III) Mesenteric part of the small intestine
| Mesenteric part of the small intestine (jejunum and ileum), structure, walls, blood supply, innervation. |
The mesenteric part is called by the presence of a mesentery near the jejunum and ileum, which is a double layer of peritoneum, obliquely attached to the posterior abdominal wall along a line from left to right from the second lumbar vertebra to the right sacroiliac joint.
Between the leaves of the mesentery pass the superior mesenteric artery and vein, which are divided into I5-20 intestinal branches, fanning out along the mesentery and interconnected by anastomoses - arcades. In the mesentery, a root 15-17 cm long is identified, which starts from the left surface of the body of the first lumbar vertebra, passes obliquely downwards and ends at the level of the right sacroiliac joint. The space of the lower floor of the abdominal cavity is divided by the root of the mesentery into two mesenteric (mesenteric) sinuses: right and left. They contain horizontally and obliquely 14-16 loops of the jejunum and ileum, covered in front by the greater omentum. The jejunum begins from the duodenum at the duodenojejunal flexure, which lies at the level of the II lumbar vertebra. Its length is 2/5 of the entire small intestine, diameter is 40-45 mm. Without a clear anatomical boundary, it passes into the ileum, which ends in the region of the ileocecal flexure, which is located in the right iliac fossa.
The ileum makes up 3/5 of the total length of the thin intestine, its diameter in the initial section is 30-35 mm, in the final section - 25-27 mm. When the intestine passes into the large intestine, a valve of the same name (valve) appears in the area of the ileocecal opening, formed by two semilunar folds of the mucous membrane and the orbicularis muscle. At 20-60 cm from the ileocecal angle on the ileum there is a Meckel's diverticulum - an embryonic remnant of the vitelline-intestinal duct.
The loops of the jejunum lie at the level of the umbilical and left lateral areas of the abdomen, occupying an almost vertical position in the left mesenteric sinus. The loops of the ileum lie in the right inguinal and lateral regions, located horizontally in the right mesenteric sinus.
The mesenteric part of the small intestine is covered by peritoneum on all sides. Along the line of attachment of the mesentery in the jejunum and ileum, the mesenteric edge is distinguished, through which the straight intestinal vessels, starting from the last vascular arcade, enter the intestine. The opposite edge is called free. Between the edges lie the walls of the intestine - anterior and posterior.
Wall structure
Ø The mucous membrane with the submucosa forms circular folds up to 8 mm high, up to half and 2/3 of the circumference of the intestine, and depressions between them. Over the entire surface of the mucosa there are intestinal villi (4-5 million), 0.2-1.2 mm in length and containing blood and lymphatic microvessels, fibrous and smooth muscle fibers inside. Between the villi lie crypts - narrow cracks. With absorption syndrome, the villi atrophy, causing, as it were, baldness of the mucosa.
Ø In the submucosa there are numerous intestinal glands, lymphoid nodules, which in the ileum are grouped into lymphoid Peyer's patches up to 3 cm long and up to 1 cm wide. In the later stages of typhoid fever, they can become necrotic and cause perforation of the intestine. The membrane contains a submucosal nerve plexus with vegetative nodules and a microvascular plexus.
Ø In the area of the funnel-shaped ileocecal opening, the mucous membrane forms two large horizontal folds: upper and lower, and between them a frenulum when the folds converge at the corners - this is the ileocecal valve (Bauhinian valve).
Ø The muscular layer consists of longitudinal and circular layers that evenly surround the mucosa with the submucosa. The circular muscle layer forms functional sphincters, the ileocecal seal for the valve of the same name. The membrane contains the myenteric nerve plexus with vegetative nodules and the microvascular plexus.
Ø A serous membrane with a subserous base provides intraperitoneal cover. It contains microvascular and fiber nerve plexuses.
The jejunum is supplied with blood from the superior mesenteric artery, which inside the mesentery breaks up into intestinal branches (jejunal and ileal), interconnected by arcuate anastomoses - arcades of several orders. From the last arcades, direct arteries are directed into the intestinal walls, which at the mesenteric edge are divided into anterior and posterior branches, which pass into the microvessels of the membranes. In addition, the ileocecal artery participates in the blood supply to the ileum. The veins of the jejunum and ileum flow through the superior mesenteric vein into the portal vein of the liver.
The afferent lymphatic vessels drain into the superior mesenteric and ileocolic lymph nodes.
Innervation is provided by the lumbar spinal ganglia, branches of the vagal trunks of the vagus nerves and the superior mesenteric plexus.
