White coating on the tongue is usually perceived as a symptom of the disease. A person, as a rule, does not consider his language. In order for us to stand in front of the mirror, stick out our tongue and begin to look at it, there must be some reason that prompted us to do so - discomfort in the throat or oral cavity or some other dissatisfaction with our health. And then we discover a white coating on the tongue (or, as they sometimes say, that our tongue is coated ). However, don't be scared right away. Even a healthy person can have a white coating on the tongue. On the other hand, plaque on the tongue can indeed be a manifestation of the disease. Therefore, it is useful to know how pathological plaque on the tongue differs from plaque, which is considered a variant of the physiological norm.
Physiological white coating on the tongue
White coating on the tongue is most often found in the morning. At night, less saliva is produced, which contributes to the activation of bacterial activity. As a result, by morning, almost all people develop a white coating on their tongue. Sometimes it is accompanied by bad breath.
As a rule, such plaque is easily removed during morning oral hygiene. When we brush our teeth, it is advisable to also brush our tongue, especially its root. Modern toothbrushes have a surface specially modified for this purpose (the other side in relation to the bristles).
However, the white coating disappears on its own as the day begins. It is erased when eating, and the greater amount of saliva released prevents it from forming again.
FEATURES OF CHRONIC PANCREATITIS IN DENTAL PATIENTS
Published in 2015, Issue August 2015, MEDICAL SCIENCES | No comments yet
Romanenko I.G.1, Lavrovskaya Y.A.2, Lavrovskaya O.M.3
1Doctor of Medical Sciences, Professor; 2graduate student; 3candidate of medical sciences, assistant, Crimean Federal University named after V.I. Vernadsky" Medical Academy named after S.I. Georgievsky
FEATURES OF CHRONIC PANCREATITIS IN DENTAL PATIENTS
annotation
The mucous membrane of the oral cavity reflects changes in the pathology of the gastrointestinal tract - chronic pancreatitis. The diagnosis of these diseases is complicated by the lack of clear ideas about their etiology and pathogenesis and the significant clinical similarity of these diseases. Diagnosis is also complicated by the clinical picture of the course of many diseases of the oral mucosa, which has changed recently.
The purpose of this article is to study the condition of the oral mucosa against the background of chronic pancreatitis.
Key words: oral mucosa, candidal stomatitis, chronic pancreatitis, oral dysbiosis.
Romanenko I. _ G .1, Lavrovskaya Ya .A.2, Lavrovskaya O . M.3 _
1Doctor of Medical Sciences, 2graduate student, 3 Candidate of Medical Sciences, Federal state autonomous institution of higher education “Crimean Federal University named after VI Vernadsky” Medical Academy named after SI Georgievsky
STATE OF ORAL MUCOSA IN PATIENTS WITH CHRONIC PANCREATITIS
Abstract
Oral mucosa reflects on itself changes in the pathology of the gastrointestinal tract – chronic pancreatitis. Diagnosis of these diseases is complicated by the lack of clear understanding of their etiology and pathogenesis, significant clinical similarity of these diseases. Also diagnosis complicates by the clinical picture of the course of many diseases of the oral mucosa that has changed in recent years.
The aim of this article is the study of changes in the oral mucosa in patients with chronic pancreatitis.
Keywords: oral mucosa, oral candidiasis, chronic pancreatitis, oral dysbiosis.
The oral mucosa can reflect metabolic disorders, pathology of individual organs and systems of the body. Changes in the oral mucosa can be strictly specific, when the appearance of the mucous membrane can make a diagnosis and determine treatment tactics. However, in most cases, the diagnosis of diseases manifested on the mucous membrane is difficult, since the clinical picture is nonspecific and is often burdened by additional unfavorable local (insufficient hygienic care, trauma, secondary infection) and general (hypovitaminosis, somatic pathology) factors [1, 2, 3].
In many systemic diseases (digestive tract, blood system, infectious diseases and many others), changes in the mucous membrane appear long before the appearance of general clinical symptoms of pathology of human organs and systems [4, 5].
Diseases of the gastrointestinal tract are often accompanied by changes in the oral cavity [6, 7].
The secretory and motor activity of the gastrointestinal tract is influenced by receptors of the oral mucosa, which are a powerful source of reflexes [2].
