Paraproctitis is an inflammation of the fatty tissue surrounding the rectum. The disease is accompanied by acute excruciating pain, persistent difficulties in defecation and emptying the bladder. In the absence of timely treatment, acute paraproctitis with a probability greater than 90% becomes chronic. With repeated exacerbations, there is a risk of the formation of fistulas, which, if events develop unfavorably, can open not only outward, but also into the abdominal cavity.
Prices for examination and treatment
General information
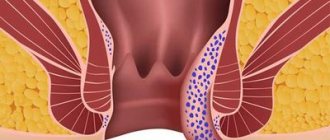
In proctology, acute paraproctitis is understood as an inflammatory process that arose in the peri-rectal tissues for the first time. The disease is an infectious pathology, accompanied by the formation of a cavity filled with pus in the tissue, which later opens into the pararectal area. Externally, it may look like a large abscess near the anus, very rarely on the buttock or inner thigh.
Chronic forms of paraproctitis occur with poor quality treatment or lack thereof. After their independent opening, the duct is scarred, the external opening is closed, but the purulent focus remains. Until it fills with exudate, the symptoms subside, and after the accumulation of pus, the process repeats.
In chronic paraproctitis, fistulas are formed - non-healing ducts, one end of which opens into the rectum, or rather in the bottom of the crypt (the depression next to the rectal sphincter, where mucus is synthesized to facilitate defecation), and the second - into the ampulla of the rectum, the perianal area, to the surface thighs or buttock, into nearby hollow organs (intestines, bladder, uterus, prostate).
The only way to eliminate paraproctitis, regardless of its form and stage, is surgical opening of the abscess, followed by drainage of the purulent cavity and suturing of the ducts.
Causes of paraproctitis
The cause of acute paraproctitis is inflammation of the Morganian crypt, a gland located in the recesses along the edge of the anal sphincter that synthesizes mucus. The source of problems is pathogenic flora - staphylococci or streptococci, Escherichia coli or Pseudomonas aeruginosa, clostridia, tubercle bacilli, etc. From the crypt, the infection spreads to the tissues located between the external and internal sphincter of the rectum, and then into the peri-rectal tissue.
Infectious paraproctitis often occurs against the background of decreased immunity or other diseases:
- digestive tract infections;
- chronic stool disorders;
- general exhaustion of the body;
- eating aggressive substances or foods containing particles that cannot be digested.
Other proctological diseases can provoke the onset of pathology:
- proctitis, or inflammation of the rectal mucosa;
- chronic hemorrhoids;
- acute or chronic anal fissure;
- cryptitis, or inflammation of the crypt;
- papillitis, or inflammation of the anal papillae.
In this case, the pathology is caused by the spread of the inflammatory process to deeper tissues.
Reasons for development
There are many factors that can contribute to the development of pathology. Among them:
- Frequent bowel disorders or constipation
- Infectious bowel diseases, E. coli
- STD
- Haemorrhoids
- Traumatization of the rectum
- Untreated anal fissures
- Colitis
- Crohn's disease
- Decreased immunity
- Poor nutrition – predominance of fatty and spicy foods in the menu
- Alcohol abuse
- Specific physical activity, lifting heavy objects
- Failure to comply with hygiene standards
The combination of reasons determines the main category of patients of the proctologist - most often men aged 25-50 years turn to the doctor with paraproctitis.
Classification
The official classification divides paraproctitis into acute and chronic. The first option includes inflammation that occurs for the first time. The second is a recurrent, that is, repeating pathological process. Acute and chronic paraproctitis is divided into types according to the localization of the purulent focus:
- subcutaneous - the abscess is located in the perianal area under a thin layer of external tissue, easily opens, rarely forms deep streaks and numerous ducts;
- intrasphincteric - the abscess is located between the layers of muscles of the external and internal sphincters, in the absence of therapy it can disrupt their functions, leading to fecal incontinence;
- ischiorectal - the abscess is located in the ischiorectal fossa deep above the anal sphincter muscles;
- pelviorectal - the purulent focus in this type of disease is localized in the depths of the small pelvis, and there may be no external ducts or abscesses on the skin of the perianal area. It is the pelviorectal form of paraproctitis that is most dangerous due to complications.
According to the stage of development, paraproctitis is divided into closed and open. The first is accompanied by acute inflammation without opening the abscess to the outside. The second is characteristic of the late stage of the disease, when the ducts independently open onto the surface of the skin or into the rectum.
