MESADENITIS
(Greek, mesos middle + aden gland + -itis; synonym
: mesenteric lymphadenitis, mesenteritis
) - inflammation of the lymph nodes of the intestinal mesentery.
Purulent M. was first described in 1913 by L. I. Malinovsky, acute M. - in 1926 by Vilensky and Khan (A. Wilensky, LL Hahn). In 1953, Maskhov (WI Masshoff) described M. caused by pseudotuberculosis pasteurella (Pasteurella pseudotuberculosis).
M. is divided into nonspecific (simple and purulent), tuberculous and pseudotuberculous. By wedge. In the course of the process, acute and chronic (recurrent) M. are distinguished.
Etiology and pathogenesis
nonspecific M. have not been finally clarified. Infectious agents can enter the lymph nodes of the intestinal mesentery enterogenously and lymphohematogenously from various primary foci located, for example, in the appendix, intestines, upper respiratory tract, lungs, etc.
Pathological anatomy
Macroscopically, with M., swelling of the mesentery of the small intestine is usually observed, in which, more often, enlarged, soft-consistency lymph is found in the area of the ileocecal angle. nodes. With purulent M., an infiltrate with necrosis and purulent fusion is formed at the site of lymph nodes. Gistol, examination of lymph nodes of the intestinal mesentery reveals lymphoid hyperplasia, leukocyte infiltration, and in tuberculous M. - a picture of specific inflammation. The progression of the process may be accompanied by inflammatory infiltration of adipose tissue of the intestinal mesentery and the development, for example, in tuberculous M., of specific peritonitis.
Clinical picture
The onset of acute nonspecific M. is usually sudden, with the appearance of cramping or constant pain, localized in the navel or to the right of it, lasting from several hours to 2-3 days. Along with this, there is an increase in temperature, increased heart rate, hiccups, nausea, vomiting, diarrhea or constipation, and sometimes hyperemia of the pharynx, face, herpes labialis. The history often contains indications of recent influenza or sore throat.
The general condition of patients in most cases remains satisfactory. It suffers significantly only with purulent M., which often occurs with severe intoxication. In this case, leukocytosis is usually determined, reaching 30,000 in 1 μl of blood and a shift in the leukocyte formula to the left. Hypoalbuminemia and an increase in globular fractions due to gamma globulin are also detected.
With chronic M. experience short-term, uncertain localization of abdominal pain, and periodic diarrhea or constipation occur. Against the background of hron, the process may worsen with a wedge, symptoms of acute M.
In a number of cases of tuberculous M. manifestations of tuberculosis of other organs are found.
Causes
The development of mesenteric lymphadenitis results from the entry of pathogenic microorganisms into the lymph nodes. Bacterial and viral infections can enter there from the inflamed intestinal wall or be carried in blood from chronic foci of infection. Thus, the disease can be diagnosed against the background of tonsillitis, infectious processes in the kidneys, and respiratory tract.
The risk group for the occurrence of mesenteric lymphadenitis includes patients with weakened immunity or congenital immunodeficiency. Mesenteric lymphadenitis is not an independent pathology, but a consequence of an existing infectious process in the body. The causative agents of the disease can be:
- viruses – cytomegalovirus, herpes virus, adenovirus, enterovirus;
- nonspecific bacteria - salmonella, E. coli, staphylococci, streptococci;
- specific bacteria - Yersinia, Mycobacterium tuberculosis.
Enteroviruses are the main cause of frequent watery diarrhea, increased gas formation and abdominal pain. The herpes virus can cause infectious and oncological processes in the body.
Diagnosis
When palpating the abdomen, pain occurs, muscle tension is determined in the right iliac and inguinal regions; symptoms of peritoneal irritation can be limited or diffuse, depending on the form of M. M. is characterized by McFadden's symptom - pain along the edge of the rectus abdominis muscle 2-4 cm below the navel; Klein's symptom - movement of the painful point from right to left when the patient turns from the back to the left side; Sternberg's symptom is pain on palpation along the line connecting the right iliac region with the left hypochondrium.
Through the anterior abdominal wall in tuberculous M., lumpy packets of dense lymph nodes can be palpated. With the help of auscultation, the so-called the “rasp” symptom is a friction noise between the sheets of peritoneum covered with tuberculous tubercles.
On a plain X-ray of the abdominal cavity, calcified lymph nodes may be visible. nodes. The diagnosis is confirmed by laparoscopy and positive tuberculin tests. However, most often the diagnosis is made only during surgery.
Differential diagnosis
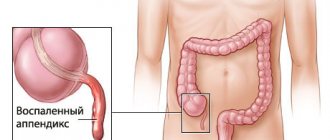
carried out with a number of surgical diseases of the abdominal organs, and primarily with acute appendicitis (see). In a number of cases, M. should be differentiated from lymphogranulomatosis (see), abdominal purpura (see Henoch-Schönlein disease) and acute infectious lymphocytosis (see Acute infectious lymphocytosis).
