Biliary pancreatitis
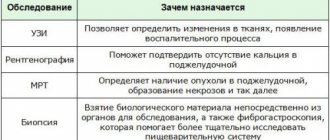
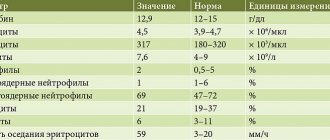
The term “chronic pancreatitis” (CP) denotes a group of chronic diseases of the pancreas (PG) of various etiologies, predominantly of an inflammatory nature, with phase-progressive focal, segmental or diffuse degenerative or destructive changes in its exocrine tissue, atrophy of glandular elements (pancreacytes) and their replacement connective (fibrous) tissue; changes in the ductal system of the pancreas with the formation of cysts and stones, with varying degrees of disruption of exocrine and endocrine functions [1]. Throughout the world, over the past 30 years, there has been an increase in the incidence of acute and chronic pancreatitis by more than 2 times. In Russia, a more intensive increase in the incidence of CP has been observed. Thus, the prevalence of pancreatic diseases among adults over the past 10 years has increased 3 times, and among adolescents - more than 4 times [2]. Biliary pathology is the most common cause of acute and exacerbation of chronic pancreatitis. One of the reasons for the formation of biliary (biliary-dependent) pancreatitis (BP) is cholelithiasis (GSD). The frequency of detection of pancreatitis in patients with cholelithiasis, according to various estimates, is 25–90% or more. Reasons for the formation of biliary pancreatitis The cause-and-effect relationship between cholelithiasis and pancreatitis is well known. The main mechanisms for the formation of BP are the reflux and retention of bile in the pancreatic ducts; it interacts with pancreatic enzymes and bacteria. In this regard, the release of bound bile acids and the activation of pancreatic enzymes in the pancreatic ductal system occur. As a result of this, its protective barrier is damaged and the pancreatic parenchyma is affected, similar to the pathological processes that develop with pancreaticobiliary reflux and accompanied by the formation of enzymatic cholecystitis [3]. As is known, an obstacle to the development of biliary-pancreatic reflux is the higher secretory pressure in the main pancreatic duct compared to the common bile duct. Therefore, the trigger for the development of PD is an increase in pressure in the ductal system of the biliary tract, which can be caused by both functional (dyssynergism in the work of the sphincter apparatus of the distal biliary tract and the main pancreatic duct, hypertonicity of the sphincter of Oddi) and organic pathology (small stones, putty-like clots). bile, strictures in the terminal part of the common bile duct, high pancreatic-biliary anastomosis, stenosing papillitis, etc.), often accompanying the course of cholelithiasis. It should be noted that biliary dysfunction and, in particular, dysfunction of the sphincter of Oddi are an integral attribute of cholelithiasis. Functional disorders due to dysfunction of the sphincter of Oddi contribute to the development of biliary-pancreatic reflux as a result of the difference in pressure in the common bile and pancreatic ducts. Even with mild biliary hypertension, the sphincter of the main pancreatic duct is not able to protect the pancreatic ductal system from pathological reflux [4]. In case of cholelithiasis, biliary sludge or stones from the gallbladder or common bile duct, entering the ampulla of Vater's papilla, can also cause the development of PD due to the creation of an obstruction to the outflow of bile and pancreatic secretions. The nature of clinical manifestations and the degree of functional disorders of the pancreas can vary significantly. In the case of rapid passage of the stone into the duodenum (duodenum), inflammatory phenomena in the pancreas quickly subside. When a calculus is strangulated in the ampulla of the major duodenal papilla, the signs of exacerbation of pancreatitis increase. The spasm of smooth muscles developing around the stone aggravates the degree of biliary hypertension and, as a consequence, the course of pancreatitis. Often in such cases, signs of obstructive jaundice appear - due to obstruction of patency due to stone obstruction of the ductal system and compression of the common bile duct by the enlarged head of the pancreas. In recent years, biliary sludge (BS) has become increasingly important in the development of PD. As a result of destabilization of the physicochemical state of bile, precipitation of its main components and the formation of BS in the gallbladder occur. Important factors contributing to the persistence of BS are hypotension of the gallbladder and hypertonicity of the sphincter of Oddi. The constant passage of BS through the bile ducts leads to damage to the mucous membrane, mainly in the area of the sphincter of Oddi. Traumatization of the mucous membrane occurs by microlites, which make up the main part of the BS. As a result of this, secondary dysfunction of the sphincter of Oddi first develops, and subsequently stenotic papillitis forms. Favorable conditions for the occurrence of biliary-pancreatic reflux with dysfunction of the sphincter of Oddi occur when there is a high connection between the common bile and pancreatic ducts or anomalies of their fusion [4]. The risk of pancreatitis is significantly higher in patients with a long and wide common bile duct, a diameter of the distal part of the main pancreatic duct of more than 2.5 mm, as well as in the presence of cysts in the common bile duct. Considering the close connection between BS and the development of acute pancreatitis, it is currently accepted that the diagnosis of idiopathic pancreatitis can be made only after excluding microlithiasis in the biliary tract [5]. The frequency of detection of BS in patients with so-called idiopathic pancreatitis is 30–75%. When examining bile within the first day from the onset of a pancreatic attack, the detection rate of BS reaches 80% [6]. Relapses of PD are promoted not only by the migration of small stones and BS along the common bile duct, but also by the exacerbation of diseases of the gastroduodenal zone, often accompanying cholelithiasis. Thus, the frequency of the combination of cholelithiasis and erosive and ulcerative lesions of the gastroduodenal zone, according to our data, reaches 25–27%. In these situations, hyperacidity of gastric juice, caused by hypergastrinemia, is an excessive stimulus for the pancreas, which, in conditions of difficult outflow of its secretions, leads to intraductal hypertension and exacerbation of the pathological process [7,8]. A feature of PD that distinguishes it from other forms of pancreatitis is the combination of exocrine pancreatic insufficiency with chronic biliary insufficiency, which affects the quality of the digestive process. Clinic The clinical picture requires, first of all, the exclusion of syndrome-related diseases, such as gastroduodenal ulcers, carcinomas of the stomach and colon, chronic antral gastritis, chronic arteriomesenteric compression, acute viral hepatitis and exacerbation of chronic viral hepatitis, exacerbation of chronic cholecystitis, pancreatic tumor, which can cause acute pancreatitis and maintain the course of CP for an indefinite period, etc. In this regard, it is necessary to examine patients to exclude the listed diseases and influence them as a factor supporting the course of CP [1]. Clinical