Age characteristics. The small intestine of a newborn has a length of 1.2-2.8 m. In the first childhood, the length increases to 4.8 m, and by 11-12 years - to 5-6 m (as in adults). Newborns and infants are characterized by a high position of the intestine and contact of its loops with the visceral surface of the liver and the anterior abdominal wall. In old and senile age, the diameter and length of the intestine increases, the height of the folds and villi of the mucous membrane decreases. All parts of the small intestine descend somewhat.
Developmental anomaly - common mesentery of the ileum and cecum. In case of violations of the rotation of the primary intestine, which happens rarely, a complete or partial opposite arrangement of the abdominal viscera is possible - situs viscerus inversus totalis seu partialis. With partial preservation of the vitelline duct (umbilical-intestinal duct), a Meckel's diverticulum is formed on the ileum - 2%.
Hormone-producing cells of the intestinal mucosa secrete secretin, pancreozymin, enterogastrin, cholecystokinin into the blood and lymph - dual-action hormones that work as mediator neuroamines (intermediaries in the transmission of nerve impulses) and as hormones that directly affect the digestive organs. Bombesin, neurotensin - VIP (vasoactive intestinal peptide), substance II, enkephalins are also produced in the mucosa of the small and large intestines, having vascular and neurogenic effects. They are able to control the functioning of the entire digestive system and, in addition, regulate the severity of pain, and create a feeling of pleasure from food taken.
| Large intestine, its sections, their topography, relationship to the peritoneum, wall structure, blood supply, innervation, regional lymph nodes, x-ray image. |
13(III) Large intestine
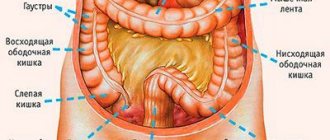
Large intestine - Intestinum crassum is a continuation of the small intestine. It is located along the perimeter of the lower and pelvic floors of the abdominal cavity, bordering the jejunal and ileal intestinal loops with a rectangular frame. Its length is 1-1.7 m, the average diameter is 3-5 cm, in the final section 4-8 cm. Digestion is completed in it and undigested residues are formed into feces. The intestinal glands secrete few enzymes, absorption is limited due to the lack of intestinal villi. The rich microbial flora synthesizes a number of vitamins B and K, necessary for hematopoiesis and other processes, and activates some enzymes.
Distinctive anatomical features:
Ø longitudinal ribbons – teniae coli: mesenteric, omental, free, – teniae mesocilica, teniae omentalis, teniae libera, formed by long smooth muscle bundles;
Ø haustra - haustrae coli - transverse swellings with transverse grooves between them, formed due to the redistribution of longitudinal and circular muscles;
Ø omental processes - appendicis epiploicae - up to 4-5 cm long in the form of finger-like outgrowths of the visceral peritoneum and adipose tissue, located along the free and omental bands;
Ø semilunar folds - plicae semilunaris - of the mucous membrane, forming three longitudinal rows throughout the intestine;
Ø division into sections: initial - cecum, middle - colon: ascending, transverse, descending, sigmoid colon and final section - rectum;
Ø different topographical arrangement of the sections of the large intestine and their different relationship to the peritoneum.
The cecum, caecum, teflos, is 6-8 cm long, 7-7.5 cm in diameter, has a vermiform appendix - appendix vermiformis, which begins at the convergence of three longitudinal ribbons. The intestine and appendix are located in the right iliac fossa, and are covered with peritoneum on all sides. The intestine does not have a mesentery, but the appendix has a mesentery. In the medial wall of the cecum, at the border of its transition to the ascending colon, there is an ileocecal opening, surrounded by the upper and lower semilunar folds of the mucosa with a frenulum at the junction of the folds. Inside the folds, circular muscle fibers form the sphincter. All together makes up the ileocecal valve - valva ileocaecalis - the old name for the Bauhinian valve. Below the ileocecal opening is the opening of the appendix.
The ascending colon, colon ascendens, extends upward from the cecum, is located in the right lateral region, has a length of 15-20 cm. At the visceral surface of the right lobe of the liver, the intestine forms a right (hepatic) bend - flexura coli dextra and passes into the transverse colon. The ascending colon is in posterior contact with the quadratus lumborum muscle, the transverse muscle and the right kidney; medially - with the loops of the small intestine and the psoas major muscle, in front - with the anterior abdominal wall and omentum; laterally - with the lateral abdominal wall, from which it is separated by the right paracolic groove. The peritoneum covers the intestine from the front and sides (mesoperitoneally).
The transverse colon, colon transversum, together with the mesentery - mesocolon divides the abdominal cavity into upper and lower floors, due to its horizontal position. The length of the intestine is 30-83 cm (on average 50 cm) varies due to its arched position, convex upward in the brachymorphic type and convex downward in the dolichomorphic body type. Adjacent to the intestine is the right lobe of the liver, the greater curvature of the stomach (the gastrocolic ligament connects them), the spleen in the area of the left (splenic) bend - flexura coli sinistra. The phrenocolic ligament connects this flexure of the intestine to the diaphragm. The loops of the small intestine are located below, and the duodenum and pancreas are located behind. The intestine is covered with peritoneum on all sides, the mesentery adheres to the posterior abdominal wall, and has good mobility.
