Cholecystitis can be caused by bacteria (Escherichia coli, streptococcus, staphylococcus, etc.), helminths, Giardia, fungi; cholecystitis of toxic and allergic nature occurs. Microbial flora penetrates the gallbladder ascending (from the intestine), hematogenous (through the blood) or lymphogenous (through lymph) route. Congestion of bile in the gallbladder predisposes to the development of cholecystitis, which can be caused by gallstones, compression and kinks of the bile ducts, dyskinesia of the gallbladder and biliary tract (i.e., disruption of their tone and motor function under the influence of stress, endocrine and autonomic disorders, reflexes from pathologically altered organs of the digestive system), prolapse of the viscera, pregnancy, sedentary lifestyle, rare meals, reflux of pancreatic juice into the biliary tract during dyskinesia with its damaging effect on the mucous membrane of the bile ducts and gallbladder.
The direct impetus for an outbreak of the inflammatory process in the gallbladder is often overeating, especially eating fatty and spicy foods, drinking alcoholic beverages, or an acute inflammatory process in another organ (tonsillitis, pneumonia, adnexitis, etc.). Chronic cholecystitis can occur after acute cholecystitis, but more often it develops independently and gradually, against the background of cholelithiasis, gastritis with secretory insufficiency, chronic pancreatitis and other diseases of the digestive system, obesity.
Symptoms of chronic cholecystitis
Chronic cholecystitis is characterized by a dull, aching (sometimes sharp) pain in the right hypochondrium that is constant or occurs 1–3 hours after a heavy meal, especially fatty and fried food. The pain radiates upward, to the area of the right shoulder and neck, right shoulder blade. Dyspeptic symptoms are common: a feeling of bitterness and a metallic taste in the mouth, belching of air, nausea, flatulence, defecation disorders (possibly alternating constipation and diarrhea), as well as irritability and insomnia. Jaundice is not typical.
Signs of chronic cholecystitis are determined by ultrasound examination. The course in most cases is long, with alternating periods of remission and exacerbations; the latter often occur as a result of eating disorders, drinking alcohol, heavy physical work, acute intestinal infections, and hypothermia. The prognosis is favorable in most cases. However, often the inflammatory process contributes to the formation of gallstones.
Diagnosis of chronic cholecystitis
Diagnosis of chronic cholecystitis begins with identifying the main complaints and external signs of the disease, prompting the doctor to further the diagnostic algorithm. To clarify the diagnosis of chronic cholecystitis, the following diagnostic methods are used:
- An ultrasound of the abdominal organs,
in particular the gallbladder, can reveal the presence of stones or signs of inflammation in the gallbladder. - Cholegraphy
is an x-ray examination method that allows you to identify signs of inflammation of the gallbladder. Holegraphy is not performed during exacerbation of the disease, or during pregnancy (in these cases, ultrasound is preferred). - General and biochemical blood tests
- allow you to identify signs of inflammation and other signs characteristic of liver and gallbladder diseases - Fecal analysis for parasites
(roundworms, lamblia) is mandatory for all patients with cholecystitis.
More about the disease
Chronic cholecystitis is an inflammatory disease of the gallbladder that develops over a long period of time.
Most often, this form of inflammation develops after the manifestation of acute cholecystitis. A common cause of pathology is blockage of the excretory ducts of the gallbladder with stones, but other etiologies are also possible. Patients suffering from this disease complain of pain in the right hypochondrium, diarrhea, nausea, vomiting and other symptoms. Unpleasant sensations may periodically disappear, but during exacerbations the pain intensifies. In most cases, chronic cholecystitis is complicated by an infectious process of a bacterial or fungal nature. Pathogenic microflora can penetrate the organ from the cavity of the gastrointestinal tract or from distant anatomical areas. The development of infection is facilitated by prolonged stagnation of bile. In addition, the course of cholecystitis is negatively affected by existing diseases, such as diabetes and HIV infection. Delaying treatment increases the risk of developing dangerous complications, so it is recommended to be examined by a gastroenterologist in the early stages of inflammation, when abdominal pain and symptoms of digestive disorders appear.
