1.What is gallbladder cholesterosis?
Gallbladder cholesterosis
(CHP, synonyms “lipoidosis”, “lipoid cholecystitis”) is the accumulation and deposition of fats (in particular, the fatty alcohol cholesterol) in the mucous wall of the gallbladder, which leads to disturbances in its peristalsis and, as a consequence, to general dysfunction of the biliary system, and also promotes the formation of calculi (“gallbladder stones”).
The pathogenetic mechanisms of cholesterosis are not completely clear at the moment; research is ongoing, but most sources interpret CLD as a disorder of lipid metabolism (metabolism, processing and absorption of fats). There are focal and diffuse forms of cholesterosis
;
diffuse, in turn, is divided into reticular, polypous and mixed
.
A must read! Help with treatment and hospitalization!
A.A. Ilchenko Central Research Institute of Gastroenterology, Moscow
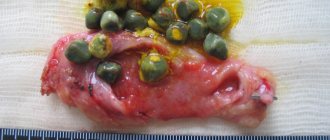
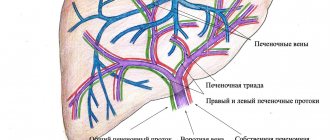
General issues of pathology Gallbladder cholesterosis is a metabolic disease characterized by the deposition of cholesterol mainly in the wall of the gallbladder. Among hyperplastic cholecystosis, gallbladder cholesterosis is the most common pathology. Despite the fact that gallbladder cholesterosis (GC) by R. Wirhov was described back in 1857, for a long time this pathology was little known to practicing doctors and was considered a rare and difficult to diagnose disease. Interest in the problem of chronic gallbladder disease has especially increased in the last decade, when it was possible to clarify the etiopathogenetic mechanisms of the disease and propose effective diagnostic methods. This served as an impetus for the development of management tactics and treatment methods for such patients. The detection rate of CVD, according to various authors, varies within extremely wide limits - from 3-5% to 50% or more. This fact can be explained by several reasons. Firstly, by methods of diagnosing CVD (macroscopic or histological assessment of surgical material or autopsies, various informativeness of instrumental research methods). Secondly, targeted research aimed at identifying not only easily diagnosed forms, but also the initial manifestations of the disease. There is also conflicting information about the frequency of detection of various forms of CVD. This is due to the fact that before surgery, as a rule, polypous forms are diagnosed, which are easier to detect compared to other forms. While in the general population of patients with chronic gallbladder disease, this form is much less common compared to others. The source of lipids accumulated in the gallbladder wall is predominantly modified low-density lipoproteins (LDL), which has been proven in in vitro studies. Modification of LDL can occur under the influence of various factors both in the blood plasma and in endothelial and smooth muscle cells. As a result, changes occur in the LDL apoprotein. These changes lead to a loss of affinity for B and E receptors, but the ability to interact with macrophage receptors (“scavenger receptors”, “garbage collectors”) is acquired [1]. Modified small LDL particles are more easily included in endocytosis and, faster than other LDL, penetrate into the gallbladder tissue, where, along with oxidized lipoproteins, they are intensively captured by macrophages and participate in the formation of foam cells. As the cell becomes overloaded with cholesterol, the synthesis and function of the macrophages' own LDL receptors ("scavenger receptors") freezes. A decrease in the contractile function of the gallbladder (GBL) with preserved absorption capacity of the walls is an additional mechanism for the formation of GBL. Moreover, despite the progression of the pathological process in CLP, there was no noticeable decrease in the absorption capacity of its mucous membrane. An increase in the absorption capacity of the gallbladder wall in chronic bile ducts is facilitated by a decrease in the concentration of bile acids and the FA/PL ratio, as well as an increase in the cholesterol/PL ratio in bile, leading to the predominance of the vesicular form of cholesterol transport. There are reticular, polypous and polypous-mesh forms of CZP (SF CZP, PF CZP, PSF CZP) (Fig. 1). Macroscopic yellowish formations on the surface of the mucous membrane of the gallbladder, upon histological examination, turn out to be nothing more than the tips of the villi, in the apical part of which there are clusters of foam cells (Fig. 2), visible through the single-layer epithelium. Clinical manifestations of chronic gallbladder disease are nonspecific and do not allow differentiating it from other chronic diseases of the gallbladder. The existing symptoms of chronic bile duct disease are caused by the addition of cholecystitis, dysfunction of the biliary tract, or the addition of cholecystolithiasis. According to ultrasound data, the frequency of combination of CP with cholecystolithiasis is 20-70% and depends on the age, gender of patients and the form of CP. It has been reported that CGD can regress with age, and therefore the clinical symptoms disappear [2]. The main method for diagnosing CVD is ultrasound. The mesh form of gallbladder gallbladder on ultrasound is determined in the form of areas of uneven thickening of the gallbladder wall with echo-positive inclusions in the form of a dotted line. Visualization of areas