Blind but dangerous
The appendix is a short and thin blind vermiform appendix 7-10 cm long, located at the end of the cecum (the initial part of the large intestine). Like any part of the intestine, the appendix produces intestinal juice, but so little that it does not play a special role in digestion. Therefore, for a long time it was considered a “mistake of nature” and was removed by the patient at the first opportunity. But recently, scientists discovered lymphoid cells in the caecum, the same as in human tonsils. And since these cells have the properties to protect the body from infections, the assumption was born that the appendix is part of the immune system.
However, the number of protective cells in it, as it turned out, is very insignificant and cannot have a strong effect on the immune system. So most experts are still confident that there is no benefit from the appendix, but the harm in case of its inflammation can be significant: acute appendicitis not diagnosed in time can cost not only health, but also life.
Chronic appendicitis
– a condition in which patients are bothered by periodic abdominal pain, characteristic of acute appendicitis, but the inflammation that begins in the appendix does not progress to the purulent stage and is stopped without surgical intervention (this does not exclude the possibility that purulent appendicitis will develop during the next exacerbation). The diagnosis of chronic appendicitis is made only after excluding all diseases that can give a similar picture - irritable bowel syndrome, colitis, Crohn's disease, etc. Treatment is surgical - the appendage is removed as planned.
Are your teeth to blame?
Experts do not agree on the exact causes of appendicitis. However, risk groups have been identified.
For example, people suffering from diseases such as chronic tonsillitis, pneumonia, persistent colds, diseases of the gastrointestinal tract, caries. As a result of these diseases, infections penetrate through the bloodstream into the appendix and provoke an inflammatory process there. So healthy teeth are the key to a healthy appendix.
There is also a stress theory. It is based on the fact that as a result of excitement in a person, a sharp narrowing of the blood vessels occurs and this leads to sudden bleeding of the appendix and the development of its inflammation.
But most often the occurrence of appendicitis is explained by blockage of the junction of the colon and the appendix, which often happens with constipation and chronic colitis.
Release form and composition
Available in the form of tablets and in the form of an injection solution. The active ingredient is drotaverine.
Papaverine has a similar effect to No-shpu. But this drug is less active, the antispasmodic effect is not so pronounced, and the duration of action is short.
Drotaverine is effective for both muscular and neurogenic spasmodic phenomena. It is worth noting that the medicine does not affect the central nervous system. It is also absolutely safe to use during pregnancy. Due to the rapid absorption of the drug into the bloodstream, uniform distribution occurs throughout all tissues of the internal organs.
How to identify him?
In most people, the appendix is located approximately halfway between the navel and the right ilium. In this place, with appendicitis, the maximum pain is felt. But if the appendix is raised to the right hypochondrium, closer to the liver, pain will appear in this area. And if the appendix is lowered into the lower part of the pelvis, then in women appendicitis is easily confused with inflammation of the appendages, in men - with the bladder.
When the process is located behind the cecum, when it is wrapped towards the kidney and ureter, pain occurs in the lower back, radiating to the groin, leg, and pelvic area. If the process is directed inside the abdomen, then pain appears closer to the navel, in the middle abdomen and even in the pit of the stomach.
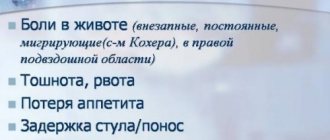
Pain occurs suddenly, without any obvious reason . At first they are not too strong - they can still be tolerated. And sometimes, from the first minutes of an attack of acute appendicitis, they become unbearable and proceed like colic.
The pain will torment a person as long as the nerve endings of the appendix are alive. When its necrosis occurs, the nerve cells will die and the pain will subside. But this is no reason to calm down. . ” On the contrary, the resolution of pain is a reason for immediate hospitalization. Acute appendicitis is accompanied by other symptoms. At the onset of the disease, general malaise, weakness, and loss of appetite appear. Nausea and sometimes vomiting may soon occur, but only once. A typical temperature ranges from 37.2 to 37.7 degrees, sometimes accompanied by chills. A white or yellowish coating appears on the tongue.
Simple techniques will help you recognize appendicitis. But keep in mind that self-diagnosis must be carried out very carefully.
Lightly tap with the pad of your bent index finger in the area of the right ilium - with appendicitis it always hurts there.
