An appendicular abscess is a delimited area of purulent inflammation of the peritoneum that arises as a result of destruction of the appendix. It manifests itself 5-6 days after the clinic of acute appendicitis with a sharp exacerbation of fever and pain, tachycardia, intoxication, and dyspeptic symptoms. The diagnosis is established after studying the anamnesis, performing a general blood test, ultrasound and radiography of the abdominal organs. An emergency operation is indicated - opening and draining the abscess. Antibacterial and detoxification therapy is prescribed; subsequently an appendectomy is performed.
General information
Appendiceal abscess is a serious and dangerous complication of destructive acute appendicitis - its phlegmonous, apostematous, phlegmonous-ulcerative or gangrenous forms. An appendiceal abscess can occur in the late period of the disease before surgery during suppuration of the appendiceal infiltrate or in the postoperative period due to the delimitation of the inflammatory process during peritonitis. According to experts in the field of abdominal surgery, the incidence of appendiceal abscess in acute appendicitis is 1-3% of cases.
Appendiceal abscess
Causes
An appendiceal abscess is usually caused by an association of Escherichia coli, non-clostridial anaerobic microflora and cocci. The suppuration of the appendiceal infiltrate with the development of an abscess is facilitated by the patient’s late seeking medical help and untimely diagnosis of acute appendicitis. After appendectomy, the development of an appendicular abscess can be caused by a decrease in the immunological reactivity of the body, high virulence of microorganisms and their resistance to antibiotics used, and sometimes by defects in surgical technique.
Pathogenesis
The formation of appendiceal infiltrate usually occurs 2-3 days after the first signs of acute appendicitis appear. Inflammation of the appendix does not spread to the entire abdominal cavity due to the protective physiological function of the peritoneum. The delimitation of the primary inflammatory focus in the caecum from the surrounding organs occurs due to the formation of fibrinous exudate, the development of adhesions and the fusion of the caecum itself with the loops of the large intestine, the portion of the caecum, the greater omentum and the parietal peritoneum.
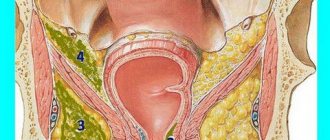
The formed appendiceal infiltrate can gradually resolve when inflammation in the caecum subsides (for example, after conservative therapy); when the appendix is destroyed and the infection spreads beyond its limits, it festers with the formation of an abscess. The location of the appendiceal abscess in the abdominal cavity depends on the location of the cecum: most often in the right iliac fossa; there may also be a retrocecal (retroperitoneal) or pelvic location of the abscess.
Periappendicular abscess
Surgery for intra-abdominal abscesses
One of the most important features of the peritoneum is its ability to delimit foci of infection.
from an infection-free abdominal cavity.
This delimitation occurs first due to fibrinous adhesions,
and later due to increasingly
dense adhesions.
It is thanks to this protective mechanism that the body in many cases is protected from generalized peritonitis.
The infection can enter the peritoneum as a result of inflammatory diseases of the appendix, female internal genital organs, stomach, liver, bile ducts, etc., as well as during operations in which the lumen of any hollow organ was opened. Since the spread of local and parenteral antibiotics, the picture of generalized peritonitis has become less severe; now it does not pose such a formidable danger to the patient as before the era of antibiotics.
However, infectious agents located in isolated intra-abdominal abscesses usually do not respond to antibiotics because these drugs are unable to penetrate the thick membrane surrounding the abscess. At the beginning of the era of antibiotics, some authors believed that it was possible to treat an intra-abdominal abscess by rinsing its cavity with an antibiotic solution injected there after puncture through a thin catheter. This method of "conservative" surgical
treatment did not live up to expectations.
If sometimes a favorable result was obtained, it was only as a result of very long-term treatment with this method, often for many weeks. Currently, surgeons have returned to the old reliable rule: uib pus, ibi evacua
(where there is pus, evacuate there 1).
An encapsulated abscess can occur in any part of the abdominal cavity, but there are also typical places for its localization. Most often observed are periappendicular ab-
processes that occur after appendicitis, a very common disease.
In a patient lying on his back, as a result of lumbar lordosis, the middle part of the abdominal cavity is located highest. The deepest parts of the abdominal cavity are the Douglas and subphrenic spaces. Wherever there are infectious materials, they usually penetrate most easily down into these deep-lying places, accumulate here and cause an abscess. It would seem that purulent exudate, as a result of gravity, should first of all fall down,
in Douglas space.
This is how it usually happens, but it doesn’t stop there. There are two more mechanisms at work, under the influence of which the infection spreads upward
under the diaphragm. One of these forces is the suction action as a result of the movements of the diaphragm (under the diaphragm the pressure is lower than in the pouch of Douglas), the second is the suction action of the capillaries in the peritoneal fissure.
Abscesses of different locations have different clinical significance. Experience shows that the septic-toxic condition caused by an abscess is more severe the closer the accumulation of pus is to the dome of the diaphragm, and the easier it is the further from it. In accordance with this, the most severe conditions are observed with subdiaphragmatic abscess, and the mildest with abscesses of the pouch of Douglas. Periappendicular abscesses and abscesses located between the loops of the small intestine, in their severity, usually occupy a place somewhere between the above forms.
This clinical observation is obviously based on the fact that in the upper part of the abdominal cavity significantly more bacteria and toxic decay elements are absorbed into the lymphatics and general circulation than from the pouch of Douglas, and this absorption also occurs much faster. Movement
The release of these substances is enhanced by the movements of the diaphragm and the suction effect of subatmospheric (erroneously called negative) pressure in the chest cavity. Often, a subdiaphragmatic abscess is accompanied by pleurisy and empyema, which aggravate the serious condition of the patient.