Hologenic diarrhea
Secretory diarrhea occurs as a result of the fact that the secretion of water into the intestinal lumen prevails over absorption. The main activators of secretion are bacterial toxins, enteropathogenic viruses, drugs, biological active substances (free bile acids, long-chain fatty acids), some gastrointestinal hormones (secretin, VIP), prostaglandins, serotonin and calcitonin. Secretory diarrhea is characterized by copious, watery stools (usually more than 1 liter). Hyperosmolar diarrhea develops when the osmotic pressure of the chyme increases, preventing the absorption of water from the intestinal lumen. Osmotic pressure in the intestinal cavity increases when absorption is impaired due to the accumulation of products of hydrolytic breakdown of nutrients in the intestinal cavity. Hyperosmolar diarrhea is characterized by profuse, loose stools with a large amount of food debris. Exudative diarrhea is characteristic of inflammatory bowel diseases and is characterized by the exudation of water and electrolytes into the intestine through damaged mucous membranes. With exudative diarrhea, the stool is liquid, often with blood and pus. Hyper- and hypokinetic diarrhea. The cause of hyper- and hypokinetic diarrhea is a violation of intestinal motor function. An increase in the transit rate is facilitated by laxatives and antacids containing magnesium salts, as well as biologically active substances, such as secretin, pancreozymin, gastrin, prostaglandins and serotonin. This type of diarrhea is characteristic of irritable bowel syndrome. With hyper- and hypokinetic diarrhea, stool is frequent and liquid, but its daily amount does not exceed 200–300 g; The appearance of stool is preceded by cramping pain in the abdomen, which subsides after defecation. The above mechanisms of diarrhea are closely related to each other, however, each nosological form of pathology is characterized by one or another predominant type of diarrhea. This explains the features of the clinical manifestations of intestinal dysfunction. One example is diseases in which diarrhea is caused by bile acids. Diarrhea caused by bile acids – hologenic diarrhea (CD) – has its own pathogenetic and clinical characteristics, as well as approaches to treatment [3,4].
Etiology and pathogenesis of HD The cause of hologenic diarrhea is the excessive flow of bile acids into the colon. Bile acids (BAs) increase the activity of adenylate cyclase in the intestinal wall with the formation of cAMP, which causes the secretion of Na+ ions and water into the intestinal lumen. The entry of a large amount of bile into the colon occurs due to malabsorption of fatty acids and an increase in the motor-evacuation function of the small intestine. Malabsorption of fatty acids can rarely be primary (congenital), quite often they are secondary (due to Crohn's disease and other inflammatory diseases of the small intestine). An increase in the rate of transit through the small intestine is caused by intestinal hormones, as well as by the FA themselves, if they enter the empty small intestine, i.e. during the interdigestive period. Asynchronous intake of fatty acids with food is observed in biliary dyskinesias, inflammatory diseases of the gallbladder or its absence (cholecystectomy). The presence of a large amount of bile in the cecum and other parts of the colon is decisive in the pathogenesis of diarrhea and pain in the right iliac region, often accompanying HD.
Peculiarities of the clinical picture of hCG Hologenic diarrhea, as a rule, is not an independent nosological form. It occurs, as already mentioned, either when a large amount of FA enters the colon due to impaired absorption in the small intestine, or rapid transit. Therefore, CD develops in patients who have undergone resection of the small intestine, with Crohn's disease, disorders of bile secretion (gallbladder disease, cholecystectomy, etc.). A characteristic sign of HD is the presence of fatty acids in the stool: it usually has a bright yellow or greenish color. Another characteristic sign of this type of diarrhea may be pain in the right iliac region, often appearing upon palpation of the cecum and ascending colon. HD has a rather persistent chronic but non-progressive course.