manifestations of PD include abdominal pain syndrome, symptoms of exocrine and endocrine insufficiency of the pancreas, and biliary insufficiency. Pain syndrome is dominant in the clinical picture of the disease in 80–90% of cases. Clinical signs of exacerbation of PD are characterized by the appearance of epigastric pain radiating to the back, right or left hypochondrium. Pain can be associated with overeating, eating spicy, fatty, fried foods; it usually appears 1.5–2 hours after eating or occurs spontaneously at night. Less commonly, pain occurs immediately after eating, especially cold fizzy drinks, and is usually associated with spasm of the sphincter of Oddi. During the attack, moderate fever is possible. The most common dyspeptic disorders are nausea, vomiting, and bitterness in the mouth. A pronounced clinical picture of acute pancreatitis develops when a calculus is strangulated in the ampulla of the major duodenal papilla with disruption of the outflow of pancreatic secretions and the addition of clinical symptoms of obstructive jaundice. Diagnostics Diagnosis is complex and includes analysis of complaints, medical history, objective examination, laboratory and instrumental research methods. A clinical blood test reveals leukocytosis; a biochemical study reveals changes in liver function tests (increased activity of transaminases, alkaline phosphatase, GGTP), as well as an increase in the level of serum amylase and lipase. It should be noted that changes in liver function tests in PD are more pronounced than in pancreatitis of alcoholic or other etiology [9]. The earliest manifestation of exocrine pancreatic insufficiency is the presence of elastase in the feces in combination with steatorrhea, neutral fat and soaps. The main instrumental diagnostic method is ultrasound. Transabdominal ultrasonography (TUS) reveals stones and/or various variants of BS in the gallbladder and common bile duct. It should be noted that the sensitivity and specificity of TUS in detecting pathology of the common bile duct does not exceed 60%. In cases of poor visualization of the common bile duct during TUS (severe flatulence, patient obesity, etc.), endoscopic ultrasonography (EUS) is used. The common bile duct can be of normal size; its expansion occurs when a stone is pinched in the terminal section or ampulla of the large duodenal papilla. The duct of Wirsung is of normal size or moderately dilated. Changes in the pancreatic parenchyma depend on the stage of the process. In the early stages, changes in the pancreas cannot be detected. Subsequently, ultrasound determines the heterogeneity of its structure and uneven contours. With exacerbation of pancreatitis, ultrasound signs of pancreatic edema are detected. To determine the patency of the biliary tract, dynamic cholescintigraphy is indicated, which makes it possible to trace the entire process of bile redistribution in the biliary system, the time of its entry into the duodenum, and also to assess the functional state of the liver [10]. Endoscopic retrograde cholangiopancreatography (ERCP) can detect pathological changes in the major duodenal papilla, common bile and pancreatic ducts. If necessary, papillotomy or papillosphincterotomy is performed simultaneously during the examination. ERCP is ineffective in the presence of stones in the common bile duct less than 5 mm in diameter, putty-like bile. In 1/3 of patients, the study can cause ERCP-induced pancreatitis [11], therefore, in patients with suspected PD, this study should be used with great caution, and EUS should be used more often for diagnostic purposes. In the presence of stenosing papillitis or biliary strictures during ERCP, bile flow is restored using sphincterotomy or stenting. Endoscopic drainage using stents gives good immediate results, but in patients with calcifications of the pancreatic head, its effectiveness is 17 times lower [12]. Recently, magnetic resonance cholangiopancreaticography has been introduced into clinical practice, allowing simultaneous assessment of the condition of the bile and pancreatic ducts. With esophagogastroduodenoscopy (EGDS), changes in the mucous membrane of the upper digestive tract are assessed, especially the nature of pathological changes in the parafaterial zone and the major duodenal papilla itself. Percutaneous transhepatic cholangiography is used in cases of uninformativeness of other imaging methods and the impossibility of performing ERCP. To select adequate acid suppressive therapy and determine the duration of treatment, computer pH-metry of the stomach is indicated. Treatment Diet therapy plays an important role in the treatment of patients with PD. Strict adherence to the diet leads to a decrease in the functional load on the gallbladder and sphincter apparatus of the biliary tract, creating conditions for maximum functional rest of the pancreas. In case of severe exacerbation in the first 3 days, the patient is prescribed complete fasting with the use of alkaline mineral waters without gas. Subsequently, the patient switches to diet No. 5. It is necessary to limit fat to 60–70 g/day, protein to 100–110 g/day. In case of severe exacerbations of pancreatitis, accompanied by vomiting, it is advisable to resort to fasting for 1–3 days. and correction of water and electrolyte balance by parenteral administration of Ringer's solution, glucose, etc. After pain has decreased and vomiting has stopped, they return to oral nutrition, which should be at least 5-6 times a day. Drug therapy does not differ from the treatment of other forms of pancreatitis and should pursue the following goals [13]: • pain relief, reduction and removal of intoxication, which transfers the process from a local organ to a multi-organ - widespread one; • stopping the progression of the edematous-interstitial stage of pancreatitis in order to prevent the development of “surgical” complications in uncomplicated and limited uninfected pancreatic necrosis; • stabilization of the clinical situation, which is achieved by creating functional rest of the pancreas with a gradual transition to functional loads; • treatment of complications of the acute period – failure of external and intrasecretory insufficiency of pancreatic functions; • treatment of surgical complications and prevention of recurrence if the causative factor persists; • rehabilitation of patients with CP. The main cause of pain in PD is hypertension in the ductal system of the pancreas. In this case, pain can be relieved by measures aimed at reducing pressure in the ducts and reducing swelling and inflammatory infiltration of the pancreas, without the use of analgesics. To suppress pancreatic secretion, ranitidine, famotidine, omeprazole, and octreotide are prescribed. It is advisable to start treatment with octreotide 100 mg 3 times a day. subcutaneously The average course of treatment is 5 days. If the clinical effect is insufficient, the daily dose of the drug is increased to 600 mcg (200 mcg every 8 hours). Synthetic analogues of octreotide suppress the exocrine function of the pancreas, the secretion of gastrin, hydrochloric acid, secretin and other biologically active substances of the gastropancreatic system. The duration of treatment is determined depending on the extent of the pathological process, the involvement of retroperitoneal