of cholesterosis improves when the intensity of the ultrasound signal decreases, with polypositional and intercostal scanning, and when the gallbladder contracts after a choleretic breakfast. Among other forms of CVD, according to our data, the mesh variant is the most common (Fig. 3). A similar trend persisted when analyzing surgical material from 500 cholecystectomies. Morphological examination revealed the most frequently reticular form of cholesterosis (71.8%), and the least common was the polypous form (8.6%) [3]. The polypous form of CGD is the most easily diagnosed and is characterized by the presence of single or multiple parietal non-displaceable formations, without a distal acoustic shadow (Fig. 4). Analysis of the ultrasound picture and data from a morphological study of the surgical material showed that out of 500 patients who underwent cholecystectomy, according to our data, in not a single case with focal or diffuse damage to the gallbladder wall was malignant growth detected. This fact is difficult to overestimate, since it justifies a more restrained approach to the choice of surgical treatment for CHD and narrowing the indications for cholecystectomy. Ultrasound criteria for the diagnosis of gallbladder gallstones are quite accurate not only for diagnosing cholesterosis, but also for making a differential diagnosis with another gallbladder pathology similar in ultrasound picture.
Tactics for managing patients with CP The introduction of high-resolution ultrasound devices into widespread clinical practice has made it possible to achieve not only significant success in the diagnosis of CP, but, most importantly, has made it possible to identify the features of the clinical course of the disease. This required the development of new approaches to the management of patients with CHD, first of all, the development of tactics for the management of such patients. Dynamic observation (from 1 to 10 years) of patients with chronic gallbladder disease, including those with the polyposis form of the disease, provided serious justification for the choice of wait-and-see management, which should currently be recognized as dominant. Literature data and our own experience of long-term follow-up of patients with various forms of CLD allowed us to develop and recommend the following tactics for managing such patients (Fig. 5). The main provisions of expectant management are: dynamic ultrasound observation with assessment of macroscopic changes in the wall of the gallbladder and the nature of the intravesical contents and, on this basis, determining indications for conservative or surgical treatment. Patients with the reticular form of CGD are subject to dynamic ultrasound monitoring 1-2 times a year with monitoring of the level of total cholesterol and LDL in the blood. If necessary, symptomatic therapy and correction of lipid metabolism are carried out. Patients with polypous and polypous-mesh forms of CGD are also subject to dynamic ultrasound monitoring every 6 months. Such patients can undergo conservative therapy using bile acids, antispasmodics and other medications aimed at relieving the clinical symptoms of the disease and correcting lipid disorders. Therapy is carried out under the control of the levels of AST, ALT, total cholesterol, HDL and LDL in the blood. If there are negative dynamics (an increase in the number of polyps and their size), the issue of surgical treatment should be decided. An ultrasound picture that does not exclude a neoplastic process or the lack of a positive effect from conservative therapy for 6-12 months is also an indication for cholecystectomy.
Treatment For a long time, the only treatment method for CHD was cholecystectomy. This circumstance was explained by the fact that the main method of diagnosing the disease was an x-ray examination, which was not very informative and, at best, made it possible to identify polypous forms of CGD. Difficulties in interpreting such polypoid formations using X-ray contrast examination of the gallbladder did not always make it possible to interpret the identified pathological changes as benign; therefore, the doctor’s opinion almost always leaned towards surgical intervention. The results of long-term dynamic observation of patients with CGD, advances in the study of the processes of bile formation and bile excretion, including in pathological conditions, as well as clarification of the pathogenesis of CGD, made it possible to substantiate the possibility of using pathogenetic therapy for cholesterosis of the gallbladder. The first results of studying the effectiveness of conservative therapy for chronic pancreatitis are quite encouraging, but at present they cannot yet be considered sufficiently successful. Conservative therapy for chronic gallbladder disease should begin with dietary recommendations, advice on restructuring skills and nutritional culture, developing adequate eating behavioral reactions, controlling body weight, and giving up bad habits. The importance of nutrition as a risk factor for cholelithiasis has been well studied in gallstone disease. There are no similar studies for gallbladder cholesterosis. However, given the unidirectionality of lipid metabolism disorders in these diseases, it can be assumed that dietary recommendations developed for patients with cholelithiasis will be useful and can be used for cholesterosis of the gallbladder.
