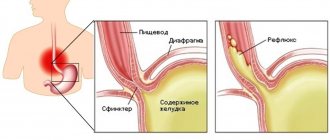
Reflux esophagitis, or “peptic esophagitis” is an inflammation of the lower esophageal mucosa caused by the action of hydrochloric acid and enzymes or bile on the esophageal mucosa.
Peptic esophagitis accompanies a hiatal hernia, occurs with gastric ulcers and its complications, with diseases of the biliary system, after gastric surgery and other diseases.
What is reflux esophagitis
The inflammatory process of the esophageal mucosa, provoked by the reflux of stomach contents, is called gastroesophageal reflux disease or reflux esophagitis.
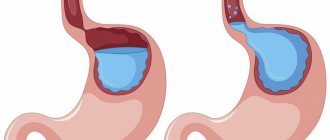
In some cases, reflux esophagitis with duodeno-gastric reflux (reflux of the contents of the duodenum) is diagnosed. During normal physiological functioning of the stomach, the glands of the mucous membrane produce non-proteolytic enzymes and hydrochloric acid to digest food. As a result of the reflux of stomach contents into the esophagus, acidic gastric juice affects the mucous membranes of the lower sections of the digestive canal. In the early stages of reflux esophagitis, the patient may experience heartburn, colic, pain and bloating in the gastrointestinal tract, as with a typical digestive disorder.
The main reasons for the development of chronic reflux esophagitis:
- peptic ulcer;
- hiatal hernia;
- constricting tight clothing;
- insufficient length of the esophagus;
- complications of chronic gastritis;
- stenosis of the pyloroduodenal meatus;
- physiological changes during pregnancy;
- underdeveloped neuromuscular system (often found in infants);
- decreased reactivity of the gastrointestinal tract (due to obesity, stress, poor nutrition).
It is quite difficult to trace the development of reflux esophagitis in the early stages, because atypical mild symptoms of the disease rarely bring patients to the gastroenterologist’s office. With a significant degree of damage to the esophagus, reflux makes itself felt with intense cutting pain, burning behind the sternum, bleeding and ulcers.
Symptoms of reflux esophagitis:
- vomit;
- heartburn;
- nausea;
- belching;
- sour belching;
- stomach pain;
- discomfort after eating;
- difficulty swallowing (lump in the esophagus).
Symptoms of the disease intensify after drinking carbonated and hot drinks, coffee, spicy and heavy foods, and overeating. In the chronic stage of the disease, dysfunction of the respiratory system, laryngospasms, respiratory distress, and bronchial asthma appear.
Four degrees of reflux esophagitis are diagnosed:
- 1st degree of reflux esophagitis - the area of damage to the mucous membrane is limited to the folds of the esophagus and is less than 5 mm in diameter.
- 2nd degree reflux esophagitis - one or more foci limited by folds of the mucosa. The localization area exceeds 5 mm in diameter.
- 3rd degree – one or more lesions located in 2 or more folds of the mucosa. The degree of damage to the esophagus is within 75%.
- Grade 4 – one or more defects localized to more than 75% of the surface of the esophageal mucosa.
Classification of esophagitis
According to the nature of the disease and its severity, esophagitis is:
- Edematous and catarrhal. These are the most common types of esophagitis, which are classified as a mild, sluggish form of the disease. Symptoms include swelling and hyperemia of the esophageal mucosa.
- Erosive. Erosive esophagitis occurs as a result of thermal or chemical burns of the mucous membrane, and can also be triggered by an acute infectious process. The disease is dangerous due to the occurrence of erosions on the surface of the mucosa and in most cases turns into an irreversible necrotic form.
- Phlegmonous. A fairly rare type that occurs due to deformation or damage to the walls of the esophagus.
- Exfoliative. The disease provokes the fusion of fibrous exudate with submucosal tissue.
- Hemorrhagic. Difficult to diagnose at an early stage. In the absence of therapy and diet, the disease causes hemorrhages in the esophagus.
- Necrotic. A severe form of acute inflammatory process, which is typical for patients with HIV. The necrotic form can also appear against the background of typhus, sepsis, candidiasis, scarlet fever, and uremia.
- Pseudomembranous (fibrinous). The main causes of fibrinous inflammation are fungal infections, acute infectious diseases and malignant tumors. The pseudomembranous type of esophagitis provokes frequent vomiting, painful dysphagia, ulceration of the mucous membrane and fibrinous deposits. After a course of therapy, dangerous scar formations may remain in the esophagus.
Based on the area of localization of inflammation of the esophageal mucosa, the following types of esophagitis are distinguished:
- Total - the lesion covered the entire esophagus.
- Distal - with damage to the lower esophagus.
- Proximal - the inflammatory process is located in the upper parts of the esophagus.
Pathogenesis of the disease
In gastroenterology they diagnose: chronic, subacute and acute esophagitis.
Reasons for the development of acute esophagitis:
- Infection (diphtheria, influenza, fungal infection and others).
