Acute calculous cholecystitis is an inflammatory pathology of the gallbladder with the formation of insoluble calculi (stones) in its cavity. This disease is one of the varieties of the pathological process of the human hepatobiliary system, it is called cholelithiasis (GSD). Therefore, the diagnosis often sounds like cholelithiasis, calculous cholecystitis. Pathology with the formation of stones is a fairly common process; it occurs mainly in women of working age.
Etiology (causes)
Stones that form in the lumen of the gallbladder are insoluble compounds. They are mineral salts, bacterial cells, bile salts, they are glued together by thick mucus. The process of their formation is provoked by various reasons, as well as provoking factors, these include:
- Hereditary predisposition.
- Gender – in women, the metabolic processes of the liver are different, so the produced bile has a thicker consistency and is prone to the appearance of sediment.
- Poor nutrition - eating at different times, indulging in fatty, fried foods, and alcohol provoke changes in the chemical composition of bile.
- Increased body weight, which affects the intensity of metabolic processes in the liver, as well as the state of bile.
- Chronic inflammatory process of the mucous membrane of the hepatobiliary system, leading to disruption of the processes of secretion and concentration of bile.
Cholelithiasis, calculous cholecystitis can develop over a long period of time, and the stones increase in size. Also, their number may vary.
Diet for cholecystitis
Diet No. 5, recommended for patients with cholecystitis, includes:
- Eating in fractional portions 5-6 times a day. It has been proven that this pattern of eating improves the flow of bile and normalizes the functioning of the gallbladder. In this case, the patient must follow a daily routine - eat at the same time.
- Consumption per day is from 85 to 90 g of proteins (half of which should be vegetable), from 70 to 80 g of fat (1/3 should be of vegetable origin), from 300 to 350 g of carbohydrates (no more than 90 g of sugar).
- Consume less than 10 g of salt per day.
- Drink about 2.5 liters of clean water per day.
- Complete abstinence from alcoholic beverages.
- Eating warm food (hot and cold are not recommended).
The calorie content of the diet of a patient with cholecystitis should be from 2100 to 2500 kcal. But, if the patient is overweight, these figures are calculated individually.
What not to eat if you have cholecystitis
Persons who have been diagnosed with cholecystitis must be from:
- meat, fish and mushroom broths;
- muffins, pastries, fried pies;
- smoked and canned products;
- fatty meats;
- milk, sour cream and high-fat cream;
- boiled eggs;
- sorrel, spinach, garlic;
- chocolate, cocoa, coffee;
- lard
Products allowed for cholecystitis
The list of products allowed for inflammation of the gallbladder includes:
- yesterday's bread (preferably rye or wheat);
- baked pies made from savory dough;
- low-fat lactic acid products;
- milk and vegetable sauces;
- egg white omelette;
- bananas and apples;
- oatmeal, buckwheat and semolina porridge;
- olive and butter;
- non-acidic baked fruits;
- marshmallows in small quantities, marshmallows, natural honey.
Calculous cholecystitis - symptoms
Manifestations of pathology of the gallbladder, structures of the hepatobiliary system with the appearance of stones have characteristic symptoms, they include:
- Feeling of heaviness, pain in the area where the liver is located (right hypochondrium).
- Disruption of the digestive process, which consists of decreased appetite, unstable stools, and bloating.
- Development of jaundice - the skin, mucous membranes, and sclera of the eyes become jaundiced, the intensity of which depends on the severity of the increase in bilirubin. Such jaundice is mechanical; it is provoked by a violation of the outflow of bile from the hepatobiliary system due to blockage by a stone.
- Hepatic colic is a characteristic symptom; it is provoked by the displacement of stones, damage to the mucous membrane by their edges, as well as spasm of the structures of the biliary tract.
The pathology can have a long course with unexpressed clinical manifestations. This is chronic calculous cholecystitis, its course can last from six months or longer.
Diagnosis and treatment of acute cholecystitis
Why does acute cholecystitis remain a pressing problem in general surgery? What are the auxiliary diagnostic methods? What is the modern management of patients with acute cholecystitis?
Acute cholecystitis still remains a pressing problem in modern emergency surgery, especially geriatric surgery, since mainly elderly and senile people are ill and undergo surgery.