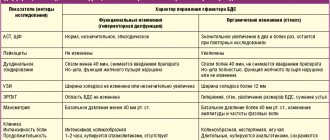
Diagnosis HD indicates the presence of bile in the stool, which can be seen by the characteristic bright yellow or greenish color of the feces. During colonoscopy, you can sometimes observe the presence of bile in the intestine: it thickly covers the walls of the cecum and ascending colon. The most accurate diagnosis of HD can be confirmed by a high concentration of FA in the feces. According to our data, which has not yet been published, the normal amount of FA in the daily amount of feces does not exceed 100 mg/g. With HD, the concentration of FA increases several times. Indirect confirmation of the possible connection of diarrhea with excess intake of bile acids into the colon are clinical and instrumental signs of gallbladder pathology (hypokinesia, changes in wall thickness, stones, etc.), cholecystectomy. Approximate formulations of diagnosis • Gallstone disease. Cholecystectomy (2008). Hologenic diarrhea. • Short small bowel syndrome. Resection of the ileum for small bowel obstruction (2007). Hologenic diarrhea. • Biliary dyskinesia. Hologenic diarrhea.
Treatment The goal of pathogenetic therapy for HD is to restore normal function of the biliary tract and eliminate the detergent effect of GI on the intestinal mucosa during the interdigestive period. To improve the function of the biliary tract, it is recommended to prescribe choleretic drugs, for example, Gepabene. The alkaloid fumarin contained in Gepabene eliminates spasms of the gallbladder and bile ducts, thereby facilitating the flow of bile into the duodenum. The presence of the hepatoprotector silymarin in the preparation helps to improve the function of hepatocytes and, consequently, improve the quality of bile. Silymarin binds free radicals and toxic substances in liver tissue; has antioxidant, membrane-stabilizing and cytoprotective effects, stimulates protein synthesis, promotes the regeneration of hepatocytes. Thus, Gepabene combines hepatoprotective and antispasmodic properties. In patients with chronic cholecystitis, when using Gepabene, choleresis increases and the contractile function of the gallbladder improves. Gepabene should be taken 1 capsule during meals, without chewing, with water. In order to capture FA during the interdigestive period, it is recommended to prescribe adsorbents. The main properties of enterosorbents are the ability to bind toxic products, normalize motility, and strengthen the protective function of the intestinal mucous barrier. Enterosorbents are prescribed between meals, i.e. 3-4 hours after eating. For patients with HD, medications used for other types of diarrhea may also be indicated (Table 2). Thus, when symptoms of excessive bacterial growth appear in the small intestine (flatulence, increased hydrogen in the exhaled air, etc.), antibacterial agents are prescribed for 5–7 days, then probiotics (Linex, Bifiform, Probifor, etc.) are prescribed for 3–4 weeks. Octreotide is indicated for patients with extensively resected small bowel. Being a synthetic analogue of somatostatin, this drug inhibits the secretion of water and electrolytes into the intestinal lumen and reduces watery diarrhea. Octreotide is prescribed subcutaneously at 100 mcg 3 times a day until diarrhea subsides. The use of such complex therapy helps to stop hologenic diarrhea within 1–2 weeks.
Conclusions 1. The pathogenetic mechanism for the development of hologenic diarrhea is an increased flow of bile into the large intestine, where it increases the secretion of water and electrolytes. 2. Hologenic diarrhea develops after extensive resection of the small intestine, including the ileum, in patients with inflammatory diseases of the ileum, biliary dyskinesias and after cholecystectomy. 3. Hologenic diarrhea developing after cholecystectomy can be considered as a separate variant of postcholecystectomy syndrome. 4. The main clinical symptoms of hologenic diarrhea are frequent watery stools with bright yellow or greenish coloration of feces and pain in the right iliac region when a large amount of bile enters the cecum. 5. For the treatment of hologenic diarrhea, it is necessary to use: a) during the interdigestive period - adsorbents that bind excess unabsorbed bile acids in the colon; b) during meals - choleretic agents that promote optimal participation of bile in intestinal digestion.
References 1. Farthing MJ Diarrhoea: a significant world wide problem. Int. J. Antimicrob. Agents 2000; 14:65–9. 2. Binder HJ Causes of Chronic Diarrhea. NEJM 2006; 355:236–9. 3. Parfenov A.I. Diseases of the ileocecal region. M.: Anacharsis 2005; 280 pp. 4. Parfenov A.I., Krums L.M., Lychkova A.E., Poleva N.I. Hologenic diarrhea. Ter. Arch.2008;80(2):33–38
Work of the organ
The gallbladder is an anatomical part of the liver. This sac-like organ is necessary for storing bile synthesized by liver cells and removing fluid into the small intestine during digestion. The release of bile into the cavity of the duodenum promotes the absorption of fatty foods and improved absorption of nutrients. There is a constant accumulation of secretion in the organ, leading to an increase in the viscosity of the fluid. After food enters the intestines, hormones stimulate the relaxation of special valves and the release of bile into the gastrointestinal tract through special ducts.