Dietary recommendations. Patients with CGD are recommended to eat fractional meals with a daily protein content of 15-20%, fats - 30%, carbohydrates - 50-55%. Allowed: dishes from lean meats - chicken (boiled, without skin), chicken, veal, rabbit meat; low-fat varieties of sausage (dietary, doctor's, etc.), beef sausages and sausages; low-fat sea and river fish - flounder, cod, pike perch, pike, etc. From dairy products: milk, low-fat kefir, low-fat cheese and cottage cheese, yogurt. All fresh and frozen vegetables and fruits, green peas, corn, beans, dried apples, dried apricots, and prunes are recommended. Bread made from wholemeal flour or with the addition of bran, porridge from oats, rice, buckwheat, rolled oats. Drinks: weak tea, coffee, mineral water, fruit juices. It is recommended to limit sweets, confectionery, and ice cream. Dishes made from fatty and fried meat, lard, butter, duck and goose dishes, pates, whole and condensed milk, sour cream, fatty cheeses and sausages, egg yolks, and strong coffee are prohibited. For overweight people, a low-calorie diet is recommended, and to increase energy expenditure, increased physical activity is recommended. Dietary recommendations are of particular importance in the elderly, 75% of whom have some kind of nutritional disorder, of which about 20% overeat, and 55% eat irrationally [4].
Indications and contraindications for conservative treatment. There are no clearly developed indications for conservative treatment for CVD. This is due, in our opinion, to two reasons. On the one hand, it is difficult to assess the effectiveness of treatment using ultrasound in various types of damage to the gallbladder wall, for example, in the mesh form of gallbladder gallbladder. On the other hand, sufficient clinical experience has not been accumulated indicating the effectiveness of conservative therapy both for different forms of CP and using different treatment regimens. At present, it should be recognized that the main indication for the use of conservative treatment is polyposis and polyposis-mesh forms of CGD. There is no clear certainty regarding the selection of patients for conservative treatment depending on the number and size of cholesterol polyps. According to some authors, the number of cholesterol polyps should not exceed 5, since under this condition it is possible to more clearly control the dynamics of the pathological process with ultrasound. Others believe that the number of polyps does not matter, since the effectiveness and duration of conservative treatment depends only on the size of the polyps. In our opinion, the number of polyps is not of fundamental importance for determining indications for conservative treatment. Firstly, damage to the gallbladder wall during cholesterosis is a dynamic process. Along with the appearance of new polyps, their spontaneous amputation may also occur. In this regard, the disappearance of some polyps can be regarded as a positive effect of treatment. Secondly, with multiple polyps, it is not always possible to count all polyps with great accuracy. And yet, one should be very careful in determining indications for conservative treatment for multiple polyps and a widespread process that covers all the walls of the gallbladder. This is due not only to the difficulty of assessing the dynamics of the pathological process during treatment, but also to the greater possibility of combination with other focal lesions of the gallbladder wall, including adenomatous polyps that require surgical treatment. An important criterion for determining indications for conservative treatment is the size of cholesterol polyps. Currently, a point of view has been formed that patients whose polyp sizes do not exceed 1 cm can be subjected to conservative treatment. This is justified by the fact that larger polyps more often have an adenomatous structure and, therefore, are more likely to become malignant. Until now, the subject of debate is the advisability of conservative treatment for chronic liver disease complicated by cholecystolithiasis. Given this course of the disease, most researchers consider it advisable to perform cholecystectomy in the presence of gallstones. However, our own observations of patients with cholecystolithiasis and analysis of the results of conservative treatment of such patients allows us to conclude that the presence of stones in the gallbladder, regardless of the form of cholesterosis, is not a contraindication to conservative treatment. When selecting patients for conservative treatment, the state of the contractile function of the gallbladder should also be taken into account. The selection criteria are the same as for cholelithiasis: the rate of emptying of the gallbladder after a choleretic breakfast should not be less than 30%. Thus, based on the above, we can formulate contraindications to conservative treatment for chronic gallbladder disease: • polypous form of cholesterosis with multiple polyps and a widespread process that covers all the walls of the gallbladder, especially in people over 60 years of age; • the presence of polyps with a diameter of more than 1 cm; • impossibility of making a differential diagnosis in order to exclude malignant lesions of the gallbladder; • reduced contractile function of the gallbladder (emptying rate less than 30%). The purpose of conservative treatment for cholesterosis of the gallbladder: • relief of clinical symptoms; • regression or stopping the progression of the pathological process in the wall of the gallbladder, elimination of dyscholia; • elimination of secondary dysfunctions of the gallbladder and biliary tract; • correction of lipid disorders; • treatment of concomitant diseases of the gallbladder (cholecystitis), pancreas (pancreatitis) and small intestine, especially with localization of the pathological process in the terminal section.
