General information
Pancreatic necrosis (necrosis of the pancreas) is a destructive disease of the pancreas, which is a serious complication of acute or chronic pancreatitis .
The ICD-10 code for pancreatic necrosis is K86.8.1. A characteristic feature of this formidable disease is the gradual necrosis of pancreatic tissue. This is a very dangerous diagnosis that poses a threat to human life. The death of this organ occurs due to the fact that the pancreatic tissue is dissolved by the enzymes that it itself produces. As a rule, this process is combined with other pathological phenomena - inflammatory processes, infection, etc.
This disease is the most severe complication of pancreatitis. As a rule, it affects young people of working age. According to medical statistics, this disease accounts for about 1% of all recorded cases of acute abdomen. However, the number of cases of this disease has been increasing recently. The high mortality rate with pancreatic necrosis is also alarming - it is 30-80%. Therefore, it is extremely important to diagnose the disease in a timely manner and begin adequate treatment immediately.
Symptoms of the disease
Symptoms of the development of the disease in the pancreas directly depend on the speed of necrotic processes and on the individual characteristics of the body. If we talk about the primary signs of necrosis, then this is pain that can occur in both the left and right hypochondrium. Moreover, it is always encircling in nature and can spread to the shoulder area or ribs.
The nature of pain can be different - pronounced or insignificant. At the same time, as medical practice shows, moderate pain during the development of necrotic processes occurs in only 6% of patients, severe pain in 40%, and unbearable pain is observed in 50% of patients, and in most of them necrosis is accompanied by the development of collapse.
Many patients confuse the pain that occurs during necrosis with the pain that occurs during a heart attack. But their main difference is that during necrotic processes, the painful sensations become less pronounced if you take a sitting position, bend your knees and press them to your stomach. In the case of a heart attack, this position of the body does not bring relief.
And speaking about what other signs of pancreatic necrosis have, the following should be highlighted:
- temperature increase;
- vomit;
- pale or red skin;
- the appearance of bluish spots on the sides of the abdominal cavity;
- feeling of bloating;
- increased gas formation;
- unpleasant sensations when pressing with fingers on the anterior part of the peritoneum.
The appearance of unexplained bruises on the sides of the abdomen is the main sign of necrosis
As a rule, severe symptoms are characteristic of extensive pancreatic necrosis, mild symptoms occur mainly with focal necrosis.
Important! When the first signs of pancreatic necrosis occur, you must call an ambulance! If the patient does not receive timely treatment, the consequences can be very different.
Pathogenesis
The basis of the pathogenesis of pancreatic necrosis is a failure in the mechanism of internal protection of the pancreas from the influence of pancreatic enzymes that destroy it. If a person drinks alcohol heavily and constantly overeats, external secretion increases significantly, the ducts of the gland are stretched, and the outflow of pancreatic juices is disrupted.
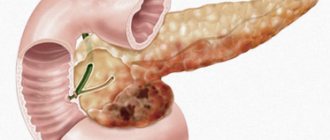
Necrosis of the pancreas develops against the background of pancreatitis - an inflammatory process of the pancreas, in which the death of part or the entire organ often occurs.
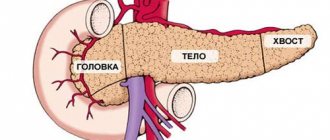
The pancreas is an organ important for the normal functioning of the body. Its main functions are the production of the main enzymes involved in digestion, as well as the regulation of blood sugar due to the production of the hormones insulin and glucagon . Accordingly, dysfunction of this organ leads to serious disturbances in the general condition of the body.
When a person feels hungry, juices and enzymes are transported through the connecting duct into the small intestine, which ensures enzymatic processing of food. Pancreatic fluid acts on the acidic environment of gastric juice, neutralizing it. In the intestines, digestive enzymes break down and process substances.
The pancreas produces the main digestive enzymes:
- lipase – breaks down fats;
- amylase – converts starch into sugar;
- chymotrypsin , trypsin - are involved in the breakdown of proteins;
- glucagon , insulin , polypeptide , etc.