Other organ functions:
- Maintaining metabolism.
- Improving small intestinal motility.
- Release of excess cholesterol and bilirubin from the body.
- Activation of enzymes necessary for the absorption of protein foods.
The gallbladder is often subject to pathological influences. Disruption of the muscular lining of the organ can impede the secretion of bile - this process not only harms digestion, but also contributes to the formation of stones that can subsequently completely block the bile ducts and damage the internal lining of the gallbladder. Normally, the organ does not contain microflora, but with diseases and anatomical defects, pathogenic and conditionally pathogenic microorganisms from the intestine may penetrate into the gallbladder.
Causes
The inflammatory process in the gallbladder can be triggered by various factors. First of all, this is stagnation of bile, which disrupts the functions of the organ and contributes to the occurrence of infection. Escherichia coli, streptococci, Giardia and other pathogenic microorganisms can penetrate from the intestines into the organ. In this case, the occurrence of infection can be a direct cause of inflammation or a consequence of such a pathological process.
Possible reasons:
- Blockage of the biliary tract, which occurs due to an anatomical defect, stones, or malfunction of the valves.
- Gallstone disease is a common pathology of the gallbladder. Stones can form in the organ due to a violation of the chemical composition of bile and stagnation of secretions.
- Malignant or benign tumor. A growing tumor can make it difficult to evacuate bile from the organ.
- Primary infections. In patients with HIV infection, a variety of viruses can infect the gallbladder.
- Impaired motility of the gallbladder and its ducts. With insufficient or chaotic contractility of the smooth muscles of the organ, the outflow of bile into the intestine becomes difficult.
A chronic form of inflammation can occur if the patient has not been treated for acute cholecystitis. This pathology persists for many years and significantly worsens a person’s quality of life.
Risk factors
There are various forms of predisposition to the disease associated with individual characteristics, primary pathologies, nutrition and heredity. Doctors must take into account the presence of risk factors for cholecystitis during examinations.
Key risk factors:
- Female gender and age from 25 to 45 years.
- Obesity and significant weight loss over several months.
- Taking certain medications. In particular, the risk of developing inflammation in the gallbladder increases with the use of hormonal drugs.
- Pregnancy.
- Chronic diseases of the intestines, liver and pancreas.
- Surgical treatment of abdominal organs, trauma.
- Chronic foci of inflammation in different parts of the body.
- Long-term parenteral nutrition.
- Poor nutrition or prolonged fasting.
- Alcohol abuse.
- Myocardial infarction and other heart diseases.
- Vascular disorders in diabetes mellitus.
- Abnormal reflux of pancreatic secretions into the gallbladder (pancreatobiliary reflux).
- Insufficient physical activity.
Effective measures to prevent pathology are based on the elimination of risk factors and are associated with the patient’s lifestyle and individual medical history.
Diagnosis and treatment of the disease
It is impossible to independently diagnose and cure cholecystitis - the symptoms are similar to liver pathologies and do not provide a complete clinical picture. To make a diagnosis, you must urgently contact a gastroenterologist. The specialist will conduct an examination and prescribe a diagnosis, which includes a comprehensive examination:
- laboratory tests (CBC, OAM, blood biochemistry);
- hardware research methods (ultrasound, MRI, CT).
Diagnostic studies allow you to localize the lesion, assess the severity of the disease and select the correct treatment tactics.
Health care
Conservative treatment of cholecystitis is prescribed to patients with a chronic or labile course of the disease. The therapeutic plan includes the following drugs:
- antibiotics to suppress pathogenic flora;
- antispasmodics to relieve pain, suppress spasms and prevent organ rupture;
- choleretic agents to restore the flow of bile;
- removal of gallstones.
Drug therapy is prescribed outside the exacerbation phase and is carried out over a long course.