tissue, and the severity of the patient’s condition. At the same time, patients are prescribed gastric secretion blockers (H2 blockers of histamine receptors, proton pump inhibitors) parenterally for 3–5 days, then per os until the structural and functional activity of the pancreas is restored, for a total of 3–4 months. Antacids with high acid-neutralizing activity are indicated every 2-3 hours. However, it should be borne in mind that the use of antacids in high doses reduces the bioavailability of a number of drugs, for example, the absorption of tetracycline antibiotics, histamine H2 receptor blockers and other drugs with which Antacids form insoluble compounds. Low molecular weight heparins, heparinoids, rheopolyglucin, etc. reduce the severity of pancreatitis. The effect is due to improved microcirculation, and in 70% of cases, the resorption of microthrombi. It should also be borne in mind that biliary hypertension and inflammation reduce the delivery of drugs to the pathological focus. In this regard, heparinization with low molecular weight heparins, by improving microcirculation, increases the effectiveness of drug therapy. Drotaverine, papaverine, platyphylline, etc. are used to relieve pain. Paracetamol has proven itself well as a pain reliever. However, the maximum dose of paracetamol should not exceed 4 g/day. Of the non-narcotic analgesics, tramadol is used 1-2 ampoules (50 mg each) intramuscularly or intravenously (slowly) or 1-2 capsules (50 mg each) orally 1-3 times a day. Buprenorphine is also used in a dose of 300 mcg per ampoule and 200 mcg per tablet. For severe and resistant pain, narcotic analgesics are prescribed: 1 ml of 1–2% promedol solution subcutaneously or intramuscularly 1–3 times a day, usually for no more than 3 days. Recent studies have shown that in cases of sphincter of Oddi dysfunction and dyskinetic intestinal disorders, which contribute to the formation of abdominal pain syndrome in CP, the selective myotropic antispasmodic mebeverine (Duspatalin) has a good effect. According to indications, polyglucin 400 ml/day, hemodez 300 ml/day, 10% albumin solution 100 ml/day, 5–10% glucose solution 500 ml/day are prescribed. with adequate amounts of insulin intravenously. In severe attacks, correction of hemodynamic disturbances and the fight against endotoxicosis are necessary. To create long-term functional rest of the pancreas, it is advisable for 3 months. continue taking gastric secretion inhibitors. At the same time, the preparations of the choice are proton pump blockers, which suppress the production of hydrochloric acid as much as possible and for a long time, which leads to a decrease in the synthesis of cholecystokinin -pancreosimine and secretin, thereby ensuring the necessary functional rest of the pancreas. According to the latest data, in patients after cholecystectomy, a long -term (for 48 weeks) acid -vicious therapy with esomeprazole - 40 mg/day is recommended to stop the exacerbation of biliarnic -dependent pancreatitis. [14]. In the presence of BS, litholytic therapy with ursodeoxichole acid drugs is indicated. The dose is selected depending on body weight, the course of treatment - up to 3 months. The diet is expanded gradually, “under the cover” of enzyme preparations that play an important role in the treatment of PSU. One of the pathogenetic justifications of the use of enzyme replacement therapy in CP is the established fact that in patients with CP reduced secretion of pancreatic enzymes in external splendor failure is the cause of pancreas of pancreas with high levels of cholecystokinin -pancreosimine in blood plasma and, as a result, helps to strengthen the pain abdominal abdominal syndrome. Therapy with enzyme preparations for CP has a greater story. During this time, many enzyme preparations different in pharmaceutical forms and composition of enzyme preparations have been tested, which made it possible to formulate the most important requirements for them [15]: • have the optimal composition of enzymes in a physiological proportion; • be acid -resistant in relation to gastric juice; • mix evenly and quickly from food; • simultaneously with food to act through the gatekeeper in the DPK; • have an optimal effect in the interval of pH 4–7; • quickly and fully release enzymes in the DPP; • Do not have side effects. One of the factors that reduce the effectiveness of enzyme replacement therapy is asynchronous intake of food lumps and enzyme preparations in the form of dragees or tablets in intestinal shells, the size of which is 5 mm or more. Experimental studies have established that it is better mixed with food in the stomach and at the same time its particles with a diameter of 1–1.5 mm leave, i.e. The effectiveness of the enzyme preparation is determined not only by the content of enzymes in one tablet or capsule, but also by its dosage form. The stated requirements are most fully met by Creon. According to numerous international studies, the bicom -bearing drug Creon has the ability to carry out passage along with food, since capsules containing mini -microspheres coated with an intestinal shell quickly dissolve in the stomach, releasing hundreds of mini -microspheres (from 280 to 500 particles with a diameter of 1.0 –1.2 mm), which more evenly distribute enzymes after their release inside the intestinal contents. When the mini -mycrospheres reach the DPC, the intestinal shell is destroyed, enzymes are released with lipolytic, amylolytic and proteolytic activity, leading to the disintegration of fats, starch and lipids. Thus, Creon, thanks to a special dosage form, creates the most optimal conditions for cramp digestive. The second advantage of Creon over other enzyme preparations lies in its high enzymatic activity, which is especially important for BP, which is accompanied by a deficiency of bile acids that directly participate in the activation of pancreatic enzymes. The enzyme composition of Creon is optimally balanced to replace exocrine pancreatic failure. As you know, with replacement enzyme therapy, the lipase activity of the drugs is of main importance. Therefore, when selecting an enzyme preparation for replacement therapy, a determining property is the activity of lipase. This is due to the fact that under PSU products and secretion of lipase are violated earlier than in amylolytic and proteolytic enzymes; Lipase is faster and more pronounced in anactivated by acidification of the DPP due to a decrease in the products of pancreatic bicarbonates; With a decrease in the pH in the DPP, the precipitation of bile acids occurs, which exacerbates a violation of fat absorption [16]. Creon is produced in various versions: Creon 10,000, Creon 25000 and Creon 40000, which contain 10,000, 25000 and 40,000 units of lipase, Adequately selected doses of Creon provide a full -fledged canvas digestion, which is accompanied by a decrease in pressure in the DPC and thereby helps to improve the outflow of bile and pancreatic secretion and a decrease in pain. In addition, Creon in patients with PSU, accompanied by pancreatic deficiency, reduces pain syndrome by type of feedback. The appointment of enzyme preparations to relieve pain is considered an early indication, since enzymatic deficiency manifests itself only after a long course of CP (for example, with