The descending colon, colon descendens (12-15 cm) starts from the left (splenic) flexure, goes downwards in the lateral section and in the left iliac fossa passes into the sigmoid colon. Posteriorly, the intestine is adjacent to the left quadratus lumborum muscle, the lower end of the left kidney, and the left iliacus muscle. In front and on the left it comes into contact with the abdominal wall along the left paracolic groove, on the right and medially with the small intestine. The peritoneum covers the intestine from the front and sides (mesoperitoneally).
The sigmoid colon, colon sigmoideum, S-romanum (15-67 cm) in the form of two loops lies in the left iliac fossa from the level of the iliac crest to the sacroiliac joint. It is covered with peritoneum on all sides (intraperitoneal), has a mesentery and has good mobility. Congenital or acquired damage to the nervous apparatus of the sigmoid colon leads to the development of Hirschsprung's disease.
The rectum, rectum, proctos, is located in the pelvic cavity and begins at the level of the III sacral vertebra, average length 15 cm, diameter 2.5-7.5 cm. Posteriorly adjacent to the sacrum and coccyx, repeating their posterior bend. In front, in men it is adjacent to the prostate, seminal vesicles, vas deferens and bladder, in women - with the uterus and vagina. A digital examination of adjacent organs is performed through the rectum. In the perineum, the intestine makes a second bend, but this time anteriorly. The peritoneum covers the beginning of the intestine on all sides, the ampulla on three sides and moving onto the bladder in men it forms a rectovesical notch, in women a deeper rectouterine notch. In the rectum, there are sacral and perineal bends, a supramullary part, an ampulla and an anal canal with an anal opening surrounded by internal and external sphincters.
The structure of the colon wall
Ø A serous membrane with a subserous base is present throughout the cecum, transverse, and sigmoid colons, where the peritoneum provides intraperitoneal cover. In the ascending, descending and rectum, it is replaced along the posterior surface by adventitia, and in the ampulla and anal canal of the rectum, adventitia is present along the entire perimeter.
Ø The muscular layer forms ribbons in a longitudinal layer (except for the rectum), and haustra in a circular layer (except for the rectum). Between the muscle layers there is a powerful muscular-intestinal nerve plexus with autonomic ganglia and a plexus of microvessels. The orbicularis muscles create functional sphincters and the internal anal. The external anal sphincter is formed by striated muscles.
Ø The mucous membrane with the submucosa forms three rows of semilunar folds in the cecum, colon and sigmoid colon; and in the rectum there are large transverse folds in the ampulla and longitudinal anal columns, sinuses, valves in the anus.
Ø The submucosa contains the neurocellular and choroid plexus, tubular intestinal glands, and lymphoid nodules. In the vermiform appendix they merge into groups, which is why the appendix is often called the “tonsil” of the abdominal cavity.
The blood supply to the colon comes from the superior and inferior mesenteric arteries, which with their branches connect in the mesentery of the transverse intestine and form the arterial intestinal circle - an intersystem anastomosis. The ileocecal artery departs from the superior artery to the cecum and appendix, the right colon to the ascending colon, and the middle colon to the transverse. It anastomoses with the left colic branch of the inferior mesenteric artery (Riolan arch) - the old name for the arterial circle of the intestine.
The descending colon, sigmoid colon, and supramullary rectum receive branches from the inferior mesenteric artery: the left colon, sigmoid, and superior rectum. The ampulla and the anal canal rectum are supplied with blood by the middle and lower rectal arteries from the internal iliac artery. An intersystemic arterial anastomosis is formed in the rectum due to the connections between the superior and middle rectal arteries.
The veins of the colon flow into the portal vein of the liver, except for the middle and lower rectal veins, which flow into the inferior vena cava system through the iliac veins. Porto-caval anastomoses in the form of venous plexuses are formed between the rectal veins in the wall of the supramullary part and the ampulla. In the lower third of the ampulla and the anal canal, the plexus is called hemorrhoidal. With varicose veins and thrombosis of the veins of this plexus, hemorrhoids occur.
The afferent lymphatic vessels of the colon enter the nodes - ileocolic, cecal (anterior, posterior, appendicular), mesenteric-colic, sigmoid. From the rectum they flow into other lymph nodes - internal iliac (sacral), subaortic, superior rectal.