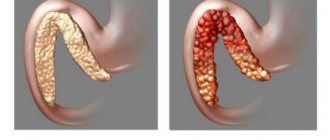
If in healthy people the enzymes produced by the pancreas are active directly in the digestive tract, then in patients with damage to the ducts of the gland, the enzymes directly affect the pancreas. Against the background of increased pressure inside the ducts, edema of the parenchyma develops, the acini of the pancreas are destroyed, and proteolytic enzymes are activated prematurely. As a result, the gland “poisons” itself. Due to the activation of lipase, necrosis of fat cells occurs, under the influence of elastase, blood vessels are destroyed, and activated enzymes, as well as breakdown products, end up in the bloodstream. In this case, there is a toxic effect on all tissues and organs. First of all, damage occurs to the liver, kidneys, heart, and brain.
With pancreatic necrosis, three stages of tissue death are determined:
- Toxemic - toxins of bacterial origin appear in the blood, the gland actively produces enzymes.
- Development of an abscess - a purulent inflammatory process of tissues and organs that surround the pancreas develops.
- Purulent changes in tissues - if purulent sepsis develops, immediate surgical intervention is required, as this condition is life-threatening.
Clinical manifestations of chronic pancreatitis
Manifestations of chronic pancreatitis depend on its form, stage, duration of development, complications encountered, and concomitant diseases.
The leading clinical symptom is pain. It occurs due to the development of increased pressure in the pancreatic ducts, or due to the development of pancreatitis-associated neuritis. The mechanisms of pain are described above, but it is worth noting that the spread of pain is associated with the involvement of the nerve plexuses, which are located between the lobules of the gland, in the inflammatory process, as well as pressure on them from the enlarged inflamed gland or pseudocysts.
Most often, at the beginning of the disease, the only complaint is pain above the navel
, it may bother you for several years. The pain is of a girdling nature, it can be debilitating, constant, or it can be paroxysmal and recurring. It can radiate to the back, to the left shoulder blade and shoulder, to the left side of the chest, and less often to the right. However, cases of pain radiating to the iliac and groin region, as well as to the genitals, have been described. The connection with food is of particular importance - pain appears after every meal, especially sour, spicy, salty, as well as those that stimulate bile secretion, for example, yolk, fat. Patients do not tolerate alcohol well.
Much later, digestion is disrupted: various dyspeptic disorders, steatorrhea, pancreatogenic diarrhea, insufficiency of intestinal absorption, malabsorption syndrome appear, which occurs due to insufficient production of enzymes in the pancreas. A person loses weight, becomes weaker, and calcifications appear in the pancreas. Little insulin is produced, which leads to secondary diabetes mellitus.
Classification
Depending on the predominance of damaging mechanisms, three forms of the disease are determined:
- Adipose – with increased lipase activity, pancreatic adipose tissue is destroyed. After lipase appears outside the pancreatic capsule, it acts, provoking the appearance of areas of necrosis in the layers of the peritoneum, the greater and lesser omentum, the mesentery, and internal organs. aseptic peritonitis and multiple organ failure subsequently develop .
- Hemorrhagic - with increased elastase activity, microcirculatory disorders predominantly develop, resulting in vasospasm . For a short time - several days, and sometimes hours - toxemia provokes paresis of the vascular wall, vasodilation, and blood flow in the gland tissues slows down. This leads to a sharp increase in the likelihood of blood clots and, later, ischemic necrosis . Initially, the vascular wall is destroyed thicker than the pancreas, and later in other organs. The consequence of all these processes is hemorrhage into the retroperitoneal tissue and internal organs. The main symptom that characterizes hemorrhagic pancreatic necrosis is effusion into the abdominal cavity with the presence of blood in it. The disease develops rapidly, so in doctors’ reports you can often see the conclusion: “The cause of death is hemorrhagic pancreatic necrosis.”
- Mixed - with approximately the same activity of elastase and lipase, the signs of fat necrosis and hemorrhagic imbibition are equally pronounced.
Depending on the prevalence of pathological manifestations, two forms are defined:
- local (one area affected);
- diffuse (two or more areas are affected).
Depending on the rate of progression:
- progressive;
- sluggish.
Depending on the depth of the lesion:
- surface;
- deep;
- total.
Depending on the course of the disease:
- recurrent;
- progressive;
- retrogressive;
- fulminant;
- abortive.