A significant place in the structure of diseases of the gastrointestinal tract is occupied by diseases that occur with a decrease in the enzymatic function of the pancreas and the mucous membrane of the small intestine [8, 9, 10].
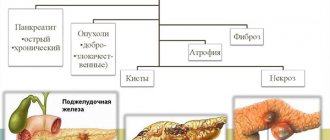
These include chronic pancreatitis - a group of chronic diseases of the pancreas with varying degrees of disruption of exocrine function [8, 11].
One of the serious complications of chronic pancreatitis is the development of intestinal dysbiosis, against the background of which various inflammatory-dystrophic diseases, including dental ones, easily arise [12].
The purpose of this study was to study the condition of the oral mucosa in patients with chronic pancreatitis.
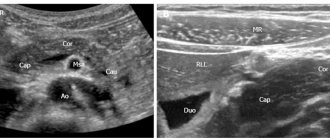
Materials and methods of research. Our studies involved 114 people (main group) with chronic pancreatitis and 34 people (control group) without general somatic pathology aged from 25 to 65 years. The average duration of the disease with chronic pancreatitis was 6 years ± 2.5 years.
The level of hygiene was determined according to the Fedorov-Volodkina GI [13], the simplified hygiene index (IG) Green-Vermillion-OHI-S (1964) [13]. The rate of salivation was calculated to assess the functional activity of the salivary glands and expressed by the volume of secreted unstimulated saliva per unit of time (ml/min) [13]. Determination of saliva acidity (pH) was performed using a universal indicator (litmus) standard paper strip with a graduated pH scale of 5.2-7.4 [13]. In order to study the level of hygienic knowledge in the prevention of dental diseases in patients with chronic pancreatitis, a survey was conducted using a questionnaire specially developed by us during the first visit to the dentist.
The object of our study was mixed unstimulated oral fluid. In the patients we observed, unstimulated oral fluid was collected in the morning on an empty stomach after preliminary rinsing of the mouth with tap water. It was forbidden to brush your teeth with a toothbrush in the morning or use dental rinses. After 3 minutes, patients spit saliva into a test tube through a funnel. After centrifugation, the volume of oral fluid was measured, the supernatant was collected in dry penicillin vials, hermetically sealed and frozen until the study.
An indicator of microbial contamination was the activity of urease [14], and an indicator of the level of nonspecific immunity was the activity of lysozyme [14]. Based on the ratio of the relative activities of urease and lysozyme, the degree of dysbiosis was calculated according to Levitsky [14].
Research results and discussion. In the patients we observed with chronic pancreatitis, there was hyperemia of the oral mucosa, icterus of the mucous membrane of the soft palate, the tongue in all patients of the main group was coated with a yellow-white coating, dry mouth, and impaired taste sensitivity were noted. All patients with chronic pancreatitis showed thinning of the red border of the lips and the appearance of chronic cracks in the corners of the mouth. In 84 (73.7%) patients, candidal stomatitis of the oral mucosa was diagnosed.
The examined patients had an unsatisfactory level of oral hygiene: Fedorov-Volodkina GI 2.4±0.11 and 1.6±0.03 (p>0.02), Green-Vermillion GI 2.0±0.09 and 1, 1±0.02 (p>0.01) in the main and control groups, respectively. A study of the functional activity of the major salivary glands revealed a reduced salivation rate in patients with CP of 0.21±0.05 ml/min. The level of salivary acidity (pH) in patients of the main group averaged 5.6±0.05, which was lower than the control group value of 6.9±0.05.
Table 2 presents the results of determining the activity of urease and lysozyme in oral fluid. In patients with chronic pancreatitis, urease activity increases significantly (p<0.01), which indicates an increase in microbial contamination of the oral cavity. At the same time, the activity of lysozyme decreases, which indicates a weakening of the antimicrobial forces of the oral mucosa.
Activity of urease and lysozyme in unstimulated oral fluid in patients with chronic pancreatitis
Table 1
Note: p – in comparison with gr. 1
Based on the ratio of the relative activities of urease and lysozyme, the calculated degree of dysbiosis shows that in patients with chronic pancreatitis the degree of oral dysbiosis increases 5 times.