In case of acute cholecystitis of the organ, abdominal or laparoscopic cholecystectomy is performed. Surgery to remove the gallbladder is indicated for patients with an acute attack, rupture of the organ, or in the absence of positive results of conservative treatment.
Lifestyle correction
Comprehensive treatment of cholecystitis includes normalization of nutrition. Patients are recommended a therapeutic diet that is aimed at gradual weight loss and minimizes the damage that fatty foods cause to the biliary tract. Alcoholic drinks are also completely excluded from the diet. Optimized physical activity is a prerequisite for patients, especially those with obesity. A complex of therapeutic and preventive gymnastics allows you to lose weight and helps restore the flow of bile during physiological stagnation.
Medical offers treatment of cholecystitis in Lobnya. Help for patients with inflammation of the gallbladder consists of an integrated approach in which the patient receives:
- consultations with a highly qualified gastroenterologist;
- fast and accurate diagnosis;
- a treatment plan developed in accordance with the severity of the condition and the individual characteristics of the body.
Our clinic specialists recommend combining conservative therapy with normalization of nutrition and lifestyle correction.
Forms of the disease
Doctors classify chronic cholecystitis based on the cause of inflammation and the nature of the disease. There is also a classification based on the severity of symptoms.
Basic forms:
- Chronic calculous cholecystitis is the most common variant of the disease, resulting from blockage of the excretory ducts of the organ with stones. Characterized by severe symptoms during exacerbations. The inflammatory process can spread to adjacent anatomical structures, including the diaphragm and pleura.
- Chronic noncalculous cholecystitis is a rarer form of the disorder, often diagnosed in patients with severe illness. In this case, the inflammatory process occurs due to injury, surgery, severe infection and other reasons not related to the formation of stones. If not treated in a timely manner, non-calculous cholecystitis can cause the patient's death.
The danger of chronic inflammation is due to the erased symptoms. Patients pay attention to unpleasant sensations only during exacerbations, as a result of which the disease gradually progresses and causes complications.
General characteristics of the disease
The gallbladder is one of the important visceral organs that is involved in liver function and digestion. As a result of exposure to provoking factors, the outflow of bile is disrupted and focal inflammation occurs, which is localized in the tissues of the organ. The inflammatory process gradually worsens, damaging the walls and changing the quality characteristics of bile.
More than 70% of patients with cholecystitis are middle-aged women.
Depending on the course and provoking factors, inflammation of the gallbladder is divided into 2 types:
- Acute calculous cholecystitis. It manifests itself during an intense course of the inflammatory process and is accompanied by pronounced clinical symptoms.
- Chronic cholecystitis (calculous and non-calculous). It is characterized by a long course, with periodic increase and attenuation of symptoms.
The acute form of biliary inflammation often progresses to the chronic stage. As a result of a long course, purulent foci and nodular formations appear in the tissues, then irreversible changes in the structural tissues occur.
Symptoms and signs
The symptomatic picture of the disease depends on the severity of the inflammatory process, the age of the patient and the frequency of exacerbations. The predominant symptom is usually pain in the right hypochondrium, spreading to the back and central abdominal area. If the inflammation affects the diaphragm, pain may occur in the right arm and shoulder blade.
Additional signs:
- Tension in the abdominal muscles.
- Severe weakness, fatigue.
- The appearance of cold sweat.
- Nausea and vomiting.
- Lack of appetite.
- Loose stools.
- Bloating.
- Cardiopalmus.
- Dyspnea.
- Low blood pressure.
- Yellowing of the skin and mucous membranes.
- Substernal pain.
Due to insufficient intake of vitamins and minerals in the body, symptoms such as pale skin and constant fatigue occur. As complications develop, more severe pathological signs appear. If you have prolonged sharp abdominal pain and persistent fever, you should seek medical help as soon as possible.
You need to see a doctor
- If there is pain in the right hypochondrium (abdominal pain). In chronic cholecystitis, the pain is dull, aching, lasting from several hours and days to several weeks. A characteristic feature of pain in chronic cholecystitis is its occurrence or intensification after eating fatty or fried foods. In chronic cholecystitis, pain from the right hypochondrium spreads upward to the right shoulder and neck. Often, against the background of a dull aching pain, the patient notes short attacks of acute cutting pain, characteristic of exacerbation of chronic cholecystitis.
