Hemorrhoids – literally translated from Greek as “bleeding” – are the most common proctological disease associated with hypertrophy and varicose veins of the rectum with the formation of hemorrhoids and the risk of bleeding.
Hemorrhoids occur with equal probability in men and women; they affect about 120-145 people out of 1000, that is, about 25% of the adult population. In the structure of proctological morbidity, it occupies 43%.
Hemorrhoids can be acute or chronic, external, internal or combined (depending on the location of the hemorrhoids), primary or secondary (as a complication of other diseases and conditions), complicated or not.
Causes of hemorrhoids
The appearance of hemorrhoids is associated with congenital insufficiency of the development of veins or venous stasis, varicose veins of the rectum that develop during life.
Risk factors for developing hemorrhoids:
- sedentary lifestyle;
- age from 35 to 55 years;
- sedentary or standing work;
- heavy physical labor, pregnancy and childbirth, causing an increase in intra-abdominal pressure;
- constipation and diarrhea;
- congenital venous insufficiency (weakness of the vascular wall and venous valves of the rectal veins);
- chronic heart failure;
- stagnation in the systemic circulation;
- chronic pelvic inflammation;
- portal hypertension;
- pelvic neoplasms (bacterial salpingoophoritis, prostatitis or cystitis);
- alcoholism;
- errors in nutrition (spicy foods, lack of fluid, lack of fiber, overeating);
- intoxication of various origins (including anabolic steroids, contraceptives, chemotherapy, long-term use of psychotropic drugs).
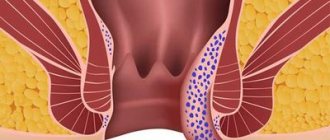
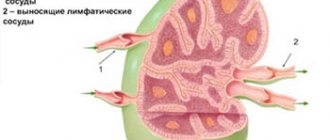
In the rectal area there are cavernous veins connected by anastomoses to the arteries of the rectum.
These plexuses ensure the retention of feces by the rectum and defecation itself, and participate in the rectal immune barrier. Disruption of venous outflow and increased arterial inflow lead to stagnation of blood in the pelvis, overstretching of the vein wall with the formation of nodes. The trophism of the longitudinal muscle of the submucosal rectum decreases and, as a result, a fibromuscular framework of the hemorrhoidal node is formed, displacing it from the anal canal externally or into the intestinal lumen. At first, they fall out and correct themselves when straining, then they require manual reduction, and in severe cases, surgical treatment.
The scarlet color of arterial blood during hemorrhoidal bleeding is explained by the presence of anastomoses between varicose cavernous veins and rectal arteries.
How to treat acute thrombosis of external hemorrhoids?
Possibilities of surgical treatment
There are two main operations for the treatment of acute thrombosis of an external hemorrhoid: removal of the entire node or just the thrombus from it. The first operation is called economical (partial) hemorrhoidectomy (removal of only the external hemorrhoid), the second is thrombectomy. Both operations are effective in terms of eliminating pain within 2-3 days after their implementation, however, after an operation to evacuate a blood clot, a relapse (reoccurrence of a blood clot) is more common.
Economical (partial) hemorrhoidectomy of a thrombosed node involves incision of the skin around the node, its isolation and removal along with the thrombus. The operation can be performed under local anesthesia.
After removal of a hemorrhoid, a small wound surface is formed, which can cause pain, especially during bowel movements. But usually the pain is much less pronounced than in the presence of a thrombosed node, and only sometimes requires taking tablet painkillers.
Thrombectomy is performed through a skin incision over the thrombus, after which the thrombus is removed and 1-2 sutures may be placed at the incision site. This intervention is almost always performed under local anesthesia.
Conservative treatment
Conservative treatment (tablets and local remedies - ointments and suppositories) is mainly aimed at relieving pain caused by a blood clot, reducing swelling and inflammation of the hemorrhoid, and normalizing the frequency and quality of stool. Pharmacies offer a large number of drugs for the treatment of hemorrhoidal disease, but they are all approximately equal in effectiveness and can be used to treat acute thrombosis of the external hemorrhoid. Local remedies (ointments and suppositories) mainly have an analgesic and anti-inflammatory effect. Topical agents with an anticoagulant effect in the treatment of acute thrombosis are effective only for the temporary prevention of new blood clots or, if the drug contains an analgesic component, for pain relief. Tablets are also used for pain relief (non-steroidal anti-inflammatory drugs, paracetamol) and normalization of venous blood flow in the pelvis (in the rectal area), for example, flavonoids. In addition, conservative treatment is also carried out after surgery to eliminate possible postoperative symptoms. A conservative treatment regimen can only be determined by a specialist, and it is better to select a combination of drugs in each specific case, depending on the characteristics of each patient.
Symptoms of hemorrhoids
- Constipation.