The cecum and colon are innervated by branches of the lumbar spinal ganglia and vagal trunks of the vagus nerves, as well as branches of the sympathetic mesenteric plexuses. The sigmoid and rectum receive branches of the sacral spinal ganglia and parasympathetic splanchnic pelvic nerves, inferior mesenteric and hypogastric sympathetic plexuses.
Age characteristics. The large intestine of newborns is short (63-66 cm), does not have transverse swellings (haustra) and omental appendages, the bends are not pronounced, and lies high. The ascending colon is short and underdeveloped. Its intensive formation begins from the 6th month of a child’s life. The transverse colon has a short mesentery - up to 2 cm. In the descending colon, transverse swellings are slightly visible. The sigmoid colon is up to 20 cm long and lies high, distended with original feces - meconium. Its loop is in contact with the cecum, located in the opposite ileal fossa. The rectum of newborns has not yet formed an ampoule; bends and folds of the mucous membrane are not pronounced. It is elongated in length and retains a cylindrical shape throughout.
Haustrae and ribbons in the cecum and colon appear in the 6th month of the thoracic period, and omental appendages appear in the second year of life. All of them are finally formed by the age of 6-7 years. The ileocecal (Bauginian) valve becomes well defined by the age of 3 years. The valve of the appendix begins to form in infancy. At the end of the first year, the length of the colon increases to 83 cm, and at 10 years it is 118 cm.
Developmental anomaly - common mesentery of the ileum and cecum. In case of violations of the rotation of the primary intestine, which happens rarely, a complete or partial opposite arrangement of the abdominal viscera is possible - situs viscerus inversus totalis seu partialis. The developmental defect is atresia of the anus, when the anal membrane does not break through during development.
On a contrast X-ray, the haustra and functional sphincters are clearly visible in the colon; in the rectum - ampoule, canal and relief of the mucous membrane. The general appearance and position of all parts of the colon are clearly visible.
| Mesenteric part of the small intestine (jejunum and ileum), structure, walls, blood supply, innervation. |
The mesenteric part is called by the presence of a mesentery near the jejunum and ileum, which is a double layer of peritoneum, obliquely attached to the posterior abdominal wall along a line from left to right from the second lumbar vertebra to the right sacroiliac joint.
Between the leaves of the mesentery pass the superior mesenteric artery and vein, which are divided into I5-20 intestinal branches, fanning out along the mesentery and interconnected by anastomoses - arcades. In the mesentery, a root 15-17 cm long is identified, which starts from the left surface of the body of the first lumbar vertebra, passes obliquely downwards and ends at the level of the right sacroiliac joint. The space of the lower floor of the abdominal cavity is divided by the root of the mesentery into two mesenteric (mesenteric) sinuses: right and left. They contain horizontally and obliquely 14-16 loops of the jejunum and ileum, covered in front by the greater omentum.
The jejunum begins from the duodenum at the duodenojejunal flexure, which lies at the level of the II lumbar vertebra. Its length is 2/5 of the entire small intestine, diameter is 40-45 mm. Without a clear anatomical boundary, it passes into the ileum, which ends in the region of the ileocecal flexure, which is located in the right iliac fossa.
The ileum makes up 3/5 of the total length of the thin intestine, its diameter in the initial section is 30-35 mm, in the final section - 25-27 mm. When the intestine passes into the large intestine, a valve of the same name (valve) appears in the area of the ileocecal opening, formed by two semilunar folds of the mucous membrane and the orbicularis muscle. At 20-60 cm from the ileocecal angle on the ileum there is a Meckel's diverticulum - an embryonic remnant of the vitelline-intestinal duct.
The loops of the jejunum lie at the level of the umbilical and left lateral areas of the abdomen, occupying an almost vertical position in the left mesenteric sinus. The loops of the ileum lie in the right inguinal and lateral regions, located horizontally in the right mesenteric sinus.
The mesenteric part of the small intestine is covered by peritoneum on all sides. Along the line of attachment of the mesentery in the jejunum and ileum, the mesenteric edge is distinguished, through which the straight intestinal vessels, starting from the last vascular arcade, enter the intestine. The opposite edge is called free. Between the edges lie the walls of the intestine - anterior and posterior.
Wall structure
Ø The mucous membrane with the submucosa forms circular folds up to 8 mm high, up to half and 2/3 of the circumference of the intestine, and depressions between them. Over the entire surface of the mucosa there are intestinal villi (4-5 million), 0.2-1.2 mm in length and containing blood and lymphatic microvessels, fibrous and smooth muscle fibers inside. Between the villi lie crypts - narrow cracks. With absorption syndrome, the villi atrophy, causing, as it were, baldness of the mucosa.