Depending on the severity of the manifestations of the disease, several of its degrees are determined:
- Mild degree - as a rule, this is edematous or diffuse necrosis with small foci.
- Medium degree - diffuse or local with more pronounced foci.
- Severe degree - diffuse or total with large foci.
- An extremely severe stage - pancreatic necrosis is accompanied by complications leading to irreversible consequences and death.
Causes
A number of factors that provoke necrotic processes in pancreatic tissues are determined:
- regular excessive consumption of alcohol;
- constant overeating, abuse of smoked, fried and fatty foods;
- peptic ulcer;
- gallstones;
- the presence of abdominal injuries and previous surgical interventions in this area;
- severe infectious diseases.
Under the influence of these factors, pancreatic dysfunction can develop, which leads to pancreatitis and pancreatic necrosis. But, as a rule, pancreatic necrosis manifests itself against the background of occasional alcohol intake. Studies have confirmed that in most cases, pancreatic necrosis developed after an episode of drinking alcohol in very large quantities.
Causes of development of chronic pancreatitis
Depending on the causes, primary
and
secondary
.
To understand the mechanism of development of pancreatitis, it should be noted that the pancreas constantly produces enzymes for better absorption of protein, fatty and carbohydrate foods (proteases, nucleases, lipase, amylase) - the excretory function of the gland. In total, about 1.5 liters of pancreatic juice are secreted per day. The enzymes produced in the gland are in an inactive state until they leave the pancreatic ducts and enter the duodenum. There, under the influence of food and bile, they become active and participate in the absorption of food.
Under some pathological conditions, enzyme activation occurs in the tissues of the pancreas itself. Its “self-digestion” begins, resulting in areas of necrosis and hemorrhage. Inflammation and swelling of the gland tissue occurs. Tissue breakdown products and enzymes enter the blood, poisoning the body. Intoxication affects all systems: cardiovascular, nervous, excretory, liver. Swelling of the small intestine, mesentery, etc. appears.
Beginning of primary
Pancreatitis is usually associated with processes in the pancreas itself, for example, after injury, alcohol abuse, impaired blood supply to the gland, some viral diseases, and narrowing of the main pancreatic duct, which impedes the outflow of enzymes that the gland excretes. It is also believed that primary pancreatitis can develop with a chronic lack of protein nutrition.
In diseases such as cholelithiasis, ulcerative, and diverticular diseases, the pancreas suffers secondarily. At the same time, joint coordinated work on food processing is disrupted. Swelling of the large duodenal papilla, duodenal dyskinesia and duodenostasis, stones in the bile ducts or inflammation in them contribute to the entry of bile, bacteria, emulsified fat into the pancreatic duct, or form a mechanical obstacle to the outflow of pancreatic juice, which leads to increased pressure and destruction walls of the pancreatic ducts. Both factors create conditions for premature activation of enzymes in its tissues, the development of inflammation, necrosis, and hemorrhages.
Chronic pancreatitis is considered to be a polyetiological disease.
The main etiological factors are:
- chronic alcoholism;
- cholelithiasis, choledocholithiasis;
- post-traumatic narrowing or obstruction of the pancreatic ducts;
- exposure to chemicals, including some medications;
- hyperlipidemia;
- insufficient protein nutrition (malnutrition);
- hereditary predisposition (L-antitrypsin deficiency and other genetic factors);
- hyperparathyroidism (hypercalcemia),
- cystic fibrosis (the most common factor in children),
- idiopathic factors.
Alcoholism is recognized as the most common cause of chronic pancreatitis. However, it is known that it occurs only in every 10th person who abuses alcohol. The average period for the development of chronic pancreatitis due to alcohol abuse is 18 years for men and 11 years for women. A typical combination of conditions in which its development actually occurs is good socio-economic living conditions of the patient (Western European countries, Japan, USA), male gender, age over 35 years, high level of daily fat intake, consumption of more than 20 g of alcoholic beverages daily ( in terms of pure ethyl alcohol).