Among patients in general surgical departments of a clean profile, acute cholecystitis is the most common pathology, occurring at the level of acute appendicitis and even exceeding it (in our clinic this disease is found in 20-25% of the total contingent of patients in the pure department).
In terms of the absolute number of deaths, acute cholecystitis exceeds acute appendicitis, strangulated hernias, and perforated gastroduodenal ulcers, only slightly inferior to acute intestinal obstruction. The overall postoperative mortality rate varies in various institutions within the range of 2-12%, does not tend to decrease and reaches 14-15% during operations at the height of an attack, and in elderly people - 20%, increasing sharply with age. During emergency operations in patients over 80 years of age, postoperative mortality exceeds 40-50%, which makes these operations extremely risky [1, 2, 3, 4].
At the same time, planned and delayed operations performed against the background of subsided acute inflammatory phenomena, after a comprehensive examination and preparation of patients, give significantly better results. Postoperative mortality in such cases reaches 0.5-1% for some surgeons.
The most common pathology is acute calculous cholecystitis as the most common manifestation of cholelithiasis. Acalculous processes occur in the practice of emergency surgery in no more than 2-3% of cases - these are mainly vascular lesions of the gallbladder in people with widespread atherosclerosis, diabetes mellitus, etc.
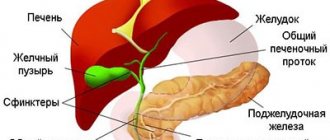
More than half (up to 60%) of patients suffer from localized forms of purulent-destructive inflammation of the gallbladder without involvement of the bile ducts and other organs of the hepato-pancreato-duodenal zone in the pathological process. Literature data and our 25 years of experience, covering many hundreds of radiopaque, ultrasound and endoscopic studies of the biliary tract at the height of an attack of the disease, indicate that acute cholecystitis is almost always acute obstructive (occlusive) cholecystitis caused by blockage of the cervical segment of the bladder with stones or cystic duct. The factor of acute occlusion with disconnection of the gallbladder from the ductal system is leading in the pathogenesis of progressive inflammatory destruction of the bladder wall, since the resulting intravesical hypertension and disruption of the physiological drainage of the organ lead to acute disturbances of microcirculation in its wall, primarily in the mucosa, with the development of its necrosis, phlegmonous and through gangrenous changes in the wall with subsequent perforation. This process develops especially quickly against the background of a virulent enterogenous infection.
At the same time, elderly and senile patients are characterized by a particularly early and rapid development of the purulent-necrotic process in the wall of the bladder, and the clinical picture of the disease does not always allow a correct assessment of the form of the inflammatory process, since there is often no parallelism between the clinical manifestations and morphological changes in the wall of the bladder and abdominal cavities. There are often cases when, with very weak and erased clinical manifestations of the disease, the surgeon finds pronounced destructive changes in the bladder during the operation with developing peritonitis. All of the above forces us, on the one hand, to constantly adhere to the tactics of active surgical treatment of the disease, taking into account the rapidity of development of destructive changes in the gallbladder, and on the other hand, to take into account the high risk of forced emergency operations at the height of an attack in severe somatic patients.
This tactic is based on the early use of modern highly informative methods for objective diagnosis of the pathological process in the gallbladder and abdominal cavity, followed by active therapeutic measures and can be presented in patients without jaundice in the form of the following system. Only patients with signs of widespread peritonitis are operated on urgently - in the first hours after admission, at any time of the day or night. In this case, the process is verified laparoscopically if necessary.
The remaining patients undergo intensive conservative treatment during the first day, aimed at stopping the inflammatory process and restoring the natural outflow of contents from the gallbladder. As part of this treatment, an emergency ultrasound is performed, which provides objective information about the size of the gallbladder, the condition of its walls and lumen, the presence of stones and perivesical complications.
If the conservative treatment has a positive effect and the ultrasound picture is calm, the patient continues to undergo conservative treatment and a comprehensive examination, against which the indications for delayed or planned surgical treatment are clarified.