Below we will consider only the surgical treatment of the most common, typical abscesses. There are no general rules for opening atypical abscesses that occur in other parts of the abdominal cavity. To open all forms of abscesses, one should, in principle, choose a treatment that provides the opportunity to drain the entire abscess cavity (even its deepest point) to the outside without the infection spreading to adjacent areas of the serous cover (peritoneum, pleura).
Opening an abscess is still referred to by the old term: oncotomy
(from Greek
onkos =
mass, tumor +
temnein
= cut).
This term is very unfortunate, since the designation "onko" is usually used in the field of medical science that deals with tumors - in oncology (onkos + logos =
law, word). In the two designations, only the part indicating an increase in mass is common. It would be correct to completely abandon the misleading term “oncotomy”.
Periappendiceal abscess is a known complication of acute appendicitis. With this complication, in the area of the right iliac fossa, resistance the size of a walnut to a fist is felt, which is spontaneous and painful on palpation. In thin patients, a protrusion is sometimes visible. General symptoms (fever, lethargy, leukocytosis) are usually typical, but with a low grade infection they may be absent. Periappendiceal infiltrate is difficult to distinguish from an abscess, and physical examination often does not make it possible to make a diagnosis. Rather, it helps to navigate the time that has passed since the onset of the disease, leukocytosis and temperature. Surgeons often mistake chronic periappendiceal infiltration in elderly people for a tumor of the cecum.
A periappendiceal abscess should be opened extraperitoneally.
On the right side of the palpable protrusion, parallel to the Poupart ligament, a skin incision 8-10
cm long is made.
After the individual muscle layers of the abdominal wall are dissected along the same line, the inflamed, edematous preperitoneal adipose tissue is widely exposed.
It is most advisable to go through the fatty tissue with a blunt instrument and then use a sharp finger to
eager to penetrate into the depths. If you approach the abscess from the side, then, as a rule, you first enter its cavity without opening the free abdominal cavity. As soon as pus begins to come out, the entrance hole into the abscess cavity is widened by repeatedly pushing apart the jaws of a blunt instrument. The cavity is palpated with a finger, possible pockets are opened bluntly, and the position of the appendix is determined.
When opening a periappendicular abscess, one should not strive to remove the appendix, since it is undesirable to delay the operation. In addition, one must be careful that when attempting to perform an appendectomy, the free abdominal cavity does not open and pus does not penetrate there, which can cause generalized peritonitis. An appendectomy should be performed simultaneously with opening the abscess cavity only in cases where the appendix is at hand and can be easily and quickly removed.
The widely opened abscess cavity is drained.
It is not recommended to use conventional drainage from a thick rubber tube, since in just 2-3 days it can cause a bedsore on the wall of the already inflammatory intestine.
The wall of the cecum, under constant pressure, becomes necrotic, and a fecal fistula occurs. It is best to use the so-called. cigarette drainage
made from a strip of rubber, or otherwise
drainage .
You can easily make it yourself from a rubber glove. This drainage ensures good drainage and prevents bedsores. 2-3 soft drainage tubes can be inserted into the large abscess cavity.
After a week, the drains are replaced with new ones, also soft. After a few weeks, the cavity is cleared, its walls are adjacent to each other. It is recommended to perform an appendectomy after a few months, because where a periappendiceal abscess has once appeared, a second one often appears.
An abscess of the pouch of Douglas usually occurs as a complication of inflammation of the appendix of the cecum or internal female genital organs. If 4-6 days after surgery there is a fever, leukocytosis, frequent urge to urinate and defecate in the lower abdomen, you should think about an abscess of the pouch of Douglas. The general condition of patients is usually good, the diagnosis is not difficult to make: by digital examination of the rectum, it is determined whether the anterior wall of the rectum protrudes in the form of an elastic formation, whether there is a pronounced fluctuation and significant sensitivity when pressed.
Rice. 5-497. Puncture for abscess of Douglas pouch with Rotter
Pie.
5-498.
Opening a Douglas pouch abscess with a Rotter
. A Douglas pouch abscess is opened through the rectum.
or
through the vagina.
It is important to completely empty the bladder by catheterization before surgery because damage to the bladder during puncture of the abscess is less likely when the bladder is completely emptied.
The patient is given anesthesia lying on his back and then placed in the position for stone cutting.
Autopsy through direct porridge.
The sphincter is stretched with 2-3 fingers according to
Recamier,
access to the rectum is provided with long spatulas. The most strongly protruding section of the anterior wall of the intestine is sought and, after smearing with iodine, it is punctured in the anterior direction with a puncture needle inserted
into the Rotter
(Fig. 5-497),
or with an ordinary long, thick injection needle.
If the tip of the needle gets into the abscess cavity, then
is usually emptied through the needle (you must first remove the mandrel
Rotter .
To ensure free outflow of pus, the amount
which is sometimes more than one liter, you need to expand the hole made by the needle.
The easiest way to do this expansion is with the Rotter tool,
the forceps of which, using a groove, are guided along the puncture needle through the intestinal wall into the abscess cavity.
In the abscess cavity, the jaws of the forceps move apart, pus flows out freely (Fig. 5-498).
If you don't have a Rotter tool,
then the anterior wall of the rectum is pierced near the puncture needle with a sharp scalpel, and then an ordinary forceps or other blunt instrument is inserted through the hole into the abscess cavity.