Complications
What complications can arise after mesadenitis? Mesenteric lymphadenitis usually responds well to conservative treatment. However, the progression of the pathology can lead to the development of complications and the need for surgery. Among the most likely consequences of mesadenitis, experts highlight the following:
- suppuration of the lymph nodes;
- abdominal abscess;
- peritonitis;
- generalized lymphadenitis;
- sepsis;
- adhesive formations;
- intestinal obstruction.
Abscess
An abdominal abscess is a localized abscess. The formation and progression of the disease is facilitated by the presence of the following bacteria:
- aerobic group: Proteus, Escherichia coli, staphylococci, streptococci;
- anaerobic group: clostridia, bacteroides, fusobacteria.
In the early stages, there are no symptoms characteristic of this particular pathology. Patients have a high body temperature, chills and tachycardia. There is severe nausea and loss of appetite. The muscles of the anterior wall of the abdominal cavity are sharply tense. There is also paralytic obstruction in the anus.
Abdominal pain above the navel
As the pathology develops, severe discomfort appears in the abdomen, stool and urination are disrupted. With the development of pathology in the subphrenic region, pain appears in the hypochondrium, radiating under the scapula.
The pain intensifies when you inhale. The patient’s walking also changes – the body tilts to the side. The most effective treatment for an abscess is surgery. In case of extensive purulent process, an incision is made in the anterior wall of the abdominal cavity.
For small abscesses, a drainage method is used. At any stage of the disease, antibacterial agents are prescribed. In addition, drugs are prescribed to suppress intestinal microflora.
The insidiousness of the disease is that even after surgery and cleansing of the organ, it can recur. If there are several abscesses, the prognosis is poor. According to statistics, from ten to thirty-five percent of patients die from an abdominal abscess.
Peritonitis
Peritonitis is an inflammation of the serous layer of the peritoneum. The difficulty of diagnosis lies in the fact that the manifestations of the pathology are similar to the signs of the diseases that caused this complication. The clinical picture largely depends on the stage of the pathological process, the nature of the pathology, the patient’s age and medical history.
The first stage of peritonitis develops rapidly and lasts for 24 hours. Symptoms are local. The patient's general condition is serious. The second stage is called toxic. Local signs gradually fade or disappear completely. Patients are in a confused state of mind and show complete indifference to what is happening. The temperature reaches 42 degrees, the pulse is practically not palpable.
The last, terminal stage is irreversible. The patients are in the intensive care unit and are connected to artificial life support. Multiple organ failure develops with dysfunction of almost all organs and systems of the body.
The survival prognosis directly depends on timely diagnosis and correctly selected treatment tactics. If the patient consulted a doctor when the first alarming signs appeared and was provided with competent medical care, a favorable outcome is observed in more than eighty percent of cases.
Treatment
Treatment of acute nonspecific M. is conservative: rest, antibiotics, desensitizing agents, physiotherapeutic procedures, perirenal blockades. With a wedge, a picture of an acute abdomen (see), laparotomy (see) is indicated. If it is performed for suspected acute appendicitis, then the operation is completed, as a rule, by removal of the appendix and lymph biopsy. node. A solution of novocaine with antibiotics is injected into the mesentery of the small intestine. For purulent M., the abscess cavity is opened and drained. In the postoperative period, antibiotics and physiotherapeutic procedures are prescribed. For tuberculous M., specific treatment is indicated.
Forecast
, as a rule, favorable.
Prevention
consists of timely sanitation of foci of hron, infection.
Folk remedies
Photo: wallpaperscraft.com
With such a disease, you should not hope that it will be possible to cope with it at home. Qualified medical assistance and immediate prescription of the necessary treatment are required. However, you can help your body fight the disease. You should start by following the regime. During the period of exacerbation, it is strictly bed rest; in the chronic course, you need to refrain from intense physical activity and lifting weights. It is also necessary to switch to a gentle diet. Meals should be fractional, at least 4 times a day. Dishes should be prepared in crushed or pureed form. During an exacerbation, special attention is paid to drinking plenty of fluids. This is necessary to remove toxins from the body, as a result, the symptoms of intoxication are reduced.
Infusions and decoctions of herbs will provide good help. The greatest effect for this disease is a decoction of blackberry root. The beneficial properties of blackberries have been known since ancient times. It has antipyretic, tonic, anti-inflammatory and bactericidal effects, which significantly helps in the treatment of mesadenitis.
As you know, decoctions and infusions with chamomile and calendula have analgesic and anti-inflammatory effects, which will help reduce pain and have a beneficial effect on the course of the disease.