- Pain in the anus.
- Burning and itching around the anus.
- Maceration of the skin of the perianal area.
- Sphincter weakness.
- Mucous discharge from the rectum.
- Hemorrhoids are painful brown lumps that periodically appear in the anus at the entrance to the rectum or externally during defecation or other straining.
- Discharge of scarlet blood from the anus.
Acute hemorrhoids are characterized by:
- severe pain;
- bleeding from the anus that is difficult to stop.
Chronic hemorrhoids are accompanied by:
- infrequent and less intense pain;
- spotting, scanty, but constant bloody discharge.
Additional signs of hemorrhoids (not always included in the clinical picture):
- weakness, dizziness;
- dyspnea;
- depression;
- sensation of a foreign body and incomplete emptying.
What are external hemorrhoids? A little anatomy
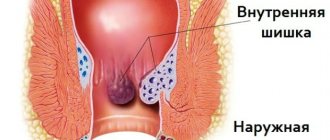
External hemorrhoids (plexuses) are formations located under the skin on the border of the anal canal and perianal (around the anus) skin. They are venous plexuses (Fig. 3). Usually they do not manifest themselves in any way, are not visible and cannot be detected by touch. As the condition worsens chronically
changes occur in internal hemorrhoids and in external hemorrhoids, leading to their enlargement and loss of connection with the muscular ring of the anal canal. However, the most significant changes in the external nodes occur when a blood clot occurs in them.
Rice. 3. Diagram of the anal canal, at the exit of which the external hemorrhoids are located (number 7 in the diagram).
Stages (degrees) of hemorrhoids
I degree:
- acute hemorrhoids: painful, tight-elastic small nodules in the anal area;
- chronic hemorrhoids: occasional bleeding without prolapse of hemorrhoids.
II degree:
- acute hemorrhoids: increased pain; compaction and enlargement of hemorrhoids, capable of prolapse and self-reduction into the intestinal lumen; redness of the skin around the anus; anal sphincter spasm;
- chronic hemorrhoids: prolapse and self-reduction of hemorrhoids, sometimes with bleeding from the rectum. The prolapse of nodes into the intestinal lumen or externally is provoked by straining.
III degree:
- acute hemorrhoids: inflammation and hyperemia spread to surrounding tissues; pain intensifies; around the anus - unreducible purple-bluish, dense, thrombosed painful nodes with foci of necrosis; risk of significant bleeding;
- chronic hemorrhoids: hemorrhoids periodically prolapse into the intestinal lumen or externally, and are reduced manually.
IV degree – chronic hemorrhoids: hemorrhoids fall out and cannot be reduced on their own.
At stages 3 and 4, the weak, thin longitudinal muscle cannot contract normally, so independent reduction of the node is impossible. If you do not manually adjust it in a timely manner, complications such as paraproctitis, fever, bleeding, and anal fissures develop.
How does acute thrombosis of the external hemorrhoid manifest?
Patients with acute thrombosis of the external hemorrhoid complain of a protrusion, “bump” (neoplasm) and/or pain of varying intensity in the anus. The size of the “bump” can range from several millimeters to several centimeters and is often accompanied by swelling of the surrounding tissues (up to the entire circumference of the anal canal). In some patients, the disease proceeds without pain, but most assess the pain as significant or unbearable.
To assess the degree of pain, a special visual analogue scale is used, in which you can independently determine the severity of pain. After all, this is the key point when choosing a treatment method. Surgical treatment will be most effective when the severity of pain is 7 or more points, while for pain up to 4 points, a conservative method of treatment can be considered optimal.
Rice. Visual analogue scale for pain assessment.
Pain usually worsens during bowel movements and/or sitting. The pain and swelling can be severe, even unbearable for several days. The intensity of pain depends on the size of the blood clot and its location in relation to the anal sphincter muscles. In general, manifestations of the disease can persist for several weeks, in exceptional cases longer. Sometimes spontaneous evacuation of a blood clot from a hemorrhoid occurs. This is preceded by necrosis (destruction) of the skin over the thrombus, and the thrombus seems to “fall out” of the node. Externally, this is accompanied by the sensation of a “bursting” ball and the release of a small amount of blood. Usually, after evacuation of the blood clot, the pain and discomfort in the anus gradually decrease. However, necrosis of the mucous membrane above the thrombus does not always end only with the evacuation of the thrombus; necrosis can continue to spread to the hemorrhoid itself and surrounding tissues, which is why this condition requires consultation with a specialist. After acute thrombosis subsides, the patient is most often left with so-called “skin fringes” - excess skin where the thrombosis was. They do not require medical treatment, but may cause cosmetic discomfort.
Complications of hemorrhoids
- Paraproctitis (inflammation of the tissues around the rectum).