Conclusions. Clinical manifestations of chronic pancreatitis on the oral mucosa are characterized by the appearance of candidal stomatitis, a decrease in salivation, and the occurrence of oral dysbiosis. The body's antimicrobial enzyme systems are weakened, which also complicates the course of candidal stomatitis. The inextricable connection of pancreatic diseases with lesions of the oral mucosa indicates the relevance of the problem of studying the characteristics of the course, timely diagnosis, differentiated treatment and prevention of relapses of diseases of the oral mucosa in patients with chronic pancreatitis.
Literature
- Banchenko, G.V. Language is the “mirror” of the body / G.V. Banchenko, Yu.M. Maksimovsky, V.M. Grinin. – M.: OJSC “Dentistry”, 2000. – 407 p.
- Banchenko, G.V. Combined diseases of the oral mucosa and internal organs / G.V. Banchenko. – M., Medicine, 1979. – 190 p.
- Gashurov, A.V. Morphology and histochemistry of the oral mucosa in normal conditions and in some pathological conditions: abstract. dis. ...cand. honey. Sci. – M., 2002. – 20 p.
- Therapeutic dentistry. Disease of the mucous membrane of the empty mouth / M.F. Danilevsky [ta insh.]. - K., 2010. - 640 p.
- Diseases of the oral mucosa / ed. L.M. Lukins. – N. Novgorod, 2003. – 210 p.
- Morozova, S.I. Diseases of the oral mucosa: Atlas / S.I. Morozova, N.A. Savelyeva - M.: Medical Information Agency LLC, 2012. - 272 p.: ill.
- Diseases of the mucous membrane of the mouth and lips / L.A. Tsvetkova-Aksamit [and others]. – M.: MEDpress inform, 2009. – 208 p.
- Okhlobystin, A.V. Antisecretory drugs in the treatment of patients with chronic pancreatitis / A.V. Okhlobystin // Clinical perspectives in gastroenterology, hepatology, 2014. – No. 3. – P.13-20.
- Nair, J. Chronic Pancreatitis / RJ Nair, L. Lawler, MR Miller // Am Fam Physician. – 2007. – Vol. 76, No. 11. – R.1679–1688.
- Schibli, S. Proper usage of pancreatic enzymes / S. Schibli, PR Durie, ED Tullis // Curr. Opin. Pulm. Med. – 2002. – Vol.8, No. 6. – P. 542–546.
- Serebrova, S.Yu. Chronic pancreatitis: a modern approach to diagnosis and treatment / S.Yu. Serebrova // Russian Medical Journal. Diseases of the digestive system. – 2008. – T. 10. – No. 1. – P. 30.
- Comprehensive assessment of the state of intestinal microbiocenosis in patients with chronic pancreatitis / E.S. Horowitz [et al.] // JMEI. – 2013. – No. 4. – P. 73-76.
- Popruzhenko, T.V. Prevention of major dental diseases / T.V. Popruzhenko, T.N. Terekhova. – Moscow, MEDpress – inform, –2009. – 464s.
- Enzymatic method for determining oral dysbiosis for screening pro- and prebiotics: method. recommendations / A.P. Levitsky [and others]. – K.: State Financial Center MZU, 2007. – 23 p.
References
- Banchenko, GV Yazyik – “zerkalo” organizma / GV Banchenko, Yu.M. Maksimovskiy, V. M. Grinin. – M.: OAO “Stomatologiya”, 2000. – 407 s.
- Banchenko, GV Sochetannyie zabolevaniya slizistoy obolochki polosti rta i vnu-trennih organov. – M., Meditsina, 1979. – 190 s.
- Gashurov, AV Morfologiya i gistohimiya slizistoy obolochki polosti rta v norme i pri nekotoryih patologicheskih sostoyaniyah: avtoref. dis. ... kand. med. nauk. – M., 2002. – 20 s.
- Terapevtichna stomatologIya. Zahvoryuvannya slizovoYi obolonki porozhnini rota / MF Danilevskiy. – K., 2010. – 640s.
- Zabolevaniya slizistoy obolochki polosti rta / pod red. LM Lukinyih. – N. Novgorod, 2003. – 210 s.
- Morozova, SI Zabolevaniya slizistoy obolochki polosti rta: Atlas / SI Moro-zova, NA Saveleva – M.: OOO “Meditsinskoe informatsionnoe agentstvo”, 2012. – 272 s.: il.