Factors contributing to pancreatic damage include an unbalanced diet. Hereditary (familial) chronic pancreatitis is very rare. The first signs of it appear in children aged 10-12 years. Signs of congenital chronic pancreatitis, in addition to family history, are:
- the occurrence of pain in the upper abdomen in early childhood in the absence of other etiological factors;
- detection of pancreatic calcification;
- a sharp expansion of its ducts with the presence of stones in them.
A more frequent combination of chronic pancreatitis with blood group 0 (I) was noted.
Bile duct stones are a fairly common cause of pancreatitis in the population, mainly in women in Western Europe and North America. CP is combined with cholelithiasis very often, and the disease, caused by the presence of a chronic infection in the biliary tract, occurs in approximately 25% of patients with cholelithiasis. The main reason for the development of chronic pancreatitis in cholelithiasis is the emergence of conditions for the reflux of bile into the pancreatic duct:
- strangulation of a stone in the major papilla of the duodenum;
- trauma and prolonged spasm of the sphincter;
- papillitis or papillostenosis due to frequent injury to the papilla by small stones.
Sometimes the inflammatory process passes from the gallbladder and hepatic ducts directly to the pancreas through the venous and lymphatic vessels.
In diseases that occur with impaired liver function (cirrhosis or chronic hepatitis), bile is secreted, containing a large amount of free radicals and peroxide compounds, which, when entering the pancreatic ducts, themselves can cause an inflammatory reaction, but also stimulate pancreatic enzymes, promoting its “self-digestion”.
In addition, the cause of the development of secondary pancreatitis can be diseases of the duodenum, such as duodenitis, its diverticula and ulcerative deformity. In these diseases, as a result of inflammation or deformation in the duodenum, pressure increases, the function of the sphincter apparatus of the major papilla is disrupted, which is aggravated if a papillotomy was previously performed. Under such conditions, duodenal contents are thrown into the pancreas and bile ducts, pancreatic enzymes inside the gland tissue are activated, and the process of tissue destruction begins.
The development of chronic pancreatitis may be a direct consequence of perforation (penetration) of a gastroduodenal ulcer in the pancreas.
A number of drugs can have a damaging effect on the pancreas:
- corticosteroid drugs (“steroid pancreatitis”, “steroid diabetes”);
- ACTH;
- estrogens and estrogen-containing contraceptives;
- diuretics, etc. when taken for a long time.
Pancreatitis also develops with an overdose of drugs containing calcium and vitamin D. The use of chemotherapy drugs, metronidazole, nitrofurans in some cases leads to the development of chronic pancreatitis.
Disruption of arterial blood supply creates conditions for the formation of some forms of CP. If it develops in a young person aged 19 to 20 years and the cause cannot be determined, then this variant of the disease is called idiopathic.
Symptoms of pancreatic necrosis
Signs of this disease may appear several hours or days after the influence of factors provoking the disease has been noted.
The main symptom is pain manifested in the left hypochondrium. Also, pain can radiate to the sides, back, and be felt in the pit of the stomach. The pain is constant, quite intense or moderate. It can be encircling, radiating to the shoulder, scapula, so a person may have the impression that a heart attack . The pain becomes stronger after the patient eats. This may cause nausea and repeated vomiting. Pancreatic necrosis without pain is impossible.
The following symptoms of pancreatic necrosis are also likely:
- redness of the skin, as due to damage to the pancreas substances that dilate blood vessels enter the blood;
- flatulence is a consequence of rotting and fermentation in the intestines;
- bluish or purple spots on the abdomen, buttocks and sides - the so-called Gray-Turner symptom ;
- gastrointestinal bleeding is a consequence of the destructive effect of enzymes on the walls of blood vessels;
- temperature increase;
- tension of the anterior abdominal wall, pain on palpation;
- dry mucous membranes, skin, thirst are a consequence of dehydration;
- decreased blood pressure ;
- confusion, delirium.
The disease, as a rule, begins acutely, and most often patients associate its first signs with excessive alcohol consumption and a significant violation of the diet. Doctors testify that most of these patients are admitted to hospitals while still intoxicated, which confirms the rapid development of pathological changes in the gland. There is a direct relationship between the severity of pain and the severity of necrosis. If destructive changes spread to the nerve endings, this leads to a gradual decrease in the severity of pain. But this sign, combined with intoxication, is quite alarming in terms of prognosis.