- Mechanical damage (trauma, burn).
- Allergic reaction.
In the pathogenesis of allergic and infectious esophagitis, the main cause of the development of the disease is considered to be a failure in the body’s immune system.
Depending on the cause of occurrence, the following types of chronic esophagitis are distinguished:
- Nutritional – as a result of consumption of spicy and hot foods, alcohol.
- Professional – regular inhalation of caustic chemical fumes.
- Congestive – with congestion in the esophagus.
- Allergic – associated with food allergies.
- Dysmetabolic – pathogenesis is tissue hypoxia, hypovitaminosis, intoxication of the body.
- Ulcerous (idiopathic) - characterized by an unclear etiology and similarity to ulcerative colitis.
Causes of reflux disease
One of the most common causes of the disease is poor nutrition (with a predominance of spicy foods in the diet) and abuse of alcoholic beverages. Other provoking factors include:
- Stress.
- Exposure to chemicals.
- Pregnancy period (because the stomach is slightly compressed).
- Long-term smoking (how to clean a smoker's lungs).
- Excess weight.
- Digestive problems.
- Taking medications (antibiotics, NSAIDs, etc.).
- Hormonal imbalance (due to dysfunction of the thyroid gland).
- Prolonged fasting.
Any of the above factors can provoke an exacerbation.
Symptoms of esophagitis
Symptoms of acute esophagitis
The symptoms of the inflammatory process depend on the cause of the disease, the degree of damage to the esophagus, side pathologies of the gastrointestinal tract and the reactive forces of the body. The catarrhal form of esophagitis in most cases develops without obvious symptoms, therefore it is diagnosed at the stage of significant hyperemia of the esophageal mucosa.
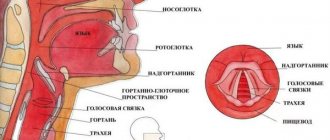
Severe types of esophagitis with lesions of the mucous membrane and pathologies of the esophagus are manifested by acute pain radiating to the cervical region, a burning sensation behind the sternum, severe heartburn and difficulty swallowing.
In the absence of comprehensive measures, diet and proper rehabilitation, severe esophagitis leads to stenosis, progression of dysphagia, scar formation, and regurgitation of digested food. Late diagnosis and lack of therapeutic correction for esophagitis are dangerous due to the occurrence of bloody vomiting, as well as painful shock.
Symptoms of chronic esophagitis
Chronic esophagitis is characterized by:
- chest pain;
- belching;
- heartburn.
In infants, insufficient production of the sphincter of the digestive system can be determined by repeated regurgitation after feeding and symptoms of malnutrition.
If you experience similar symptoms, consult your doctor
. It is easier to prevent a disease than to deal with the consequences.
Diagnosis of esophagitis
Localization of painful symptoms in acute esophagitis in most cases allows you to quickly identify the pathology and prescribe the necessary laboratory and computer tests.
In the acute stage of the disease, the following is carried out:
- fluoroscopy with barium (if necessary);
- endoscopic biopsy;
- X-ray of the esophagus
; - Abdominal ultrasound
; - esophagoscopy;
- histology.
In case of congenital malformations of the esophagus, impaired motor function can be detected by esophagomanometry. The study gives an accurate picture of the contractile activity of the esophagus, displays peristalsis, the work of the upper and lower esophageal sphincters. Esophagomanometry is prescribed to patients with suspected atypical functioning of the esophagus (dysphagia, dyspepsia, odynophagia), as well as at the preparatory stages for antireflux operations.
General recommendations for the treatment of esophagitis
After confirming the diagnosis of esophagitis, patients should:
- Identify and eliminate irritants that provoke the development of the inflammatory process.
- After consultation with a specialist, start taking antacid gels and coating medications.
- Quit smoking (nicotine irritates the mucous membranes).
- Prohibition on consumption of alcohol and carbonated drinks.
- Follow a strict diet: avoid spicy, rough, sour, spicy, fatty and hot foods.
- Prohibition on taking tranquilizers, theophylline, prostaglandins, sedatives.
- The last meal should be 2 hours before bedtime.
- Do not wear clothes that are tight or tight at the waist.
When undergoing therapy and rehabilitation, it is important to maintain activity and a healthy lifestyle.
Treatment of acute esophagitis
- If the disease was caused by a chemical burn of the esophagus. For 1-2 days, food intake is limited, gastric lavage is performed and restorative drugs (famotidines and antacids) are prescribed.
- In case of obvious intoxication of the body. To maintain the metabolic, excretory, transport and thermoregulatory functions of the body, the specialist prescribes infusion therapy (parenteral administration of electrolytes, water, nutrients and medications). The second stage after the exacerbation is relieved is drug treatment to restore the esophageal mucosa and gastrointestinal reactivity.
- Acute esophagitis caused by infectious processes. A course of antibiotics and supportive therapy is prescribed.
- Ulcerative esophagitis. Enveloping drugs and anesthetics are recommended.