In the presence of clinical (palpable tense painful gallbladder) and ultrasound signs (large tense gallbladder with thickened stratified walls with or without the presence of stones in the cavity) of destructive cholecystitis and the ineffectiveness of short conservative treatment, somatically unburdened patients under 60 years of age undergo urgent surgery in the first 24 -48 hours of stay in the department.
If the same symptoms are present in elderly and senile patients, as well as in younger, but somatically burdened patients, urgent laparoscopy is performed at the same time, allowing an objective visual assessment of the condition of the gallbladder and abdominal cavity. If laparoscopy reveals signs of massive through destruction of the bladder wall, patients undergo emergency surgery.
In the absence of massive through necrosis of the bladder wall, at the first stage of treatment, a transparietal decompressive puncture of the gallbladder is performed under laparoscope control, removing the liquid contents, washing the bladder cavity and introducing an anti-inflammatory medicinal mixture containing an antibiotic, hydrocortisone and contrical into the cavity of the emptied, washed bladder. Manipulation, as a rule, gives a quick therapeutic effect: pain disappears, body temperature and leukocytosis normalize, and the gallbladder contracts.
With effective decompressive puncture, most patients undergo the second stage of treatment—delayed cholecystectomy—after five to seven days. The interval between these stages is used for intensive examination and preparation of patients for surgery.
The most severely elderly and senile patients with high (IV-V degrees) surgical and anesthetic risk do not undergo surgery after effective puncture decompression of the gallbladder. They undergo intensive conservative treatment under dynamic clinical and ultrasound control. It is this, the most severe contingent of patients, that has a particularly high probability of postoperative mortality during forced emergency operations at the height of an attack, and for them the ability to avoid surgery is tantamount to saving life.
The operation of choice in the vast majority of cases is cholecystectomy. Only in very rare cases, in the most severely elderly patients with a high surgical and anesthetic risk, in case of insufficient effectiveness of puncture decompression of the gallbladder, cholecystomy is performed under local anesthesia.
This differentiated tactics of active surgical treatment of elderly and senile patients has been developed, implemented and carried out in the clinic since 1974, when we first proposed and performed therapeutic transparietal decompressive puncture of the gallbladder under laparoscope control for acute destructive cholecystitis and established its high effectiveness in relieving acute cholecystitis. attack of the disease.
Our many years of experience in performing this manipulation indicate that the most effective and safe puncture of the bladder is performed on the second or third day of the development of an attack of the disease, when there is persistent occlusion of the cervical segment and sufficient thickness and inflammatory infiltration of the bladder wall. The manipulation ends with laparoscopic drainage of the subhepatic space, especially in the presence of local peritonitis. A puncture microcholecystostomy is necessary only if there are signs of biliary (ductal) hypertension.
Puncture is not effective if there is no liquid content in the bladder, if its cavity is tightly filled with stones, or if the bladder is wrinkled, which is usually detected by preliminary ultrasound. Puncture is technically difficult in the presence of perivesical infiltrate, which happens when it is performed at a later stage (more than three days) in the development of the disease. The puncture is dangerous due to the possible subsequent leakage of bile into the abdominal cavity when the slightly changed bladder wall is punctured, which happens when the manipulation is performed too early. Taking into account all these data, we consider it mandatory to participate in every emergency laparoscopic examination of a surgeon, who, together with the endoscopist, resolves all issues related to the therapeutic component of the study.
The use of such two-stage treatment tactics made it possible to reduce the number of the most dangerous emergency operations by six times and significantly reduce overall and postoperative mortality, which in some years dropped below 2%.
Over the past five years, the clinic has treated 1,463 patients with acute cholecystitis, 44% of them underwent surgery, the rest were discharged after effective conservative treatment. This surgical activity (44-46%) for acute cholecystitis has been stable over the past 15 years. Among the discharged patients, many were fundamentally indicated for planned surgical treatment, which was not performed for various reasons.
The predominant patient population is female – 81%. At the same time, 30% of the deaths were men. In terms of age, 67% of the operated patients were over 60 years old, including 32.5% over 70 years old and 6% over 80 years old.
Among the operated patients, almost all belong to the group with late admission (more than 24 hours from the onset of a painful attack). This means that this time is lost for active conservative treatment.