Ø In the submucosa there are numerous intestinal glands, lymphoid nodules, which in the ileum are grouped into lymphoid Peyer's patches up to 3 cm long and up to 1 cm wide. In the later stages of typhoid fever, they can become necrotic and cause perforation of the intestine. The membrane contains a submucosal nerve plexus with vegetative nodules and a microvascular plexus.
Ø In the area of the funnel-shaped ileocecal opening, the mucous membrane forms two large horizontal folds: upper and lower, and between them a frenulum when the folds converge at the corners - this is the ileocecal valve (Bauhinian valve).
Ø The muscular layer consists of longitudinal and circular layers that evenly surround the mucosa with the submucosa. The circular muscle layer forms functional sphincters, the ileocecal seal for the valve of the same name. The membrane contains the myenteric nerve plexus with vegetative nodules and the microvascular plexus.
Ø A serous membrane with a subserous base provides intraperitoneal cover. It contains microvascular and fiber nerve plexuses.
The jejunum is supplied with blood from the superior mesenteric artery, which inside the mesentery breaks up into intestinal branches (jejunal and ileal), interconnected by arcuate anastomoses - arcades of several orders. From the last arcades, direct arteries are directed into the intestinal walls, which at the mesenteric edge are divided into anterior and posterior branches, which pass into the microvessels of the membranes. In addition, the ileocecal artery participates in the blood supply to the ileum. The veins of the jejunum and ileum flow through the superior mesenteric vein into the portal vein of the liver.
The afferent lymphatic vessels drain into the superior mesenteric and ileocolic lymph nodes.
Innervation is provided by the lumbar spinal ganglia, branches of the vagal trunks of the vagus nerves and the superior mesenteric plexus.
Age characteristics. The small intestine of a newborn has a length of 1.2-2.8 m. In the first childhood, the length increases to 4.8 m, and by 11-12 years - to 5-6 m (as in adults). Newborns and infants are characterized by a high position of the intestine and contact of its loops with the visceral surface of the liver and the anterior abdominal wall. In old and senile age, the diameter and length of the intestine increases, the height of the folds and villi of the mucous membrane decreases. All parts of the small intestine descend somewhat.
Developmental anomaly - common mesentery of the ileum and cecum. In case of violations of the rotation of the primary intestine, which happens rarely, a complete or partial opposite arrangement of the abdominal viscera is possible - situs viscerus inversus totalis seu partialis. With partial preservation of the vitelline duct (umbilical-intestinal duct), a Meckel's diverticulum is formed on the ileum - 2%.
Hormone-producing cells of the intestinal mucosa secrete secretin, pancreozymin, enterogastrin, cholecystokinin into the blood and lymph - dual-action hormones that work as mediator neuroamines (intermediaries in the transmission of nerve impulses) and as hormones that directly affect the digestive organs. Bombesin, neurotensin - VIP (vasoactive intestinal peptide), substance II, enkephalins are also produced in the mucosa of the small and large intestines, having vascular and neurogenic effects. They are able to control the functioning of the entire digestive system and, in addition, regulate the severity of pain, and create a feeling of pleasure from food taken.
| Large intestine, its sections, their topography, relationship to the peritoneum, wall structure, blood supply, innervation, regional lymph nodes, x-ray image. |
13(III) Large intestine
Large intestine - Intestinum crassum is a continuation of the small intestine. It is located along the perimeter of the lower and pelvic floors of the abdominal cavity, bordering the jejunal and ileal intestinal loops with a rectangular frame. Its length is 1-1.7 m, the average diameter is 3-5 cm, in the final section 4-8 cm. Digestion is completed in it and undigested residues are formed into feces. The intestinal glands secrete few enzymes, absorption is limited due to the lack of intestinal villi. The rich microbial flora synthesizes a number of vitamins B and K, necessary for hematopoiesis and other processes, and activates some enzymes.
Distinctive anatomical features:
Ø longitudinal ribbons – teniae coli: mesenteric, omental, free, – teniae mesocilica, teniae omentalis, teniae libera, formed by long smooth muscle bundles;
Ø haustra - haustrae coli - transverse swellings with transverse grooves between them, formed due to the redistribution of longitudinal and circular muscles;
Ø omental processes - appendicis epiploicae - up to 4-5 cm long in the form of finger-like outgrowths of the visceral peritoneum and adipose tissue, located along the free and omental bands;
Ø semilunar folds - plicae semilunaris - of the mucous membrane, forming three longitudinal rows throughout the intestine;
Ø division into sections: initial - cecum, middle - colon: ascending, transverse, descending, sigmoid colon and final section - rectum;
Ø different topographical arrangement of the sections of the large intestine and their different relationship to the peritoneum.