Prices for examination and treatment
Diagnosis of paraproctitis
Diagnosis of subcutaneous paraproctitis is quite simple. The abscess, located in the subcutaneous tissue of the perianal zone, manifests itself quickly and clearly: pain, hyperemia of the skin on the affected side and smoothness of the folds of the perianal skin. When the abscess is located near the anus, it can take on a slit-like shape. Palpation in the area of inflammation is sharply painful, but there may not be fluctuations at first, since this symptom occurs later.
Ishiorectal paraproctitis can produce changes visible to the eye in the late stage, when pronounced asymmetry of the buttocks and smoothing of the perianal folds are noticeable. Therefore, if a patient comes in about chilling, deterioration in health, sleep, and at the same time he is bothered by dull constant pain in the rectum and pelvis, aggravated by defecation, but there are no visible changes in the anus, conduct a digital examination of the rectum. Already in the very early stages of the disease, it is possible to detect flattening of the intestinal wall above the anal canal, smoothness of the folds of the mucous membrane, the presence of compaction and sharp pain on the affected side.
Submucosal paraproctitis is diagnosed by digital examination of the rectum. Typically, a pronounced bulging of the abscess into the intestinal lumen is determined. Pus can spread both downward, into the subcutaneous tissue space, and upward, exfoliating the mucous membrane of the lower ampullary part of the rectum. Submucosal paraproctitis often opens spontaneously into the intestinal lumen and, if drainage is sufficient, spontaneous recovery may occur. Pelvic-rectal (pelviorectal) paraproctitis is the most severe and is often diagnosed late. The inflammatory process is localized deep in the pelvis. The upper border of the pelviorectal space is the pelvic peritoneum, the lower border is the levator ani muscle. External examination of the perineum usually does not allow diagnosing pelviorectal paraproctitis. Its signs, visible during an external examination of the patient, appear only in a late stage.
Pelviorectal abscess, as a rule, can be recognized using only digital examination of the rectum.
Symptoms of paraproctitis
The clinical picture for acute and chronic paraproctitis is similar except for details. In acute inflammation, the symptoms are pronounced, arise and grow quickly, and are accompanied by signs of general intoxication of the body. With chronic manifestations of inflammation intensify and subside in waves.
The main signs by which acute and chronic paraproctitis can be recognized:
- dull pain in the perianal area, radiating to the rectum, perineum, and sometimes to the lower back;
- local redness of the skin in the perianal area, sometimes involving the anal folds;
- swelling of the anal folds;
- the presence of a pronounced subcutaneous abscess in the perineum near the anus, on the buttock or inner thigh;
- discharge of pus from the anus during defecation or straining.
Against the background of the described symptoms, patients are worried about fever, increased body temperature, and fatigue.
Paraproctitis that has passed into the chronic stage is accompanied by less intense symptoms, since the contents of the abscess periodically leak out. This leads to relief of symptoms, but does not exclude their recurrence. With this form of the disease, permanent ducts are formed that connect the purulent focus with the surface of the body or internal organs - fistulas. After the outpouring of pus, the mouth tightens and opens again only after the re-accumulation of exudate.
Chronic paraproctitis (rectal fistulas)
If acute paraproctitis is not treated correctly, the abscess breaks out on its own, or under the influence of other factors, the internal opening of the abscess forms a fistula. A perianal fistula is a thin canal that connects the anus to an opening in the skin near the anus. Chronic paraproctitis is characterized by stages of remission and exacerbation.
Pus can accumulate in the lumen of the fistula, causing swelling and pain. The fistula can drain (break through) on its own, in which case the symptoms disappear for a while and return when the lumen of the fistula becomes clogged again. Periodic exacerbations occur due to constant infection of the fistula with pathogenic flora of the rectum.
Complications
Acute and chronic paraproctitis is fraught with life-threatening complications:
- purulent melting of the intestinal wall and fiber, as a result of which the contents of the gastrointestinal tract are poured into the peritoneal space, causing infection of organs and sepsis;
- peritonitis;
- rupture of an abscess into the rectum, vagina with their infection;
- formation of rectal-vaginal fistulas.
The most complex consequences are provoked by chronic paraproctitis. With its long-term existence, there is a risk of scarring of the ampulla of the rectum, as well as both anal sphincters (internal and external). As a result of this, there are:
- persistent problems with bowel movements;
- incontinence (incontinence of feces and gases);
- incomplete closure of the anus;
- malignant changes in damaged tissues.
To avoid this, do not ignore the symptoms of the disease or try to treat it yourself. Remember that paraproctitis cannot be eliminated by conservative methods! Even the “easiest” option requires surgical intervention and observation by a proctologist.