99% of patients had calculous cholecystitis, while over 2/3 (67.5%) had destructive forms of inflammation (phlegmonous, gangrenous, perforative, ulcerative changes in the bladder wall). 15% of those operated on had peritonitis of varying extent and 6% had ductal pathology detected during surgery (without jaundice).
Urgent ultrasound diagnostics were performed in 98.8% of patients, usually the next day after admission. Moreover, only in 3% of cases, during the initial examination, the acalculous nature of the disease was mistakenly established, which was refuted by repeated examinations or surgery.
Urgent laparoscopic examination, as a rule, after ultrasound, was subjected to 39% of patients, of which 70% underwent therapeutic decompressive puncture of the gallbladder with a positive effect. None of these patients required emergency surgery. 68% were operated on in a delayed and planned manner, and 32% were not operated on - they were discharged after the process had completely subsided or transferred to other departments for the treatment of severe concomitant pathology.
In total, among the operated patients, only 7.5% underwent emergency operations, the rest underwent delayed and planned operations.
Of particular interest are the data of bacteriological examination of cystic and ductal bile, performed in 76% of operated patients. 70% of the crops were sterile and only 30% showed growth of flora - most often E. coli. Only in one case was St.aureus sown and in four cases - St.epidermidis. in three of them in association with E. coli. Thus, it is possible that acute cholecystitis often begins as an aseptic process with the development of aseptic necrosis of the bladder wall in conditions of cystic hypertension, followed by infection during a prolonged attack.
Over the past 5 years, 25 people out of 651 operated patients died from acute cholecystitis in the clinic - the average postoperative mortality was 3.8%. Among the dead, only 12% are under 60 years old, the remaining 88% are over 60 years old, including 50% over 70 years old, 30% over 80 years old, 12% over 90 years old.
All the deceased had severe destructive forms of bladder damage due to calculosis, while 17 of the 25 deceased had intra-abdominal perivesical complications (peritonitis, abscesses) and 9 had severe ductal pathology (choledocholithiasis, cholangitis) in combination with peritonitis.
After emergency operations at the height of the attack, 14 out of 25 died, after delayed operations - 11, of which 10 had severe ductal pathology. At the same time, in the clinic there is practically no mortality during planned operations for uncomplicated calculous cholecystitis.
Of the 25 deaths, 16 died from non-surgical causes (acute disorders of cerebral and coronary circulation, severe pneumonia, etc.).
9 people died from complications of the underlying disease. Thus, deaths occurred mainly in elderly and senile people who suffered from severe complicated forms of cholelithiasis and multiple organ concomitant pathologies, which were often the main cause of death, more often after emergency operations forcedly performed at the height of an attack of the underlying disease. Literature 1. Pantsyrev Yu. M., Lagunchik B. P., Nozdrachev V. I. // Surgery. 1990. No. 1. P. 6-10. 2. Tagieva M. M. // Surgery. 1998. No. 1. P. 15-19. 3. Fedorov V.D., Danilov M.V., Glabai V.P. Cholecystitis and its complications. Bukhara, 1997, p. 28-29. 4. Shulutko A.M., Lukomsky G.I., Surin Yu.V. et al. // Surgery. 1989. No. 1. P. 29-32.
Treatment
After diagnosing the pathology using ultrasound and other methods of visualizing stones, therapy is carried out. It is aimed at surgical removal of stones. Depending on their size, number, nature of the edges, surgery can be performed using open access through an incision in the anterior abdominal wall, as well as laparoscopic techniques (a gentle access method with removal of stones). Also, depending on the severity of the pathology or the presence of complications, stones or the entire gallbladder are removed.
Diagnosis of the disease
“If you are experiencing similar symptoms, we advise you to make an appointment with your doctor.
You can also make an appointment by phone. The source of inflammatory processes is pathogenic microorganisms that penetrate through the lymph or hematogenously into the gallbladder and disrupt the outflow of bile. Diagnosis of cholecystitis aims to determine the type of pathology - the treatment regimen depends on this.
To make an accurate diagnosis, a series of studies are carried out:
- Ultrasound of the gallbladder - allows you to detect stones, determine the shape, size, contractile function;
- Biochemical blood test;
- FGDS (gastroscopy).