The cecum, caecum, teflos, is 6-8 cm long, 7-7.5 cm in diameter, has a vermiform appendix - appendix vermiformis, which begins at the convergence of three longitudinal ribbons. The intestine and appendix are located in the right iliac fossa, and are covered with peritoneum on all sides. The intestine does not have a mesentery, but the appendix has a mesentery. In the medial wall of the cecum, at the border of its transition to the ascending colon, there is an ileocecal opening, surrounded by the upper and lower semilunar folds of the mucosa with a frenulum at the junction of the folds. Inside the folds, circular muscle fibers form the sphincter. All together makes up the ileocecal valve - valva ileocaecalis - the old name for the Bauhinian valve. Below the ileocecal opening is the opening of the appendix.
The ascending colon, colon ascendens, extends upward from the cecum, is located in the right lateral region, has a length of 15-20 cm. At the visceral surface of the right lobe of the liver, the intestine forms a right (hepatic) bend - flexura coli dextra and passes into the transverse colon. The ascending colon is in posterior contact with the quadratus lumborum muscle, the transverse muscle and the right kidney; medially - with the loops of the small intestine and the psoas major muscle, in front - with the anterior abdominal wall and omentum; laterally - with the lateral abdominal wall, from which it is separated by the right paracolic groove. The peritoneum covers the intestine from the front and sides (mesoperitoneally).
The transverse colon, colon transversum, together with the mesentery - mesocolon divides the abdominal cavity into upper and lower floors, due to its horizontal position. The length of the intestine is 30-83 cm (on average 50 cm) varies due to its arched position, convex upward in the brachymorphic type and convex downward in the dolichomorphic body type. Adjacent to the intestine is the right lobe of the liver, the greater curvature of the stomach (the gastrocolic ligament connects them), the spleen in the area of the left (splenic) bend - flexura coli sinistra. The phrenocolic ligament connects this flexure of the intestine to the diaphragm. The loops of the small intestine are located below, and the duodenum and pancreas are located behind. The intestine is covered with peritoneum on all sides, the mesentery adheres to the posterior abdominal wall, and has good mobility.
The descending colon, colon descendens (12-15 cm) starts from the left (splenic) flexure, goes downwards in the lateral section and in the left iliac fossa passes into the sigmoid colon. Posteriorly, the intestine is adjacent to the left quadratus lumborum muscle, the lower end of the left kidney, and the left iliacus muscle. In front and on the left it comes into contact with the abdominal wall along the left paracolic groove, on the right and medially with the small intestine. The peritoneum covers the intestine from the front and sides (mesoperitoneally).
The sigmoid colon, colon sigmoideum, S-romanum (15-67 cm) in the form of two loops lies in the left iliac fossa from the level of the iliac crest to the sacroiliac joint. It is covered with peritoneum on all sides (intraperitoneal), has a mesentery and has good mobility. Congenital or acquired damage to the nervous apparatus of the sigmoid colon leads to the development of Hirschsprung's disease.
The rectum, rectum, proctos, is located in the pelvic cavity and begins at the level of the III sacral vertebra, average length 15 cm, diameter 2.5-7.5 cm. Posteriorly adjacent to the sacrum and coccyx, repeating their posterior bend. In front, in men it is adjacent to the prostate, seminal vesicles, vas deferens and bladder, in women - with the uterus and vagina. A digital examination of adjacent organs is performed through the rectum. In the perineum, the intestine makes a second bend, but this time anteriorly. The peritoneum covers the beginning of the intestine on all sides, the ampulla on three sides and moving onto the bladder in men it forms a rectovesical notch, in women a deeper rectouterine notch. In the rectum, there are sacral and perineal bends, a supramullary part, an ampulla and an anal canal with an anal opening surrounded by internal and external sphincters.
The structure of the colon wall
Ø A serous membrane with a subserous base is present throughout the cecum, transverse, and sigmoid colons, where the peritoneum provides intraperitoneal cover. In the ascending, descending and rectum, it is replaced along the posterior surface by adventitia, and in the ampulla and anal canal of the rectum, adventitia is present along the entire perimeter.
Ø The muscular layer forms ribbons in a longitudinal layer (except for the rectum), and haustra in a circular layer (except for the rectum). Between the muscle layers there is a powerful muscular-intestinal nerve plexus with autonomic ganglia and a plexus of microvessels. The orbicularis muscles create functional sphincters and the internal anal. The external anal sphincter is formed by striated muscles.
Ø The mucous membrane with the submucosa forms three rows of semilunar folds in the cecum, colon and sigmoid colon; and in the rectum there are large transverse folds in the ampulla and longitudinal anal columns, sinuses, valves in the anus.
Ø The submucosa contains the neurocellular and choroid plexus, tubular intestinal glands, and lymphoid nodules. In the vermiform appendix they merge into groups, which is why the appendix is often called the “tonsil” of the abdominal cavity.