Diagnostics
Diagnosis of any type of inflammation of the perirectal tissue includes confirmation of the diagnosis based on existing symptoms, as well as differentiation of pathology from other proctological anomalies:
- teratomas of perirectal tissue;
- abscess of Douglas space;
- rectal tissue cysts;
- osteomyelitis of the lower spine;
- epithelial coccygeal duct;
- tuberculous fistulas and fistulas due to Crohn's disease.
To confirm paraproctitis, in addition to collecting anamnesis and complaints, use:
- laboratory blood test (a purulent process is indicated by an increase in leukocytes, neutrophils and ESR);
- physical examination of the rectum and perianal area (digital examination);
- anoscopy and sigmoidoscopy (these types of studies are not used for acute inflammation due to their pain and risk of sphincter spasm);
- canal probing or fistulography (x-ray contrast study);
- X-ray of the pelvic organs with or without contrast.
Diagnostic data helps to detect a purulent focus and all its ducts in order to choose the right treatment tactics.
Treatment of paraproctitis
The only way to eliminate the pathology without consequences for the overall health and functioning of the rectal sphincter is to perform surgery. During the operation, the doctor will open the abscess, drain its cavity and ducts, and remove the source of inflammation - the crypt. The tactics of surgery for acute and chronic processes differ slightly.
If the diagnosis reveals acute paraproctitis, the abscess is opened and drained under general anesthesia. The procedure takes place in several stages:
- Based on external signs or x-rays, the doctor opens the abscess and cleans it of purulent contents.
- Rinses the abscess cavity, treats it with antiseptics and antimicrobials.
- Excises necrotic tissue.
- Finds the source of inflammation (infected crypt) and excises it.
- Sutures wounds and, if necessary, leaves drainage tubes for drainage of exudate.
After the intervention, a course of anti-inflammatory drugs and antibiotics is prescribed. Until postoperative wounds are completely healed, a gentle diet that excludes constipation is recommended, as well as daily treatment of the perianal area with antiseptics.
In chronic forms of the disease, the purpose of surgical intervention is to eliminate the main source of inflammation and fistulas. It is carried out in the subacute period, when the abscess has already opened, but epithelization of the mouth has not yet occurred. In case of exacerbation, antibiotic therapy is first carried out, the fistulas are opened and drained, and then their excision begins. For this use:
- classic excision with a scalpel into the rectal lumen is a simple intervention suitable for removing fistulas located in the submucosa of the rectum;
- excision of the fistula with subsequent suturing of the fistula tightly and plastic surgery - differs from other methods by separating the mucomuscular flap and moving it to the mouth of the fistula to eliminate the risk of re-inflammation;
- ligature treatment of a fistula is a method that is used to eliminate high-lying fistulas, involving the introduction of a ligature into the duct with removal and fixation of its ends outward;
- Gabriel's operation - excision of the fistula using a probe, followed by cleaning the cavity and installing drainage until signs of inflammation are completely eliminated.
In modern proctology, lasers and radioknives are widely used to eliminate fistulous tracts and purulent lesions. They reduce the likelihood of infection of postoperative wounds and relapse of inflammation. When using them, the risk of scar tissue formation is lower, which makes the prognosis more favorable and reduces the risk of complications in the form of sphincter and rectal dysfunction.
Complications of paraproctitis
The most dangerous complication of acute paraproctitis is the spread of inflammation to the cellular spaces of the pelvis, purulent melting of the rectal wall. In this case, the intestinal contents enter the perirectal tissue and the possibility of widespread spread of infection opens up. There have been cases of purulent melting of the urethra. Considering the immediate proximity to the pelvic peritoneum and the communication of the pelvic tissue with the retroperitoneal tissue, we cannot exclude the possibility of pus breaking into the abdominal cavity and retroperitoneal space. Such complications, as a rule, arise when elderly, debilitated patients, diabetes mellitus or vascular disorders are late in visiting a doctor.
After opening the abscess spontaneously or surgically without eliminating the purulent tract and the affected crypt, a rectal fistula usually forms in the future. If a fistula has not formed, but a focus of inflammation remains in the area of the anal glands and intersphincteric space, then after some time a relapse of acute paraproctitis occurs.
Prognosis and prevention
With timely treatment, the prognosis for recovery is good. In the absence of medical care, acute forms of paraproctitis always progress to the chronic stage, and they are complicated by the spread of infection, purulent melting and necrosis of the pelvic organs, and sepsis.
To prevent paraproctitis, careful hygiene of the perianal area, adherence to PN standards to maintain normal stools, as well as timely treatment of proctological diseases are recommended.