prolonged stone mining, especially in people with multiple small calculi in the gallbladder), and pain occurs immediately. The anti -Bolea effect of Creon is associated with a high content of protease (thripsin) as part of an enzyme preparation. Proteases destroy realizingpeptides (cholecystokinin -pancreosimine and secretin), released in the initial parts of the DPC and stimulating pancreatic secretion. Thus, proteases cause a decrease in pancreatic secretion and provide functional rest of the pancreas. Creon has the highest activity of thripsin: Creon 10,000 contains 600 FIP proteases, Creon 25000 - 1000 FIP proteases. The latest studies have shown that Creon is able to suppress the inflammatory process in the pancreas. This is confirmed by a decrease in the blood level of pro -inflammatory (IL - 8, TNFα) and an increase in the level of anti -inflammatory (IL --10) cytokines, as well as a decrease in TGF --β, reflecting the processes of fibrogenesis. The long -term intake of Creon reaches not only the replacement targets, but also slows down the progression of the development of connective tissue in the parenchyma of the pancreas at the PSU [17]. The selection of doses of pancreatic enzymes is carried out individually. In a severe degree of pancreatic failure, it is recommended to take a drug with a lipase content of at least 25,000–40,000 units during the main meal, in intermediate meals - an additional 10,000–5,000 units [18]. Creon has a high safety index, which allows it to use it in pediatric practice, including in infants. The drug is allowed for use in people professing Islam. Thus, numerous observations demonstrate a variety of clinical effects of Creon, which allows you to consider it a “gold standard” in the treatment of patients with PSU. For the prevention of cholangitis and abscesses of the PJSC, antibiotics of a wide spectrum of action are used. In addition, antibacterial therapy helps to restore the intestinal microbiocenosis disrupted during housing and communal services, and also prevents the exacerbation of chronic calculent cholecystitis. Cyprofloxacin, Imipenem, cefoxim, cefotaxim, etc. are shown. The limitation for the use of ceftriaxone is the formation of BS when taking it. It should be borne in mind that a number of antibacterial drugs are toxic to the acinar cells of the pancreas (tetracycline, rifampicin, isoniazide, amphotericin). In patients with housing and communal services, as well as after cholecystectomy, excessive bacterial growth syndrome (SIBR) in the small intestine is detected. According to our data, in a group of patients who suffered cholecystectomy, Siberia was detected in 58%, and among patients with housing and communal services - in 28% of cases. The results can be explained by the fact that after cholecystectomy the concentration of bile acids in bile and its bactericidal properties are reduced [19]. According to A.I. Pastukhov, in patients with chronic biliarn -dependent pancreatitis after Siberian cholecystectomy was detected in 33% of cases [14]. Our studies show that the best clinical effect in these situations has rifaximin in a daily dose of 800-1200 mg, the duration of the reception is 7 days. The dose and duration of antibacterial therapy are determined by the severity of the patient's condition, laboratory indicators and data of instrumental research methods. With dysfunction of the sphincter apparatus of the biliary tract, gimecron or furniturer in conventional dosages (treatment course - 2–4 weeks) are indicated; In the presence of holelithiasis - cylinder dilatation, papillosphinterotomy with the extraction of stones. The restoration of the outflow of bile and pancreatic juice is one of the main and indispensable conditions in the treatment of PSU. In order to prevent BP, it is necessary to carry out adequate housing and communal services in the early stages, and at the stage of calcium cholecystitis - timely cholecystectomy. Literature 1. Minushkin O.N. Chronic pancreatitis: some aspects of pathogenesis, diagnosis and treatment // Consilium Medicum. 2002. T. 4. No. 1. P. 23–26. 2. Maev I.V., Kazyulin A.N., Kucheryovy Yu.A. and others. Some issues of epidemiology of chronic pancreatitis // Clinical -epidemiological and ethno -ethnic problems of digestive diseases: Materials of the III East Siberian Gastroenterological Conference / Ed. prof. V.V. Tsukanova. Krasnoyarsk, 2003. S. 9–52. 3. Ilchenko A.A. Enzymatic cholecystitis // Experimental and clinical gastroenterology. 2009. No. 7. S. 70–73. 4. Ilchenko A.A. Diseases of the gall bladder and biliary tract: hands for doctors. 2nd ed., Refined. and additional M.: LLC "Publishing House" Medical Information Agency ", 2011. 880 p. 5. SHEBLI JM, Ferrari Junior Ap, Silva Mr et al. Biliary Microcristals in Idiopathicacute Pancreatitis: Clue for Occult Underlying Biliary Etiology // Arg. Gastroenterol. 2002. Apr - jun. Vol. 37 (2). R. 93–101. 6. Ilchenko A.A. Diagnosis of biliary sweetie in the practice of a doctor -therapist of the clinic. Directory of a polyclinic doctor. 2009. No. 10. S. 59–63. 7. Selezneva E.Ya., Ilchenko A.A. The clinical features of the course of gallstone disease, combined with peptic ulcer of the duodenum and pathogenetic features of their development // Experimental and clinical gastroenterology. 2011. No. 4. S. 31–36. 8. Selezneva E.Ya., Ilchenko A.A. Gallstone disease combined with peptic ulcer of the duodenum. Review of literature // Experimental and clinical gastroenterology. 2008. No. 2. P. 48–55. 9. Diseases of the liver and biliary tract. Hands for doctors / under. ed. V.T. Ivashkina. M.: LLC "Publishing House" M -VEV ", 2002. 416 p. 10. Ilchenko A.A., Shibaeva L.O., Khorodarev N.N. et al. The value of dynamic cholecintography in gallstone disease // Russian gastroenterological journal. 2000. No. 2. C. 13–20. 11. Ilchenko A.A. Endoscopic retrograde cholangiopancreaticography: Is the effective prevention of ERCPG -induced pancreatitis possible? // Experimental and clinical gastroenterology. 2008. No. 3. P. 62–71. 12. Khal S., Zimmermann S., Genz I. et al. RISK FACTORS For Failure of Endoscopic Stenting of Biliary Sticktures in Chronic Pancreatitis: A Prospective Follow - UP Study // AM. J. Gastroenterol. 2003. Vol. 98. P. 2448–2453. 13. Minushkin O.N. Chronic pancreatitis: issues of pathogenesis, diagnosis and treatment // Trudal patient. 2003. T. 1. No. 3. S. 26–30. 14. Pastukhov A.I. The results of a comprehensive treatment of chronic biliary -dependent pancreatitis after cholecystectomy: abstract. diss. ...cand. honey. Sci. M., 2010. 23 p. 15. Ilchenko A.A. Biliary pancreatitis // Experimental and Clinical Gastroenterology. 2005. No. 5. S. 10–16. 16. Maev I.V. Diseases of the duodenum / I.V. Maev, A.A. Samsonov. M.: Medpress, 2005.511 p. 17. Maev I.V., Kucheryovy Yu.A. Pancreatic diseases. In 2 vol. T. 2. / I.V. Maev, Yu.A. Coacher. M.: Medicine, 2008.558 p. 18. Recommendations of the Scientific Society of Gastroenterologists of Russia on the diagnosis and treatment of chronic pancreatitis // Experimental and clinical gastroenterology. 2011. No. 7. S. 122–129. 19. Mechetina T.A., Ilchenko A.A. The efficiency of rifaxine (alpha normalizer) for excessive bacterial growth syndrome in patients after cholecystectomy // Experimental and clinical gastroenterology. 2010. No. 4. S. 100–104.