- Esophagitis with purulent foci. They rinse and prescribe a course of antibiotics. If purulent inflammation (phlegmon, abscess) does not go away, and the heavy structure of the esophagus is not prone to dilatation, surgical debridement is recommended.
- For serious pathologies of the esophagus that cannot be treated with medication, surgical correction is prescribed. It is possible to perform resection or plasty of the esophagus.
Treatment of chronic esophagitis
When treating chronic inflammation of the esophagus, drugs are taken that reduce the content of hydrochloric acid in gastric juice (antacids, inhibitors) and suspensions to enhance the tone of the cardia (cholinomimetics).
Positive dynamics of esophageal restoration during the treatment of chronic reflux esophagitis is achieved with physiotherapeutic influence:
- mud therapy;
- balneotherapy;
- amplipulse therapy;
- electrophoresis using ganglion blockers.
Full diagnostics and treatment can be completed in any modern gastroenterological center
.
Treatment of esophagitis with folk remedies
- 1st method – dandelion flowers. Yellow flowering dandelions (inflorescences) should be washed in cold water, sprinkled with sugar and crushed until juice appears. 1 teaspoon of the resulting syrup is diluted with ½ glass of purified water and taken 30 minutes before meals.
- Method 2 – potatoes with sugar. Potato tubers should be grated on a fine grater and the juice should be squeezed out of the resulting pulp. Dilute 1 teaspoon of sugar in ½ glass of potato juice and take 15 minutes before meals.
- 3rd method – dill seeds. Dill helps to effectively relieve acute inflammation of the esophagus and heartburn. 2-3 teaspoons of seeds are poured into a glass of water (60-80°C) and covered with a lid for several hours. Drink 1 tablespoon of the strained solution 4 times a day 15 minutes before meals.
- 4th method – Jerusalem artichoke. A couple of earthen pear tubers and one medium apple are grated and taken 2 times a day (between meals).
Prohibited Products
The list of prohibited foods includes those that provoke belching and heartburn, and also increase the secretion of gastric juice, that is, they are irritating (spicy, sour, cold and hot foods).
You should avoid taking extractives and essential oils: they stimulate the formation of hydrochloric acid.
You should also not eat foods rich in fats, since fats stay in the stomach for a long time and increase the secretion of gastric and pancreatic juices.
It is recommended to refrain from foods that increase gas formation.
List of prohibited products:
- fresh wheat and rye bread, muffins, fried pies, donuts, pancakes, pancakes, pastries;
- rich broths from meat, fish, poultry, okroshka, borscht, strong vegetable broths;
- fatty meat, stringy meat (duck, goose, pork);
- fatty, salted or pickled fish;
- canned meat and fish;
- lard, spicy sausages, smoked meats;
- fast food, semi-finished products;
- sour fruits and berries (citrus fruits, currants, green apples);
- vegetables containing coarse fiber (white cabbage, sauerkraut, radish, radish, bell pepper, eggplant, turnip);
- onions, garlic, sorrel, spinach, all types of legumes;
- ice cream, chocolate;
- spices (bitter and allspice, coriander, suneli hops, bay leaf and parsley/dill with caution, mustard, horseradish);
- high-fat dairy products, sour kefir;
- fried or hard-boiled eggs;
- sharp and fatty cheeses;
- kvass, strong tea and coffee, carbonated, especially sweet drinks;
- millet, pearl barley, corn, barley;
- large pasta
Consequences of esophagitis
Common complications of esophagitis:
- phlegmon, abscess;
- stenosis – narrowing of the esophagus;
- perforation – rupture of the walls of the esophagus;
- peptic ulcer (with Barrett's diagnosis);
- metaplasia - degeneration of the surface epithelium of the esophagus (precancerous condition).
Timely diagnosis of the disease will help to avoid complications and irreversible pathologies in the gastrointestinal tract. After completing a course of therapy, the patient must follow a diet for a long time, the recommended diet and undergo a follow-up examination.
Prevention of esophagitis
The best prevention of esophagitis and other gastrointestinal diseases is:
- Mode.
- Proper nutrition.
- Normalized intake of biostimulants.
- Consuming warm (but not hot) food.
- Quitting smoking and excessive alcohol consumption.
- Do not take antibiotics or other drugs without a doctor's prescription.
In case of chronic esophagitis, the patient must undergo regular medical examinations from the attending physician and go to sanatorium-resort treatment once or twice a year.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
There are several drugs that reduce the frequency of spontaneous (unprovoked) valve openings.
The most famous of them is baclofen .
This drug is popular among neurologists, they use it to reduce muscle spasticity.
The instructions do not officially indicate use for GERD!
There is a very small amount of scientific work on its use in children, but the available data say: the drug helps well with GERD, but the frequency of side effects from the central nervous system is quite high.
This drug is reserved for extreme situations.
In the next article, I will tell you when doctors suggest surgery to treat GERD in a child.
Photo at the beginning of the article from Tanaphong [email protected] _2chinda
3, total, today