After removing the needle between the two jaws of the forceps, a thick drainage tube is inserted into the abscess cavity, which is attached from the outside with a safety pin to prevent it from sliding deeper.
Opening through the vagina.
Using spatulas, access to the posterior vaginal fornix is provided, and the puncture needle is passed through it posteriorly into the abscess cavity. Then proceed in exactly the same way as when opening an abscess through the rectum.
After the operation, the drainage left in the abscess cavity is attached with a bandage so that it cannot slip out. After 2 to 3 days, the drainage tube usually comes out spontaneously with the first bowel movement. By this time, the abscess cavity is emptied to such an extent that the introduction of a new drainage tube is not required. It is almost incredible that in such a short time (just a few days!), under the influence of good drainage, a giant purulent abscess can be cured. If the abscess cavity, due to too early adhesion of the edges of the wound, fills again (increase in temperature, fluctuation), then its contents can easily be drained by blunt expansion of the hole.
Subphrenic abscess
Subdiaphragmatic are all abscesses that arise in the area between the diaphragm and the mesentery of the transverse colon or this colon itself, therefore, not only those that are in contact with the diaphragm, but also those abscesses that are located under the liver, because they all have a common etiology and pathogenesis and often occur simultaneously. .
The wide subdiaphragmatic region is divided by the organs and ligaments located in it into several spaces, which under normal conditions communicate with each other and in which, as a result of inflammatory adhesions
Symptoms of appendicular abscess
The onset of the disease is manifested by the clinical picture of acute appendicitis with a typical pain syndrome and increased body temperature. After 2-3 days from the onset of the attack, as a result of delimitation of inflammation in the caecum, the acute phenomena subside, the pain becomes dull, drawing in nature, the temperature decreases, and normalization of the general condition is noted. On palpation, the abdominal wall is not tense, participates in the respiratory act, in the right iliac region there is slight pain and the presence of a sedentary compaction without clear contours - appendicular infiltrate.
The development of an appendiceal abscess on the 5th–6th day of the disease is manifested by a deterioration in the general condition of the patient, sudden rises in temperature (especially in the evening), chills and sweating, tachycardia, symptoms of intoxication, poor appetite, intense pain of a pulsating nature in the right iliac region or lower abdomen, increasing pain when moving, coughing, walking.
On palpation, mild signs of irritation of the peritoneum are noted: the abdominal wall is tense, sharply painful at the site of the appendiceal abscess (positive Shchetkin-Blumberg sign), lags behind when breathing, a painful tight-elastic formation is felt in the right lower quadrant, sometimes with softening in the center and fluctuation.
The tongue is covered with a dense coating, dyspeptic symptoms are observed: stool disturbances, vomiting, bloating; with an interintestinal location of the appendiceal abscess - the phenomenon of partial intestinal obstruction, with a pelvic abscess - an increased urge to urinate and bowel movement, pain during defecation, discharge of mucus from the anus. When an appendiceal abscess ruptures into the intestines, there is an improvement in well-being, a decrease in pain, a decrease in temperature, and the appearance of loose stools with a large amount of foul-smelling pus.
Abscess appendicular
An appendicular abscess is a limited purulent inflammation of the peritoneum that develops as a result of a process in the appendix; it is a complication of acute appendicitis. It can be located in the right iliac fossa (interintestinal) or in the pouch of Douglas (in the pelvic cavity). The restriction of the abscess results from gluing of the peritoneum, and then the formation of adhesions between the intestinal loops, their mesenteries and the omentum. Symptoms and course:
Severe pain in the right iliac region or lower abdomen, the development of a painful infiltrate of a tight-elastic consistency, sometimes with signs of softening in the center, fever, vomiting, stool disturbances, etc. Digital examination through the rectum or vagina greatly helps in diagnosis. The resulting abscess can break into the intestinal lumen, which usually ends in self-healing, into the abdominal cavity - leading to diffuse peritonitis, into the retroperitoneal space - the development of phlegmon. Stages:
- The onset of the disease is a typical attack of acute appendicitis.
- If there are signs of acute appendicitis, the formation of an appendiceal infiltrate should be assumed within 2-3 days, and its abscess formation and development of an appendiceal abscess within 5-6 days.
- Palpation is a painful, immobile tumor-like formation in the right iliac region; its lower pole can be determined during vaginal or rectal examination.
- There are no clinical signs of widespread peritonitis.
- The ongoing treatment of appendiceal infiltrate is ineffective.
- Increase in body temperature to 39-40 °C with chills. Increase in infiltrate in size (approaching the anterior abdominal wall), increased pain on palpation.
- Increasing intensity of throbbing pain.
- The appearance of signs of peritoneal irritation.
- An increase in the difference between body temperature measured in the armpit and rectum.
- Skin hyperemia and fluctuation are late signs.
- In some cases - phenomena of intestinal obstruction, diffuse peritonitis.
Treatment:
Initially, conservative: antibiotic therapy, rest, diet, fight against intoxication. With a clearly limited abscess, surgical intervention is indicated: opening the abscess. In case of an abscess of the pouch of Douglas, the opening is performed through the posterior vaginal fornix or through the anterior wall of the rectum (after puncture of the abscess - along the needle). If the appendix is not removed, the inflammation of which is complicated by an abscess, an urgent operation is indicated: removal of the appendix, opening and drainage of the abscess cavity.