For comparison, also tap on the left iliac region, which in case of inflammation of the appendix will not cause pain. Attention: you cannot carry out palpation (feeling the abdomen with your hands) yourself, there is a danger of rupturing the appendix, which usually leads to peritonitis.
Try coughing loudly: increased pain in the right iliac region will tell you that you have appendicitis.
Apply gentle pressure with your palm to the area of your abdomen where it hurts the most. Hold your hand here for 5-10 seconds. The pain will ease slightly. Now remove your hand. If pain appears at this moment, this is a sign of acute appendicitis.
Take a fetal position, that is, lie on your right side and pull your legs towards your body. With appendicitis, abdominal pain will ease. If you turn on your left side and straighten your legs, it will intensify. This is also a sign of acute appendicitis.
But self-diagnosis should be limited to this. Do not hesitate to consult a doctor, since appendicitis itself, and all the diseases that it can masquerade as (renal colic, exacerbation of pancreatitis or cholecystitis, peptic ulcers of the stomach and duodenum, acute inflammation of the bladder, kidneys, female organs), require hospitalization!
Treatment protocol for patients with acute appendicitis
Classification:
Morphological form: catarrhal, phlegmonous, gangrenous.
Complications: appendiceal infiltrate, perforation, appendiceal abscess, peritonitis (limited, widespread), retroperitoneal phlegmon, pylephlebitis.
Diagnostics.
In the emergency department, after examination by a surgeon, within 1 hour from the time of admission, the patient should undergo the following tests: general clinical blood test, blood biochemistry, coagulogram, general urinalysis, blood group and Rh factor, ECG, chest x-ray and abdominal cavity, ultrasound examination of the abdominal cavity.
In cases of unclear clinical picture, computed tomography of the abdominal cavity and pelvis is performed. All female patients are subject to examination by a gynecologist. If necessary, consultations are carried out with a urologist and a therapist.
If the clinical picture is unclear and there are no obvious signs of other acute surgical pathology, dynamic observation is indicated for 12 hours with an assessment of clinical and laboratory instrumental data over time.
If an unclear clinical picture persists after a 12-hour observation and it is impossible to exclude acute appendicitis, as well as for the purpose of differential diagnosis with other acute diseases of the abdominal and pelvic organs, diagnostic laparoscopy is indicated as the final stage of diagnosis, which, if necessary, can be transformed into laparoscopic appendectomy.
In any doubtful cases, if it is impossible to exclude acute appendicitis, the choice of treatment is decided in favor of surgery. If a diagnosis of acute appendicitis is established, surgical treatment should be started within 2 hours from the moment of diagnosis.
Anesthesia.
The priority option is combined endotracheal anesthesia.
Surgical tactics.
The priority is to perform video laparoscopic appendectomy.
Contraindications to videolaparoscopic appendectomy are: severe cardiovascular and respiratory failure, widespread peritonitis, severe adhesions in the abdominal cavity, severe scarring on the anterior abdominal wall due to previous operations. If there are contraindications to videolaparoscopic appendectomy and there are no indications for performing a median laparotomy (see below), appendectomy from the Volkovich-Dyakonov approach is indicated.
During laparoscopic appendectomy, the mesentery of the appendix is coagulated in parts using Ligasure bipolar electrocoagulation and divided. The base of the process is ligated with three ligatures to form Reder nodes. Between two distal ligatures, the appendix is intersected, the stump is treated with iodine or alcohol, then, depending on the diameter, the appendix is removed from the abdominal cavity through a trocar or in an endocontainer through a trocar incision.
If there are inflammatory changes in the area of the base of the appendix, its stump, after preliminary ligation with a ligature, is immersed in a purse-string and (or) “Z”-shaped suture. If it is impossible to reliably cover the stump of the appendix with a purse-string and (or) “Z”-shaped suture, resection of the dome of the cecum with the stump of the appendix using Eshelon or EndoGia devices is recommended. The operation always ends with at least one drainage tube left in the pelvic cavity.
If there is a visual picture of catarrhal appendicitis and the clinical picture of the disease does not correspond to morphological changes, an additional inspection of the ileum (at least 1 meter) and uterine appendages for the pathology of these organs is indicated.