- With vomiting, which is a less constant symptom of chronic cholecystitis and, like pain, occurs mainly after the patient violates the dietary regimen. In addition to vomiting, patients with chronic cholecystitis may experience prolonged nausea, a bitter or metallic taste in the mouth, and decreased appetite.
- If you are worried about bloating, constipation and diarrhea, these are quite common symptoms of chronic cholecystitis, indicating a gradual deterioration of its function and a disorder of the digestive process. Bloating, diarrhea, or constipation are rarely caused by chronic cholecystitis alone. As a rule, in patients with more or less long experience of this disease, there is a parallel disorder of the function of the stomach and pancreas (gastritis and pancreatitis), which also affects the quality of digestion.
- Patients with advanced cholecystitis may experience severe weakness, a predisposition to frequent colds, decreased performance, and irritability.
Diagnostics
A gastroenterologist can prescribe the necessary examinations for the patient. During the appointment, the doctor will ask the patient about complaints and study anamnestic information. A physical examination may reveal jaundice, bloating, and tenderness in certain areas of the body. Based on the data received, the doctor will prescribe the necessary instrumental and laboratory tests.
Necessary diagnostic procedures:
- Ultrasound examination of the gallbladder and bile ducts. The advantages of the method are safety and real-time imaging of organs. The doctor can immediately detect stones in the gallbladder, changes in the walls of the organ and other pathological signs indicating cholecystitis.
- Blood tests to identify inflammatory and infectious processes. With severe inflammation in the blood, the number of leukocytes increases. Also a diagnostic criterion is the concentration of liver enzymes.
- Collecting bile from an organ using duodenal intubation. The specialist sends the resulting material to the laboratory to detect pathogenic microflora.
- X-ray contrast examination of the gallbladder (cholecystography). The doctor receives information about the size, shape and functional activity of the organ. Using this study, you can detect anatomical abnormalities, gallstone disease or other ailments.
If the doctor is unable to make a diagnosis after requesting the results of the listed tests, an additional gastroscopy, computed tomography or survey laparoscopy may be prescribed. It is necessary to determine the cause of inflammation as accurately as possible.
Treatment
For chronic cholecystitis, the main treatment method is a special diet that reduces the negative impact on the organ. Medications may be prescribed to eliminate infection and inflammation. If the disease causes dangerous complications, such as gallbladder gangrene or peritonitis, surgical intervention is necessary.
Main purposes:
- Therapy with a therapeutic diet. The patient needs frequent small meals. It is necessary to avoid constant consumption of fatty foods, alcohol, beans and fried meat. The diet should be followed for a long time to prevent relapse of the disease. When the gallbladder is removed, patients are prescribed a lifelong diet.
- Antibiotics and anti-inflammatory drugs. For chronic infection, it is recommended to obtain a sample of the microflora by probing and select an effective antimicrobial agent using a laboratory test.
- Antispasmodics and pain relievers to relieve symptoms.
- Choleretic medications. Medicines in this group are used to improve the excretion of bile into the duodenum.
Doctors include removal of the gallbladder or removal of stones blocking the ducts of the organ as the main methods of surgical treatment of cholecystitis. Severe complications of the disease may require complex open surgery in the abdominal cavity.
Features of the treatment of constipation in diseases of the gallbladder
Treatment of constipation that develops against the background of the above-mentioned diseases requires an individual comprehensive approach, which may include the following measures:
- nutrition correction (compliance with therapeutic diet No. 5 and 5a);
- organizing an optimal drinking regime (you should drink about 1.5–2 liters of clean water per day);
- increase in physical and motor activity;
- therapeutic exercises;
- massage;
- physiotherapeutic procedures (electrical stimulation of the intestine - exposure to electric current, during which the intestine contracts, simulating natural urges);
- drug therapy. May include taking laxatives, as well as drugs that enhance the formation of bile (choleretics) and stimulate the contractile function of the gallbladder (cholekinetics).
Up to contents