Surgical treatment: before surgery, premedication with antibiotics and metronidazole is necessary. Under general anesthesia, the abscess is opened; it is better to use extraperitoneal access. The cavity is washed with antiseptics and drained with double-lumen drainages for active aspiration of the contents with rinsing in the postoperative period. It is better to refrain from inserting tampons into the wound. In the postoperative period, detoxification therapy, antibiotics (aminoglycosides) in combination with metronidazole (Trichopol).
In the postoperative period, careful drainage care is carried out, washing and aspiration of the cavity contents, antibiotic therapy - a combination of aminoglycosides (Streptomycin, Gentamicin, Amgent, Garamicin, Amikacin, Selemicin, Farcycline, Amitsin) with metronidazole, detoxification and restorative therapy. The drainage remains until the purulent contents are separated from the wound. After removal of the drainage tube, the wound heals by secondary intention. If an appendectomy has not been performed, it is performed as planned 1-2 months after the inflammation has subsided.
Complications
Opening an appendicular abscess into the abdominal cavity leads to the development of peritonitis, accompanied by septicopyemia - the appearance of secondary purulent foci of various locations, increasing signs of intoxication, tachycardia, and fever. Complications include retroperitoneal or pelvic phlegmon, purulent paracolitis and paranephritis, liver abscess, subphrenic abscess, purulent portal vein thrombophlebitis, adhesive intestinal obstruction, urinary tract infections, abdominal wall fistulas.
Diagnostics
In recognizing an appendiceal abscess, data from anamnesis, general examination and the results of special diagnostic methods are important. During vaginal or rectal digital examination, the abdominal surgeon is sometimes able to palpate the lower pole of the abscess as a painful protrusion of the vaginal vault or the anterior wall of the rectum. The results of a general blood test for appendiceal abscess show an increase in leukocytosis with a shift in the leukocyte formula to the left, and a significant increase in ESR.
An abdominal ultrasound is performed to clarify the location and size of the appendiceal abscess and to identify fluid accumulation in the area of inflammation. A survey X-ray of the abdominal organs reveals a homogeneous darkening in the iliac region on the right and a slight displacement of the intestinal loops towards the midline; in the area of the appendicular abscess, the level of fluid and the accumulation of gases in the intestine (pneumatosis) are detected. An appendicular abscess must be differentiated from torsion of an ovarian cyst, diffuse purulent peritonitis, or a tumor of the cecum.
Surgery for intra-abdominal abscesses
An encapsulated abscess can occur in any part of the abdominal cavity, but there are also typical places for its localization. The most common are periappendiceal abscesses that occur after appendicitis, a very common disease.
In a patient lying on his back, as a result of lumbar lordosis, the middle part of the abdominal cavity is located highest. The deepest parts of the abdominal cavity are the Douglas and subphrenic spaces. Wherever there are infectious materials, they usually penetrate most easily down into these deep-lying places, accumulate here and cause an abscess. It would seem that purulent exudate, as a result of gravity, should first of all fall down into the pouch of Douglas. This is how it usually happens, but it doesn’t stop there. There are two more mechanisms at work, under the influence of which the infection spreads upward and under the diaphragm. One of these forces is the suction action as a result of the movements of the diaphragm (under the diaphragm the pressure is lower than in the pouch of Douglas), the second is the suction action of the capillaries in the peritoneal fissure.
Abscesses of different locations have different clinical significance. Experience shows that the septic-toxic condition caused by an abscess is more severe the closer the accumulation of pus is to the dome of the diaphragm, and the easier it is the further from it. In accordance with this, the most severe conditions are observed with subdiaphragmatic abscess, and the mildest with abscesses of the pouch of Douglas. Periappendicular abscesses and abscesses located between the loops of the small intestine, in their severity, usually occupy a place somewhere between the above forms.
This clinical observation is obviously based on the fact that in the upper part of the abdominal cavity significantly more bacteria and toxic decay elements are absorbed into the lymphatics and general circulation than from the pouch of Douglas, and this absorption also occurs much faster. The movement of these substances is enhanced by the movements of the diaphragm and the suction effect of subatmospheric (erroneously called negative) pressure in the chest cavity. Often a subdiaphragmatic abscess is accompanied by pleurisy and empyema, which aggravate the patient’s serious condition.
Below we will consider only the surgical treatment of the most common, typical abscesses. There are no general rules for opening atypical abscesses that occur in other parts of the abdominal cavity. To open all forms of abscesses, one should, in principle, choose a treatment that provides the opportunity to drain the entire abscess cavity (even its deepest point) to the outside without the infection spreading to adjacent areas of the serous cover (peritoneum, pleura).
Opening an abscess is still referred to by the old term: oncotomy (from the Greek onkos = mass, tumor + temnein = cut). This term is very unfortunate, since the designation "onko" is usually used in the field of medical science that deals with tumors - in oncology (onkos + logos = law, word). In the two designations, only the part indicating an increase in mass is common. It would be correct to completely abandon the misleading term “oncotomy”.