With secondary (superficial) appendicitis, the main (primary) pathological process is sanitized; appendectomy is performed only in the presence of a destructive form of inflammation of the appendix (phlegmonous, gangrenous).
The removed vermiform appendix is sent for histological examination. The effusion and contents of abscesses are sent for bacteriological examination to identify the microflora and its sensitivity to antibiotics.
In cases where widespread fibrinous (purulent-fibrinous) peritonitis is detected during surgery, midline laparotomy and appendectomy are indicated (see section “Peritonitis”).
The use of antibiotics in acute appendicitis.
- Antibiotic prophylaxis.
Antibiotic prophylaxis is indicated in all cases of surgery for acute appendicitis.
Antibiotic prophylaxis is carried out with generation cephalosporins. The first dose of the drug (2 g) is administered intravenously 30 minutes before the start of surgery.
In case of acute catarrhal appendicitis, 2 g of the drug is re-administered after 12 hours.
For destructive forms of appendicitis, antibacterial therapy is carried out in the postoperative period.
- Antibacterial therapy.
In case of acute phlegmonous appendicitis, therapy is carried out with generation cephalosporins in a dosage of 2 g x 2 times a day - 5 days.
In acute gangrenous appendicitis, with complications such as perforation, abscess, peritonitis, a combination of third-generation cephalosparins (4 g/day), aminoglycosides (amikacin 7.5 mg/kg - 2 times a day), metronidazole (2 g/day) is indicated. .
Surgical tactics for appendiceal infiltration.
The clinical and instrumental picture of appendiceal infiltrate without signs of abscess formation is a contraindication to surgery - hospitalization, conservative therapy (antibacterial, local hypothermia), computed tomography, ultrasound in dynamics are indicated in order to exclude its abscess formation. After resorption of the infiltrate, patients should be examined (after 3-6 months) and, if necessary, operated on as planned. In cases of abscessation of the appendiceal infiltrate, confirmed by ultrasound or computed tomography, opening and drainage of the abscess under ultrasound control or extraperitoneal access according to Pirogov is indicated.
If laparoscopy reveals a dense appendiceal infiltrate, drainage of the abdominal cavity is performed. If a dense appendicular infiltrate is detected during a traditional operation, appendectomy is unacceptable - the area of infiltration should be delimited by 2-3 gauze swabs removed through the wound. In the future, these patients are given antibacterial therapy until the infiltrate is resorption.
To drink or not to drink no-shpu
It is the patient’s personal decision to accept or refuse an antispasmodic drug.
An adult can withstand severe pain. The child’s nervous system has not fully formed, and the pain threshold is lower than that of an adult. Therefore, when pain occurs in the abdominal area, the doctor allows the baby to be given one tablet of No-shpa. This is the only drug that acts only on the place where the muscles are constrained by spasm. The nervous system remains intact, but the child’s condition improves significantly.
Contraindications
It is worth noting that this drug has contraindications:
- Individual intolerance to the active substance contained in the product.
- Kidney dysfunction.
- Insufficient liver functionality, decreased activity.
- Diseases of the cardiovascular system in acute or chronic form.
- The tablet contains an auxiliary component - lactose monohydrate. For people suffering from intolerance to this component, taking No-shpa is prohibited. This applies to people with impaired absorption of carbohydrate compounds.
- Small children under six years of age should not take the product.
- Breastfeeding period. Absorption into the bloodstream and subsequent distribution throughout the body leads to the fact that No-spa ends up in breast milk.
Side effects
Before taking pills, you should consult your doctor. If the doctor's recommendations and instructions are not followed, undesirable effects occur, called side effects:
- From the digestive tract, there is constant nausea and lack of stool, which in case of appendicitis negatively affects the patient’s condition.
- In the central nervous system, the drug provokes headache, dizziness and sleep disturbance (absence).
- Cardiac system. The heart rate rapidly increases and tachycardia occurs. Blood pressure drops and hypotension develops.
- Allergy. It manifests itself as itching, skin rash, and urticaria. The skin of the face and genitals swells (angioedema develops). Anaphylactic shock may occur due to exceeding the permissible dose. The patient's blood pressure drops sharply, breathing stops, and the pulse increases.
If any of these symptoms of overdose appear, you should go to the hospital and stop taking the medicine.