Cochrane
Review Question
The question of how long should pass after a sudden attack of acute pancreatitis due to cholelithiasis before removal of the gallbladder is the subject of much debate.
We set out to answer this question by conducting a thorough search of the medical literature for studies that compared when laparoscopic cholecystectomy was performed. We included only randomized controlled trials (studies that can help us avoid incorrect conclusions if they are designed and conducted appropriately). We searched relevant literature for studies up to January 2013. Two authors independently assessed which studies should be included and extracted data to minimize bias. Laparoscopic cholecystectomy was considered “early” if it was performed within three days of the sudden onset of symptoms. Laparoscopic cholecystectomy was considered “late” if it was performed more than three days after the onset of symptoms. For severe acute pancreatitis, laparoscopic cholecystectomy was considered “early” if it was performed immediately after the patient with a sudden attack of pancreatitis was admitted to the hospital. If laparoscopic cholecystectomy was performed on the next hospital admission, it was considered “late.”
Relevance
The pancreas is an abdominal organ that secretes digestive juices that help digest food. It also contains insulin-secreting cells that maintain blood sugar levels. Acute pancreatitis is a sudden inflammatory process in the pancreas that can affect neighboring organs or affect other body systems, including the circulatory system. Depending on the presence of organ failure (such as the kidneys, lungs, or circulatory system), as well as the presence of local complications such as fluid collection around the pancreas, pancreatitis can be classified as severe acute pancreatitis or mild acute pancreatitis. Patients with severe pancreatitis have organ failure, local complications, or both. In patients with mild pancreatitis, such signs are not observed. The two main causes of acute pancreatitis, reported in more than 80% of cases, are gallstones and alcohol. Removal of the gallbladder (cholecystectomy) is the definitive treatment and is performed to prevent further attacks of acute gallstone pancreatitis and only if the patient is not contraindicated for surgery. Laparoscopic removal (minimal access surgery) of the gallbladder is the current preferred method of cholecystectomy, with more than 99% of patients recovering completely from the procedure without any serious health consequences.
Characteristics of studies
We identified one trial that compared early versus late laparoscopic cholecystectomy in patients with mild acute pancreatitis. Of the 50 participants in this trial, 25 had early laparoscopic cholecystectomy, while the remaining 25 had late laparoscopic cholecystectomy. All 50 participants were alive at the end of the trial. There were no significant differences between the two groups in terms of complications among study participants. Health-related quality of life was not reported in this trial. There was no conversion to open cholecystectomy in either group. The total length of hospital stay for early laparoscopic cholecystectomy was approximately two days less than for the late laparoscopic cholecystectomy group. The trial did not report the duration of the period of temporary disability or cost. We did not consider trials that compared early versus late laparoscopic cholecystectomy in patients with severe acute pancreatitis.
Main results
Based on the observational results of one trial, there appears to be no evidence of an increased risk of complications after early laparoscopic cholecystectomy. Early laparoscopic cholecystectomy may reduce overall hospital stay in people with mild acute pancreatitis. For mild acute pancreatitis, if appropriate equipment and specialist skills are available, early laparoscopic cholecystectomy is preferable to late. There is currently no evidence to support or refute the effectiveness of early laparoscopic cholecystectomy for severe acute pancreatitis. Further well-designed randomized controlled trials in people with severe and mild forms of acute pancreatitis are needed.
Quality of evidence
One trial reviewed was at high risk of bias, meaning its conclusions were likely to be incorrect as a consequence of the way the study was designed and conducted.
In surgical practice, acute postoperative pancreatitis (APP) is one of the most dangerous and common complications after surgery on the abdominal and retroperitoneal organs [15]. Mortality when AKI occurs varies from 19.5 to 80% and depends on the severity of the process. In destructive forms of AKI, the probability of death reaches 100% [23, 28, 32].
Assessment of the incidence of AKI is controversial, since some surgeons consider a deviation from the norm in laboratory parameters (such as increased levels of urine diastase and blood amylase) to be sufficient to establish this complication, while others take into account only its severe forms with a clear clinical picture. In addition, the duration of the postoperative period in each specific case is not precisely determined [30].
That is why the incidence of AKI, according to various sources [15, 17, 32, 40, 74], varies widely from 0.08 to 100%.
Most often, AKI develops after surgical interventions on the pancreas (PG) itself and, according to various authors [11, 15, 34, 40, 67], ranges from 1.9 to 100%.
In addition, a high incidence of this complication is observed after operations on organs that have an anatomical and functional connection with the pancreas. After gastric resection for duodenal ulcer, AKI was noted in 7.9 -31.4% of patients, after surgery for gastric cancer - 1.8 - 21.8% of cases [37, 39, 62]. Duodenoplasty (DP) is complicated by AKI with an incidence of 12–35% [6, 7], and operations on the gallbladder and extrahepatic bile ducts lead to AKI in 0.2–9.6% of patients [15, 26, 40, 55]. Laparoscopic cholecystectomy is accompanied by the development of AKI in no more than 1.8% of cases [2, 55].
Surgical interventions with the application of a biliodigestive anastomosis, endoscopic retrograde cholangiopancreatography (ERCP) and associated medical procedures lead to AKI in 0.5-40.5% of patients [19, 32, 58, 71].
In the work of T. White et al. [74] indicated that in 10 out of 70 patients they observed, AKI developed when direct pancreatic injury was excluded, i.e. after orthopedic and vascular operations. According to L. Hashimoto et al. [59] and G. Sakorafas et al. [70], cardiac surgery and operations on large vessels are accompanied by the development of AKI in 0.06-27% of cases. In addition, cases of AKI have been described after excision of neck melanosarcoma, strumectomy, pneumonectomy, cystostomy, cesarean section, hemorrhoidectomy, cataract removal, radical mastectomy, tonsillectomy, and hip replacement [60, 64]. A case of the development of severe pancreatitis in a patient who underwent lithotripsy for urolithiasis was described [48].
The given figures indicate, first of all, the high prevalence of this postoperative complication, the relevance of the issue of its diagnosis, treatment and prevention.
Etiology
AKI is a multi-etiological disease. There are many mechanisms of damage to the pancreatic parenchyma that can lead to the development of this complication, alone or in combination. I.V. Maev, Yu.A. Kucheryaev [22] highlight the most significant of them:
— direct trauma to the pancreas during mobilization of the stomach, splenectomy, etc.;
— duodenal hypertension associated with the characteristics of the intervention or the course of the postoperative period;
- biliary hypertension that occurs during operations on the biliary tract;
— pancreatic ischemia due to post-traumatic systemic and regional circulatory and microcirculation disorders;
— hyperstimulation of the exocrine apparatus of the pancreas after prolonged fasting.