After pain appears, after some time the patient begins to experience vomiting. She is difficult to tame and does not bring relief. The vomit contains blood clots and bile. Due to constant vomiting, dehydration develops, which leads to dry skin and a coated tongue. Diuresis gradually slows down. Flatulence, stool and gas retention are noted. These symptoms are accompanied by fever .
Due to fluctuations in glucose levels, toxemia and hyperfermentemia, the brain is affected and encephalopathy . If the inflammatory process progresses, the pancreas increases significantly in size. An infiltrate forms in the abdominal cavity. This condition is life-threatening for the patient.
Acute pancreatitis and pancreatic necrosis
Acute pancreatitis is a condition requiring emergency treatment. If qualified assistance is not provided on time, a life-threatening condition – pancreatic necrosis – may develop.
- The main reason
It is generally accepted that pancreatitis most often develops in people who abuse alcohol. This is wrong. If a person drinks alcohol regularly every day, the pancreas adapts to this effect, and it takes a serious boost for inflammation to occur. Most often, pancreatitis develops in those who have drunk low-quality alcohol. A common story: with acute abdominal pain, which later turns out to be pancreatitis, a young man is admitted to the hospital, who was having fun somewhere, celebrating something and at some point drank an unknown alcoholic drink.
- Mechanism of development of pancreatitis
The secretion of the pancreas contains enzymes that facilitate the digestion of food and is an aggressive substance. Inflammation begins due to the fact that the pancreas suddenly needs to produce a large amount of secretion. This happens when certain foods enter the gastrointestinal tract: a person ate fatty foods, or drank alcohol - or ate fatty foods and washed them down with alcohol. The main pancreatic duct opens into the ampulla of the major duodenal papilla. The common bile duct also opens into it. The sphincter of the duodenal papilla (sphincter of Oddi) doses the release of secretions into the duodenum. If a lot of pancreatic secretion is suddenly released, but it cannot exit into the intestine due to the fact that the sphincter does not open so often, the pancreas becomes overfilled with secretion and inflammation develops. The gland is divided into the head, isthmus, body and tail. Inflammation begins from the head of the pancreas - from its initial sections.
- Symptoms
The first symptom of acute pancreatitis is pain in the epigastric region - in the solar plexus area. The pain is not acute, but constant, aching, nagging. It is annoying and oppressive in nature. The patient cannot find a body position that would alleviate the situation. This pain often radiates to the back, lower back. Dyspeptic symptoms develop - nausea, vomiting, repeated loose stools. Due to painful shock, tachycardia occurs, blood pressure decreases, and cold sticky sweat appears.
- Emergency help
The situation when a patient develops the above symptoms is an emergency. If you experience symptoms of acute pancreatitis, you do not need to take medications on your own. Also, you don’t need to think that these are “hunger” pains and eat them, hoping for relief. It won't get better, it will only get worse. You should immediately call an ambulance or go to the emergency department of a hospital.
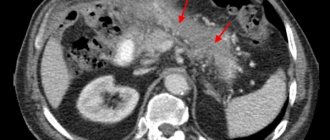
Ilyinskaya Hospital is ready around the clock to provide emergency care to patients with acute pancreatitis. First of all, an ultrasound examination of the abdominal cavity will be performed to detect swelling of the pancreas and dilation of the main pancreatic duct. To clarify the diagnosis, a computed tomography scan of the abdominal organs is performed. A biochemical blood test is promptly performed to confirm that the patient actually has pancreatitis (amylase increases).
Acute pancreatitis is a surgical disease; therapists do not deal with it. If a patient with acute pancreatitis comes to the Ilyinsk hospital on time, he is hospitalized in a hospital and therapy is immediately started, the task of which is to reduce the swelling of the pancreatic tissue. Special anti-inflammatory drugs and antispasmodics are used.
- Pancreatic necrosis
One of the most dangerous complications of acute pancreatitis is pancreatic necrosis. Due to inflammation, edema and impaired blood supply, necrosis of pancreatic tissue occurs. As a result of necrosis, pancreatic secretion begins to enter the abdominal cavity and is absorbed by the peritoneum. In addition, it affects the walls of blood vessels, causing erosive bleeding. Pancreatic necrosis is a life-threatening condition that requires immediate surgical intervention.