- Zabolevaniya slizistoy obolochki rta i gub / LA Tsvetkova-Aksamit .– M.: MEDpress inform, 2009. – 208 s.
- Ohlobyistin, AV Antisekretornyie preparatyi v lechenii bolnyih hronicheskim pankreatitom / AV Ohlobyistin // Klinicheskie perspektivyi v gastroenterologii, gepatologii, 2014. – # 3. – S.13-20.
- Nair, RJ Chronic Pancreatitis / RJ Nair, L. Lawler, MR Miller // Am Fam Physician. – 2007. – Vol. 76, No. 11. – S. 1679–1688.
- Schibli, S. Proper usage of pancreatic enzymes / S. Schibli, PR Durie, ED Tullis // Curr. Opin. Pulm. Med. – 2002. – Vol.8, No. 6. – S. 542–546.
- Serebrova, S. Yu. Hronicheskiy pankreatit: sovremennyiy podhod k diagnostike i lecheniyu / S.Yu. Serebrova // Russian Meditsinskiy Zhurnal. Bolezni organov pischevareniya. – 2008. – T. 10. – No. 1. – S. 30.
- Kompleksnaya ocenka sostoyaniya mikrobiocenoza kishechnika u bolnyh hronicheskim pankreatitom /ES Gorovic .– // ZHMEHI. – 2013. – No. 4. – S. 73-76.
- Popruzhenko, TV, Terehova TN Profilaktika osnovnyh stomatologicheskih zabolevanij. – Moskva, MEDpress – inform, – 2009. – 464s.
- Fermentativnyj metod opredelenija disbioza polosti rta dlja skrininga pro- i prebiotikov: metod. rekomendacii/AP Levickij. – K.: GFC MZU, 2007. – 23 s.
Pathological plaque on the tongue
If the white coating on the tongue is caused by an illness, it persists throughout the day. A thin white coating occurs with any ARVI. It disappears as soon as the patient recovers.
Particular attention should be paid to the compaction of plaque. The body of the tongue is not visible through the thick coating. Such plaque is difficult to remove. Thick plaque is considered a sign indicating the severity of the disease.
The color of the coating on the tongue is also important. The more intense the color, the more serious the pathology that caused the plaque. The color of plaque is not only white. A yellowish tint to the plaque may be associated with a malfunction of the gallbladder or pancreas. Gray plaque is possible in case of stomach disease - gastritis, peptic ulcer. In some severe infectious diseases, plaque may acquire a black, bluish or greenish tint.
However, it should be taken into account that the color of plaque can be affected by smoking, drinking and eating.
What can cause pathological plaque?
The main reason is a malfunction of the internal organs. However, there are two other possibilities: smoking and improper oral hygiene. For active smokers, a yellowish coating is a constant companion, which may not indicate anything bad about health other than the presence of a bad habit. If you don't brush your mouth properly, your tongue will be completely ignored. It is wrong to brush your teeth alone. Bacteria accumulate on the surface of the tongue; they also need to be removed. To clean the tongue, many toothbrush manufacturers make a special brush on the other side. There are also scrapers for the surface of the tongue.
If a person does not smoke and maintains proper hygiene, but there is still plaque, then this may be an indicator of the following diseases:
- Diseases of the digestive system (the most common cause) are ulcers, gastritis, diseases of the gallbladder, pancreas, and liver. Usually in such cases the plaque is accompanied by a persistent unpleasant odor that does not go away even after cleaning.
- Diseases of the respiratory system - tuberculosis, bronchitis, asthma.
- Infectious diseases - influenza, sore throat, ARVI, acute respiratory infections.
- Reduced immunity.
- Diseases of teeth and gums.
- Changes in acid-base balance due to medications.
Diseases that cause plaque on the tongue:
- stomatitis;
- thrush (candidiasis). Caused by fungi of the genus Candida. The disease can be caused by long-term use of antibiotics or decreased immunity. With oral candidiasis, a typical manifestation is a dense milky-white coating that covers the tongue in spots. Similar spots may also appear on the roof of the mouth or gums. In severe cases, plaque covers the entire tongue as well as the walls of the throat, making swallowing and breathing difficult.