To relieve dyspeptic disorders, it is necessary to use drugs that normalize the motor-evacuation function of the upper digestive tract and biliary tract. Prokinetics (metoclopramide, domperidone, cisapride, mebeverine, etc.) play a leading role in the treatment of dyspeptic disorders. Drugs in this group improve motor function, mainly of the proximal gastrointestinal tract. Long-term use of metoclopramide (Cerucal) for chronic pancreatitis is impossible due to the development of side effects. Domperidone (Motilium) is more preferred, which is almost free of the side effects characteristic of metoclopramide. The drug has a more pronounced antiemetic effect compared to metoclopramide, and therefore is especially effective in relieving nausea. For bloating, meteospasmil, 1 capsule 3-4 times a day. The cause of pain in chronic gallbladder disease is secondary dysfunction of the gallbladder and sphincter apparatus of the biliary tract. To relieve biliary colic and abdominal pain, various smooth muscle relaxants are used - myotropic antispasmodics. Anticholinergic drugs (atropine, platyphylline, metacin, belladonna preparations, antispasmodic, etc.) are widely used, which block muscarinic receptors of the cell membrane, resulting in a decrease in the intracellular calcium concentration, which ultimately leads to relaxation of the myocyte. Anticholinergic drugs are contraindicated in the presence of concomitant diseases: glaucoma, prostate adenoma, and also during pregnancy. To relieve biliary colic and abdominal pain in chronic bile ducts, other antispasmodics are also used (drotaverine - 1-3 tablets orally or 2-4 ml intramuscularly; papaverine orally 0.04-0.06 g 3-5 times a day or IM - 1-2 ml of 2% solution 2-4 times a day; bencyclane orally 100-200 mg 1-2 times a day for 3-4 weeks, then maintenance doses - 100 mg 2 times a day ). It should be kept in mind that these drugs have a generalized effect on all smooth muscle, including blood vessels and the urinary tract, which may limit their use in CKD. The antispasmodic effect of these drugs is quite weak and short-lived, which in some cases requires increasing the dose and taking them again. Accumulated information about the mechanisms of action of bile acid preparations in cholecystolithiasis suggests their effectiveness in chronic bile duct disease. Bile acid preparations for cholesterosis of the gallbladder are used in the same doses as for dissolving cholesterol gallstones: CDCA in a daily dose of 15 mg/kg body weight, UDCA - 10 mg/kg body weight. The results of our own observation of 74 patients with polypous and polypous-reticular forms of chronic bile duct [5] showed that the effectiveness of ursotherapy depends on the number and size of polyps, the timing of treatment, as well as the nature of macroscopic changes in the gallbladder bile. In patients with single CP, the frequency of complete dissolution of polyps is statistically significantly higher compared to patients with multiple CP. In the presence of homogeneous bile in the gallbladder, the effectiveness of ursotherapy during treatment up to 1 year was the highest and amounted to 95.8% (complete dissolution of all CP was found in 12.5%, part of CP - in 41.7%, reduction - in 41, 7%; no effect was obtained - only in 4.2% of cases). While in the presence of heterogeneous bile and suspension of microlites it amounted to 80%, clots or thick heterogeneous bile - 54.2%, putty-like bile - was minimal and did not exceed 37.5%. The frequency of CP dissolution increases with increasing duration of treatment and reaches its maximum value after 10-12 months of treatment [6]. Recent studies have shown that with chronic liver disease, morphological changes are detected in the hepatocyte, indicating a violation of lipid metabolism. Moreover, they can be minimal in the