Periappendicular abscess
Periappendiceal abscess is a known complication of acute appendicitis. With this complication, in the area of the right iliac fossa, resistance the size of a walnut to a fist is felt, which is spontaneous and painful on palpation. In thin patients, a protrusion is sometimes visible. General symptoms (fever, lethargy, leukocytosis) are usually typical, but with a low grade infection they may be absent. Periappendiceal infiltrate is difficult to distinguish from an abscess, and physical examination often does not make it possible to make a diagnosis. Rather, it helps to navigate the time that has passed since the onset of the disease, leukocytosis and temperature. Surgeons often mistake chronic periappendiceal infiltration in elderly people for a tumor of the cecum. A periappendiceal abscess should be opened extraperitoneally. On the right side of the palpable protrusion, parallel to the Poupart ligament, a skin incision 8-10 cm long is made. After the individual muscle layers of the abdominal wall are dissected along the same line, the inflamed, edematous preperitoneal adipose tissue is widely exposed. It is most advisable to go through the fatty tissue with a blunt instrument, and then carefully penetrate into the depths with your finger. If you approach the abscess from the side, then, as a rule, you first enter its cavity without opening the free abdominal cavity. As soon as pus begins to come out, the entrance hole into the abscess cavity is widened by repeatedly pushing apart the jaws of a blunt instrument. The cavity is palpated with a finger, possible pockets are opened bluntly, and the position of the appendix is determined. When opening a periappendicular abscess, one should not strive to remove the appendix, since it is undesirable to delay the operation. In addition, one must be careful that when attempting to perform an appendectomy, the free abdominal cavity does not open and pus does not penetrate there, which can cause generalized peritonitis. An appendectomy should be performed simultaneously with opening the abscess cavity only in cases where the appendix is at hand and can be easily and quickly removed. The widely opened abscess cavity is drained. It is not recommended to use conventional drainage from a thick rubber tube, since in just 2-3 days it can cause a bedsore on the wall of the already inflammatory intestine. The wall of the cecum, under constant pressure, becomes necrotic, and a fecal fistula occurs. It is best to use the so-called. cigarette drainage made from a strip of rubber, or otherwise Penrose drainage. You can easily make it yourself from a rubber glove. This drainage ensures good drainage and prevents bedsores. 2-3 soft drainage tubes can be inserted into the large abscess cavity. After a week, the drains are replaced with new ones, also soft. After a few weeks, the cavity is cleared, its walls are adjacent to each other. It is recommended to perform an appendectomy after a few months, because where a periappendiceal abscess has once appeared, a second one often appears.
Abscess of Douglas pouch
An abscess of the pouch of Douglas usually occurs as a complication of inflammation of the appendix of the cecum or internal female genital organs. If 4-6 days after surgery there is a fever, leukocytosis, frequent urge to urinate and defecate in the lower abdomen, you should think about an abscess of the pouch of Douglas. The general condition of patients is usually good, the diagnosis is not difficult to make: by digital examination of the rectum, it is determined whether the anterior wall of the rectum protrudes in the form of an elastic formation, whether there is a pronounced fluctuation and significant sensitivity when pressed. The pouch of Douglas abscess is opened through the rectum or vagina. It is important to completely empty the bladder by catheterization before surgery because damage to the bladder during puncture of the abscess is less likely when the bladder is completely emptied. The patient is given anesthesia lying on his back and then placed in the position for stone cutting. Autopsy through direct porridge. The sphincter is stretched with 2-3 fingers using Recamier, access to the rectum is provided with long spatulas. The most strongly protruding section of the anterior wall of the intestine is sought and, after smearing with iodine, it is punctured in the anterior direction with a puncture needle inserted into a Rotter instrument, or with an ordinary long thick injection needle. If the tip of the needle gets into the abscess cavity, then foul-smelling pus is usually emptied through the needle (you must first remove the mandrel from the Rotter needle). To ensure the free outflow of pus, the amount of which is sometimes more than one liter, it is necessary to widen the hole made by the needle. The easiest way to carry out this expansion is with the Rotter instrument, the forceps of which are guided along the puncture needle through the intestinal wall into the abscess cavity using a groove. In the abscess cavity, the jaws of the forceps move apart, and the pus flows out freely. If there is no Rotter instrument, then the anterior wall of the rectum is pierced near the puncture needle with a sharp scalpel, and then an ordinary forceps or other blunt instrument is inserted through the hole into the abscess cavity. After removing the needle, a thick drainage tube is inserted into the abscess cavity between the two branches of the forceps, which is attached from the outside with a safety pin to prevent it from sliding deeper. Opening through the vagina. Using spatulas, access to the posterior vaginal fornix is provided, and the puncture needle is passed through it posteriorly into the abscess cavity. Then proceed in exactly the same way as when opening an abscess through the rectum. After the operation, the drainage left in the abscess cavity is attached with a bandage so that it cannot slip out. After 2-3 days, the drainage tube usually comes out spontaneously with the first bowel movement. By this time, the abscess cavity is emptied to such an extent that the introduction of a new drainage tube is not required. It is almost incredible that in such a short time (just a few days!), under the influence of good drainage, a giant purulent abscess can be cured. If the abscess cavity, due to too early adhesion of the edges of the wound, fills again (increase in temperature, fluctuation), then its contents can easily be drained by blunt expansion of the hole.