Many authors [9, 27, 41] consider organ trauma during surgical procedures to be the main cause of postoperative complications. As a result, tissue ischemia, stasis and hypertension of the ductal system, leakage and action of pancreatic juice on the wound surface occur [41]. A.A. Shelagurov in 1970 [45] formulated a “traumatic theory” of the occurrence of AKI, according to which, when pancreatic tissue is damaged, a cytokine is released that activates pancreatic enzymes.
However, cases have been described when surgery was performed outside the abdominal cavity, and there was no pancreatic injury, and yet pancreatitis developed in the postoperative period [3]. The etiopathogenesis of AKI in such situations is associated with impaired microcirculation, which occurs as a result of extravascular and transcapillary translocation of fluid, platelet aggregation, thrombosis of small vessels of the pancreas, leading to its ischemia. Massive blood loss with transfusion of large doses of canned blood can also be an important factor [71].
Damage to the acinar tissue of the pancreas leads to the effusion of pancreatic juice, however, enterokinase is required to activate autolysis processes, i.e. contact of juice with bile and intestinal contents, which is not always the case. Therefore, according to modern ideas about the etiology of AKI, in addition to trauma to the pancreatic parenchyma, the presence of pancreatic hypertension is considered a necessary condition for its occurrence, since under these conditions intestinal contents and bile are refluxed into the pancreatic ducts, which leads to the activation of pancreatic enzymes [18, 26, 61, 67 ]. It follows that duodenal hypertension is also an important etiological factor in the development of AKI.
Another etiological factor is considered to be an increase in pressure in the pancreatic ductal system and extrahepatic bile ducts due to post-traumatic edema of the major duodenal papilla (MDPD), which occurs due to its reflex reactions during operations on the biliary tract [18, 26, 63]. This is to a certain extent confirmed by the fact that in the majority of patients, AKI develops after operations on the extrahepatic bile ducts, especially after direct interventions on the bile duct (during its bougienage, papillosphincteroplasty), forced probing of the bile ducts with hard metal instruments, often with the formation of a “false tract” ", difficulties in removing stones fixed in the BSDPC [19, 46].
According to some authors [15, 18, 70], one of the main causes of AKI is pancreatic ischemia due to systemic or regional circulatory disorders that occurs during surgery or in the early postoperative period. E.S. Katanov [15] in the etiology of the ischemic form of AKI considers the most significant factors to be disturbances of the systemic circulation, reflex disorders of organ hemodynamics and disturbances of blood flow in the main arterial and venous vessels during their ligation, etc.
There is also an opinion that the cause of the development of AKI may be an infectious agent that enters the gland through direct intraoperative contact [30]. In clinical medicine, the results of the work of M.N. are important. Molodenkova [23], N.N. Korenevich [16], who experimentally showed the possibility of developing rapidly occurring hemorrhagic pancreatic necrosis under the influence of ovalbumin and Escherichia coli
and
Salmonella abortis
- microorganisms that are often found in bile.
According to the “allergic theory”, AKI develops as a result of sensitization of the body by exo- and endogenous factors, which leads to damage to acinar cells and the entry of antigens into the bloodstream with the subsequent formation of antibodies to them [16]. The validity of the “allergic theory” is confirmed by data [51] on an increase in the level of immune complexes circulating in the blood, a decrease in the absolute and percentage content of T-active and T-total lymphocytes.
And yet, the leading role in the genesis of AKI is played by the initial state of the pancreas, the readiness for the development of inflammatory and destructive processes in it in the early postoperative period. According to many authors [38, 46], from 7.1 to 63.8% of patients who developed this complication suffered from chronic pancreatitis.
The etiological factors listed above trigger the processes of activation of pancreatic enzymes and autocatalytic reactions, determining the further pathogenesis of the development of AKI, which is no different from that in any other form of acute pancreatitis.
Diagnostics
Several factors should be highlighted that greatly complicate the diagnosis of AKI. Firstly, the clinical manifestations of AKI develop against the background of the patient’s initially severe general condition, caused by concomitant diseases, as well as the severity of the surgical intervention itself [26]. Secondly, the clinical picture of this complication manifests itself against the background of symptoms of the postoperative period and is smoothed out by the therapy, including painkillers. Thirdly, in 25-30% of patients the severity of the condition is regarded as a manifestation of another postoperative complication [42]. Often the disease occurs under the guise of intestinal paresis, anastomositis, residual effects of peritonitis, etc. [27]
AKI very often leads to severe impairment of the motor function of the duodenum, as evidenced by dull pain in the epigastric region or left hypochondrium that is poorly controlled by conventional analgesics, accompanied by persistent nausea and repeated vomiting of gastric contents mixed with bile.
Very characteristic of pancreatitis is swelling in the epigastric region, which does not decrease with decompression and gastric lavage - Gobier's symptom. This is associated with isolated paresis of the transverse colon and is detected by plain radiography of the abdominal organs.
Percussion reveals tympanitis, especially high in the epigastrium and in the projection of the lateral canals of the abdomen. Dullness may be detected in sloping areas of the abdominal cavity, which varies depending on the position of the patient’s body (free fluid in the abdominal cavity). At the same time, exudate begins to be released through the drainages, often hemorrhagic in nature, with high amylase values.
The most common, simple and cheap biochemical method for diagnosing AKI is the determination of amylase activity in the blood and urine. However, the sensitivity and specificity of this method range from 30 to 92% and from 20 to 60%, respectively [22]. In addition, to date there is no consensus regarding the threshold values confirming the diagnosis of “acute pancreatitis”. Some authors focus on the upper limit of the norm [68], others on values 3-6 times higher [65]. In domestic medicine, values 2-4 times higher than normal are usually taken into account, i.e. amylase is above 60-120 g/h·l [36, 47].
Some authors [52], in order to increase the accuracy of AP diagnosis, propose to determine alpha-amylase activity not in blood serum, but in tears. In their opinion, this is technically much simpler and faster, since it does not require taking blood from a vein and obtaining serum. In addition, the determination of amylase in tears is more accurate, since the activity of amylase in tears is much higher than in the blood (4 times) and persists for 7 days. Amylase activity in the tears of healthy people ranges from 193.5±20.9 U/l (130-250 U/l). When amylase rises to more than 300 U/l, AP is diagnosed. However, this method has not yet found its widespread use in practice.
