenko D. P. Surgical and endoscopic methods of treating diseases of the major duodenal papilla of the duodenum and their clinical and anatomical rationale. Kursk, 2005. 143 p.
A. S. Vorotyntsev, Candidate of Medical Sciences, Associate Professor
GBOU VPO First Moscow State Medical University named after. I. M. Sechenova Ministry of Health and Social Development of Russia, Moscow
Contact information about the author for correspondence
Methods for diagnosing duodenitis
Diagnostics plays an important role. An incorrect or inaccurate diagnosis will affect the entire treatment. Therefore, you should not be afraid and refuse diagnostic procedures prescribed by your doctor.
Gastroscopy
- Cost: 3,000 rub.
More details
- EGDS (esophagogastroduodenoscopy) - using a flexible probe equipped with a video camera, the doctor examines the esophagus, stomach and duodenum. Using this method, you can see redness and swelling of the mucous membrane, erosion, and with a decrease in tone, smoothing of folds, the presence of nodules, hemorrhages and other signs that can be used to diagnose duodenitis.
- X-ray using a contrast agent (barium sulfate), which allows you to identify anatomical disorders, signs of inflammation, obstruction, the presence of an ulcer or tumor, signs of impaired intestinal tone and motility.
- Ultrasound diagnostics allows you to evaluate nearby organs, diseases of which can lead to duodenitis.
- A laboratory examination is prescribed (general blood test, biochemical analysis, examination for the presence of Helicobacter pylori infection, and others).
- Fecal occult blood test to ensure there are no bleeding ulcers or erosions.
- General analysis of stool (coprogram), which helps to identify signs of disturbances in duodenal digestion.
How is the disease diagnosed?
At the initial appointment, the doctor will conduct a survey and examination; if duodenitis is suspected, he will definitely refer you for gastroscopy, as well as clinical blood tests. The following additional diagnostic tools are used:
- X-ray of the stomach, duodenum;
- laboratory tests of gastric juice;
- analysis for Helicobacter Pylori;
- gastroduodenal intubation;
- coprogram (stool analysis);
- “biochemistry” of blood, etc.
If a specialist suspects possible malignancy of pathological areas, a portion of the mucosal tissue is collected and subsequently examined.
Based on the examination results, the doctor determines the form and type of inflammatory disease and prescribes effective treatment.
Treatment of duodenitis
First of all, it is necessary to normalize your diet. As a rule, a therapeutic diet is prescribed (table No. 1 in the acute stage and No. 5 in the chronic stage).
In acute cases of the disease, it is allowed to consume weak tea, cocoa, low-fat cottage cheese, eggs, oatmeal and semolina porridge, and pureed soups. Prohibited: mushrooms, peppers, sweets, coffee, fatty meat and fish, buns. During chronic exacerbation, vegetable soups, bread, lean meats (beef, chicken), and non-acidic fruits are allowed. The same things are prohibited as in the acute stage. During the period of remission, you can eat any food, but in moderation. Preference should be given to a healthy and proper diet and not to overeat.
Medicines are prescribed depending on the cause of the disease.
- Antibiotic therapy for Helicobacter Pylori infection
- Medicines to reduce acid production in the stomach.
- Preparations with an enveloping effect.
- Anti-inflammatory drugs.
- Pancreatic enzymes.
- Medicines aimed at restoring the mucous membrane (cytoprotectors).
- Antispasmodic drugs.
- If helminths are present, take medications to get rid of them.
- With high psycho-emotional stress, sedatives may be prescribed.
Attention! All medications are prescribed only by a doctor based on an analysis of the medical history, examination and research. Self-medication is unacceptable. Information about medications is given for informational purposes only.
Treatment of lymphedema
Complex physical decongestant therapy (CPDT) is a method that is the gold standard in the treatment of lymphostasis, which often achieves tangible results and significantly reduces swelling, which leads to an improvement in the patient’s quality of life.
This technique includes:
- manual lymphatic drainage massage;
- compression therapy (banding with low-tensile bandages in the 1st phase, wearing flat compression hosiery in the 2nd phase);
- skin care;
- therapeutic exercises.
Complications of the disease
Since the disease is not always pronounced, many people let the disease take its course. When taking painkillers, do not rush to see a doctor. But relief of symptoms will never replace proper treatment, and its absence can lead to the following adverse consequences:
- duodenal ulcer with perforation (a through hole in the intestinal wall);
- intestinal bleeding;
- acute pancreatitis (inflammation of the pancreas);
- jaundice (if the secretion of bile from the ducts into the duodenum is impaired, bilirubin in the blood increases);
- duodenal dystrophy.
Surgical treatment of lymphedema
There are many methods of surgical treatment of lymphedema, which have a number of indications and contraindications.
Microsurgical techniques are also used:
- Transfer of vascularized lymph nodes from another part of the body to the affected area (VLNT).
- Lymphatic-venous anastomoses (LVA): VLNT and LVA are microsurgical procedures that can improve physiological drainage of lymphatic fluid and eliminate the need for constant wearing of compression garments in some patients. These procedures provide better results when there is less damage to the patient's lymphatic system.
- Suction-assisted protein lipectomy (SAPL). This technique is more effective in the later stages of lymphedema and allows you to remove excess fatty tissue that cannot be removed by conservative therapy for lymphedema or VLNT or LVA operations.
Prognosis and prevention
A timely diagnosis and prescribed treatment will help solve the problem of acute duodenitis. If the disease has progressed to a chronic stage, then it is necessary to regularly see a gastroenterologist. Optimally – 1-2 times a year. In general, the prognosis is favorable.
Preventive measures are aimed at eliminating nutritional problems, giving up alcohol and smoking. It is necessary to promptly identify and treat other diseases of the gastrointestinal tract. Never take medications without a doctor's prescription, especially for a long period. After all, even seemingly harmless aspirin can lead to the development of duodenitis. In the chronic course of the disease, it is useful to visit sanatoriums and resorts. Do not forget about the rules of hygiene to prevent infections with helminths and Helicobacter.
At the CELT clinic you can see a gastroenterologist, as well as undergo all the necessary examinations and tests.
Stages of lymphedema
Stage 0 – lymphatic vessels are damaged, but there is no swelling yet due to the body’s compensatory mechanisms
Stage 1 – transient mild swelling that occurs gradually throughout the day. When pressed with a finger, a hole is formed
Stage 2 – the skin begins to thicken (fibrosis), it is not always possible to make a dimple in the skin, the swelling is significant and dense, does not go away after rest
Stage 3 – severe swelling and skin changes
(Clinical classification of lymphedema, International Society of Lymphology)
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Gastroscopy (videoesophagogastroduodenoscopy) | 6 000 |
| Ultrasound of the abdominal organs (liver, gall bladder, pancreas, spleen) | 3 800 |
| Fluoroscopy and radiography of the stomach | 4 800 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Signs and symptoms of lymphedema
- Swelling of the extremities, including the arms, hands, legs, feet. This may be the entire limb or just part of it. It can be one-sided or two-sided.
- Swelling proximally to the chest, shoulder, pelvis, groin, genitals, face/intraoral tissues.
- Pain and feeling of fullness, discomfort in the joints.
- Limbs may feel heavy and painful.
- Decreased mobility and range of motion of the affected limb.
- Change in sensitivity.
- Skin changes such as redness and fever.
- Hyperkeratosis (thickening of the skin) and lymphangiectasia (dilated superficial lymphatic vessels)