The blood supply to the colon comes from the superior and inferior mesenteric arteries, which with their branches connect in the mesentery of the transverse intestine and form the arterial intestinal circle - an intersystem anastomosis. The ileocecal artery departs from the superior artery to the cecum and appendix, the right colon to the ascending colon, and the middle colon to the transverse. It anastomoses with the left colic branch of the inferior mesenteric artery (Riolan arch) - the old name for the arterial circle of the intestine.
The descending colon, sigmoid colon, and supramullary rectum receive branches from the inferior mesenteric artery: the left colon, sigmoid, and superior rectum. The ampulla and the anal canal rectum are supplied with blood by the middle and lower rectal arteries from the internal iliac artery. An intersystemic arterial anastomosis is formed in the rectum due to the connections between the superior and middle rectal arteries.
The veins of the colon flow into the portal vein of the liver, except for the middle and lower rectal veins, which flow into the inferior vena cava system through the iliac veins. Porto-caval anastomoses in the form of venous plexuses are formed between the rectal veins in the wall of the supramullary part and the ampulla. In the lower third of the ampulla and the anal canal, the plexus is called hemorrhoidal. With varicose veins and thrombosis of the veins of this plexus, hemorrhoids occur.
The afferent lymphatic vessels of the colon enter the nodes - ileocolic, cecal (anterior, posterior, appendicular), mesenteric-colic, sigmoid. From the rectum they flow into other lymph nodes - internal iliac (sacral), subaortic, superior rectal.
The cecum and colon are innervated by branches of the lumbar spinal ganglia and vagal trunks of the vagus nerves, as well as branches of the sympathetic mesenteric plexuses. The sigmoid and rectum receive branches of the sacral spinal ganglia and parasympathetic splanchnic pelvic nerves, inferior mesenteric and hypogastric sympathetic plexuses.
Age characteristics. The large intestine of newborns is short (63-66 cm), does not have transverse swellings (haustra) and omental appendages, the bends are not pronounced, and lies high. The ascending colon is short and underdeveloped. Its intensive formation begins from the 6th month of a child’s life. The transverse colon has a short mesentery - up to 2 cm. In the descending colon, transverse swellings are slightly visible. The sigmoid colon is up to 20 cm long and lies high, distended with original feces - meconium. Its loop is in contact with the cecum, located in the opposite ileal fossa. The rectum of newborns has not yet formed an ampoule; bends and folds of the mucous membrane are not pronounced. It is elongated in length and retains a cylindrical shape throughout.
Haustrae and ribbons in the cecum and colon appear in the 6th month of the thoracic period, and omental appendages appear in the second year of life. All of them are finally formed by the age of 6-7 years. The ileocecal (Bauginian) valve becomes well defined by the age of 3 years. The valve of the appendix begins to form in infancy. At the end of the first year, the length of the colon increases to 83 cm, and at 10 years it is 118 cm.
Developmental anomaly - common mesentery of the ileum and cecum. In case of violations of the rotation of the primary intestine, which happens rarely, a complete or partial opposite arrangement of the abdominal viscera is possible - situs viscerus inversus totalis seu partialis. The developmental defect is atresia of the anus, when the anal membrane does not break through during development.
On a contrast X-ray, the haustra and functional sphincters are clearly visible in the colon; in the rectum - ampoule, canal and relief of the mucous membrane. The general appearance and position of all parts of the colon are clearly visible.
Topography of the colon. Its departments, blood supply, innervation, lymphatic drainage.
ascending colon,
colon ascendens, begins at the level of the confluence of the ileum with the caecum. It is located in the right lateral region of the abdomen and rises from the cecum to the right hypochondrium, where it forms flexura coli dextra and passes into the transverse colon. The length of the colon ascendens in adults is 18-20 cm.
The ascending colon is projected onto the abdominal wall in the right lateral region. The ascending colon in most cases is covered with peritoneum in front and on the sides, and in the back it is devoid of peritoneal cover, that is, it is located mesoperitoneally. However, often the ascending colon lies intraperitoneally and has a mesentery. In this case, it becomes mobile.
Right flexure of the colon
Flexura coli dextra, or hepatic flexure, is located in the right hypochondrium at the level of the X costal cartilage. Here is the transition of the ascending colon to the transverse colon.
The right flexure of the colon is located intraperitoneally in almost half of the cases, a little less often - mesoperitoneally.
The blood supply to the right flexure is provided by a. colica media with its right (descending) branch.
Transverse colon,
colon transversum, begins in the right hypochondrium from the right flexure, goes in the transverse direction, and then reaches the left hypochondrium, where it passes into the left flexure of the colon.