Subphrenic abscess
Subdiaphragmatic are all abscesses that arise in the area between the diaphragm and the mesentery of the transverse colon or this colon itself, therefore, not only those that are in contact with the diaphragm, but also those abscesses that are located under the liver, because they all have a common etiology and pathogenesis and often occur simultaneously. The wide subdiaphragmatic region is divided by the organs and ligaments located in it into several spaces, which under normal conditions communicate with each other and in which encapsulated abscesses can develop as a result of inflammatory adhesions and adhesions. The liver divides the subphrenic space into two parts: suprahepatic and subhepatic. The falciform ligament (lig. falciforme hepatis) divides the suprahepatic space into right and left parts. The right-sided suprahepatic space is divided by the frontally located right coronary ligament of the liver (lig. coronarium hepatis dextrum) into anterior and posterior parts. Since this ligament is located behind the highest point of the dome of the diaphragm, the anterior-superior space is larger than the posterosuperior one. On the right, under the liver, there is only one preformed lower space (spatium inferior), located between the lower surface of the liver, the anterior surface of the right kidney, the right flexure of the colon and (on the left) the round ligament of the liver. On the left, the left coronary ligament of the liver (lig. coronarium hepatis sinistrum) runs so far behind that there is only one suprahepatic space (spatium superior). On this side, however, the subhepatic space is divided by the hepatogastric ligament (lig. hepatogastricum) located in the frontal plane and its continuation, the stomach, into two segments: the posterior-inferior and the anterior-inferior. The posteroinferior space is also called the omental bursa (bursa omentalis). Subphrenic abscess occurs on the right side approximately seven times more often than on the left. It is always accompanied by more severe clinical symptoms than periappendicular abscess or Douglas pouch abscess. The general condition of patients is usually poor. They are lethargic, intermittent fever is noted along with a shift in the leukocyte count to the left, indicating a septic or toxic condition. With a suprahepatic abscess, the presence of concomitant pleurisy is almost natural. Often the abscess contains a greater or lesser amount of gas, which is easily diagnosed by X-ray examination as a result of mirror reflection. A wide opening of the subphrenic abscess and its good drainage, stopping the accumulation and retention of pus (the drainage tube is brought to the deepest point of the abscess cavity), is always urgently necessary. The abscess should be opened extraperitoneally and extrapleurally to prevent the occurrence of life-threatening generalized peritonitis or empyema. The course of the operation is illustrated by the example of opening a right-sided suprahepatic abscess located in the posterior-superior and anterior-superior spaces.
Right suprahepatic posterosuperior abscess
To open a suprahepatic right-sided postero-superior abscess, located essentially behind the liver, the patient under intratracheal anesthesia (during the operation there is a risk of developing a right-sided pneumothorax) is turned onto the left side, a cushion is placed under his lower back on the left side so that the right side of the lower back does not sink . The patient is fixed in this position to the operating table. The abscess cavity is best opened from behind, subpleural-transdiaphragmatically. For orientation, the course of the XII rib, as well as the spinous process of the 1st lumbar vertebra, is palpated and marked by scratching. The inflection line of the parietal layer of the pleura goes from the diaphragmatic part to the costal ( sinus phreni-cocostalis) almost horizontally, slightly higher, or slightly lower, but always intersects the XII rib running obliquely. If, on the patient’s body in a standing position, a horizontal line is drawn on the injury of the spinous process of the 1st lumbar vertebra, then it will certainly be located under the line of inflection of the pleura . The skin, adipose tissue and latissimus dorsi muscle are dissected along the right XII rib. The periosteum of the 12th rib is cut with a scalpel, after which the rib is exposed with a raspator along its entire circumference. The rib is then resected. Special care is required to avoid opening the pleural cavity. Using a transverse incision at the level of the spinous process of the 1st lumbar vertebra, the lower pole of the bed of the right XII rib and to the left of the fiber of the inferior posterior serratus muscle (m. serratus posterior) and to the right of the non-XI intercostal muscle are intersected. Directly below them is a part of the diaphragm emanating from the arcuate ligament (arcus luinbocostalis), which only occasionally contains strong muscle fibers and is usually a thin aponeurosis-like formation. This formation is also intersected along the line of the horizontal incision, and now the renal fascia is visible in the lower corner of the wound and above it, in the upper corner of the wound, the liver. By moving the index finger of the right hand behind the kidney and liver deep and upward, the posterior parietal peritoneum is separated from the inner surface of the diaphragm, and as soon as the abscess is palpated, it is opened bluntly. If the abscess is not immediately found upon palpation, then it is found by aspiration using a syringe with a long puncture needle. Due to the proximity of a number of thin-walled veins (inferior vena cava, right renal and hepatic veins), it is recommended that a soft Penrose drainage (one or more) be placed in the widely opened abscess cavity rather than a hard rubber drainage tube. From the same access it is possible to open an encapsulated abscess located subhepatically in the spatium inferior, which, however, is more accessible from the front.