A more specific indicator for acute pancreatitis is an increase in blood lipase activity [22, 47]. Lipase persists in the blood longer than amylase, so using this test, acute pancreatitis can be diagnosed even several days after the onset of the disease [68]. However, hyperlipasemia, as well as increased blood amylase activity, does not have high specificity for pancreatic diseases, since it is also detected in other gastrointestinal diseases [9, 22, 47]. It is registered in 60% of patients with diseases of the hepatobiliary system, acute intestinal obstruction, renal failure, prostate cancer and other non-pancreatic diseases.
According to the results of a study by S. Raty et al. [68], a test for determining trypsinogen content in urine is sufficiently informative for early diagnosis of postoperative pancreatitis after pancreatic resections. The sensitivity and specificity of the urine trypsinogen test were estimated to be 100 and 92%, respectively. According to Russian literature [22], the sensitivity and specificity of determining the level of trypsinogen-2 in urine in the differential diagnosis of AKI and acute diseases of the abdominal organs of non-pancreatic origin reach 91-95% and 95-99%, respectively.
Based on this, the authors propose this test as a method for early diagnosis of postoperative pancreatitis.
In recent years, great importance in the diagnosis of pancreatitis, as well as in determining the prognosis and likelihood of complications, has been attached to the study of phospholipase A2 activity in the blood and urine and the determination of serum elastase-1. In pancreatitis, the sensitivity and specificity of determining phospholipase A2 activity in the blood is 100 and 90%, respectively [22]. Determination of type 1 elastase activity in the blood is considered a test for late diagnosis of pancreatitis, since its elevated level persists for 8-10 days after the attack. However, when trying to diagnose acute pancreatitis in a group of patients with various diseases of the pancreas, these indicators demonstrate low specificity, since in almost half of patients with chronic pancreatitis and pancreatic cancer their content exceeds the normal level and in some cases reaches values characteristic of patients with acute pancreatitis [ 8, 25, 52].
However, among all laboratory indicators it is difficult to single out one that could be called the “gold standard”. Many of them are highly sensitive, but they do not have sufficient specificity to reliably diagnose AKI.
Among the instrumental methods for diagnosing AKI are X-ray examination, ultrasound of the pancreas, as well as CT and MRI of the abdominal organs.
Radiological signs of AKI are: limited mobility of the domes of the diaphragm, pneumatosis of the transverse colon and left-sided pleurisy [3]. Conventional radiological signs of primary acute pancreatitis, such as pneumotization of the small intestine, regional spasm of the transverse colon, blurred contours of the left kidney, and others, are rarely found in AKI, which is associated with postoperative trauma [17].
Ultrasound examination is considered one of the most significant in the early diagnosis of AKI [33]. Among the most significant ultrasound signs of acute pancreatitis are an increase in the size of the pancreas, blurred contours, an increase in the distance between the posterior wall of the stomach and the anterior surface of the pancreas, as well as a change in its echogenicity. Dynamic monitoring using ultrasound of the state of the entire biliopancreatic system makes it possible to assess the effectiveness of conservative therapy for this complication. It is important that this method has no contraindications, and the harmlessness and painlessness of its implementation make it possible to perform multiple studies directly at the patient’s bedside.
However, according to A.L. Kostyuchenko et al. [17] the rapid development of intestinal paresis and inevitable pneumoperitoneum after laparotomy can lead to low-informative ultrasound scanning in AKI.
The use of endoscopic ultrasonography in patients with AKI allows for an objective assessment of the condition of the pancreas, to differentiate complicated forms of AKI, and also to monitor the dynamics of the pathological process in the pancreas and surrounding organs and tissues. According to M.V. Danilova et al. [9], the low invasiveness of endoscopic ultrasonography allows it to be used in the early and late period after pancreatic surgery and to identify postoperative complications. However, it is worth noting that this method is not available for most Russian clinics.
CT with bolus contrast enhancement has now established itself as the “gold standard” for assessing the severity and spread of the inflammatory process in patients with AP, as well as determining indications for surgical treatment [33]. With this method, pneumotized intestinal loops and the stomach do not interfere with the assessment of changes in the retroperitoneal tissue and the tissue of the gland itself [22].
MRI is also a promising method for diagnosing and assessing the dynamics of AKI development [74]. High-field MRI fully reflects the morphological changes in acute destructive pancreatitis [43]. The main MRI signs of acute pancreatitis are swelling, enlargement of the pancreas, necrosis of the parenchyma and surrounding fatty tissue, accumulation of free fluid in the abdominal cavity, the presence of a hemorrhagic component, infiltration of the fatty capsule of the kidney.
Computed tomography and MRI allow for accurate differential diagnosis of AKI with other postoperative conditions that determine the severity of the patient’s condition. Unfortunately, these highly informative and accurate methods are not widely used in clinical practice due to their high cost.
Prevention
Prevention of AKI is carried out both surgically and medically.
The surgical way to prevent AKI is to use gentle surgical techniques to reduce the morbidity and duration of surgery [1, 18]. In addition, it is possible to perform simultaneous surgical interventions aimed at preventing the development of AKI [44], among which biliary drainage is especially highlighted as the most effective procedure that prevents the development of post-manipulation pancreatitis [22].
Despite this, drug prevention of AKI is more common and promising, which can be divided into specific and nonspecific. Among nonspecific factors, an important role is given to preventive therapy during the preoperative preparation of the patient, including diet, the use of enzyme preparations, stabilization of water-electrolyte and protein metabolism [26]. In addition, an important component of nonspecific prevention of the development of postoperative complications, including pancreatitis, is the optimization of anesthetic management of operations [12].
Specific methods for the prevention of acute postoperative pancreatitis involve the use of drugs whose action is aimed directly at the stages of its pathogenesis. Among them are:
- protease inhibitors;
- inhibitors of exocrine secretion;
- antioxidants;
- cytostatics.
Protease inhibitors (aprotinin preparations - contrical, trasylol and gordox) are proteins that have the property of inactivating proteolytic enzymes of endogenous and exogenous origin. It has been established that the effect of these drugs is based on the inactivation of trypsin, chymotrypsin, plasmin, kallikrein; however, they have virtually no effect on their synthesis. The interaction between active pancreatic enzymes and antiproteolytic drugs occurs mainly in the blood plasma, but it is possible that this is also possible in the pancreatic tissue [18].
Great hopes were placed on a low-molecular protease inhibitor, gabexate mesylate, which, unlike drugs from the aprotinin group, has the ability to penetrate into the pancreas. Experiments by J. Wisner et al. [75] provided convincing evidence in animals for the effectiveness of its prophylactic administration. Later C. Cavallini et al. [54] demonstrated a significant decrease in the incidence of acute pancreatitis and a decrease in blood amylase levels in a group of patients who received the drug during ERCP. Other authors [50] note the ineffectiveness of gabexate mesylate administration in patients at high risk of developing pancreatitis after ERCP.