- Anal fissures.
- Hemorrhoidal bleeding.
- Thrombosis of the pelvic veins.
- Incarceration of the hemorrhoidal node.
Bleeding with hemorrhoids can be regarded as one of the most important symptoms, and as a life-threatening condition, depending on the amount of blood loss.
Minor bleeding during bowel movements appears as scarlet drops, usually not mixed with feces. They lead to the development of anemia only in 2% of cases, but they cause anxiety to the patient and require planned treatment by a proctologist. Profuse hemorrhoidal bleeding is life-threatening when the vascular wall of the hemorrhoidal node ruptures. Heavy bleeding from the anus with scarlet blood is accompanied by weakness, dizziness, sticky cold sweat, increased breathing, tachycardia and a weak pulse. These are grounds for an emergency call to emergency medical services.
While waiting for the team to arrive, the patient should be placed with his legs elevated and a cold pack placed on the anus. The patient requires emergency hospitalization.
Diagnosis of hemorrhoids
Diagnosis begins with collecting anamnesis, clarifying complaints and examination by a proctologist.
The patient is positioned in a gynecological chair with his legs adducted, knee-elbow position, and less often - on his side. A physical examination by a proctologist includes:
- digital examination of the rectum;
- anoscopy (to examine the walls of the anal canal and distal rectum);
- sphincterometry (for chronic hemorrhoids - weakness, and for acute hemorrhoids - sphincter spasm);
- colonoscopy (for differential diagnosis);
- sigmoidoscopy (diagnosis of concomitant diseases of the colon);
- X-ray of the large intestine with barium (enema).
Endoscopic examinations are performed under anesthesia, in some cases under general anesthesia.
Prevention of hemorrhoids
Preventive measures should be carried out both by people with risk factors for the development of hemorrhoids, and by those who have already begun treatment for this disease:
- physical activity: walking, fitness programs without straining, swimming, exercise therapy;
- compliance with the work and rest schedule, for example, organizing food points on the highway for drivers, “physical education” for office employees, sometimes even a temporary change of job;
- compliance with the principles of ergonomics of the work process and labor protection rules;
- a diet that includes a sufficient amount of liquid and plant fiber;
- prevention and treatment of constipation;
- careful hygiene of the anus and perineum.
In this way, it is possible to prevent exacerbation and aggravation of the severity of the disease.
Is it always necessary to treat acute thrombosis of the external hemorrhoid?
The choice of treatment method for this disease is one of the most controversial issues in general proctology. Like hemorrhoids, acute thrombosis does not turn into cancer, does not cause deadly complications, but can significantly affect the patient’s quality of life; the pain syndrome is often described as “unbearable”, with which it is “simply impossible to live.”
Our Clinic has adopted a patient-centered approach to choosing a treatment method for acute thrombosis of external hemorrhoids: the doctor, together with the patient, determine how severe the symptoms are, how much the patient’s quality of life suffers, taking into account his employment, and choose a treatment method.
Acute thrombosis of the external hemorrhoid can be treated promptly (perform surgery), conservatively (take pills and use topical ointments and/or suppositories) or not treat at all, but choose a wait-and-see approach. Research and practical experience show that surgical treatment allows you to get rid of the manifestations of the disease in a shorter time; conservative treatment also allows you to get rid of the manifestations of the disease, but over a much longer time. The absence of any treatment also ends with recovery, the timing of which differs only slightly from the timing of intensive conservative treatment. The determining factor in the choice of treatment method is the patient’s choice and his assessment of the severity of the pain syndrome, therefore, the patient’s opinion is crucial for the choice of tactics. If the patient assesses the pain as unbearable, or he urgently needs to return to work, fly to another city or country, it is more reasonable to choose surgical treatment in the scope of removing the hemorrhoidal node or evacuating the blood clot from the node. Surgical treatment usually leads to faster relief of unpleasant symptoms. If the pain syndrome allows the patient to live fully in this condition or the patient is not ready for surgical intervention, it is possible to carry out conservative treatment aimed at reducing the pain syndrome and accelerating the process of organizing and resolving the blood clot.
Treatment of hemorrhoids
If the patient consults a proctologist in a timely manner, then at stages 1 and 2 of the disease, conservative treatment is used to relieve pain, itching and bleeding, and then influence the causes of the disease.
Drugs and a diet are prescribed to thin the stool; for pain, a pararectal novocaine blockade is used. The diet for hemorrhoids includes fluid intake (from 2 liters per day), the use of food bran, seaweed, flaxseed and plantain seed in the diet. Diet therapy is used in combination with other treatment methods and does not provide an independent clinical effect.
Various dosage forms are used to treat hemorrhoids.
For local treatment, rectal gels, ointments and suppositories for hemorrhoids are prescribed: for example, Ultraproct, fluocortolone, Relief.