A decoction of cumin will help normalize intestinal function. Both a decoction and an infusion of caraway seeds are used. In children under 7 years of age and in the acute stage of the disease in adults, preference is given to a decoction; in other cases, an infusion of seeds can be used.
It should be remembered that the listed options for folk remedies only help in alleviating symptoms, but for a complete recovery you should consult a doctor and strictly follow his recommendations.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Features of mesadenitis in children
M. in children is more often observed at the age of 6-13 years, which is explained by the anatomical and physiological characteristics of the child’s lymphatic system. M. in children can be primary and secondary. Primary M. occurs as an independent disease; secondary M. occurs as a reaction of lymph nodes during intestinal infections, acute respiratory diseases, etc.
Wedge, the picture of the disease in children is characterized by pronounced abdominal pain, which is often paroxysmal in nature and causes severe anxiety in the child due to intestinal spasms and irritation of mesenteric receptors. The temperature rises to 38° and above, pallor and increased moisture of the skin are noted. Complaints of nausea and, less commonly, vomiting are common.
In acute purulent M., which occurs relatively rarely in children, the general condition sharply worsens, signs of intoxication increase, and the temperature becomes hectic. With the help of palpation of the abdomen, it is sometimes possible to detect an increase in mesenteric lymph nodes.
Chron, a nonspecific inflammation of the lymph nodes of the mesentery, often occurs, in which children for a long time complain of cramping pain in the abdomen, not always of a specific localization - more often there is pain to the right of the navel and along the root of the mesentery. The principles of treatment and prognosis are the same as in adults.
Bibliography:
Anichkov N. M., Vigdorchik I. V. and Korolyuk A. M., Differential diagnosis of tuberculous and pseudotuberculous mesadenitis, Military medical. zhurn., No. 7, p. 38, 1977; Borukhovsky A. Sh. Pseudotuberculous mesadenitis, Surgery, No. 10, p. 57, 1976; DoletskyS. Ya. and K at z-m and e t e R. I. About the nosological differentiation of the so-called acute non-specific mesoadenitis in children, Vestn, hir., t. 102, No. 5, p. 87, 1969; K u l s a r t o v S. K. About the mechanism of pain in nonspecific mesenteric lymphadenitis, Surgery, No. 6, p. 91, 1973; Pekarsky D. E. and S and d o m i r s k i y B. P. “On the etiology and classification of mesoadenitis,” Doctor, case, No. 8, p. 129, 1967; Tkachenko L. I. About mesenteric lymphadenitis in children, Pediatrics, No. 11, p. 50, 1968; Sternberg A. Ya. On the diagnosis of tuberculosis of the mesenteric glands, Doctor, newspaper, vol. 30, no. 15-16, p. 739, 1926; H a jdu N. Mesenteric adenitis in childhood simulating intussusception, Acta radiol. (Stockh.), v. 10, p. 130, 1970; Klein 4V. Nonspecific mesenteric adenitis, Arch. Surg., v. 36, p. 571, 1938; McFadden CDF Mesenteric lymphadenitis and its clinical manifestations, Brit. med. J., v. 2, p. 1174, 1927.
Yu. A. Nesterenko; A. F. Dronov (det. surgeon).
General information
There are hundreds of lymph nodes in the abdominal cavity that protect against the spread of infection. When the mesenteric glands react to the introduction of pathogens, they enlarge and become painful, causing discomfort in the abdomen.
Mesenteric adenitis is more often diagnosed in childhood. The danger of the disease is due to the fact that there is a high risk of a purulent process. A rupture of an abscess is fraught with the development of peritonitis (inflammation of the peritoneum), which can cause death. Also, in severe cases of the disease, there is a possibility of sepsis – blood poisoning.
Interesting! Research shows that those who have had mesadenitis in childhood and adolescence have a reduced risk of developing ulcerative colitis.
The causes of mesadenitis are most often associated with an attack by pathogens. Already formed foci of infection in other organs, for example, the intestines or bronchi, play a great role in the pathogenesis (mechanism of development) of pathology. Viruses and bacteria can enter the lymphatic system through the intestinal lumen, blood or lymph.
Mesadenitis develops against a background of weakened immunity. The etiology of the process is often associated with existing diseases of the digestive tract. Pathology can be acute or chronic. The first case is characterized by a sudden increase in clinical symptoms and the presence of pronounced accompanying signs. Chronic lymphadenitis has an erased course. The process takes a long time.
Mesenteritis can be nonspecific (simple and purulent), tuberculous and pseudotuberculous. The exact causes of the first type of disease are still unknown. When tuberculous mycobacteria enter the mesentery, the second type of mesadenitis develops.