Right suprahepatic anterior superior abscess
To open a right-sided suprahepatic anterior-superior abscess, the patient is placed on the left side under intratracheal anesthesia, as for opening a posterosuperior abscess. The abscess cavity is opened first from the front, subpleurally (subphrenic) and extraperitoneally. An incision about 10 cm long is made under the right costal arch and parallel to it from the xiphoid process outward and downward. All layers of the abdominal wall are intersected along this line up to the peritoneum. Passing upward with a finger, they bluntly separate the parietal peritoneum from the inner surface of the diaphragm until they reach an abscess, the wall of which is punctured, and then its cavity is widely opened. According to the author’s experience, an abscess of this localization in a patient lying in bed on his back is poorly drained towards the anterior abdominal wall, i.e. upward, in the direction opposite to gravity, because at the deepest point of the abscess and after opening its cavity there is still pus accumulates. To prevent retention of pus, the author has developed a simple method: a counterperture is applied at the back, so that the abscess cavity can be drained in this direction. A long curved forceps is inserted into the abscess cavity opened in front, its blunt end is passed along the dome of the diaphragm (along the convex surface of the liver), between the muscle and the surface of the liver posteriorly. If the abscess has not destroyed the right coronary ligament of the liver, then it is clearly felt when the end of the instrument is turned laterally (towards the right side of the patient’s body) and where the upper and posterior layers of the coronary ligament lie close to each other, the ligament is pierced from front to back. You can also do the following: turn the end of the instrument even more to the right and, bypassing the ligament, insert it behind the liver. The end of the instrument is carried further, now along the posterior surface of the liver, down to the point where the skin under the XII rib clearly protrudes with its help. The tool should be guided so that its end is located at the deepest point. The protrusion of the skin should be below the horizontal line drawn through the spinous process of the 1st lumbar vertebra. A cross section is made at this location until the tip of the instrument appears in the skin wound. In this case, in front of the abdominal wall, only the handle of the instrument is usually visible, the branches of which pass through the entire body from front to back. The posterior opening expands, and now we see the amount of pus that is emptied here. The subdiaphragmatic space is abundantly drained with thick tubes (tubes) from the side of the posterior wound, and a strip of gauze is inserted into the anterior wound. This wound heals quickly, while the posterior wound heals only after the inflammatory process has completely ended. Daily abundant rinsing of the wound cavity with physiological sodium chloride solution accelerates its healing. The above method developed by the author may seem somewhat complicated in its description, however, in practice it is very simple, drainage is performed in just a few minutes, is safe and gives excellent results (Oergely). This method, even in seriously ill patients, leads to rapid detoxification and rapid recovery. Multiple abscesses in the abdominal cavity After perforation of any organ of the abdominal cavity (the vermiform appendix of the cecum, stomach, colon) multiple purulent-septic foci may appear between the loops of the small intestine, which often quickly spread throughout the entire abdominal cavity. In such cases, an abscess of the pouch of Douglas usually occurs. A similar purulent-septic process is accompanied by sequestering pancreatitis after removal of the sequester. If such a condition is discovered during surgery, then they strive to open all the pockets, empty all abscesses, wash their cavities and, with the help of washing and suction peritoneal drainage, help free the peritoneum from infection in the postoperative period. The occurrence of multiple abscesses in the abdominal cavity is a severe complication of the underlying disease. It can only be dealt with fully equipped with modern advances in surgery, but, unfortunately, this is not always possible.
Diffuse purulent peritonitis
Typically, diffuse purulent peritonitis occurs as a result of perforation of a hollow abdominal organ or severe damage to its wall, which becomes permeable. Only in rare cases is it caused by a perforated wound or iatrogenic harm (complication after surgery). Diffuse purulent peritonitis has always been a very frightening complication in abdominal surgery; its threat has now only decreased somewhat. In any case, the timely, systematic and effective use of modern methods makes it possible to more successfully combat purulent peritonitis than 30 years ago. This clinical picture is to some extent an extreme form of multiple abscesses in the abdominal cavity: pus is found throughout or almost throughout the peritoneal cavity. Diffuse purulent peritonitis is also spoken of if certain areas of the peritoneum (omental bursa, subdiaphragmatic space, right- and left-sided fissure along the transverse colon, etc.) are closed, isolated and there is no pus in them. Previously, if a surgeon discovered diffuse purulent peritonitis during an operation, it was strictly forbidden to rinse the abdominal cavity, so as not to transfer the infection with the rinsing liquid to areas not yet captured by it. Currently, views on this issue have changed radically. In case of diffuse diffuse peritonitis, not only suction of pus from the abdominal cavity is used, not only “drying” it with napkins, but also copious washing and rinsing of the abdominal cavity in order to most completely remove infectious and toxic substances from there. It is generally accepted that the risk of spreading infection with lavage fluid is much less than the benefit of removing infectious material from the abdominal cavity. During the operation, the abdominal cavity is washed generously with 15-20 liters of isotonic sodium chloride solution at body temperature. They strive to remove purulent-fibrinous exudate from the most remote corners of the abdominal cavity. An antibiotic can be added to the saline solution, but the point is not the antiseptic effect, but the most perfect mechanical cleaning of the abdominal cavity as possible. Since it is quite obvious that bacteria cannot be washed away from the parietal and visceral peritoneum and fibrin, rinsing should continue in the postoperative period until the patient’s body mobilizes all humoral and cellular defense mechanisms and overcomes the infection. The best method is lavage and suction drainage of the abdominal cavity. The essence of such drainage is that the operation is completed by removing several thin drainage tubes from the upper part of the abdominal cavity, from each encapsulated cavity separately (Douglas, subdiaphragmatic space, etc.), and thick drainage tubes from the lower part of the abdominal cavity onto the abdominal wall through special holes. cavities. Through thin tubes, 3-4 liters of saline or Ringer's solution (45-60 drops per minute) are injected dropwise during the day, and thick tubes are connected to Biilau suction or active suction. It is much easier to describe this method than to correctly implement the described measures in practice, since the tubes are often clogged, do not drain, the injected fluid does not flow out of the abdominal cavity, etc. In the postoperative period, one must strive very patiently to ensure that drainage is as long as possible and effective. Studies with a contrast agent have shown that even 3-4 days after the operation there is still no such adhesion of the loops of the small and large intestine that would not allow for extensive lavage of the abdominal cavity (Lick). Effective flushing and suction drainage leads to rapid detoxification of the patient. In this regard, the data of V.S. Savelyev is convincing. It can be firmly stated that, along with antibiotics, as well as maintaining water-salt balance and blood transfusions, well-carried out abundant washing and suction drainage of the abdominal cavity currently provide the greatest assistance in the fight against diffuse purulent peritonitis.