- Endoscopic surgery for acute pancreatitis
If, having started conservative therapy, the doctor sees on a control ultrasound that the edema has not decreased, if biochemical blood tests show that amylase does not decrease, the patient’s well-being does not improve, this means that conservative therapy does not give the expected results and there is a risk of developing pancreatic necrosis. In such a situation, surgeons at the Ilyinskaya Hospital perform endoscopic surgery. A special thin and flexible endoscope, a duodenoscope, is inserted through the mouth into the lumen of the duodenum. The surgeon inserts a stent into the main pancreatic duct through the major duodenal papilla. Once the stent is in place, pancreatic secretions can once again flow directly into the duodenum. The pressure in the duct decreases, swelling in the gland decreases, and the development of pancreatic necrosis is excluded. Swelling of the pancreas seriously complicates these delicate manipulations; the surgeon is required to have a filigree command of endoscopic techniques.
- Laparoscopic surgery for pancreatic necrosis
If a patient develops pancreatic necrosis, surgeons at the Ilyinskaya Hospital perform an emergency minimally invasive operation. Through three small incisions (10 mm), a laparoscope and surgical manipulators are inserted into the abdominal cavity. The endoscope camera allows you to examine the pancreas under high magnification and identify foci of necrosis. Necrotic areas of the pancreas are removed, and drains are installed to drain pancreatic juice from the abdominal cavity to the outside.
- Puncture techniques for acute pancreatitis
In acute pancreatitis, pancreatic secretions and other fluids accumulate in the retroperitoneum, worsening the patient's condition. If there are indications, surgeons at the Ilyinskaya Hospital perform a minimally invasive intervention - a puncture with the installation of drains. The puncture is performed under ultrasound guidance. Drains evacuate excess pancreatic secretions, which alleviates the patient’s condition, improves the effect of conservative therapy and avoids a larger volume of surgical intervention.
- Treatment in hospital
Patients with acute pancreatitis and pancreatic necrosis require long-term hospital treatment aimed at eliminating the inflammatory process in the gland. All inpatient rooms at the Ilyinskaya Hospital are single or double. There are no obstacles to relatives visiting the patient at the Ilyinskaya Hospital; visits are available 24 hours a day. All vital indicators of the patient (pulse, pressure, oxygen saturation, etc.) are monitored by special monitors and recorded by an electronic system. To learn more.
After discharge from the hospital, dynamic monitoring of the patient is carried out by his family doctor in collaboration with the operating surgeon and other specialists.
Tests and diagnostics
If you suspect the development of necrosis, you should immediately consult a general practitioner. The specialist conducts an examination and determines the circumstances surrounding the development of the disease. He must palpate and determine the presence, nature and location of pain. If a pathology of the gland is suspected, the patient is examined by an endocrinologist. If tumors are detected on the gland, an oncologist is also involved in the treatment process.
To establish a diagnosis, instrumental and laboratory examinations are prescribed.
Laboratory studies include an extensive blood test, since with necrosis the following pathological changes are noted:
- Increased sugar levels, increased granularity of leukocytes , neutrophils.
- Increased ESR .
- Increased levels of elastase, trypsin, hematocrit as a result of dehydration.
- Increased liver enzymes due to inflammation.
- The development of necrosis is also indicated by an increased level of amylase in the urine.
- In the process of laboratory tests, the state of hormones and digestive enzymes is determined.
Also during the diagnostic process, the following studies may be prescribed:
- Ultrasound examination - to determine the uneven structure of gland tissue, identify cysts, abscesses, fluid in the abdominal cavity, stones in the bile ducts. Ultrasound also makes it possible to analyze the condition of the ducts.
- Magnetic resonance imaging, computed tomography - allow you to determine the foci of disease development, the size of the organ, and also find out whether inflammation is developing, whether there are swelling, abscesses, neoplasms, deformities.
- Angiography of gland vessels.
- Diagnostic laparoscopy.
- Puncture.
A specialist will be able to make a final diagnosis only after receiving data from all prescribed studies.