form of moderately expressed fatty infiltration or severe, up to the development of steatohepatitis, which requires appropriate drug correction. In this regard, the combined preparation of herbal origin Gepabene (contains 275 mg of fume extract and 70-100 mg of milk thistle extract) deserves attention. Previous studies have shown that Gepabene has a choleretic effect and improves the contractile function of the gallbladder. Considering the hepatoprotective effect and the ability to influence dyscholia, the drug can be used in chronic bile ducts, which are characterized by the secretion of lithogenic bile with the formation of biliary sludge, as well as in situations where these disorders are combined with pathological changes in the liver caused by lipid metabolism disorders (fatty liver, steatohepatitis). We have experience in treating 32 patients with various forms of CGD with Gepabene [7]. Patients received Gepabene 1 capsule 3 times a day for two weeks. Analysis of clinical symptoms showed that after 2 weeks of treatment, pain was relieved in most patients and dyspeptic disorders disappeared. Ultrasound examination showed an increase in the volume of the gallbladder in 76.5% of patients (on average by 7 ml), which indicated an increase in choleresis. Half of the patients showed an increase in the rate of gallbladder emptying (minimum by 3%, maximum by 50%). In all patients, according to ultrasound, signs of heterogeneous bile disappeared, and in some patients, biliary sludge. As an independent therapy, the drug is indicated for patients with a reticular form of chronic bile duct and biliary sludge in the form of a suspension of hyperechoic particles (microlites). Experience shows that therapy with Gepabene within 1 to 3 months can completely eliminate biliary sludge. Choleretic preparations of plant origin have a certain stabilizing effect on the colloidal properties of bile, normalize motor-tonic disorders of the biliary tract, improve the clinical course of the disease, but their effect on the regression of cholesterol polyps requires further study. Currently, these drugs for chronic gallbladder disease can be used as additional means of symptomatic therapy or as a maintenance course of treatment after the dissolution of cholesterol polyps with bile acid drugs. According to L.A. Zvenigorodskaya et al., in patients with ischemic heart disease and hypercholesterolemia, CGD is detected in 63.7%. Treatment with simvastatin at a daily dose of 20 mg for 4 weeks improved the course of IHD, reduced the manifestations of hypercholesterolemia, but did not affect the course of CVD [8]. Ursotherapy in the combination of CLD with cholesterol cholecystolithiasis has a more pronounced effect on cholesterol stones (CP) compared to cholesterol polyps. Thus, the average rate of regression of CP occurring independently during 1-3 months of treatment was 1.6 mm, 4-6 months – 2.0 mm, 7-9 months – 2.4 mm, 10-12 months – 2.8 mm . While in the case of a combination of CVD with cholecystolithiasis, they turned out to be lower and amounted to 1.2 mm, 1.8 mm, 2.2 mm and 2.4 mm, respectively, at the same time. At the same time, the rate of regression of stones in this group turned out to be higher than the rate of regression of CP in both groups and amounted to 2.8 mm, 3.2 mm, 4.6 mm, 6.5 mm, respectively. The long-term results of conservative therapy for chronic pancreatitis have been little studied. According to some reports, the recurrence rate of cholesterol polyps is approximately 10% per year and differs little from similar indicators after successful litholytic therapy for cholelithiasis. However, as our own experience shows, repeated courses of therapy with bile acid preparations in such cases can achieve a positive effect in a much shorter time compared to previous treatment.