The colon transversum is projected onto the anterior wall of the abdomen in the right hypochondrium, epigastric, left hypochondrium and umbilical regions.
Since both bends are located more posteriorly (with the left bend lying higher than the right), and the middle sections of the intestine are adjacent to the anterior abdominal wall, the transverse colon forms an arch directed forward and downward, the left part of which is located higher and deeper than the right.
The transverse colon is located intraperitoneally and has a well-defined mesentery, mesocolon transversum, the height of which along the midline is on average 12 cm. The upper edge of the intestine is connected to the stomach almost along its entire length through the gastrocolic ligament. The greater omentum hangs like an apron from the anterior surface of the transverse colon.
The root of the mesentery of the transverse colon along its length (about 15 cm) crosses the pars descendens duodeni, pancreas and left kidney.
Arteries
The transverse colon extends from a. colica media from the upper and a. colica sinistra from the inferior mesenteric artery. A. colica media enters the mesentery of the transverse colon and goes to its right third. Here it is divided into the right one,
or descending, and left, or ascending branches. The right branch anastomoses with a. colica dextra, and the left one with the ascending branch a. colica sinistra, forming in the mesentery of the transverse colon a. marginalis coli, which in this place is called Riolan's arc [Riolan]
Left flexure of the colon
flexura coli sinistra, where the transverse colon passes into the descending colon, is located in the left hypochondrium at the level of the cartilage of the 9th rib or the eighth intercostal space, that is, approximately 4 cm above and deeper than the right bend. This makes the left flexure more difficult to examine and mobilize.
At the top, the left curve lies lateral to the tail of the pancreas, anterior to the anterior end of the spleen, and posteriorly adjacent to the left kidney, separated from it by the peritoneum and retroperitoneal tissue.
The left flexure of the colon is most often located intraperitoneally and has a clearly defined mesentery, but it can also be located mesoperitoneally. The left flexure of the colon is fixed with lig. phrenicocolicum.
Blood supply
the left flexure (splenic angle) occurs due to the ascending branch a. Colica sinistra.
Descending colon,
colon descendens, located in the left side of the abdominal cavity. From the left bend it goes down and at the level of the left iliac crest it passes into the sigmoid colon. The intestine is projected onto the anterior abdominal wall in
left lateral abdominal region. The length of the descending colon ranges from 10 to 30 cm.
The descending colon is most often located mesoperitoneally, but sometimes has a pronounced mesentery either along its entire length or in a small area.
Blood supply
descending colon branches a. Colica sinistra and a. sigmoidea A. colica sinistra, after originating from the inferior mesenteric artery, passes under the parietal peritoneum of the left mesenteric sinus in front of the left ureter and in flexura coli
sinistra is divided into ascending and descending branches. The ascending one participates in the formation of the Riolan arch, and the descending one anastomoses with the first sigmoid artery.__
Sigmoid colon
, colon sigmoideum, is located in the left iliac fossa. It is projected onto the anterior wall of the abdomen in the groin and pubic areas. Its length is about 50 cm.
Sigmoid colon
It is located intraperitoneally and has a well-defined mesentery about 8 cm high. In this regard, the intestine is very mobile and can be located in the small pelvis, rise up to the left hypochondrium, and penetrate into the right half of the abdominal cavity.
Line of attachment of the root of the mesentery of the sigmoid colon
to the posterior abdominal wall approaches a right angle and, accordingly, has two sections: the first from the left iliac fossa goes to the right, and the second - down to the promontorium. The length of the first section is on average 9.5 cm, the second - 8 cm.
Mesentery of the sigmoid colon
crosses the left iliac vessels, testicular (ovarian) vessels and the left ureter, as well as n. genitofemoralis and n. cutaneus femoris lateralis.
Sigmoid colon
, just like the transverse one, can sometimes, with a long mesentery, move to the right iliac fossa. In such cases, one must be able to distinguish the cecum from the transverse colon and sigmoid. This is quite simple to do if you remember that the greater omentum extends from the transverse colon, and the sigmoid colon has a mesentery and well-defined omental processes, which are weakly expressed or absent on the cecum.
Blood supply of the sigmoid colon
Arteries of the sigmoid colon
, ah. sigmoideae, 2-4 in number, extending from the inferior mesenteric artery, first going retroperitoneally, and then between the layers of the mesentery. The first sigmoid artery is the largest. Each of the arteries is divided into ascending and descending branches, which anastomose with each other, with the left colon and superior rectal arteries, forming the last arcade a. marginalis coli [Drammond].
The terminal branch of the inferior mesenteric artery is the superior rectal artery, a. rectalis superior, - goes to the ampulla of the rectum. It is connected by anastomosis with the inferior sigmoid and middle rectal arteries.