Treatment with folk remedies
When a patient's pancreatic necrosis worsens, he experiences severe pain. Folk remedies that are used in parallel with the main treatment can help improve the condition a little. But, before practicing such methods, it is necessary to visit a doctor, establish a diagnosis and begin practicing the correct treatment regimen.
- The fruits of Japanese Sophora - a decoction is prepared from them. A spoonful of raw materials should be filled with 1 tbsp. boiling water and leave for 5 hours. Drink warm before every meal. The course of treatment is 10 days.
- Blueberry berries and leaves - a decoction is prepared from them by pouring boiling water over dried or fresh raw materials and boiling for 5 minutes. (2 tbsp. raw materials per 250 ml of water). Drink instead of tea.
- Immortelle herb - a decoction helps relieve pain and inflammation. To prepare the decoction, take 1 tbsp. l. dry herbs and a glass of water, cook for 5 minutes. Strain the resulting broth and drink throughout the day.
- Oat decoction helps relieve irritation and restore organ cells. To prepare the product, you need to soak the grains and wait a few days for them to sprout. Sprouted grains need to be dried and ground. Pour the mixture with cold water (1 tablespoon of oats per 1 glass of water) and leave for about half an hour. You need to drink 2 glasses of this product a day.
- Lemon – helps reduce pain. To do this, boil the lemon in water for 5 minutes, then squeeze the juice out of it and mix with raw yolk. Drink the product on an empty stomach and do not eat for three hours after it. Take it five times a day, once every three days. The course of treatment lasts several months.
- Licorice root - to prepare it you need to take 1 tbsp. l. chopped dry licorice root, the same amount of dandelion and burdock leaves. Pour the mixture with 2 cups of boiling water, drink the infusion hot, half a glass 3-4 times a day.
There are also special herbal mixtures used to treat the pancreas. But it is important to take into account that they bring benefits to the body if such preparations are taken regularly and according to the scheme approved by the doctor. Under no circumstances should you practice self-medication with folk remedies for such a terrible diagnosis as pancreatic necrosis.
Prevention
To prevent pancreatic necrosis, you need to follow some simple recommendations:
- Limit the amount and frequency of alcohol consumption.
- Avoid junk food – fast food, processed foods, soda, and minimize the consumption of fatty and fried foods.
- Do not take medications without a doctor’s prescription, especially do not abuse them.
- Try to create a diet based on natural products, try to practice split meals in small portions.
- Treat cholelithiasis in a timely manner.
- At the first symptoms indicating problems with the pancreas, consult a doctor immediately.
- Follow the principles of a healthy lifestyle.
Necrosis. Definition and reasons
The cause of necrosis is pancreatitis.
What is necrosis or pancreatic necrosis? This is the death of areas or an organ as a whole.
Necrosis is not a clinical diagnosis, since it is not established by the attending physician, but, as a rule, by a pathologist in the morgue.
This condition develops as a complication of the destructive form of pancreatitis.
The cause of the disease is pancreatitis, but the factors causing this pathology can be considered the cause of organ necrosis. What causes this pathology:
- alcohol in high doses and regularly;
- excess fatty and heavy foods in the diet;
- pathologies of the bile ducts;
- surgical intervention on the peritoneal organs.
As a rule, an acute attack of the disease occurs spontaneously after libations and a belly celebration. It is extremely rare that pancreatitis develops due to other reasons:
Diet for pancreatic necrosis
Diet for pancreatic necrosis of the pancreas
- Efficacy: therapeutic effect after 21 days
- Timing: constantly
- Cost of products: 1800-1900 rubles. in Week
Diet Table No. 5p for pancreatitis
- Efficacy: therapeutic effect after 14 days
- Timing: constantly
- Cost of products: 1400-1500 rubles. in Week
In the first days of treatment for this disease, it is necessary to practice therapeutic fasting. The doctor determines its duration individually. Next, you need to adhere to a strict diet, completely eliminating salty, fatty, smoked, sweet, fried foods, as well as alcohol from the menu. The list of prohibited products is quite wide. You cannot consume cabbage, figs, grapes, bananas, bell peppers, onions, garlic, coffee, cocoa, sausages, canned food, fatty fish, soda, mushrooms, jam, fresh bread, egg yolk, ice cream, millet and barley cereals, and baked goods.