Surgical treatment. It should be recognized that there is no consensus regarding the indications for surgical treatment for cholesterosis of the gallbladder. Proponents of cholecystectomy justify their position by the fact that accurate diagnosis of the disease before surgery is difficult [9], conservative therapy does not always achieve the desired results, requires long-term treatment and significant economic costs, and in some cases may be accompanied by side effects [10, 11]. Opponents of cholecystectomy justify their opinion by the fact that removal of the gallbladder solves only part of the problems associated directly with the pathology of the gallbladder, while after the operation dyslipidemia, dyscholia and clinical manifestations remain due to the pathological process of damage to the biliary tract, primarily the sphincter apparatus of the large duodenal papilla. Analyzing various approaches to the treatment of patients with chronic gallbladder disease, we can conclude that in recent years there has been a clear trend towards narrowing the indications for cholecystectomy. This was to a certain extent facilitated by new information about the pathogenesis of the disease, improvement of diagnostic methods, which made it possible to monitor the course of the pathological process in dynamics, as well as accumulated clinical experience in the management and conservative treatment of patients with chronic gallbladder disease. Indications for surgical treatment. Based on our own experience and literature data, we consider it possible to offer the following indications for surgical treatment for CP: 1. The difficulty of making a differential diagnosis between CP and the neoplastic process. 2. Negative dynamics, according to ultrasound, for 6 months (increase in the number and size of polypoid formations, changes in their shape and structure). 3. Attacks of biliary colic, including during ursotherapy. 4. Cholecystolithiasis – multiple stones, the total volume of which exceeds 1/4 of the volume of the gallbladder or single stones more than 1 cm in diameter (regardless of the presence or absence of clinical symptoms). 5. Decreased contractile function of the gallbladder with a gallbladder emptying rate of less than 30% (regardless of the form of chronic gallbladder disease). 6. Lack of effectiveness from conservative therapy for 6-12 months. 7. Concomitant chronic cholecystitis and pancreatitis. Clinical observations of patients after cholecystectomy show that in some patients, dyspeptic disorders and pain decrease or disappear after surgery, including in patients without cholecystolithiasis. Improvement in clinical symptoms is observed in 50-95% of cases and depends on the ejection fraction of the gallbladder and the state of the sphincter apparatus of the biliary tract before surgery [12-14]. In some cases, in patients with acalculous pancreatitis, cholecystectomy leads to an improvement in clinical symptoms, especially with frequent exacerbations of pancreatitis [15].
References 1. Zhang N., Yang Y., Steinbrecher UP Structural reguirments for the binding of modified proteins to the scevenger receptor of a macrophages // J. Biol. Chem. 1993; 268:5535-42. 2. Huegel A., Helpap B. Morphologische und klinische Aspekte der Cholezystosen // Chir. Praxis. 1988; 39 (1): 39-48. 3. Ilchenko A.A., Morozov I.A., Khomeriki S.G., Orlova Yu.N. Gallbladder cholesterosis: A guide. M.: GEOTAR-Media, 2007; 232. 4. Povorinskaya O.A., Karpenko O.M. Basic principles of nutrition for elderly patients // Handbook of a practical doctor. 2010; 3:25-30. 5. Ilchenko A.A., Orlova Yu.N. The effectiveness of ursodeoxycholic acid in cholesterosis of the gallbladder // Ther.arch. 2003; 2: 35-38. 6. Ilchenko A.A., Orlova Yu.N. Experience with the use of ursodeoxycholic acid for cholesterosis of the gallbladder // Hepatology. 2004; 3:22-27. 7. Ilchenko A.A., Orlova Yu.N., Bystrovskaya E.V. Clinical effectiveness of Gepabene in biliary pathology. IX Russian National Congress “Man and Medicine” April 8-12, 2002, M.: Abstracts of reports. 181. 8. Zvenigorodskaya L.A., Ovsyannikova O.N., Firsakova V.Yu. Treatment of patients with hypercholesterolemia and cholesterosis of the gallbladder with lipid-lowering drugs. Materials of the 6th Slavic-Baltic scientific forum “St. Petersburg Gastro-2004”. Gastroenterology of St. Petersburg. 2004; 2-3. M50. 9. Damore LJ, Cook CH, Fernandez KL et al. Ultrasonography incorrectly diagnoses gallbladder polyps // Surg. Laparosc. Endosc. Percutan. Tech. 2001 Apr; 11 (2): 88-91. 10. Khairy GA, Guraya SY, Murshid KR Cholesterolosis. Incidence, correlation with serum cholesterol level and the role of laparoscopic cholecystectomy // Saudi Med J. 2004 Sep; 25 (9): 1226-8. 11. Jones-Monahan KS, Gruenberg JC, Finger JE et al. Isolated small gallbladder polyps: an indication for cholecystectomy in symptomatic patients // Am. Surg. 2000 Aug; 66 (8): 716-9. 12. Salmenkivi K. Cholesterolosis of the gallbladder // Acta chirurgica scand. 1964; 324:1-93. 13. Kmiot WA, Perry EP, Donovan IA et al. Cholesterolosis in patients with chronic acalculous biliary pain // Br. J. Surg. 1994 Jan; 81 (1): 112-5. 14. Jones DB, Soper NJ, Brewer JD et al. Chronic acalculous cholecystitis: laparoscopic treatment // Surg. Laparosc. Endosc. 1996 Apr; 6 (2): 114-22. 15. Parrilla Paricio P., Garcia Olmo D., Pellicer Franco E. t al. Gallbladder cholesterolosis: an aetiological factor in acute pancreatitis of uncertain origin // Br. J. Surg. July 1990; 77 (7): 735-6.