- scarlet fever. In the first days of the disease, the tongue is covered with a white-gray coating. Then the coating disappears, and the tongue acquires a crimson color;
- whooping cough. A pale yellowish coating on the tongue may be accompanied by bad breath;
- dysentery. A thick white coating is typical;
- cholera. Characterized by a dark coating (even black);
- diphtheria;
- gastritis;
- stomach ulcer;
- enterocolitis;
- pancreatitis;
- stomach cancer;
- kidney diseases;
- some other diseases.
When and which doctor to contact about a coating on the tongue
As a rule, tongue coating is not the main symptom.
And it is other symptoms that tell you which doctor you should see. If plaque on the tongue is accompanied by symptoms of ARVI, you should consult a physician. If you have symptoms of gastrointestinal diseases, contact a gastroenterologist. If there are no such symptoms, and the cause of your concern is plaque, in case of white plaque you can consult a dentist, in case of yellowish or gray plaque, you can consult a gastroenterologist. And in any case, you can consult a general practitioner - family doctor or therapist. A child with a persistent coating on the tongue should be shown to a pediatrician.
Fighting methods
In order to get rid of plaque on the tongue, you first need to determine the cause of its appearance. During treatment, it is advisable to use additional methods:
- Visiting the dentist. Poor dental condition is a likely cause of the proliferation of pathogenic microorganisms.
- Consultation with a gastroenterologist. In most cases, diseases of the digestive system are the source of plaque.
- Rule out allergies to medications.
- Abstinence from drinking alcoholic beverages and smoking. Bad habits negatively affect the condition of internal organs and contribute to the disruption of beneficial intestinal microflora, which may be the cause of the problem.
We recommend reading: Why does dryness and bitterness in the mouth appear and how to treat it?
It is important to maintain oral hygiene, regularly brush your teeth and tongue, and use mouthwash.
Taking medications
In addition to dietary restrictions, therapy includes medications containing pancreatic enzymes. The medicine is prescribed exclusively by a doctor.
Folk remedies
You can get rid of the film on the tongue using a simple but effective method of traditional medicine - rinsing the mouth with water and soda. To prepare the mixture, you need to dissolve 1 tsp. powder per glass of warm boiled water. Soda solution has pronounced antiseptic properties, which helps effectively eliminate bacteria.
Rinsing with herbal decoctions - chamomile, sage, oak bark, mint - also helps against inflammatory processes in the mouth. Another excellent remedy is propolis tincture. However, due to the alcohol content in the composition, patients with pancreatitis should be careful.
Soda solution has pronounced antiseptic properties, which helps effectively eliminate bacteria and plaque. To prepare the mixture, you need to dissolve 1 tsp. powder per glass of warm boiled water.
Special food
Every person who has problems with the pancreas must follow a special diet that excludes:
- fat;
- smoked;
- pickles, canned food;
- roast;
- fast food;
- legumes;
- onions, garlic, radishes, sorrel, spinach, white cabbage, eggplant, mushrooms;
- pearl barley, barley, millet, corn grits;
- nuts;
- chocolate, cakes, pastries;
- sauces, hot seasonings;
- cocoa, coffee, strong tea;
- alcoholic and carbonated drinks.
Every person who has problems with the pancreas must follow a special diet that excludes foods harmful to the pancreas.
The patient's diet should include the following foods:
- low-fat fermented milk drinks, cottage cheese;
- lean meat, fish, poultry;
- sweet fruits and berries;
- vegetables, except those prohibited (potatoes, carrots, pumpkin, cauliflower, broccoli, green peas, zucchini are especially good);
- sugar, honey, marshmallows, marshmallows in small quantities;
- buckwheat, oatmeal, semolina, rice, pasta;
- vegetable oil, butter (in ready-made dishes);
- tea, jelly, rose hip decoction, chicory, compote.
We recommend reading: Causes of headaches with pancreatitis and methods of dealing with it
Each patient must agree with their doctor on the list of acceptable foods and an approximate daily menu. The diet may differ from that given depending on the stage of pancreatitis, individual characteristics and age of the person.
Each patient must agree with their doctor on the list of acceptable foods and an approximate daily menu. The diet may differ from that given depending on the stage of pancreatitis, individual characteristics and age of the person.