Hemostatic sponges and suppositories: spongostan, collagen hemostatic sponges based on fibrinogen and thrombin, suppositories and ointments with heparin, phenylephrine, belladonna extract.
Tablet preparations are aimed at preventing constipation, increasing venous tone and stimulating blood and lymph flow, restoring microcirculation, and fighting inflammation.
For constipation, enzymes, laxatives with emollient and osmotic effects are prescribed: psyllium preparations, lactulose and macrogol.
Angioprotectors and phlebotropic drugs are recommended to normalize hemodynamics and restore microcirculation. Among the anti-inflammatory drugs used are drugs from the group of non-steroidal anti-inflammatory drugs, although in severe cases hormonal drugs (fluocortolone) are also used.
For thrombosis of hemorrhoids, bioflavonoids are recommended; to reduce the risk of bleeding - purified microgenized flavonoid fraction (diosmin + flavonoids in terms of hesperidin) (MOFF).
Minimally invasive interventions for hemorrhoids
Minimally invasive methods of surgical treatment of hemorrhoids are used on an outpatient basis and do not require general anesthesia, a long period of rehabilitation and pain relief in the postoperative period. These include sclerosis or alloying of hemorrhoids with latex rings, desarterization of the terminal branches of the superior hemorrhoidal artery, and infrared laser photocoagulation.
Surgery for hemorrhoids
At stage III, in advanced cases, surgical treatment of hemorrhoids under general anesthesia is used - removal of the node (hemorrhoidectomy).
Preparation for surgery includes:
- 2 days of a slag-free diet;
- an enema the day before and before surgery or taking Fortrans 1 glass every quarter of an hour;
- in some cases - antibiotics.
The postoperative period includes dressings and a slag-free diet.
The first stool occurs after 5-7 days and may be painful with some bleeding. Hemorrhoids are a serious proctological disease that reduces the quality of life and can, in some cases, pose an immediate threat. The risks of developing complications increase when visiting a proctologist late.
At stages 1 and 2, properly selected treatment can solve the problem or lead to long-term remission, but fear of a proctological examination and a false sense of shame prevent patients from seeking help.
At stages 3 and 4, the intervention of a proctologist-surgeon is required; this requires more time and causes additional discomfort. The arsenal of modern coloproctology has sufficient means for treating hemorrhoids in the early stages, which increases the quality and level of safety of life for a person who is familiar with this common unpleasant disease firsthand.
Internal hemorrhoids: treatment and diagnosis
The only sure way to get a complete picture of the disease is a comprehensive diagnosis. It includes a proctological examination, endoscopic examination, laboratory and clinical studies of the intestinal walls and feces.
Treatment can be divided into 2 types of therapy. Conservative involves taking venotonic drugs with angioprotective properties. In more severe stages, medications will not bring the desired effect, but will only remove symptoms. In such cases, it would be advisable to choose an operational method to solve the problem:
- Sclerotherapy;
- Hemorrhoidectomy;
- Laser vaporization;
- Ligation with latex rings.
“Phlebodia 600” is a treatment for internal hemorrhoids and varicose veins of the lower extremities, which can reduce the symptoms of the disease, tone the vessels and normalize blood flow in the affected vein. You can find out about the medicine in more detail and get advice from a phlebologist on our website in a special window.
Bibliography
- Vovk, E.I. Hemorrhoids: emergency care, treatment strategy, prevention / E.I. Vovk. - Text: electronic // Russian Medical Journal, 2001 - No. 20. — URL: / (date accessed 12/26/2021).
- Clinical recommendations “Hemorrhoids”, 2020. Developer: All-Russian public organization “Association of Coloproctologists of Russia”. - Text: electronic. - URL: (access date 12/26/2021).
- Mudrov, A.A. Perioperative management of patients with chronic hemorrhoids/A.A. Mudrov.-Text: direct //Medical Council, 2012. - No. 3.- P.40-44.
- Rivkin, V.L. Modern ideas about the pathogenesis, forms and treatment of hemorrhoids / V.L. Rivkin. - Text: immediate. // Consilium Medicum, 2017. - No. 19 (7.1. Surgery). – pp. 57-61.
- Savelyev, V.N. Relationship between the incidence of hemorrhoids and professions and gender in the urban district of Izhevsk for 2015 and 2022 / V.N. Savelyev, L.I. Gadelshina, K.A. Merzlikina.- Text: direct // // StudNet, 2020. – No. 12 – pp. 14-19.
- Styazhkina, S.N. Hemorrhoids as a leading problem in proctology/S. N. Styazhkina, A.A. Khairullin, L.I. Gadelshina, K.A. Merzlikina. – Text: immediate // StudNet, 2022. – No. 4 – P. 19-21.