2. Symptoms of the disease
There is still no consensus on whether cholesterosis should be considered an independent disease or considered in the context of more general cholecystopathy. Indeed, the clinical manifestations of cholesterosis
very similar to the symptoms of biliary dyskinesia or cholecystitis:
- discomfort or dull pain in the right hypochondrium that occurs after eating (especially acute);
- dyspepsia (“upset stomach”);
- paroxysmal pain in the right hypochondrium (considered a more or less specific symptom of cholesterosis, but can also be a consequence of blockage of the duct with a stone).
Sometimes cholesterosis occurs latently
, without any tangible manifestations.
Statistics
It is generally accepted that cholesterosis affects mainly women of young and mature age (over 35 years old).
with increased body weight, prone to excessive unhealthy eating.
Visit our Hepatology page
Possible complications
The negative consequences of cholesterosis develop rarely and are associated with neglect of the symptoms of the disease and lack of treatment. Possible complications include:
Signs of atherosclerosis of the aorta and heart
- accumulation of calcium in the walls of the bladder - calcification of the walls;
- atherosclerosis;
- cholecystitis;
- liver cholestasis;
- development of cholelithiasis;
- bacterial overgrowth syndrome;
- anemia;
- weight loss or obesity, others.
Some of these factors relate to both possible causes of the disease and complications. This is due to the lack of definitive research into cholesterosis.
3.Diagnosis of the disease
Considering the unclear etiology and the lack of clear nosological criteria, as well as the frequent combination of cholesterosis with cholelithiasis and biliary dyskinesia, the diagnosis of CGD can cause certain difficulties. Usually a set of clinical tests is prescribed, but in most cases it is possible to clarify the clinical picture (differences in the thickness of the gallbladder membrane) only with the help of hardware diagnostic methods:
- radiography;
- Ultrasound of the gallbladder;
- magnetic resonance cholangiography.
Often, cholesterosis is diagnosed only by the results of surgery on the gallbladder (cholecystotomy, cholecystectomy) or at autopsy.
About our clinic Chistye Prudy metro station Medintercom page!
4.Treatment of cholesterosis
Therapy for cholesterosis is usually included in a set of measures aimed at treating dyskinesia:
- a diet with minimal cholesterol and an emphasis on vegetable oils;
- fractional meals;
- choleretic drugs;
- antispasmodics, analgesics (in the presence of pain);
- drugs that restore the natural balance of acids and cholesterol;
- antibacterial agents (if an infection is diagnosed).
In the case of severe and treatment-resistant symptoms, as well as in the presence of severe comorbid (concomitant) diseases (stones, polyposis, etc.), the treatment of choice is cholecystectomy
– removal of the gallbladder.
In most cases, the prognosis is favorable.
Diet
Diet is an important part of the treatment of cholesterosis, necessarily complementing drug treatment. In medical terminology, it is called table No. 5. The basic principles of nutrition for gallbladder damage are the following:
- you can eat: vegetable soups, boiled chicken and beef, porridge with water, sweet fruits, wheat bread, low-fat dairy products, weak tea, herbal infusions, dried fruit compote;
- you need to eat often, but little by little;
- take additional vitamins;
- drink at least 1 liter of clean water;
- don't overeat.
The diet during surgical treatment is prescribed individually. For the first few days before and after surgery, nutrition is strictly limited; table No. 5 is used 1–2 weeks after the start of the recovery period.