Currently, the greatest prospects in the prevention and treatment of acute postoperative pancreatitis are associated with the use of synthetic analogues of somatostatin: octreotide, stylamine, sandostatin and octreotide depot [10, 24, 26].
According to a number of authors [56, 66, 67, 76], preventive administration of somatostatin analogs is quite effective, but a positive effect was not achieved in all studies performed according to the rules of evidence-based medicine. This, in particular, was demonstrated in a group of patients at high risk of developing pancreatitis after ERCP. According to A. Andruilli et al. [50], prophylactic use of somatostatin drugs did not reduce the incidence of acute postoperative pancreatitis.
In recent years in Russia, the domestically produced drug octreotide has become widely used in the prevention of acute destructive pancreatitis, including postoperative pancreatitis [13, 14, 36].
The results of studies [14, 35, 36] showed that in terms of reducing the exocrine function of the pancreas, octreotide has a spectrum of action almost identical to the spectrum of action of natural somatostatin, and is not inferior in this criterion to another synthetic analogue of foreign production - sandostatin, which has been widely used for a long time. used in clinical practice.
The mechanism of action of octreotide is based on the suppression of adenylate cyclase and the associated decrease in cyclic adenosine monophosphate (cAMP) in the cell.
The inhibitory effect of octreotide on gastric G cells leads to inhibition of gastrin production, which leads to a decrease in the secretion of pepsin and hydrochloric acid, as well as the main stimulators of digestive enzymes and bicarbonates in the pancreas - cholecystokinin, secretin and vasointestinal peptide. A decrease in the formation of motilin leads to a decrease in the motor activity of the gastrointestinal tract [49, 65, 75].
The authors [53] suggest administering octreotide subcutaneously, the first dose of 200 mcg 1 hour before surgery, after surgery - 100 mcg 3 times a day for the next 7 days, but there are other schemes for its use. Thus, when predicting significant trauma to the pancreas and, as a consequence, the possible development of severe forms of AKI, the dosage of the drug is increased by 2 times and it is 600 mcg per day.
E.S. Sirota [29], in order to prevent postoperative pancreatitis, suggests administering octreotide subcutaneously or intravenously at 0.1 mg 3 times a day for 3 days after surgery.
However, some foreign authors [49, 57] indicate that somatostatin derivatives are not effective enough to treat AKI and reduce mortality in patients with this complication. Moreover, for preventive purposes (for example, in elective surgery on the organs of the upper abdominal cavity), inhibition of exocrine pancreatic secretion using these drugs significantly reduces the number of complications.
Recently, studies have appeared [10, 13] reporting an effective reduction in the incidence of postoperative pancreatitis when prescribed long-acting forms of synthetic somatostatin analogues (10 mg octreotide depot 7 days before surgery) in patients operated on for gastric cancer. According to Yu.S. Polushina et al. [26], the use of octreotide depot according to the above scheme reduced the incidence of pancreatitis by 4.5 times and prevented severe forms of this postoperative complication.
N.N. Krylov et al. [20] assessed the effectiveness of drug prevention of acute postoperative pancreatitis with octreotide, octreotide depot, 5-fluorouracil (5-FU) in combination with dalargin in 325 patients operated on for gastric cancer. In the 1st group of patients, octreotide was used to prevent AKI according to the following regimen: 200 mg before surgery, 100 mg 3 times a day after surgery for 6 days. In group 2, AKI was prevented with depot octreotide, which was administered at a dosage of 0.01 g 7 days before surgery. In group 3, 5-FU was used with dalargin and contrical according to the following regimen: 5-foruracil - 500 mg intraoperatively, 500 mg each for 3 days after surgery; dalargin - 5.0 ml intraoperatively and 5.0 ml for 6 days; Kontrikal was administered at a dose of 20,000 units intravenously for 6 days. According to the results of the study, when using octreotide, acute pancreatitis was observed in 13% of patients, the use of octreotide depot was the most effective and did not avoid the development of AKI in only 4.2% of patients, and in the group in which 5-FU was used to prevent AKI , contrical and dalargin, this complication developed in 20% of patients.
Of the antioxidant drugs for the prevention of AKI V.V. Shabanov [40] suggests intravenous use of thioctacid and ubiquinone-compositum. According to the author, these drugs reduce the severity of the postoperative period, as well as the absolute and relative risk of developing this complication by 11.4 and 100%, respectively, in patients with stomach and esophageal cancer.
Among the drugs that suppress the secretory activity of pancreatic cells, for a long time special attention was paid to cytostatics - pyrimidine derivatives - 5-FTU and fluorafur. These compounds are considered the most effective inhibitors of the enzyme-producing activity of pancreatic cells, since they selectively accumulate in the pancreas, inhibiting protein synthesis in it [17]. It has been proven that the synthesis of amylase and trypsin decreases 15 minutes after the start of intravenous infusion of the drug. In addition, its breakdown releases fluoroacetic acid, which can inhibit lipase [26].
A number of authors propose combination regimens for the prevention of AKI. E.S. Sirota [29] used antimetabolites (5-fluorouracil; sandostatin), antioxidants (Mexidol, vitamin E), parenteral nutrition with subsequent transfer to the enteral route of food intake, as well as antibiotic therapy to prevent postoperative pancreatitis in patients with abdominal, thoracic and thoracoabdominal injuries for the entire period of treatment. The proposed regimen for the prevention of AKI was used in 51 patients, and in none of the cases did the development of this complication occur.
Considering the significant role of impaired microcirculation in the pancreas in the pathogenesis of acute pancreatitis, V.I. Lupaltsov [21] reports on the advisability of preventing microcirculatory disorders in organ tissue during operations in the pancreaticoduodenal zone, which may be effective in preventing complications. For this, the author proposes intravenous administration of rheopolyglucin-complamine-trental mixture, which, according to his data, reduced the incidence of acute pancreatitis in the group of operated patients from 35 to 12%.
From the data presented, it follows that at present, issues of assessing the likelihood of developing AKI have not been fully developed; there are no clear recommendations on methods for preventing pancreatitis in the intraoperative period, based on the severity of certain prognostic risk factors [53]. In addition, the economic costs of preventing AKI do not always justify the hopes placed on it. Therefore, the issue of clinical and economic effectiveness of the prevention of postoperative pancreatitis remains relevant to this day. Which drug is most effective, whether preventive treatment should be carried out for all patients or those belonging only to the risk group, whether complex therapy is necessary or whether it is enough to limit ourselves to drugs with one mechanism of action - these and many other problems are still unresolved.