During this period, you are allowed to eat the following foods:
- boiled vegetables;
- porridge with water - oatmeal, rice, semolina, buckwheat;
- lean meat - veal, chicken;
- dairy products;
- baked fruits;
- crackers;
- refined vegetable oils – 10 g per day;
- vegetarian soups with potatoes, carrots, zucchini, pumpkin.
Your doctor will help you create the right diet. This diet must be strictly followed for about a month. If the dynamics are positive, the diet is gradually expanded.
Nutrition after surgery should be supervised by a specialist for the first time. Before the operation, the patient does not eat at all. A day after surgery, he is prescribed parenteral nutrition, using special solutions with a complex of nutrients. Such solutions contain fatty acids, amino acids , minerals, and vitamins. About a week after the operation, the patient begins to have food administered through a tube into the stomach.
Then, after some time, the patient gradually switches to a gentle diet, in which carbohydrates are the basis of the diet, and fats are kept to a minimum. Food needs to be chopped and eaten small and little by little. You should not overeat; the menu should include only boiled and steamed food.
Consequences and complications
Pancreatic necrosis is a dangerous disease, and if it develops rapidly, the patient may die within 24 hours after its onset. Whether a person can survive fat necrosis depends on how affected the gland is, how widespread the damage is, and how large the area of edema is.
With pancreatic necrosis, the following consequences are possible:
- rupture of the biliary tract;
- cerebral edema;
- damage to lung tissue;
- bleeding and, as a consequence, decomposition of the pancreas and stomach;
- peritonitis;
- peptic ulcer;
- enzyme deficiency;
- intoxication of the gastrointestinal tract;
- thrombosis of venous arteries;
- pancreatic fistulas;
- pancreatic cyst;
- suppuration in the pancreas;
- state of shock.
In addition, necrosis of the pancreas can lead to diabetes mellitus , rectal or pancreatic cancer.
Prognosis for pancreatic necrosis of the pancreas
It is important to understand that pancreatic necrosis is a very dangerous disease, and, unfortunately, the chances of surviving pancreatic necrosis depend on many circumstances. The likelihood of survival is reduced by old age, delays in seeing a doctor, arterial hypertension in the patient, the presence of other dangerous diseases, etc.
The prognosis for pancreatic necrosis after surgery with timely treatment is as follows: mortality is about 50%. After surgery for severe forms of necrosis, mortality can reach 95%. Therefore, early contact with a doctor increases the chances of successful treatment.
Types of necrotic processes
Like any other disease, pancreatic necrosis has its own classification. Depending on the extent of its spread, this disease is divided into:
- to focal (necrotic processes are observed only in certain areas of the pancreas, for example, in the tail or head);
- extensive (when most of the organ is affected).
According to the speed of development, necrosis can be:
- sluggish (develops slowly);
- progressive (develops very quickly).
Extensive pancreatic necrosis
Based on the type of pathological process, this disease is divided into:
- to hemorrhagic;
- hydropic;
- hemostatic;
- destructive;
- functional.
List of sources
- Dibirov M.D., Yuanov A.A. Pancreatic necrosis. Diagnostic and treatment protocol. Educational and methodological manual. Moscow, 2012, p. 366
- Ermolov A.S., Ivanov P.A., Blagovestnov D.A. and others. Diagnosis and treatment of acute pancreatitis. M., 2013, “VIDR”, p. 382
- Mitryakov P.S. Modern methods of treating patients with pancreatic necrosis // International Journal of Experimental Education. – 2016. – No. 9-2. – P. 221-224;
- Acute pancreatitis (Diagnosis and treatment protocols) / S.F. Bagnenko [and others]; St. Petersburg Research Institute of Emergency Medicine named after. I.I. Dzhanelidze. - St. Petersburg, 2004.
- Savelyev V.S., Filimonov M.I., Burnevich S.Z. Pancreatic necrosis. MIA, 2008, p. 259
- Sakhno V.D., Mainulov A.M., Vlasova N.V., Bochkareva I.V. Necrotizing pancreatitis, treatment protocols. Annals of Surgical Hepatology, 2005, vol. 10, no. 1, p. 107 – 112