Treatment of appendicular abscess
At the infiltrate stage, emergency surgery for acute appendicitis is contraindicated; it is treated conservatively in a hospital setting: strict bed rest is prescribed, cold on the stomach for the first 2-3 days, then heat, a gentle diet, and antibiotic therapy. Laxatives and narcotic drugs are excluded. Sometimes, in order to resolve the infiltrate, perinephric novocaine blockades are prescribed. If the appendiceal infiltrate is completely resolved, a planned appendectomy is performed after 1-2 months, since repeated attacks of acute appendicitis, the development of infiltrate, abscess and severe complications are possible.
Treatment of a formed appendicular abscess is surgical: the abscess is opened and drained, access depends on the location of the abscess. In some cases, with an appendiceal abscess, percutaneous drainage can be performed under ultrasound guidance using local anesthesia. Surgical opening and emptying of the abscess is performed under general anesthesia using a right-sided lateral extraperitoneal approach.
In case of pelvic appendicular abscess, it is opened in men through the rectum, in women - through the posterior vaginal fornix with a preliminary test puncture. The purulent contents of the appendicular abscess are aspirated or removed with tampons, the cavity is washed with antiseptics and drained using double-lumen tubes. Removal of the caecum is preferable, but if this is not possible, it is not removed due to the risk of pus spreading into the free abdominal cavity, injuring the inflamed intestinal wall that forms the wall of the appendiceal abscess.
In the postoperative period, careful drainage care, washing and aspiration of the cavity contents, antibiotic therapy (a combination of aminoglycosides with metronidazole), detoxification and restorative therapy are carried out. The drainage remains until the purulent contents are separated from the wound. After removal of the drainage tube, the wound heals by secondary intention. If an appendectomy has not been performed, it is performed as planned 1-2 months after the inflammation has subsided.
Publications in the media
Appendiceal abscess is a complication of acute appendicitis, limited peritonitis (an abscess containing the appendix. Its walls can be the greater omentum, intestinal loops and other organs), located in the peritoneal cavity or retroperitoneal tissue (right iliac region, small pelvis, subphrenic space, retrocecal space ). Frequency : 14–19% of cases of appendiceal infiltration. The predominant gender is female, because Women often associate pain syndrome with diseases of the internal genital organs and do not consult a surgeon in a timely manner.
Etiology and pathogenesis • Abscess formation of appendiceal infiltrate (errors in diagnosis, inadequate treatment, late consultation with a doctor) • In case of progression, the abscess may break into the abdominal cavity with the development of peritonitis, into the retroperitoneal space (with the formation of retroperitoneal phlegmon) or into hollow organs (more often into the intestinal lumen).
Clinical picture • The onset of the disease is a typical attack of acute appendicitis. • If there are signs of acute appendicitis, the formation of an appendiceal infiltrate should be assumed within 2–3 days; within 5–6 days, its abscess formation and the development of an appendiceal abscess should be assumed. • Palpation - a painful, immobile tumor-like formation in the right iliac region, its lower pole can be determined during vaginal or rectal examination. • There are no clinical signs of widespread peritonitis. • The ongoing treatment of appendiceal infiltrate is ineffective ••• Increase in body temperature to 39–40 °C with chills ••• Increase in infiltrate in size (approaching the anterior abdominal wall), increased pain on palpation ••• Increasing intensity of throbbing pain ••• Appearance signs of peritoneal irritation ••• Increased difference between body temperature measured in the axilla and rectum • Skin hyperemia and fluctuation are late signs. • In some cases - phenomena of intestinal obstruction, diffuse peritonitis.
Laboratory studies • Gradually increasing leukocytosis with a nuclear shift to the left • Significant (up to 30–40 mm/h) increase in ESR.
Special research methods • Rectal or vaginal examination - severe pain, sometimes you can palpate the lower pole of the formation • Plain radiography of the abdominal organs - fluid level in the right half of the abdominal cavity • Ultrasound allows you to determine the size of the abscess and its exact location.
Treatment - surgical: opening and drainage of the abscess cavity • Anesthesia - general, with puncture drainage under ultrasound - local • Access is determined by the localization of the abscess •• Pirogov access is typical - right-sided lateral extraperitoneal •• For pelvic localization - access through the rectum or posterior vaginal fornix •• Percutaneous drainage under ultrasound or computed tomography (CT) control • Removal of the appendix is not the purpose of the operation, but if possible, it is preferable • The abscess cavity is washed with antiseptics • Double-lumen tubes are used as drainages for washing and active aspiration of contents in the postoperative period • B postoperative period - detoxification and antibacterial therapy.
Diet. In the initial period - diet No. 0.
Complications • Opening of an abscess into the free abdominal cavity, intestinal lumen, on the skin of the right iliac region • Sepsis • Pylephlebitis • Liver abscess
The prognosis is serious and depends on the timeliness and adequacy of surgical intervention.
ICD-10 • K35.1 Acute appendicitis with peritoneal abscess
Prognosis and prevention
If left untreated, an appendicular abscess can spontaneously rupture into the intestinal lumen, abdominal cavity or retroperitoneal space, sometimes into the bladder or vagina, and very rarely through the abdominal wall to the outside. The prognosis is serious, the outcome of the disease is determined by the timeliness and adequacy of surgical intervention. Prevention of appendiceal abscess consists of early recognition of acute appendicitis and performing an appendectomy in the first 2 days.
You can share your medical history of what helped you in the treatment of appendiceal abscess.